Abstract
Purpose
To describe the natural history of nasal vestibulitis in patients receiving taxane chemotherapy, including incidence, severity, and associated symptoms.
Methods
Eligible patients with minimal or no baseline nasal symptoms were enrolled in this natural history study at initiation of a new chemotherapy regimen. Patients completed nasal symptom logs each time they received a chemotherapy dose. This manuscript reports upon the patients who received paclitaxel, docetaxel, or non-taxane non-bevacizumab chemotherapy. The proportions of patients within each cohort reporting any treatment-emergent nasal symptoms were estimated, with corresponding exact 95% confidence intervals. A cumulative incidence function was estimated within the chemotherapy cohorts to calculate the cumulative incidence rate of treatment-emergent nasal vestibulitis, treating death and disease progression as competing risks.
Results
Of the 81 evaluable patients, nasal symptoms were reported by 76.5% (58.8%, 89.3%) receiving paclitaxel, 54.2% (32.8%, 74.5%) receiving docetaxel, and 47.8% (26.8%, 69.4%) receiving non-taxane and non-bevacizumab chemotherapy. Of the three pairwise chemotherapy group comparisons, both the tests comparing the cumulative incidence function between the paclitaxel and non-taxane non-bevacizumab chemotherapy cohorts and between the paclitaxel and docetaxel cohorts achieved statistical significance at the 5% level with a higher incidence of treatment-emergent nasal vestibulitis in the paclitaxel cohort in both comparisons (P = 0.026 and P = 0.035, respectively). These significant differences were retained in the cumulative incidence function regression analysis controlling for age, smoking history, allergies, and asthma. Most patients in the paclitaxel cohort reported nasal symptoms as moderate or severe (56%).
Conclusion
Patients receiving paclitaxel chemotherapy experience a high incidence of nasal symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nasal vestibulitis—dryness, crusting, pain, and bleeding of the nares due to inflammation—was first reported in 2015, in patients receiving targeted therapy agents, such as tyrosine kinase inhibitors [1]. In 2018, this nasal symptom complex was reported among patients receiving chemotherapy [2]. In the latter study, the authors surveyed 100 patients at Mayo Clinic who had undergone at least 6 weeks of chemotherapy. While 41% of all of the surveyed patients reported nasal symptoms, 71% of those receiving taxanes reported such. After controlling for other factors, the odds of experiencing nasal symptoms was 4.86 times higher in taxane-receiving patients, compared to those who did not receive taxanes (90% CI: 2.01, 11.76).
The pathophysiology of nasal vestibulitis is not entirely clear. It has been postulated that cancer-directed therapies may disrupt the nasal epithelium, contributing to overgrowth of colonizing organisms, and thus cause nasal symptoms [3, 4]. In a prior study, the majority of patients reported that nasal symptom severity was moderate, or worse, and that they wished to discuss their symptoms with their oncology provider [2].
Pursuant to the above work, the current study was developed to prospectively characterize the natural history of nasal vestibulitis in patients receiving chemotherapy with taxanes and other chemotherapy agents.
Methods
Eligibility criteria
Patients were eligible for inclusion in this natural history study if they planned to undergo cancer treatment with (1) paclitaxel, (2) docetaxel, (3) nab-paclitaxel, (4) bevacizumab (without a concomitant taxane), or (5) a variety of other chemotherapy regimens that did not contain the above agents. Eligible patients needed to be scheduled to receive chemotherapy for 2–4 months and to be willing and able to complete questionnaires about nasal symptoms with each dose of chemotherapy. Patients were excluded from participation if they had received chemotherapy within the prior 3 months, had reported a predisposition to more than 1 nosebleed per month, or who verbally reported baseline dryness, pain, bleeding, or scabbing nasal symptoms of at least 3 on a 0–10-point Likert scale, from no nose symptoms (corresponding to a score of 0) to nose symptoms as bad as they can be (corresponding to a score of 10).
Study oversight
The protocol was approved per US federal guidelines, and patients provided IRB-approved informed written consent.
Protocol procedures
Patients were to complete a nasal symptom questionnaire at baseline, within 7 days prior to starting systemic antineoplastic therapy. This questionnaire asked about the presence of any nasal symptoms and symptom severity: on average, at best, and at worst, using 0–10-point Likert scales (from no nose symptoms, score of 0, to nose symptoms as bad as they can be, score of 10); additionally, patients were queried about details of their nasal symptoms regarding dryness, pain, bleeding, scabbing, and any other problems. They were also queried about their history of seasonal allergies, use of blood thinners including aspirin, smoking history, concurrent eye symptoms, and whether they had experienced nasal hair loss. These questions were informed by reports of nasal symptoms and other factors gleaned during a previous nasal vestibulitis survey study [2].
Patients were then asked to complete a similar nasal symptom log each time they received a dose of cancer-directed therapy. These nasal symptom log items mirrored questions from the baseline questionnaire, asking about the presence of any nasal symptoms, symptom severity, and description of nasal symptoms; they also asked patients about suspected causes for nasal symptoms and attempted treatments. Patients continued to complete symptom logs until the therapy regimen was stopped by their cancer provider (e.g., due to cancer progression or poor tolerability) or until 4 months had passed.
Chart reviews were conducted, and study personnel documented the cancer-directed therapy agents given at the time of each survey, whether nasal symptoms were noted in the chart and, if so, by which provider (nurse, advanced practitioner, physician) and provider treatment recommendations.
Statistical considerations
Patients were assigned to a cohort based upon receipt of one of the following therapies: (1) paclitaxel, (2) docetaxel, (3) nab-paclitaxel, (4) bevacizumab (without a concomitant taxane), or (5) a variety of other chemotherapy regimens that did not contain the above agents. Twenty-five patients were to be recruited to each cohort of this natural history study—with a goal of 20 evaluable patients per cohort. Evaluable patients were defined as having completed the baseline nasal symptom questionnaire, received at least 2 of their prescribed chemotherapy doses, and completed at least 2 corresponding follow-up nasal symptom questionnaires.
The primary endpoint was an event of treatment-emergent nasal vestibulitis (i.e., a score > 0), defined as an event of nasal vestibulitis that occurred post-baseline (i.e., after the 1st dose of chemotherapy) that was not present at baseline, or an event of nasal vestibulitis that worsened post-baseline, compared to baseline. The primary objective was to estimate the incidence proportion of treatment-emergent nasal vestibulitis, defined as the proportion of patients who, at any time during exposure to chemotherapy, reported at least one treatment-emergent event of nasal vestibulitis, overall and within each of the cohorts of patients. With 20 evaluable patients in each cohort, the maximum width of a two-sided 95% exact confidence interval for the incidence proportion was ± 22.8%.
For the primary analyses, binomial proportions of patients reporting any treatment-emergent nasal symptoms were estimated with corresponding exact 95% confidence intervals for the true but unknown population proportion. We also graphically summarized the estimated proportions according to the specific nasal symptom (bleeding, dryness, pain, scabbing, other) within each cohort. Further, for each patient who experienced treatment-emergent nasal vestibulitis, the worst (i.e., highest score) patient-reported rating was computed, and the proportion of patients reporting mild (score 1–3), moderate (score 4–7), and severe (score 8–10) were tabulated overall and within the different cohorts. Associations between severity and the cohorts were assessed using a χ2 test.
For secondary analyses, a cumulative incidence function was estimated within the cohorts in order to calculate the cumulative incidence rate (i.e., time to initial onset) of treatment-emergent nasal vestibulitis, treating death and disease progression as competing risks [5]. To assess the effect of therapy on the cumulative incidence function of treatment-emergent nasal vestibulitis in the presence of potential confounding variables, a cumulative incidence function regression model was also used for multiple regression analyses [6]. The covariates included in the regression model included age at baseline (years), smoking history (currently, in the past, never), allergy history (yes, no), and asthma history (yes, no).
The current report involves the patients entered on three cohorts of this study (paclitaxel, docetaxel, and non-taxane non-bevacizumab chemotherapy), as accrual on the other 2 cohorts has not yet been completed. No statistical adjustment was made for performing multiple tests. P values are two sided and reported as continuous values.
Results
Baseline characteristics
This study accrued 85 patients to the paclitaxel, docetaxel, and non-taxane non-bevacizumab cohorts. Non-taxane, non-bevacizumab chemotherapy regimens were varied and included combinations of agents, such as anthracyclines, platinums, and antimetabolites, Four patients (one in the paclitaxel cohort, one in the docetaxel cohort, and two in the other cohort) did not receive two or more chemotherapy treatments or did not complete two or more nasal symptoms surveys and therefore were deemed unevaluable for the primary endpoint of treatment-emergent nasal vestibulitis.
Few patients reported nasal symptoms at baseline (Table 1). Most patients (59.3%) completed the study once they ended their planned antineoplastic therapy; less frequently, patients stopped the study due to finishing 4 months of therapy (22.2%), toxicity of therapy (9.9%), disease progression (7.4%), or death (1.2%).
While the study was written to have the patients complete questionnaires, it was discovered that initial surveys were collected by a nurse asking patients about their symptoms. This affected the first 30 patients entered onto the protocol. Since most of the initial patients entered on the study were receiving paclitaxel, ten additional patients were recruited into the paclitaxel cohort. Fifty-five of the total patients reported in this manuscript completed paper surveys on their own; the results of the patients who completed surveys on their own were not substantially different from the results of the entire group.
Incidence of nasal vestibulitis
A higher percentage of patients who received paclitaxel experienced new, unpleasant nasal symptoms, compared with patients who received docetaxel or other chemotherapy agents. The percentage of patients (95% CI) with nasal symptoms, for patients receiving paclitaxel, docetaxel, and non-taxane chemotherapy, were 76.5% (58.8%, 89.3%), 54.2% (32.8%, 74.5%), and 47.8% (26.8%, 69.4%). Of the evaluable patients reported in this manuscript, 51 patients (62.9%) experienced nasal symptoms.
The cumulative incidence curves of treatment-emergent nasal vestibulitis for each of the three cohorts are shown in Fig. 1. The cumulative incidence at 1, 2, and 3 months, respectively, with death and disease progression considered competing risks was 52.9%, 70.6%, and 76.5% within the paclitaxel cohort, 29.2%, 45.8%, and 54.6% within the docetaxel cohort, and 30.4%, 39.5%, and 45.4% within the non-taxane chemotherapy cohorts. A three-sample test of equality of the cumulative incidence functions was statistically significant (P = 0.028). Of the three pairwise cohort comparisons, both the tests comparing the cumulative incidence function between the paclitaxel and non-taxane non-bevacizumab cohorts and between the paclitaxel and docetaxel cohorts achieved statistical significance at the nominal 5% level with a higher incidence of treatment-emergent nasal vestibulitis in the paclitaxel cohort in both comparisons (P = 0.026 and P = 0.035, respectively). These significant differences were retained in the cumulative incidence function multiple regression analysis controlling for age, smoking history, allergies, and asthma.
Descriptions of nasal vestibulitis
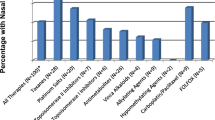
Patients frequently reported nasal dryness and epistaxis, as a part of nasal vestibulitis (Fig. 2). Many patients also reported “other” symptoms, most commonly, nasal drainage.
Moderate to severe symptoms were reported in 55.9% of the patients in the paclitaxel cohort, 45.8% of patients in the docetaxel cohort, and 21.7% of the patients who received non-taxane non-bevacizumab chemotherapy (overall P = 0.037; Fig. 3), with the only pairwise comparison achieving statistical significance at the nominal 5% level being the comparison between paclitaxel and non-taxane non-bevacizumab cohorts (P = 0.010).
When asked about what might be causing nasal symptoms, the majority of patients with symptoms (70.6%) thought this was due to chemotherapy. Only two patients reported potential concurrent infections; one thought the infection caused the nasal symptoms. Other patients were unsure (15.7%), or thought symptoms were related to dry air (7.8%) or allergies (3.9%). Many patients reported concurrent nasal hair loss (78.4%) and/or eye symptoms (72.5%).
Chart documentation of nasal vestibulitis
Sixteen patients (31.4% of the patients with nasal symptoms) had chart documentation of nasal symptoms. In 5 patients (31.3%), this was reported by a nurse practitioner or physician assistant, in 6 patients (37.5%), this was reported by a nurse, and in 3 patients (18.8%), this was reported by a physician; 2 patients had documentation by both a nurse and another provider (12.5%). Six patients had chart documentation of the provider recommending a treatment, including rose geranium in sesame oil nasal spray (50.0%), Ayr nasal gel (33.3%), and nasal saline (16.7%). One patient was referred for an otolaryngology consultation, due to epistaxis.
Discussion
In the current prospective natural history study, the higher incidence of nasal symptoms observed in the patients receiving paclitaxel chemotherapy, when compared with patients receiving non-taxane chemotherapy, is consistent with results from the prior retrospective study that led to the current project [2]. Although the sample size was relatively small, this finding provides some evidence that nasal vestibulitis is more prominent in patients receiving paclitaxel than other non-taxane non-bevacizumab chemotherapy agents. Given the similarities between the taxane agents, the trend for more nasal vestibulitis in the docetaxel-receiving patients was not surprising.
The relatively low rate of chart documentation of nasal symptoms (31%), in the patients that claimed that they had such on questionnaires, is especially noteworthy. While clinicians at the study sites were likely more aware of the symptom complex, due to the visibility of the clinical study, it is possible that the lack of reporting was due to a limited understanding of nasal vestibulitis. For instance, providers, unfamiliar with the prior study, might assume nasal symptoms are mild, or they might not know ways to improve nasal vestibulitis, both of which could contribute to poor documentation. This knowledge deficit might be improved through provider education about the severity and pervasiveness of nasal symptoms in patients receiving taxanes. Furthermore, the paucity of data collected by chart reviews, compared with questionnaires, underscores the continued importance of patient-reported outcome measures in improving the understanding of the side effects of cancer-directed therapies.
Interestingly, nasal symptoms were frequently reported by patients in all cohorts of this study, whereas only 41% of all of the patients in the prior retrospective study reported nasal symptoms [2]. This may be due to the prospective nature of this study: patients reported upon nasal symptoms frequently over time, rather than at a single time point, likely contributing to higher frequencies of reported symptoms. There is also a possibility that the patients enrolled in this prospective study were primed to report nasal symptoms that they might not otherwise have mentioned to their clinicians. However, the low reported frequency of mild symptoms, particularly reported in the paclitaxel cohort, and the similarity between reports of moderate to severe symptoms between this prospective and the prior retrospective study suggest that priming alone is unlikely to account for this finding. The high frequency of reported symptoms may be due to the higher proportions of patients in the paclitaxel arm in the current study, where nasal symptoms were the most frequent, when compared with the previous study [2].
Further study is needed to better understand the pathophysiology of nasal vestibulitis. While nasal vestibulitis symptoms might be secondary to overgrowth of colonizing nasal organisms, they do not appear to be associated with clinically significant infections [3, 4]. Furthermore, it is not clear why nasal vestibulitis is frequently reported among patients receiving paclitaxel, when compared with other chemotherapy agents, or whether these symptoms are related to dosing frequency. A majority of patients receiving paclitaxel in the current study reported nasal discharge; this was infrequently reported in two prior retrospective studies [1, 2] but might provide a better understanding of the pathophysiology of this symptom complex. In addition, many patients with nasal symptoms also reported loss of nasal hairs and eye symptoms; it is also possible that these symptoms are interrelated.
In total, this current work should make oncology providers more aware of nasal vestibulitis symptoms in patients receiving chemotherapy. Treatment options for managing this prominent issue should be investigated. Given retrospective evidence that suggests that rose geranium in sesame oil nasal spray may provide a benefit for patients with nasal vestibulitis [7], a randomized placebo-controlled clinical trial is currently ongoing to address this treatment approach (NCT 04620369).
Data availability
N/A.
References
Ruiz JN, Belum VR, Boers-Doets CB, Kamboj M, Babady NE, Tang YW, Valdez TA, Lacouture ME (2015) Nasal vestibulitis due to targeted therapies in cancer patients. Support Care Cancer 23(8):2391–2398
Cathcart-Rake E, Smith D, Zahrieh D, Jatoi A, Yang P, Loprinzi CL (2018) Nasal vestibulitis: an under-recognized and under-treated side effect of cancer treatment? Support Care Cancer 26(11):3909–3914
Wertheim HF, Melles DC, Vos MC, van Leeuwen W, van Belkum A, Verbrugh HA et al (2005) The role of nasal carriage in Staphylococcus aureus infections. Lancet Infect Dis 5(12):751–762
Haug RH (2012) Microorganisms of the nose and paranasal sinuses. Oral Maxillofac Surg Clin North Am 24(2):191–196 vii-viii
Gray RJ (1988) A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat 1988:1141–1154
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94(446):496–509
Cathcart-Rake EJ, Smith D, Zahrieh D, Loprinzi CL (2018) Rose geranium in sesame oil nasal spray: a treatment for nasal vestibulitis? BMJ Support Palliat Care
Acknowledgements
We would also like to acknowledge Eric Wolfe, who provided preliminary statistical support and mentorship of Shaylene McCue.
Code availability
N/A.
Funding
This work was supported by the Breast Cancer Research Foundation and by the Gateway for Cancer Research. Mario Lacouture is supported in part through the NIH/NCI Cancer Center Support Grant P30 CA008748.
Author information
Authors and Affiliations
Contributions
Study conception and design: ECR, CL, DS, ML
Acquisition of data: ECR, CL, SY, AO, TR, JP, ST, BF
Analysis and interpretation of data: ECR, DZ, SM, CL
Drafting of manuscript: ECR, CL, DZ
Critical revision: ECR, DZ, DS, SY, SM, AO, ST, ML, TR, JP, BF, CL
Corresponding author
Ethics declarations
Ethics approval
This work was approved by the Mayo Clinic Institutional Review Board.
Consent to participate
All patients consented to participate in this study, consistent with international ethical guidelines.
Consent for publication
All authors consent to the publication of this manuscript.
Conflict of interest
Dr. Lacouture and Dr. Loprinzi have disclosures that are outside of the present work. The remaining authors do not have any disclosures. Please see disclosure statements for details.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cathcart-Rake, E.J., Zahrieh, D., Smith, D. et al. Natural history of nasal vestibulitis associated with paclitaxel, docetaxel, and other chemotherapy agents: a Minnesota Cancer Clinical Trials Network (MNCCTN) study. Support Care Cancer 29, 6253–6258 (2021). https://doi.org/10.1007/s00520-021-06190-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06190-0