Abstract
Purpose
Patient-perceived quality of care has become an increasingly important index within the healthcare setting. We examined patient-reported overall quality of care and patient experiences in three specific domains of care (physician communication, nursing care, and care coordination) in a sample of Chinese patients with advanced cancer.
Methods
A cross-sectional study was conducted with stage IV cancer patients (N = 202) who were recruited from a public, tertiary hospital in Beijing. Study participants completed surveys administered by a research assistant. Multivariable regression analysis was conducted to examine the extent to which patient demographic factors (age, gender, socioeconomic status), disease/treatment factors, and domain-specific care were associated with overall quality of care.
Results
A majority of patients reported overall quality of care scores that we were either excellent (23%) or very good (41%). Patients reported highest ratings in the domain of nursing care (M = 87.57, SD = 31.05), followed by physician communication (M = 68.93, SD = 32.30), and care coordination (M = 66.79, SD = 25.17). Better perceived physician communication (b = 0.17, p < 0.01), care coordination (b = 0.26, p < 0.01), and higher socioeconomic status (b = 11.30, p < 0.05) were associated with higher overall quality of care.
Conclusions
A majority of patients with advanced cancer in this Chinese hospital reported positive overall quality of care. Physician communication and care coordination are potential areas to focus on to improve patient-reported overall quality of care. Understanding perceptions of care quality will allow opportunities to improve delivery of healthcare.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Individuals with a terminal diagnosis of cancer are a vulnerable group of patients in the healthcare system as they receive news about limited prognosis, confront mortality, discuss end-of-life care options, and receive treatment for symptoms [1, 2]. The quality of care for terminal illness in China has been reported to be poor as compared with other countries, as China scored below average in terms of palliative healthcare environment, human resource, affordability of care, community engagement, and quality of nursing care [3]. This study did not, however, consider patients’ perspectives on their quality of care, which is crucial to improving care delivery for patients with advanced cancer. Such data will be potentially important to government led initiatives for improving the levels of oncology palliative care in China [4, 5].
Quality of care is assessed through a wide range of indicators from different perspectives such as healthcare providers, regulators, and care recipients [6, 7]. Although healthcare institutions may vary in their use of quality of care indicators, patient-perceived overall quality of care as well as their experiences in specific care domains (e.g., communication with healthcare providers, coordination of care) are consistently important indices to consider [8,9,10,11]. In China, there is increasing awareness of the importance of measuring quality of care [12, 13]; most prior studies have focused on measuring patient satisfaction, which is a related but distinct concept [14,15,16]. There is particular paucity of studies that examined perceived quality of care in patients with terminal illness such as advanced cancer.
There is a need to directly survey patients with advanced cancer on their perception of overall quality of care and experience in specific care domains. Experiences of care refer to patient observations as they interact with the healthcare system, such as having easy access to information and feeling like they are treated as a unique individual and respected [17, 18]. In this study, experiences of care that we focus on are the domains of physician communication, nursing care, and care coordination (e.g., waiting time to receiving treatment, efficiency of referral systems, coordination among medical team members) [10, 19]. Experiences of patients with healthcare providers and the healthcare system have been reported to be associated with perceived quality of care [20,21,22].
The primary aim of this study is to investigate patient-reported overall quality of care and experiences in three specific domains of care—physician communication, nursing care, and care coordination—in a sample of Chinese patients with advanced cancer. We hypothesized that the majority of patients would report perceived overall quality of care and the experiences in the three specific domains of care to be above the midpoint (neutral) response category. As a secondary aim, we explored potential determinants of overall quality of care: demographic factors, disease/treatment factors, and experiences in specific domains of care. Identifying factors associated with experiences of care will allow opportunities and means to improve the delivery of healthcare to this group of patients.
Methods
Design, sampling, and recruitment
This study is part of a multicountry effort titled “Asian Patient Perspectives Regarding Oncology Awareness, Care and Health (APPROACH)” to assess gaps in care received by patients with advanced cancer seeking care at major public hospitals in low- and middle-income countries in Asia [23]. The present study recruited patients aged 21 years or older, had a diagnosis of a stage IV solid tumor cancer, were aware of their cancer diagnosis, had received anticancer treatment prior to the interview, were citizens of China, and were able to speak and understand Mandarin Chinese. The one-time, cross-sectional study was conducted at outpatient clinics and inpatient wards of a class A tertiary hospital in Beijing, China.
We contacted senior physicians of various departments treating patients with advanced cancer, including medical oncology, radiology, surgery, gynecology, respiratory medicine, geriatrics, and the international medical department. These departments collectively receive about 400 new advanced-stage cancer patients per month. Between June 2016 and January 2017, 260 patients were referred to the study by participating departments. The patients were approached by trained research assistants and 202 patients were invited to participate. Fifty-eight patients were excluded for not having the right cancer staging, being unaware of their cancer diagnosis, being too weak to participate, or being cognitively impaired as assessed by the referring healthcare provider and/or the study coordinator. Written informed consent was obtained from all participants prior to their participation in the study, which entailed completing surveys with the assistance of a research assistant as necessary (i.e., to read the questions aloud to the study participant). The study was approved by the Ethics Review Boards of the, Chinese Academy of Medical Sciences (reference S-I 173) and the National University of Singapore (NUS 2883/B-15-319).
Measures
The survey was first designed by the study investigators in English as part of the APPROACH study initiated by the Lien Centre for Palliative Care in Singapore [23]. The survey was professionally translated into Mandarin and back-translated into English. Differences were reconciled and the resulting survey instrument was used in cognitive interviews with 10 patients. Based on feedback from the cognitive interviews and from the first author, further revisions were made before the survey was administered to the study sample.
Demographic variables
Sociodemographic characteristics such as age, gender, marital status, and number of education years were captured. Socioeconomic status (SES) was assessed using the item: “How would you rate the economic status of your household?”. We classified the response “Poor” as low SES, “Lower middle class” as middle SES, and “Upper middle class” and “Wealthy” as high SES in this study.
Disease/treatment factors
We measured patients’ perceived disease severity with one item: “Do you know the current stage (i.e. severity) of your cancer?”. Response choices were “Early stage (stage I, II, or III)”, “Advanced Stage (Stage IV)”, or “I don’t know”. Patient symptom burden was calculated by averaging the severity of symptoms reported in a checklist of ten common symptoms (pain, breathlessness, etc.) found in the FACIT-Palliative scale [24]. Treatment setting was coded as inpatient or outpatient.
Overall quality of care
One item was used to measure patient-perceived overall quality of care: “Overall how would you rate the quality of your healthcare since diagnosis?” based on the CANCORS study [10, 19]. Patients responded on a 5-point scale with the categories “excellent,” “very good,” “good,” “fair,” and “poor.” Higher scores indicate greater perceived overall quality of care.
Experiences of care
Three domains of care were examined based on questions used in the CANCORS project [10, 19]: physician communication (5 items; example item, “How often did your doctors explain things in a way you could understand?”), nursing care (2 items; example item, “How often did your nurses treat you with courtesy and respect?”), and care coordination (6 items; example item, “How often did the doctors, nurses, and other medical staff providing your care seem to work well together as a team?”). The authors had adapted the 13 items from the Consumer Assessment of Healthcare Providers and Systems core survey [25] and their prior research [11, 26]. Response options for the items were “always,” “sometimes” or “never,” and for some items, “not applicable.” Each domain was converted into a 100-point scale, with 0 representing worst possible quality of care and 100 representing optimal quality of care. In the current study, domain scores showed good internal reliability (α = 0.69 for physician communication, α = 0.91 for nursing care, and α = 0.77 for care coordination).
Data analysis plan
Descriptive statistics on the sample’s sociodemographic and clinical characteristics and study variables of interest were tabulated. Multivariable regression analysis was conducted to examine the extent to which patient demographic factors (age, gender, SES), disease/treatment factors (awareness of diagnosis, symptom burden, treatment setting), and specific experiences of care domains (physician communication, nursing care, and care coordination) were associated with overall quality of care; the selection of these variables was informed by prior literature [10, 11]. Overall quality of care scores was converted to a 100-point scale to ease interpretation of associations with the experience of care domains. All categorical variables were dummy-coded prior to being entered into the model. Statistical significance was set at p < 0.05 and when the confidence interval does not include the value 0. Analyses were conducted using the Statistical Package for the Social Sciences version 25 [27]. Post hoc power analyses indicated that our regression model had over 90% power given the sample size, number of variables, statistical significance level (α = 0.05), and proportion of variance explained (R2 = 0.32).
Results
A total of 202 patients consented to participation and completed the surveys. Based on the assessment of patients’ mental competence and overall comprehension of survey items (captured via a set of seven items filled by the research assistant at the end of the interview), 18 patients were excluded from analysis.
Patient characteristics
The sample of 184 advanced solid cancer patients ranged from 20 to 87 years of age (M = 58 years, SD = 13.71). Of the 184 participants, 53% were male, 88% were married, and 86% declared no religion. They reported an average of 12 years (SD = 3.81 years) of education, which is equivalent to completion of high school/secondary education. Approximately 50% of participants rated their households as high SES. Gastrointestinal (35%) and respiratory (28%) cancers were most common diagnoses. Table 1 presents detailed sociodemographic characteristics of the sample.
Descriptive findings on patient-reported overall quality of care and experiences of care
The majority of patients reported overall quality of care scores above the midpoint response category: 23% of the sample reported “excellent” and 41% of the sample reported “very good.” The average reported score was 3.80 (SD = 0.92), which corresponds approximately to “very good.” For the specific experiences of care domains, a plurality of patients reported the highest response category for all items in the care domains measured. Patients reported ratings that were highest in the domain of nursing care (M = 87.57, SD = 31.05), followed by physician communication (M = 68.93, SD = 32.30), and care coordination (M = 66.79, SD = 25.17).
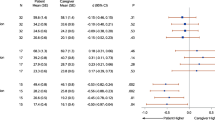
Factors associated with overall quality of care
Table 2 presents results from the multivariable regression examining factors associated with overall quality of care. Better perceived physician communication (b = 0.17, CI = 0.05–0.29), care coordination (b = 0.26, CI = 0.10–0.41), and higher socioeconomic status (b = 11.30, CI = 0.36–22.25) were associated with increased overall quality of care. The total variance explained by the model (R2) was 32%.
Discussion
The current study investigated patient-reported overall quality of care and experiences in care in a sample of Chinese patients with advanced cancer. The majority of patients with advanced cancer in our study reported “very good” and “excellent” quality of care, with the average score being equivalent to “very good.” Our findings are generally consistent with a previous study of 136 hospitals across China where quality of healthcare was generally rated to be high [28]. Subsequently, patients reported highest ratings of patient experiences in the domain of nursing care, followed by physician communication, and care coordination. This is consistent with the findings reported previously in a sample of advanced lung and colorectal cancer patients in the USA [10].
In exploring potential correlates of overall quality of care, we found that better perceived physician communication, better perceived care coordination, and higher socioeconomic status were associated with increased overall quality of care. This is largely congruent with previous reports of patient experiences with physicians [21, 22] and care coordination (i.e., waiting time) [20] being important determinants of overall quality of care. We did not find an association between nursing care and overall quality of care as a previous study with hospitalized patients has found [29]. Although the majority of our sample was inpatient, one-third was outpatient, where nursing care may not be as relevant and as important an aspect of perceived overall quality of care.
Patients rated the experiences of care in the domains of physician communication and care coordination to be lower than the domain of nursing care. These same domains were found to be more important correlates of overall quality of care compared with nursing care. This finding highlights not only what patients think of the services received but also what they consider important when they seek and receive care: good communication experiences with their physicians and having a smooth experience of care coordination. Anecdotally from the clinic, poorer perceived quality of care can stem from miscommunication between patients or their family with the healthcare team, such as not understanding or misunderstanding important medical information given (e.g., treatment options or patient prognosis). Patients and families are also likely to complain about quality of care when they are frustrated with care coordination, such as getting timely appointments and cohesiveness/sharing of information within the healthcare team.
Given our findings, physician communication and care coordination domains are modifiable factors that may be targeted as quality improvement endeavors initiated at an institutional or higher level. For instance, one strategy could be the intentional training of physicians to be comfortable in healthcare-related communication, especially pertaining to delicate matters such as breaking news about terminal disease diagnosis and limited prognosis and discussing end-of-life treatment options [30,31,32]. Staff training to improve customer service experiences and implementation of system-level protocols to smoothen healthcare logistics (e.g., effort to consolidate multiple appointments to reduce frequency of hospital visits) can also be minor, but meaningful modifications that can have potential significant impact on patient experiences [33, 34]. In many countries, surveys of patient-perceived quality of care are becoming mandatory in the hospital setting as a quality improvement tool, as healthcare regulators shift toward a patient-centered approach [35,36,37].
There are several limitations of the study to be acknowledged. The study design was cross-sectional, and as such did not allow drawing of causal conclusions. We also recruited only from one site in Beijing China, so the results may not be generalizable to other hospitals and regions in the country. The SES variable that we used was one that was self-determined by participants, and thus our findings should be interpreted with caution. Nevertheless, this paper provides a first step in examining the perceptions on advanced Chinese cancer patients that we hope will allow means to improve delivery of healthcare to this group of patients. Future studies can build upon this preliminary work to further research in this area.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request. The corresponding author has full control of the primary data and agrees to the journal to reviewing the data if requested.
References
Mitchell AJ, Chan M, Bhatti H, Halton M, Grassi L, Johansen C, Meader N (2011) Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol 12(2):160–174
Kolva E, Rosenfeld B, Pessin H, Breitbart W, Brescia R (2011) Anxiety in terminally ill cancer patients. J Pain Symptom Manag 42(5):691–701
Economist Intelligence Unit (2015) The 2015 Quality of Death Index: ranking palliative care across the world
The National Health and Family Planning Commission (2017) The basic standards, management practices and practice guidelines for hospice care in the hospice care center. http://www.nhc.gov.cn/yzygj/s3593/201702/c8f7e7bb2c6943a384cfd2a42ffcf686.shtml. Accessed 15 Dec 2019
National Health Committee (2019)
Chassin MR (1998) Is health care ready for six sigma quality? Milbank Q 76(4):565–591
Mainz J (2003) Defining and classifying clinical indicators for quality improvement. Int J Qual Health Care 15(6):523–530
Cleary PD (2016) Evolving concepts of patient-centered care and the assessment of patient care experiences: optimism and opposition. J Health Polit Policy Law 41(4):675–696
Darby C (2005) Measuring the patient’s perspective on the interpersonal aspects of cancer care. Outcomes Assess Cancer: Measures, Methods, and Applications 290–304
Ayanian JZ, Zaslavsky AM, Arora NK, Kahn KL, Malin JL, Ganz PA, Van Ryn M, Hornbrook MC, Kiefe CI, He Y (2010) Patients’ experiences with care for lung cancer and colorectal cancer: findings from the cancer care outcomes research and surveillance consortium. J Clin Oncol 28(27):4154–4161
Ayanian JZ, Zaslavsky AM, Guadagnoli E, Fuchs CS, Yost KJ, Creech CM, Cress RD, O'Connor LC, West DW, Wright WE (2005) Patients’ perceptions of quality of care for colorectal cancer by race, ethnicity, and language. J Clin Oncol 23(27):6576–6586
Wang X, Su S, Li S, Bao H, Zhang M, Liu D, Jiang H, Wang J, Liu M (2017) Development of quality indicators for non-small cell lung cancer care: a first step toward assessing and improving quality of cancer care in China. BMC Cancer 17(1):603
Lin C, Cohen E, Livingston PM, Mohebbi M, Botti M (2019) Achievement of patients’ preferences for participation in oncological symptom management and its association with perceived quality of care. Patient Prefer Adherence 13:83
Zhang C, Chen B, Ly J (2017) Research on patient satisfaction in top tertiary public hospitals in Shanghai. Chinese Hospitals 21(9):33–35
You LM, Aiken LH, Sloane DM, Liu K, He GP, Hu Y, Jiang XL, Li XH, Li XM, Liu HP (2013) Hospital nursing, care quality, and patient satisfaction: cross-sectional surveys of nurses and patients in hospitals in China and Europe. Int J Nurs Stud 50(2):154–161
Liu Y, Wang G (2007) Inpatient satisfaction with nursing care and factors influencing satisfaction in a teaching hospital in China. J Nurs Care Qual 22(3):266–271
Bull C, Byrnes J, Hettiarachchi R, Downes M (2019) Reliability and validity of patient-reported experiences measures: a systematic review
Quality AfHRa (2017) What is patient experience? https://www.ahrq.gov/cahps/about-cahps/patient-experience/index.html. Accessed April 1, 2020
Malin JL, Ko C, Ayanian JZ, Harrington D, Nerenz DR, Kahn KL, Ganther-Urmie J, Catalano PJ, Zaslavsky AM, Wallace RB (2006) Understanding cancer patients’ experience and outcomes: development and pilot study of the cancer care outcomes research and surveillance patient survey. Support Care Cancer 14(8):837–848
Nottingham QJ, Johnson DM, Russell RS (2018) The effect of waiting time on patient perceptions of care quality. Qual Manag J 25(1):32–45
Weaver KE, Aziz NM, Arora NK, Forsythe LP, Hamilton AS, Oakley-Girvan I, Keel G, Bellizzi KM, Rowland JH (2014) Follow-up care experiences and perceived quality of care among long-term survivors of breast, prostate, colorectal, and gynecologic cancers. J Oncol Pract 10(4):e231–e239. https://doi.org/10.1200/jop.2013.001175
Leung JM, Udris EM, Uman J, Au DH (2012) The effect of end-of-life discussions on perceived quality of care and health status among patients with COPD. Chest 142(1):128–133. https://doi.org/10.1378/chest.11-2222
Jacob J, Palat G, Verghese N, Chandran P, Rapelli V, Kumari S, Malhotra C, Teo I, Finkelstein E, Ozdemir S (2019) Health-related quality of life and its socio-economic and cultural predictors among advanced cancer patients: evidence from the APPROACH cross-sectional survey in Hyderabad-India. BMC Palliat Care 18(1):94
Lyons KD, Bakitas M, Hegel MT, Hanscom B, Hull J, Ahles TA (2009) Reliability and validity of the functional assessment of chronic illness therapy-palliative care (FACIT-pal) scale. J Pain Symptom Manag 37(1):23–32
Hays RD, Shaul JA, Williams VS, Lubalin JS, Harris-Kojetin LD, Sweeny SF, Cleary PD (1999) Psychometric properties of the CAHPS™ 1.0 survey measures. Med Care 37:MS22–MS31
Arora NK, Weaver KE, Clayman ML, Oakley-Girvan I, Potosky AL (2009) Physicians’ decision-making style and psychosocial outcomes among cancer survivors. Patient Educ Couns 77(3):404–412
Nie NH, Bent DH, Hull CH (1975) SPSS: statistical package for the social sciences, vol 227. McGraw-Hill, New York
Hu L, Ding H, Hu G, Wang Z, Liu S, Liu Y (2019) How perceived quality of care affects outpatient satisfaction in China: a cross-sectional study of 136 tertiary hospitals. Inquiry 56:0046958019895397
Otani K, Waterman B, Faulkner KM, Boslaugh S, Dunagan WC (2010) How patient reactions to hospital care attributes affect the evaluation of overall quality of care, willingness to recommend, and willingness to return. J Healthc Manag 55(1):25–38
Back AL, Arnold RM, Baile WF, Fryer-Edwards KA, Alexander SC, Barley GE, Gooley TA, Tulsky JA (2007) Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med 167(5):453–460
Hoerger M, Epstein RM, Winters PC, Fiscella K, Duberstein PR, Gramling R, Butow PN, Mohile SG, Kaesberg PR, Tang W (2013) Values and options in cancer care (VOICE): study design and rationale for a patient-centered communication and decision-making intervention for physicians, patients with advanced cancer, and their caregivers. BMC Cancer 13(1):188
Detmar SB, Muller MJ, Wever LD, Schornagel JH, Aaronson NK (2001) Patient-physician communication during outpatient palliative treatment visits: an observational study. Jama 285(10):1351–1357
Wentlandt K, Krzyzanowska MK, Swami N, Rodin GM, Le LW, Zimmermann C (2012) Referral practices of oncologists to specialized palliative care. J Clin Oncol 30(35):4380–4386
Morita T, Miyashita M, Yamagishi A, Akizuki N, Kizawa Y, Shirahige Y, Akiyama M, Hirai K, Matoba M, Yamada M (2012) A region-based palliative care intervention trial using the mixed-method approach: Japan OPTIM study. BMC Palliat Care 11(1):2
Darby C, Crofton C, Clancy CM (2006) Consumer assessment of health providers and systems (CAHPS): evolving to meet stakeholder needs. Am J Med Qual 21(2):144–147
Zucca A, Sanson-Fisher R, Waller A, Carey M, Boadle D (2017) The first step in ensuring patient-centred quality of care: ask the patient. Eur J Cancer Care 26(1):e12435
Luxford K, Piper D, Dunbar N, Poole N (2010) Patient-centred care: improving quality and safety by focusing care on patients and consumers
Acknowledgments
A sincere thank you to the volunteers from Beijing Ren Ai Charity Foundation and the 48 doctors from Gynecology, Surgery, Emergency and other departments of PUMCH for their enduring support.
Funding
This study was funded by the Lien Centre for Palliative Care.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(20 kb).
Rights and permissions
About this article
Cite this article
Ning, X., Krishnan, A., Li, X. et al. Perceived quality of care and its associated factors among Chinese patients with advanced cancer: findings from the APPROACH study in Beijing. Support Care Cancer 29, 1395–1401 (2021). https://doi.org/10.1007/s00520-020-05559-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05559-x