Abstract
Objectives
Postoperative shoulder joint dysfunction has been observed at a certain rate after breast cancer surgery with axillary lymph node dissection. The purposes of this study were to verify the feasibility and effects of home-based exercise using a DVD and clarify the target of intensive intervention with physiotherapy by identifying the factors that cause postoperative shoulder dysfunction.
Methods
The study comprised 237 female patients who underwent breast cancer surgery with axillary lymph node dissection, whose data were acquired until 3 months postoperatively. All patients were instructed to exercise at home using a DVD. Range of motion (ROM) of shoulder flexion and abduction and the disability of the arm, shoulder, and hand (DASH) score were measured before surgery, 1 week and 1, 2, and 3 months after surgery. As factors influencing the recovery of shoulder ROM at 3 months after surgery, the presence or absence of radiation and factors up to 1 month after surgery (age, body mass index, the relationship between operated side and dominant side of the hand, treatment modalities, and complications).
Results
Shoulder ROM and DASH scores had gradually recovered from 1 week to 3 months postoperatively. As the results of the multivariate analysis, the factors that were associated with the recovery of ROM of shoulder flexion at 3 months were the side of surgery corresponding to the dominant hand (negative factor) and the presence of paresthesia at 1 week postoperatively (positive factor) (p < 0.05). Radiation therapy and the side of surgery corresponding to the dominant hand were negative factors for the recovery of shoulder abduction (p < 0.01). Regarding the feasibility of the home exercise, 214/229 (93.4%), 172/210 (81.9%), and 139/206 (67.5%) of patients performed exercise at least once a day at 1, 2, and 3 months after surgery, respectively.
Conclusion
Our result indicated that the side of surgery corresponding to the dominant hand was the inhibiting factor for recovery for both shoulder flexion and abduction at 3 months after surgery. Home-based exercise with DVD was considered feasible. For the verification of this effectiveness, a randomized control study should be planned in the future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer has a high prevalence rate in women in Japan. Advances in medicine and technology have led to earlier detection and better treatment options of breast cancer, resulting in higher survival rates. Breast cancer surgery might result in upper extremity impairments, functional limitations, and disabilities such as pain, stiffness, lymphedema, cording, decreased strength and range of motion (ROM), and decreased activity tolerance [1,2,3,4]. While survivors have increased in numbers, these complications have been frequently observed following breast cancer treatment [5,6].
To improve postoperative shoulder joint dysfunction, several physical therapy interventions have been conducted, and some certain effects such as an early improvement in ROM at a relatively short-term observation have been reported [7,8,9,10,11]. Although there were some differences in the rate of upper limb dysfunction according to previous reports, a certain rate of patients who had some upper limb dysfunction after surgery even with those interventions of physiotherapy existed. Yang et al. reported a prevalence rate of 26.8% of upper limb dysfunction in patients at 1 year after breast cancer surgery [12].
ROM limitation of the operated side becomes a restriction in activities of daily living (ADL) such as dressing and grooming; thus, there is a possibility that it may negatively affect the quality of life (QOL) [13]. Therefore, it follows to evaluate the benefits of intervention methods by clarifying factors affecting postoperative ROM and upper limb function. Although chemotherapy, body mass index (BMI), mastectomy, and many others have been reported as factors influencing postoperative ROM [13,14,15], examining these factors that influence postoperative ROM remains unclear.
This study aimed to prospectively verify the feasibility and effects of home-based exercise using a DVD on postoperative ROM and clarify factors that might cause postoperative shoulder dysfunction.
Materials and methods
Patients
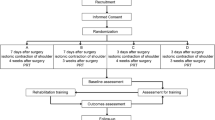
Out of the patients with breast cancer who underwent mastectomy with lymph node dissection at our institution from November 2013 to December 2016, 237 patients were referred to the Department of Rehabilitation Medicine and whose investigated parameters for 3 months were available. Preoperative data of 14 cases were unavailable. The patients’ demographic data (N = 223) are shown in Table 1. Among them, 145 patients, whose preoperative flexion and abduction were more than 140 degrees and less than 90% recovery at 1 week after surgery and whose data were available preoperatively and until 3 months postoperatively, were selected for statistical analyses (Fig. 1).
Data collection and measurements
Shoulder joint ROM (flexion and abduction) was measured using a goniometer (the University of Tokyo type) by one skilled occupational therapist (OT) or one skilled physical therapist (PT) preoperatively and at 1 week and 1, 2, and 3 months postoperatively. The reliability of measurements was checked separately by measuring the parameters three times each on 11 healthy subjects. Intra- and inter-class correlation coefficient (ICC) and standard errors of measurement (SEM) were calculated. The intra-rater reliability with ICC values and SEM of each therapist were ICC: 0.863 (95%CI: 0.647–0.957), SEM: 2.06 and ICC: 0.934 (95%CI: 0.829–0.980), SEM: 2.80 for flexion and ICC: 0.900 (95%CI: 0.752–0.969), SEM: 1.61 and ICC: 0.945 (95%CI: 0.857–0.987), SEM: 1.86 for abduction; the inter-rater reliability with ICC values and SEM were ICC: 0.732, SEM: 4.10 for flexion and ICC: 0.824, SEM: 2.83 for abduction. The 3-month postoperative shoulder joint flexion and abduction were classified into two groups: recovered by over 90% and less than 90% compared with preoperative values. At the same time, as a secondary endpoint, upper limb function was investigated using disability of the arm, shoulder, and hand (DASH) score (the Japanese Society for Surgery of Hand version of DASH questionnaire which was validated in the Japanese patients with upper extremity disorders) [16]. DASH questionnaire (disability/symptom module) includes 30 items consisting of 23 questions on disorders of daily activities using upper limbs and seven questions on symptoms. DASH score ranged between 0 and 100, and higher scores indicated that there were signs of upper limb disorder [17].
As factors influencing the recovery of shoulder ROM, age (under 60 years or over 60 years), BMI (less than 25 or more than 25), surgical site (dominant hand or non-dominant hand), level of the lymph node dissection (level 1 or level 2 and higher), resection of the pectoralis minor muscle (yes or no), preoperative chemotherapy (yes or no), postoperative chemotherapy (yes or no), postoperative hormonal therapy (yes or no), postoperative radiotherapy (yes or no), presence/absence of pain, paresthesia, seroma, wound complications, and soft tissue tightness of the upper limbs or axilla were measured and investigated. The presence or absence of pain and paresthesia was examined at 1 week and 1, 2, and 3 months postoperatively. The presence or absence of seroma wound complications and soft tissue tightness of the upper limbs or axilla was investigated 1 month postoperatively.
Rehabilitation program
As part of the preoperative rehabilitation during hospitalization, guidance was given for upper limbs exercise using a DVD in which an instructor demonstrated how to move the upper limbs properly. The contents of exercise on the DVD were as follows. The exercise lasted for about 15 min and was composed of seven movements. The instructions were as follows: tighten the fist and open the hand repeatedly in a standing position, turn one or both arms slowly in a circle motion around the shoulder joint without raising the arm, and move the shoulder up and down while being aware of the scapula movement. The shoulder exercises were repeated. Thereafter, the “climbing up the wall” exercise was performed. This was performed by standing against the wall, placing the palm on the wall with the elbow joint flexed naturally, and gradually raising the arm to reach the fingers as high as possible up the wall while being aware of pain. If pain worsened, the instructor told the participants to stop, rest for a while, and start over again. The participants repeated this exercise while standing sideways against the wall. The next exercise involved movement of latching a necklace behind the neck, followed by the movement of latching a bra behind the back. Finally, shoulder joint flexion and abduction were performed gently, alternating the arms.
Postoperative rehabilitation was started at the first and second postoperative days with exercising distal to the elbow joint. From the third postoperative day to the day of drain withdrawal, the upper limb ROM exercise was performed within 90 degrees of the shoulder joint flexion and abduction. After drain removal, the shoulder ROM was not restricted, and the upper limbs and ADL exercises were adjusted according to the degree of pain. On holidays when there was no regular physiotherapy, nurses played the upper limb exercise DVD on the large monitor located at the ward corridor and carried out upper limb exercises together with the patients under the guidance of nurses. During the period of rehabilitation and at the day of discharge, guidance was given by PT, OT, or nurses on how to deal with adverse events such as axillary web syndrome, seroma, surgical site infection, general fatigue, and prevention of lymphedema. Patients were also instructed to perform the exercise at home using a DVD at least once a day after discharge. If they had not enough time to perform the full version of the DVD contents, we recommended the parts of the exercise of the axilla extension, as much as possible. These movements were presumably considered effective to prevent soft tissue contracture; soft tissue contracture around the axilla, where the surgical incision was made, would occur after axillary lymph node dissection. Moreover, after surgery, even if pain or paresthesia occurred, the patients were encouraged to continue the exercise within the tolerance of symptoms. The report of implementation status of self-exercise using a DVD at home (a home exercise diary) was requested to describe, in the schedule table, the number of repeat times, the duration time of the whole exercise, and the number of times the DVD was played. The validity of the home exercise diary as a tool for adherence to reflect exercise participation during home-based rehabilitation has been reported [18]. At the first, second, and third months after surgery, OT and PT checked out the exercise implementation status of the patients and evaluated their upper limb function at the out-patient clinic. According to the condition, the patients were given guidance on ADL, exercise, and the chance of consultation for adverse events such as lymphedema.
Statistical analysis
Studies on the factors affecting the recovery of ROM at 3 months after surgery were conducted in patients whose shoulder ROM was recovered to less than 90% of the preoperative values 1 week postoperatively. Logistic analysis was carried out to examine the effective associated factors on more than 90% recovery of the shoulder ROM (flexion/abduction). Univariate analysis was performed to examine the influence of the factors (age, BMI, dominant hand/tumor laterality relationship, factors related to therapy, and factors related to postoperative symptoms) on the shoulder ROM recovery and summarized by odds ratio. We used a multiple logistic regression with selected predictors by the stepwise procedure from factors measured within 1 month (except for RT) (p < 0.05). Factors with a p value of less than 0.1 in univariate analysis were selected for multivariate analysis. Stata version 14.0 (Stata Corp LP, College Station, TX, USA) was used as the statistical analysis software.
Results
The implementation status of home exercise was investigated in the patients excluding missing values. At 1, 2, and 3 months after surgery, 214/229 (93.4%), 172/210 (81.9%), and 139/206 (67.5%) of the patients performed exercise at least once a day, respectively. The median of the implementation time (min-max) was 20 min (0–180 min), 10 min (0–150 min), and 10 min (0–50 min), respectively. The median number of DVD viewings per day (min-max) was 1 (0–10), 0 (0–10), and 0 (0–3), respectively. The proportion of patients who exercised using the DVD was 56.3%, 26.7%, and 18.4%, respectively at each month.
The time course curves of shoulder ROM (flexion/abduction) from before surgery to 3 months after surgery show the tendency to gradually improve until 3 months after surgery; ROM decreased the most at 1 week postoperatively. In the abduction ROM, variations in recovery were large and individual differences were recognized compared with flexion ROM at 1 week and 1 month after surgery (Fig. 2). Three months after surgery, the proportion that ROM was not recovered by 90% in flexion and abduction was 17.0% and 19.3% respectively.
The postoperative course of the DASH score showed a recovery trend similar to ROM (Fig. 3). In the DASH score, the rate of patients who did not recover to more than 90% of the preoperative level at 3 months was 30.0%.
The results of the univariate analysis are shown in Fig. 4. In shoulder flexion, the recovery was worse (p < 0.05) with the presence of pain (3 months postoperatively) and better with the presence of paresthesia at 3 months. In shoulder abduction, the recovery was worse (p < 0.05) when surgery was performed on the side of the dominant hand, the lymph node dissection level was ≥ 2, the pectoralis minor muscle was excised, preoperative chemotherapy was administered, the patient underwent radiotherapy, the patient experienced pain (1, 2, and 3 months postoperatively), or no postoperative chemotherapy was administered.
Based on the results of the univariate analysis, multiple logistic regression analysis was performed using the candidate factors measured within 1 month (except for RT) for flexion: the side of surgery, postoperative chemotherapy, paresthesia (1 week postoperatively), and seroma (1 month postoperatively) and for abduction: the side of surgery, lymph node dissection level, the pectoralis minor muscle excision, preoperative chemotherapy, radiotherapy, and pain (1 month postoperatively), and postoperative chemotherapy. The results of multiple logistic regression analyses are shown in Table 2. Recovery was negatively associated with surgery being performed on the side of the dominant hand and was positively associated with the presence of paresthesia (1 week postoperatively) (p < 0.05). Recovery of abduction ROM in the shoulder at 3 months was negatively associated with surgery being performed on the side of the dominant hand and the presence of radiotherapy (p < 0.05).
Discussion
Concerning the implementation status of home exercise, the number of implementations, the implementation time, and number of DVD viewings over time tended to decrease. Although we did not investigate the correlation between the improvement in the shoulder function and the implementation status, one of the causes was thought to be the loss of motivation in exercising over time, as the shoulder joint function improved. Regarding the number of times the DVD was viewed, it was thought that those patients would exercise without using the DVD because the content was memorized by repeatedly watching. Petito et al. reported that the implementation rates of home exercise were 84.4%, 72.7%, and 47.1%, respectively at 14, 75, and 105 days postoperatively [19]. They also observed the implementation rate diminishing with the gradual improvement in shoulder ROM and concluded that their home exercise program was feasible and effective. Considering the rate of implementation at 3 months postoperatively in our program was about 70%, there was no problem with our home exercise program using a DVD, regarding to its feasibility.
Observational studies have reported that the incidence of deterioration of shoulder ROM at 1 year postoperatively ranges from 20 to 31% [1, 7, 20, 21]. In this study, we observed a proportion of patients whose recovery of shoulder ROM was limited 3 months after surgery (flexion and abduction: 17.0% and 19.3% respectively). Although we could not compare this proportion with those of other studies because of the difference in follow-up periods, the proportion of the patients with impaired shoulder ROM at 3 months in our study were seemingly acceptable.
Kilgour et al. reported a preliminary study on a group (n = 16) that performed home-based exercise using home exercise video and a group (n = 11) that conducted verbal instructions using ordinary brochure [10]. Although it was a short-term study, the evaluation was conducted at 2 weeks postoperatively and good results were reported. The effectiveness of home exercise using a DVD needs to be furtherly clarified through a randomized control trial.
Regarding the influence of the relationship between the hand dominance and the operated side, previous studies have reported similar results at the final observations. Levy et al. reported the side of involvement was a significant factor for abduction ROM impairment at 1 month when the involved side was contralateral to hand dominance (p ≤ 0.04) [15]. But they mentioned that later assessment (> 12 months after surgery) revealed reduced recovery of function when the dominant limb was the affected side. Additionally, Dantas de Oliveira et al. reported the same result (p = 0.05) in their cross-sectional study of 869 cases [13]. In our study, the side of surgery corresponding to the dominant hand negatively affected shoulder ROM (flexion and abduction) recovery at 3 months. Considering the possible cause of these results, daily use of the dominant hand, such as carrying and lifting might affect the tension of the surgical wound or cause lymphedema and, consequently, could impair recovery of the shoulder function.
Radiotherapy was also extracted as a cause of ROM (shoulder abduction) limitation in our study. It may be possible that the ROM impairment was caused by the influence on the soft tissue damage caused by radiotherapy. Yang et al. reported upper limb dysfunction at 12 months after surgery was associated with the type of surgery (mastectomy) and radiotherapy [12]. It has been reported that patients with breast cancer after surgery often suffer from less shoulder mobility that can substantially worsen during radiotherapy [22]. Several reports on interventions by exercise for the upper limb dysfunction during radiotherapy have mentioned some benefits of supervised exercise with a limitation of the small sample size to their study [23,24]. Considering the results of these reports, since radiotherapy for breast cancer is one of the apparent risk factors of the upper limb dysfunction, more effective interventions must be developed in the future. On the other hand, in this study, RT was not a significant negative factor for the recovery of shoulder flexion. As a possible reason for the different consequences, the area of skin tightness caused by RT might hinder the stretch of the skin for abduction rather than for flexion of the shoulder.
Because the DASH scoring system includes household chores, garden work, light recreation, transportation needs, and sexual activities, the score can be greatly influenced by factors such as age, conditions of joints other than upper limbs, mental status after cancer notification, and malaise due to preoperative chemotherapy. Although we did not conduct an investigation of the factor analysis on the recovery of the DASH score after breast cancer surgery, those confounding factors might be taken into consideration.
There were several limitations to our study. As we did not include a control group, the effect of home-based exercise using the DVD was not clear. To verify the effectiveness of the use of an exercise DVD, a randomized control study should be performed in the future. Since we analyzed only cases with axillary lymph node dissection in this study, the results may be different if sentinel cases would have been included. In addition, our study did not include the cases with shoulder dysfunction preoperatively and the cases of more than 90% recovery at 1 week after the operation. As we do not know what kind of exercise therapy is useful for ROM improvement, it should be clarified by a further study. In addition, the change of diameters of upper limbs before and after surgery was not investigated in this study. Therefore, the influence of lymphedema on the upper limb function should be investigated in a further study.
Conclusion
In conclusion, the side of surgery corresponding to the dominant hand and radiation therapy were negative factors for recovery of shoulder ROM. Although home-based exercise using a DVD was considered feasible, about 20% of the patients still had difficulties with shoulder ROM. In future research, patients with those factors might be targeted to investigate new effective interventions to prevent shoulder dysfunction after axillary lymph node dissection.
References
Devoogdt N, Van Kampen M, Christiaens MR, Troosters T, Piot W, Beets N, Nys S, Gosselink R (2011) Short- and long-term recovery of upper limb function after axillary lymph node dissection. Eur J Cancer Care (Engl) 20(1):77–86
Gosselink R, Rouffaer L, Vanhelden P, Piot W, Troosters T, Christiaens MR (2003) Recovery of upper limb function after axillary dissection. J Surg Oncol 83(4):204–211
Gomide LB, Matheus JP, Candido dos Reis FJ (2007) Morbidity after breast cancer treatment and physiotherapeutic performance. Int J Clin Pract 61(6):972–982
Moskovitz AH, Anderson BO, Yeung RS, Byrd DR, Lawton TJ, Moe RE (2001) Axillary web syndrome after axillary dissection. Am J Surg 181(5):434–439
Nesvold IL, Dahl AA, Løkkevik E, Marit Mengshoel A, Fosså SD (2008) Arm and shoulder morbidity in breast cancer patients after breast-conserving therapy versus mastectomy. Acta Oncol 47(5):835–842
Rietman JS, Geertzen JH, Hoekstra HJ, Baas P, Dolsma WV, de Vries J, Groothoff JW, Eisma WH, Dijkstra PU (2006) Long term treatment related upper limb morbidity and quality of life after sentinel lymph node biopsy for stage I or II breast cancer. Eur J Surg Oncol 32(2):148–152
Box RC, Reul-Hirche HM, Bullock-Saxton JE, Furnival CM (2002) Shoulder movement after breast cancer surgery: results of a randomised controlled study of postoperative physiotherapy. Breast Cancer Res Treat 75(1):35–50
Beurskens CH, van Uden CJ, Strobbe LJ, Oostendorp RA, Wobbes T (2007) The efficacy of physiotherapy upon shoulder function following axillary dissection in breast cancer, a randomized controlled study. BMC Cancer 7:166
Cinar N, Seckin U, Keskin D, Bodur H, Bozkurt B, Cengiz O (2008) The effectiveness of early rehabilitation in patients with modified radical mastectomy. Cancer Nurs 31(2):160–165
Kilgour RD, Jones DH, Keyserlingk JR (2008) Effectiveness of a self-administered, home-based exercise rehabilitation program for women following a modified radical mastectomy and axillary node dissection: a preliminary study. Breast Cancer Res Treat 109(2):285–295
McNeely ML, Campbell K, Ospina M, Rowe BH, Dabbs K, Klassen TP, Mackey J, Courneya K (2010) Exercise interventions for upper-limb dysfunction due to breast cancer treatment. Cochrane Database Syst Rev 16(6):CD005211
Yang EJ, Park WB, Seo KS, Kim SW, Heo CY, Lim JY (2010) Longitudinal change of treatment-related upper limb dysfunction and its impact on late dysfunction in breast cancer survivors: a prospective cohort study. J Surg Oncol 101(1):84–91
Dantas de Oliveira NP, Guedes TS, Holanda AM, Reis MA, da Silva CP, Rocha e Silva BL, Maia de Almeida GC, de Souza DL (2017) Functional disability in women submitted to breast cancer treatment. Asian Pac J Cancer Prev 18(5):1207–1214
Ashikaga T, Krag DN, Land SR, Julian TB, Anderson SJ, Brown AM, Skelly JM, Harlow SP, Weaver DL, Mamounas EP, Costantino JP, Wolmark N (2010) National Surgical Adjuvant Breast, Bowel Project. Morbidity results from the NSABP B-32 trial comparing sentinel lymph node dissection versus axillary dissection. J Surg Oncol 102(2):111–118
Levy EW, Pfalzer LA, Danoff J, Springer BA, McGarvey C, Shieh CY, Morehead-Gee A, Gerber LH, Stout NL (2012) Predictors of functional shoulder recovery at 1 and 12 months after breast cancer surgery. Breast Cancer Res Treat 134(1):315–324
Imaeda T, Satoshi T, Nakao Y, Nishida J, Hirata H, Ijichi M, Kohri C, Nagano A (2005) Validation of the Japanese society for surgery of the hand version of the disability of the arm, shoulder, and hand questionnaire. J Orthop Sci 10:353–359
Jester A, Harth A, Wind G, Germann G, Sauerbier M (2005) Disabilities of the arm, shoulder and hand (DASH) questionnaire: determining functional activity profiles in patients with upper extremity disorders. J Hand Surg (Br) 30(1):23–28
Lahham A, McDonald CF, Mahal A, Lee AL, Hill CJ, Burge AT, Cox NS, Moore R, Nicolson C, O’halloran P, Gilles R, Holland AE (2018) Acceptability and validity of ahome exercise diary used in home-based pulmonary rehabilitation: a secondary analysis of a randomized controlled trial. Clin Respir J 12(6):2057–2064
Petito EL, Nazario ACP, Martinelli SE, Facina G, De Gutierrez MGR (2012) Application of a domicile-based exercise program for shoulder rehabilitation after breast cancer surgery. Rev Lat Am Enfermagem 20(1):35–43
Albert US, Koller M, Kopp I, Lorenz W, Schulz KD, Wagner U (2006) Early self-reported impairments in arm functioning of primary breast cancer patients predict late side effects of axillary lymph node dissection: results from a population-based cohort study. Breast Cancer Res Treat 100(3):285–292
Kärki A, Simonen R, Mälkiä E, Selfe J (2005) Impairments, activity limitations and participation restrictions 6 and 12 months after breast cancer operation. J Rehabil Med 37(3):180–188
Senkus-Konefka E, Jassem J (2006) Complications of breast-cancer radiotherapy. Clin Oncol (R Coll Radiol) 18(3):229–235
Kneis S, Wehrle A, Ilaender A, Volegova-Neher N, Gollhofer A, Bertz H (2018) Results from a pilot study of handheld vibration: exercise intervention reduces upper-limb dysfunction and fatigue in breast cancer patients undergoing radiotherapy: VibBRa study. Integr Cancer Ther 17(3):717–727
Hwang JH, Chang HJ, Shim YH, Park WH, Park W, Huh SJ, Yang JH (2008) Effects of supervised exercise therapy in patients receiving radiotherapy for breast cancer. Yonsei Med J 49(3):443–450
Funding
This work was supported by Japan Agency for Medical Research and Development (AMED) (grant number: 16ck0106215).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was conducted with the approval of the Shikoku Cancer Center Ethical Committee (H24-No.13).
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kikuuchi, M., Akezaki, Y., Nakata, E. et al. Risk factors of impairment of shoulder function after axillary dissection for breast cancer. Support Care Cancer 29, 771–778 (2021). https://doi.org/10.1007/s00520-020-05533-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05533-7