Abstract
Purpose
It is not known which side effects (SEs) cancer patients undergoing definitive radiotherapy (RT) perceive as worse than others. Our objectives were to (1) identify the worst SEs in patients receiving definitive RT-predominant treatment using patient-reported outcomes and (2) investigate the prominence of physical SEs relative to psychosocial SEs.
Methods
In a single-center outpatient radiation oncology clinic, patients were surveyed on the final day of definitive RT. Sixty-seven cards listed SEs (40 physical and 27 psychosocial), and patients ranked the five most severe. Fifteen points were assigned to the top five selected SEs with descending scores of 5, 4, 3, 2, and 1.
Results
Fifty-five patients completed ≥ 4 weeks of RT with or without concurrent chemotherapy and had not received ≥ 4 weeks of neoadjuvant chemotherapy. Patients with head and neck and pelvis cancers perceived physical SEs as worse relative to psychosocial SEs; physical SEs filled 78% and 69% of the 15 points, respectively. In breast cancer patients, however, psychosocial SEs filled 45% of the 15 points in breast cancer patients (anxiety, depression, and sequelae), compared to 25% in others (P = 0.007). Affects my work, home duties, a SE not associated with the treatment itself, was the most frequently cited psychosocial SE (20% of cohort) and was ranked ninth overall.
Conclusion
Perceptions of SEs of cancer RT are dominated by physical quality of life (QoL) concerns and are influenced by the anatomic area receiving RT. Psychosocial QoL concerns are significantly more frequent in breast cancer patients.
Trial registration
ClinicalTrials.gov Identifier: NCT02978846
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Health-related quality-of-life (HRQoL) considerations play a growing role in disease management as cancer treatment and survival improve. This progress reflects improvements in both patient well-being and patient suffering. HRQoL, defined as a patient-reported assessment of one’s perceived physical, psychological, and social well-being, is nebulous and inherently difficult to measure [1,2,3]. Patient-reported outcomes (PRO) have hence become a powerful tool for gauging HRQoL and patient suffering [4, 5]. A practical method that may improve the HRQoL of a patient undergoing active treatment is to identify and address the symptoms the patient reports as the most severe (i.e., PRO), rather than offering treatments for symptoms that do not bother a patient or are not present.
Interestingly, it is not clear which side effects (SEs) are worse than others from the patient’s perspective (i.e., perception). Three studies have examined perceptions of SEs [6,7,8], but all three only evaluated patients with advanced cancer receiving chemotherapy (CT) alone. No studies report which side effects patients undergoing a prolonged course of chemoradiotherapy (CRT) perceive as the most severe.
Patients receiving CT alone perceive psychosocial side effects (SEs) to be increasingly prominent in severity when compared with physical SEs [6,7,8]. Improvements in symptom management and precision of treatment delivery have decreased toxicity and improved outcomes and are thought to be the reason for this shift. High psychosocial distress is associated with poorer adherence to treatment recommendations [9], lower satisfaction with care [10], worse quality of life [11], and even with decreased survival [12]. Psychological resource intervention is the best predictor of improved anxiety and depression [13].
We examined the perceptions of SEs of patients treated with RT with and without concurrent CT. The primary objective of this study was to examine perceptions of SEs in patients receiving RT-predominant care. The secondary objective was to investigate the prominence of physical SEs relative to psychosocial SEs. The purpose of the study is to identify which SEs are perceived as the most severe in order to allow for personalized symptom management. This was not a hypothesis-driven study, but we did expect patients to perceive psychosocial SEs at least equally as severe to physical SEs.
Methods and materials
Study population and design
Eligible cancer patients from a large urban teaching hospital participated in the study. Inclusion criteria included having received ≥ four consecutive weeks of definitive RT with or without concurrent CT, being ≥ 18 years of age, having the ability to understand and willingness to sign a written informed consent, being able to read English or Spanish, and having experienced SEs. Primary central nervous system disease or patients with brain metastases were excluded to minimize the confounding role of cognitive impairment. Written informed consent was obtained from each subject or guardian. Demographics and disease characteristics are shown in Table 1.
We wanted our study to focus on RT-driven treatments and their resulting SEs, so patients who had received ≥ 4 weeks of CT prior to CRT start were excluded in order to prevent pre-existing CT-associated SEs from confounding the primary goal. All aspects of their therapy were unaffected by the study. It was permissible for patients to have received surgery before radiation therapy.
On the final day of CRT, we asked each eligible patient if they had SEs from treatment. If they confirmed this, they were offered enrollment. Each patient was shown a set of cards which were comprised of two groups, 40 cards in Group A (physical SEs) and 27 in Group B (psychosocial SEs) (Table 2). On each card was the name of one potential SE of treatment. The cards were shown one at a time. Patients selected all cards that named a SE they attributed to their treatment. They then selected the 5 “most troublesome” cards from both Group A and from Group B, leaving up to 10 remaining cards. Finally, cards showing top 5 physical and top 5 psychosocial SEs were combined and shuffled, then the patient ranked them in order of severity. A score of 5, 4, 3, 2, and 1 was assigned to top 5 selected SEs in order of the most, second, third, fourth, and fifth severe. No points were assigned to SEs beyond the top 5. This summated to a total of 15 points per patient. Type and severity of SEs were endpoints. This process, as well as the list of SEs, was intentionally emulated from the three prior studies that examined perceptions of SE [6,7,8]. The list of SEs in the previous studies was not validated. In order to have our list of SEs be more RT-specific, we decided to refine our list of physical SEs. Eight SEs associated only with chemotherapy were removed, six SEs associated only with RT that would not have been in the original lists were added, and three SEs were combined with ones that overlapped with another (e.g., sore mouth and sore throat were combined to sore mouth and/or throat), and modifying 1 SE. This summated to 40 physical SEs versus 45 in the original studies. The addition of RT-specific SEs was based on a chapter review of the Handbook of Evidence-Based Radiation Oncology [14].
For each patient, we calculated a “Psychosocial SE Score,” defined here as the percentage of the total score of 15 that were Group B-Psychosocial SEs. For example, if a patient had two Psychosocial SE cards ranked in the top five, one in the first position, and one in the fourth position, and the rest were Physical SE cards, their percentage of Psychosocial SE Score was 47% [(5 + 2)/15].
Statistical analysis
We performed t tests to compare the psychosocial SEs in terms of the mean Psychosocial SE Score between various patient groups. We used t tests rather than ANOVA because the differences between the three locations generally fell into two rather than three values (i.e., H&N and Pelvis were similar) (Table 1). For comprehensiveness, ANOVA was performed during analysis and results did not change. A logistic regression model was further performed including previously identified variables associated with different mean Psychosocial SE scores (P value ≤ 0.1), and regression coefficients were reported. Fisher’s exact test was used to test the association between patient characteristics with depression and insomnia status.
SAS 9.4 (SAS Institute, Cary, NC, USA) was used to perform all analyses. All tests were two-sided at a significance level of 0.05.
Results
Fifty-five patients agreed to take part in the study. No patients declined enrollment. Table 2 lists all symptoms in order of frequency in patients’ top five SEs. A median of 25 cards were selected per patient (group A median = 17; group B median = 8). The first value in parentheses next to select SEs indicates its rank in the top 10 overall SE list, and the second value indicates its total score using the aforementioned 15-point system.
Median age was 59 (range 25–80). The most common malignancies in the group were breast (31%, n = 17), head and neck (25%, n = 14), prostate/genitourinary (15%, n = 8), gynecologic (11%, n = 6), and gastrointestinal (15%, n = 8). Ten (18%) patients received systemic treatment before CRT. Thirty (55%) patients received systemic treatment during RT; 17 of these were single agent cisplatin or platinum-based regimens, 7 were hormonal therapy with leuprolide or trastuzumab, and 6 were capecitabine or 5-fluorouracil-based regimens. Median RT dose was 52 Gy (range 41.4–79.2 Gy). Median time from biopsy to CRT completion was 169 days, or 5.6 months (range 77–4181 days).
Identification of patients with more severe psychosocial side effects
Mean Pyschosocial SE Score for the entire group was 32% (standard deviation (SD) 0.27), with a median of 27% (range 0–93%). Table 1 shows patient demographics and their respective Pyschosocial SE Scores on univariate analysis. Patients whose cancer was incidentally discovered reported more severe psychosocial SEs than those whose cancer was discovered from symptoms (Psychosocial SE Score 43% vs 23%, P = 0.004). Patients receiving concurrent systemic treatment reported less severe psychosocial SEs than others (23% vs 41%, P = 0.011). Breast cancer patients reported more severe psychosocial SEs than others (45% vs 25%, P = 0.007). Compared to patients with RT to the breast, thorax, or abdominal regions, those with RT to the head and neck reported less severe psychosocial SEs (22% vs 45%, P = 0.005) as did those with pelvic cancers (21% vs 45%, P = 0.008). Patients with > 6 months time from cancer biopsy to CRT completion reported more severe psychosocial SEs when compared to patients with ≤ 6 months time (44% vs 21%, P = 0.001).
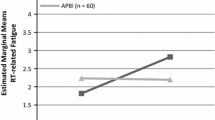
A logistic regression was performed that included the variables with P values ≤ 0.1. The results are shown in Fig. 1 and Table 3. Breast diagnosis (adjusted P = 0.031), Location (breast/thorax/abdominal: P = 0.007), and > 6 months from biopsy diagnosis to RT completion (P = 0.04) remained significant in predicting more severe psychosocial SEs.
Psychosocial side effect scores for select characteristics. Variables that were significantly (P ≤ 0.1) associated with Psychosocial SE Score in Table 1 were included in a logistic regression, and resultant P values are shown. Psychosocial SE Score is defined as the percentage of the 15-point total score that was psychosocial SEs. Patients with a breast diagnosis, B/T/A location of RT, and > 6 months from biopsy diagnosis to RT completion remained significant in predicting more severe Psychosocial SE Scores. SE side effects, B/T/A breast/thorax/abdomen, RT radiation therapy
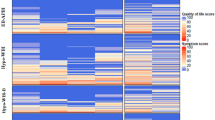
Identification and ranking of side effects by location of RT
Identifying and ranking overall SEs was less useful because the most severe physical SEs tended to depend on anatomic location of RT. Whereas previous similar studies arranged the patients by chemoregimen since certain CT causes particular physical SEs (e.g., alopecia with doxorubicin, neuropathy with paclitaxel), we arranged the patients based on location of RT. This fell into three locations, the head and neck (14 patients), the thorax/breast/abdomen (22 patients), and the pelvis (19 patients). The top 10 SEs for each location are shown in Table 4 along with its frequency in the top 5 within that subgroup and its absolute score using our 15-point scoring system. Over half (6 of 10, shaded) SEs in breast/thorax/abdomen patients were psychosocial, compared with 2 and 1 (shaded) in head and neck and pelvis patients, respectively.
Supplementary Table 1 shows select symptoms that were significantly associated with particular characteristics. Eighty-eight percent of patients that did not live with a significant other perceived “feeling down (depression)” as a severe SE, compared to 13% of patients that did live with a significant other (P = 0.005). Ninety percent of patients receiving systemic treatment during RT perceived “Difficulty sleeping” as a severe SE, compared to 10% of patients that did not receive systemic treatment (P = 0.016).
Discussion
A majority of symptoms are a small cohort
The SEs of cancer CRT reported by our patients and their resultant ranking by relative severity formed a distinctive profile. Physical SEs constituted 7 of the top 10 concerns, and psychosocial SEs constituted 3: the 6th, 9th, and 10th ranked symptoms. A median of 25 symptoms was attributed to their treatment, 17 of which were physical and 8 psychosocial. A smaller number of SEs, however, constitute the large majority of symptoms perceived as the most severe. Tables 2 and 4 demonstrate how most of the symptoms are reported at low rates of < 10% frequency. Few symptoms are reported by > 10% of the patients, and even less are reported at > 20% frequency. This information allows the clinician to focus on a more manageable and concise list of symptoms in which to optimize their knowledge and treatment.
Table 2 shows that affects my work, home duties was the most frequently cited psychosocial SE, ranked ninth overall, and was included among the five most severe SEs in one in five patients. In the most recent iteration in 2002, this SE was ranked fourth overall [6]. In contrast, in the 1983 study, the most severe psychosocial SEs tended to be associated with the process of treatment itself (e.g., thought of coming for treatment, the length of time required at the clinic, fear of having a needle) [7]. This demonstrates the continued improvements in cancer treatment and supportive therapies and confirms the importance of assessing a patient’s social support network.
Other findings include patients not living with a significant other more likely to perceive depression as a severe SE (Supplementary Table 1) although this group was not more likely to perceive psychosocial symptoms as more severe than physical symptoms (Table 1). This is consistent with the literature, which has found that widowed or separated patients report depression scores worse than do married patients [15]. Also, patients who received systemic treatment during RT were more likely to perceive insomnia as severe, as were (numerically) males, patients < 60 years, and those receiving higher doses of RT (Supplementary Table 1). The authors believe that this may be due to increased fatigue from the addition of concurrent CT.
Breast cancer patients and psychosocial side effects
On the final day of definitive CRT, we found that breast cancer patients perceive psychosocial symptoms as more severe than do patients with other cancer diagnoses. This is a novel finding. In our study, nearly half (45%) of the most severe symptoms in breast cancer patients were psychosocial, compared to 25% in non-breast cancer patients. Furthermore, the two SEs headaches, migraine and constantly tired ranked fourth and seventh overall, respectively, in breast/thorax/abdomen cancer patients but are absent in the top 10 for head and neck and pelvis patients (Table 4). These particular SEs are two of the most common somatic symptoms of underlying depression [16, 17]. The rise in these two SEs and their corresponding absence in the other two locations, subgroups which received higher doses of RT and higher reception of concurrent systemic treatment, may indicate somatic manifestations of anxiety and depression. If so, this would summate > 75% of their most severe symptoms as psychosocial in origin. As mentioned, high psychosocial distress is associated with poorer adherence to treatment recommendations [9], lower satisfaction with care [10], worse quality of life [11], and even with decreased survival [12, 13].
Improved precision of breast cancer treatment in all three treatment modalities (surgical, medical, and radiation oncology) has decreased physical symptoms. Tools like Oncotype DX eliminate the need for CT in select early stage patients, and none of our breast cancer patients received neoadjuvant or adjuvant CT. Mastectomy rates have decreased as lumpectomy rates have increased which has improved toxicity. Hypofractionated RT has begun to replace standard fractionation RT which has also improved toxicity [18]. Since we required each patient to select their five worst SEs, psychosocial symptoms may have filled the void left by a reduction in the physical symptoms.
Limitations
The primary limitation of the study is the use of relative rather than absolute severity of symptoms. This was the inherent design of the study, however. Also, the study was terminated early because the investigators observed, as we mentioned earlier, that the same small number of SEs was being repeatedly listed as the most severe. This is demonstrated by the dramatic decrease in frequency in Table 2. However, this did lead to the study being underpowered, which led to weaker statistical significance. The results of our trial should be interpreted in the context of the type of patients that were enrolled. This study has inherent cross-sectional design limitations, primarily that exposure and outcome are simultaneously assessed and temporal relationships cannot be confirmed. We did not screen for preexisting psychiatric conditions. Patients may have employed recall bias, selecting side effects that they more readily retrieved from memory; however, we tried to lessen this by displaying all of the most common side effects.
Conclusions
In conclusion, this study presents PROs about which symptoms are the most severe when receiving definitive CRT and contributes new data to an increasingly important topic. This information helps clinicians identify the most common symptoms to in order to improve patients’ HRQoL. Perceptions of SEs of cancer RT are dominated by physical QoL concerns and are influenced by the anatomic area receiving RT. The most severe psychosocial SEs are not treatment-based but rather are major functional and social aspects of HRQoL. Breast cancer patients have significantly worse psychosocial SEs relative to physical SEs when compared to non-breast cancer patients, and they may benefit from routine cognitive behavioral intervention referrals.
References
Guyatt GH, Feeny DH, Patrick DL (1993) Measuring health-related quality of life. Ann Intern Med 118(8):622–629
Testa MA, Simonson DC (1996) Assessment of quality-of-life outcomes. NEJM. 334(13):835–840
Karimi M, Brazier J (2016) Health, health-related quality of life, and quality of life: what is the difference? Pharmacoeconomics. 34(7):645–649
Deshpande PR, Rajan S, Sudeepthi BL, Nazir CA (2011) Patient-reported outcomes: a new era in clinical research. Perspect Clin Res 2(4):137
Anker SD, Agewall S, Borggrefe M, Calvert M, Jaime Caro J, Cowie MR, Ford I, Paty JA, Riley JP, Swedberg K, Tavazzi L, Wiklund I, Kirchhof P (2014) The importance of patient-reported outcomes: a call for their comprehensive integration in cardiovascular clinical trials. Eur Heart J 35(30):2001–2009
Carelle N, Piotto E, Bellanger A, Germanaud J, Thuillier A, Khayat D (2002) Changing patient perceptions of the side effects of cancer chemotherapy. Cancer. 95(1):155–163
Coates A, Abraham S, Kaye SB, Sowerbutts T, Frewin C, Fox RM, Tattersall MHN (1983) On the receiving end—patient perception of the side-effects of cancer chemotherapy. Eur J Cancer 19(2):203–208
Griffin AM, Butow PN, Coates AS, Childs AM, Ellis PM, Dunn SM, Tattersall MHN (1996) On the receiving end V: patient perceptions of the side effects of cancer chemotherapy in 1993. Ann Oncol 7(2):189–195
Atkins L, Fallowfield L (2006) Intentional and non-intentional non-adherence to medication amongst breast cancer patients. Eur J Cancer 42(14):2271–2276
Essen L, Larsson G, Öberg K, Sjödén PO (2002) Satisfaction with care’: associations with health-related quality of life and psychosocial function among Swedish patients with endocrine gastrointestinal tumours. Eur J Cancer Care 11(2):91–99
Stark D, Kiely M, Smith A, Velikova G, House A, Selby P (2002) Anxiety disorders in cancer patients: their nature, associations, and relation to quality of life. J Clin Oncol 20(14):3137–3148
Steel JL, Geller DA, Gamblin TC, Olek MC, Carr BI (2007) Depression, immunity, and survival in patients with hepatobiliary carcinoma. J Clin Oncol 25(17):2397–2405
Penninx BW, Guralnik JM, Havlik RJ et al (1998) Chronically depressed mood and cancer risk in older persons. J Natl Cancer Inst 90(24):1888–1893
Hansen EK, Roach M (2010) Handbook of evidence-based radiation oncology, 2nd edn. Springer, New York, NY
Sellick SM, Edwardson AD (2007) Screening new cancer patients for psychological distress using the hospital anxiety and depression scale. Psycho-Oncol. 16(6):534–542
Ohayon MM, Schatzberg AF (2003) Using chronic pain to predict depressive morbidity in the general population. J Clin Psychiatry 60(1):39–47
Tylee A, Gandhi P (2005) The importance of somatic symptoms in depression in primary care. Primary care companion to the. J Clin Psychiatry 7(4):167–176
Jagsi R, Griffith KA, Boike TP, Walker E, Nurushev T, Grills IS, Moran JM, Feng M, Hayman J, Pierce LJ (2015) Differences in the acute toxic effects of breast radiotherapy by fractionation schedule: comparative analysis of physician-assessed and patient-reported outcomes in a large multicenter cohort. JAMA Oncol 1(7):918–930
Funding
This study did not have any grants or financial support.
Author information
Authors and Affiliations
Contributions
All authors have read and approved the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary Table 1
Association between patient characteristics and select symptoms (in top 5 cards). P values were based on two-sided t-tests. (DOCX 13 kb)
Rights and permissions
About this article
Cite this article
Williams, P.A., Cao, S., Yang, D. et al. Patient-reported outcomes of the relative severity of side effects from cancer radiotherapy. Support Care Cancer 28, 309–316 (2020). https://doi.org/10.1007/s00520-019-04820-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-04820-2