Abstract
Purpose
To understand patient preferences for integrative therapeutics and/or modalities during cancer care.
Methods
Cancer patients currently going through treatment were recruited from the Mayo Clinic in Arizona. Participants were asked to engage in 1 of 4 focus groups to understand preferences regarding integrative therapeutic modalities in cancer treatment. Focus group data were transcribed and analyzed using thematic analysis. Eighty-five percent of inter-coder reliability was achieved with four team investigators.
Results
Nineteen cancer patients participated in four focus groups with mixed cancer types (42% breast cancer), gender (53% female), and age (69% over age 60). Focus group analyses resulted in five themes with respect to preferences regarding integrative therapeutic modalities among cancer patients: (1) preference regarding accurate and congruent information; (2) preference regarding stress and symptom management; (3) preference regarding discussion of integrative therapies with healthcare providers (4) preference regarding support from family and friends; and (5) preference regarding personalized holistic care.
Conclusions
Patients have a desire to discuss integrative therapeutic aspects of their cancer treatment with healthcare providers. Understanding patient preferences allows opportunity for oncology providers to increase awareness/education of integrative therapeutic modalities. Increased integrative therapeutic knowledge may best support recovery and increased quality of life.
Implications
Qualitative research may facilitate understanding the scope of cancer patient preferences regarding the desire and use of integrative therapeutic modalities. A conceptual understanding of cancer patient preferences regarding integrative therapies and modalities may best inform successful direction and efficacy of treatment strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the USA alone, there are more than 1.7 million new cancer cases and 600,640 deaths occurring in 2018 [1, 2]. Each year, these cancer patients are met with a challenging myriad of health issues. Cancer-related symptoms span a broad spectrum including physical pain, fatigue, and depression [3]. Although the bedrock of cancer care remains in conventional treatments, there is a strong and growing trend in the direction of incorporating integrative approaches such that therapeutics beyond conventional care are utilized to improve patient health and well-being. This type of approach and the accompanying practices were previously considered complementary and alternative medicine (CAM) practices [4]. Reportedly, 50–80% of adult patients with cancer have utilized some type of CAM health-related practice during their cancer journey. Across research and institutions, efforts have been made to establish a universally accepted name to give definition to the broad category of complementary and alternative medicine; however, at present time, this domain is still referred to by multiple titles. For purposes of this paper, the term—Integrative Therapies—will be used to define and reference the discussed complementary and alternative health-related modalities.
Integrative therapies have been commonly used and long considered as a valuable set of resources for patients with cancer [5, 6]. Integrative therapies use a whole person and multidimensional approach to cancer care, addressing multiple aspects of one’s health ranging from physical and psychosocial to spiritual influences [3]. Integrative therapies such as acupuncture, mind-body therapies, and movement practices are used along with conventional treatments like chemotherapy and radiation therapy. Integrative therapies have been utilized in symptom management, stress relief, improved quality of life, and reduced cancer recurrence—this relationship had been more prevalent in recent decades [6,7,8]. For example, acupuncture has been shown to improve patients’ quality of life and to help lessen some side effects of cancer treatment, such as fatigue and depression [9]. Several studies also have found that mindfulness approaches such as yoga and meditation have beneficial effects on several cancer-related physical and psychosocial symptoms, such as pain, nausea, vomiting, blood pressure, anxiety, and sleep disturbance [10]. While there is a high prevalence of integrative therapeutic modality use among cancer patients, understanding about patient preferences is limited to prevalence of use rather than appreciating rationale of choices.
Many studies have reported rates of integrative therapy use from 30 to 80% among various populations of cancer types, geography, and other factors [5, 11,12,13,14]. The range of reported prevalence is affected further by the specific therapies and modalities included in the study questionnaire assessment tool. For example, a population-based study of prevalence of integrative therapy use by cancer patients found that the most prevalent type of integrative therapy was prayer/spiritual practices (61.4%), followed by relaxation (44.3%), faith/spiritual healing (42.4%), nutritional supplements/vitamins (40.1%), and meditation (15%) [5]. While rates of integrative therapy use have been reported, we have very little in-depth insight about the patients’ perspectives on the integrative therapeutic modalities and preferences in cancer care. Although previous studies have examined integrative therapy use among cancer patients [5, 15], many utilized quantitative method approaches while qualitative studies are far less common. It remains unclear why patients choose integrative therapies or how they engage in specific integrative therapeutic modalities during their cancer care; additionally, little is understood about the barriers and facilitators in this decision-making process.
Integrative therapies focus primarily on healing and well-being, rather than disease management and cure; as such, its role is broad in the support of the cancer care journey. Comprehensive qualitative approaches are needed to better understand factors that contribute to the preferences of integrative therapies, and the functions of different integrative therapeutic modalities among cancer patients. The purpose of the current study is to understand the group and individual patient preferences regarding the use of integrative therapeutic modalities in cancer care.
Methods
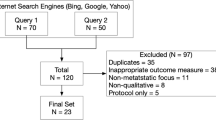
Participants and recruitment
Through selective sampling, patients who were currently undergoing or scheduled for cancer treatment between September 2014 and April 2015 at the Mayo Clinic in Arizona were recruited; the Mayo Clinic in Arizona provides care to 4700 cancer patients annually. Inclusion criteria included adult patients receiving cancer care at the Mayo Clinic in Arizona and were able to attend the focus group session. Participants were recruited through Medical Oncology and Radiation Oncology providers via physician invitation. If a patient expressed interest, the lead investigator explained the details of the study and, if the patient agreed to participate, he or she was screened for eligibility and completed a consent form to engage in a focus group discussion exploring cancer patient preferences with respect to Integrative Medicine and Health. No compensation or incentive was provided. The Mayo Clinic Institutional Review Board approved the study and patients provided written informed consent.
Conducting the focus groups
Focus group participants were asked to complete a hand-written survey indicating their basic demographics and additionally to answer (hand-written) questions related to the use and/or desire to use various integrative therapeutic modalities (yes vs. no). The focus groups were moderated by a trained integrative medicine physician using a series of 10 questions (see Appendix A) designed to explore factors impacting decisions in cancer care. The study questions were focused on healthcare during cancer treatment, nutrition, exercise, supplement or botanical use, stress management, additional integrative modalities, and potential barriers (see Appendix A). An outline for the focus group discussion was developed following a review of the literature and consultation with qualitative researchers and medical oncologists. The same discussion guide and questions were used across all focus groups. Focus groups lasted a maximum of 2 h and were videotaped. A research assistant took detailed field notes during the focus groups and the groups were audio-taped and transcribed verbatim. Transcriptions of each session were created with patient identifying information removed. The final number of focus groups was determined by reaching the proposed total number of participants and achieving information saturation.
Data analysis
Data analyses and reporting were conducted by the research team using thematic analysis as the analytical technique [16]. Steps in the qualitative analytical process included line-by-line coding, content analysis, and codebook development based on sorting and synthesis of codes into categories and major themes. The codebook was further developed with exemplar quotes from participants, which supported the identified categories and themes. Thematic analysis techniques identified sub-categories, which were then combined into categories and overarching themes/high-level categories that depicted the participants’ perspectives of integrative medicine modalities [17]. Data from each focus group were initially analyzed separately and manually coded by four study team investigators. Emergent themes were then compared across all groups until the inter-coder reliability was consistently at least 80% on 95% of the codes [18]. Inter-coder reliability was calculated as the total number of agreements and disagreements for all codes combined over the total number of agreements for all codes [19]. Through this process, four coders were able to check coding agreement on focus group transcripts and consistently got 85% inter-coder reliability.
Results
Demographics
In total, 19 cancer patients (53% female) participated in four focus groups (average participation per session included 5 patients ranging from 2 to 8) at the Mayo Clinic, Arizona. Focus groups were mixed between cancer types, gender, and age including 42% breast cancer patients, and 69% over the age of 60. Participants’ overall cancer care experience ranged from 5 to 10 (1 = Terrible, 5 = Neutral, and 10 = As good as it could be). On average, participation per session included 5 patients (range 2–8).
Integrative therapy use
Patients reported their specific use of integrative therapeutic modalities via written survey (Table 1). Among 19 participants, 72% (n = 13) reported the use of integrative therapy that focuses on nutrition, followed by breathing exercises (55.6%, n = 10), IV Nutraceuticals (44.4%, n = 8), natural product (41.2%, n = 7), and meditation (38.9%, n = 7).
Patient preferences and perspective regarding integrative therapeutic modalities
Five major themes emerged from the data that identify preferences regarding integrative therapeutic modalities among cancer patients: (1) preference regarding accurate and congruent information; (2) preference regarding stress and symptom management; (3) preference regarding discussion of integrative therapies with healthcare providers; (4) preference regarding support from family and friends; and (5) preference regarding personalized holistic care.
Preference regarding accurate and congruent information
Many participants voiced a strong desire for access to more accurate and relevant information and resources related to integrative therapies. Many participants expressed “lack of knowledge” and “uncertainty” about the use of integrative therapies in cancer care as a primary barrier to incorporating integrative therapies. Specifically, participants communicated their confusion and uncertainty with regard to the safety and use of botanicals and other natural products. “I took quite a few natural products all through treatment, but I don’t totally understand how they would work with my well-being.”
However, despite the theme of confusion and uncertainty, 37% of focus group participants reported using some form of natural product (supplements and botanicals) during their cancer treatment. In addition, participants expressed a desire to better understand the available integrative services/therapies and additional advice regarding when these modalities would be most appropriate in their cancer care plan. “What’s been confusing for me when and where different services are available to you through my treatment? I’m still trying to learn that.” Further, the focus group participants expressed a preference for integrative therapeutic materials to be provided consistently throughout their cancer care plan. “I just need the information to know where to get it from.”
I did see the dietician and she gave me a packet of information and we went over my diet and what is good for you and what is not good for you. But throughout the treatment, I guess I would say that I need more information.
Participants communicated their desire for increased availability of and access to more thorough and detailed integrative therapeutic information/resources.
Preference regarding stress and symptom management
Focus group participants verbalized frequently struggling with stress and its various effects and outcomes; they reported a range of symptoms including physical pain and emotional distress. Participants reported that the impact of the cancer-related stress they experienced increased negative symptoms such as memory loss and fatigue. Further, participants expressed that the stress they experienced interfered with their ability to implement and retain knowledge, such as applying specific nutrition recommendations. Among the focus groups, several participants reported the use of stress management techniques, particularly meditation, to provide relief. Some meditation type therapy and exercise are great forms of stress reliever.
I saw the social worker and did some of the imagery and the meditation. It helped, it did help me a little bit as far as some of the techniques, with regards to the breathing and taking myself somewhere else when I was feeling stressed, particularly with the chemo.
Collectively, many participants shared the belief that the mind-body techniques of integrative therapies could be a useful means of managing cancer-related stress.
Preference regarding discussion of integrative therapies with healthcare providers
Many of the focus group participants said they were interested in having the opportunity to discuss or extend the conversation about the use of integrative therapies with their healthcare team, specifically including decisions related to nutrition and exercise. Some participants reported that they were willing to initiate the discussion about their use of integrative therapies with HCPs to get helpful advice.
Well this is my second time around with breast cancer and what I learned the first time around is just that you have to ask questions and talk about the different treatment options including integrative therapies with your doctor. This time I had wonderful advice from my doctors here about incorporating exercise and nutrition and really took that to heart. I feel that helped with my experience during all three phases of my treatment.
I’ll probably just use my doctor’s guidance and make some decisions. They haven’t told me when I am going to be doing my other treatment but I’ll still work with my oncologist to get advice and any recommendation.
While patients often expressed a conviction of trusting they were in the appropriate place for their cancer care, they expressed a desire for further guidance from their health care providers (HCPs) surrounding the use of integrative therapies. Patients discussed the importance of being able to trust and turn to their healthcare providers regarding the use of integrative therapies.
I think that’s where the trust with your team comes into play. When I first began doing my research, it was very difficult to decide whether the treatment modality that was being prescribed for me was going to be the most successful.
Preference regarding support from family and friends
The focus group participants expressed a desire to know friends and family members’ previous experiences with integrative therapies and/or how they currently engage in specific integrative therapeutic modalities. Specifically, participants often received information and support from family members and friends regarding integrative therapeutic modalities, especially with respect to about nutrition and supplements.
I think one of the biggest helps for me has been through my faith community, loosely organized women, who share with one another their experiences and their treatment modalities from the different organizations, hospital units, in the greater Phoenix area, or outside of Phoenix. Some have gone to other parts of the country for their treatments and its everyone has been different so it’s you know how do you decide what your modality that’s been suggested for you is right or not when you see all of these other people doing something very different.
As might be expected, patients conveyed the importance of being able to receive support from family and friends and share information about different integrative therapeutic modalities.
Preference regarding personalized holistic care
Participants expressed a belief that combining conventional medicine and integrative therapeutic strategies would provide more personalized holistic approach to their care- this perception captures the core of integrative therapies. Participants shared a desire for their providers to consider all options combining both conventional biomedical treatments and integrative therapeutic treatments.
I was able to access some information at Mayo and incorporate a lot of what they shared with me. But that is depending on what your needs are, how long will you know. I think we all understand there’s a natural sort of demand on CAM treatment.
In order to get personalized care, participants also emphasized the importance of communication between providers and patients. “I think the best advice I would give is just not to be afraid to ask questions. One thing I’ve learned was just no questions a bad question and talk to your oncologist and ask them questions.” In addition, a few participants want minimal information materials, or “only what I need to know (personalized),” through access to ongoing research trials and professional publications. “There’s so much literature, it’s overwhelming.”
Discussion
The primary aim of this study was to understand the group and individual patient preferences regarding the use of integrative therapeutic modalities in cancer care. Data summarized from focus groups illustrated the following five themes related to cancer patient preferences regarding integrative therapies: (1) preference regarding accurate and congruent information; (2) preference regarding stress and symptom management; (3) preference regarding discussion of integrative therapies with healthcare providers; (4) preference regarding support from family and friends; and (5) preference regarding personalized holistic care.
Many participants in this study had no prior experience with integrative therapeutic modalities. Specifically, study participants reported lack of knowledge and appropriate guidance about integrative therapies as reasons for not yet incorporating these modalities and healthcare strategies. Participants further expressed a desire for more accurate and congruent information regarding a timeline to help them detail and understand when certain integrative therapeutic modalities may be most beneficial in their cancer care journey. This theme runs parallel to the vision of the Society for Integrative Oncology (SIO) to further develop clear, usable, methodologically strong, and transparent guidelines on the use of integrative therapies for patients with specific types of cancer. Clearly, there is a need and great opportunity for healthcare providers to inform cancer patients about the general and specific uses of integrative therapies to best support patient recovery, health, and quality of life. Increased awareness of and education regarding integrative therapeutic practices would allow patients to make more informed decisions. Future research will contribute to the understanding of patient preferences and efficacy of integrative therapeutics.
Furthermore, cancer patients in the focus groups expressed a desire for receiving a personalized holistic care. Combining conventional medicine and integrative therapeutic strategies would provide more personalized holistic approach to their care consider all options combining both conventional biomedical treatments and integrative therapeutic treatments. This patient-focused theme is also consistent with the vision of the SIO with the intention being that: “…research inform the true integration of complementary modalities into oncology care so that evidence-based complementary care is accessible and part of standard cancer care for patients across the curriculum.” Previous research also suggests that combining complementary modalities with mainstream conventional therapies was effective into the overall strategy of symptom control in patients with cancer, including pain management and mood disorders such as depression and anxiety [3, 20, 21]. However, integrative therapies can be helpful for some but not all patients. Parameters to identify the appropriate types of integrative therapeutic modalities and their potential risks/benefits to deliver a personalized care are not clear. Future research is needed to develop practical methods for providers based on research evidence, clinical judgment, and patients’ preferences, which will guide HCPs to make appropriate recommendations.
Collectively, participants expressed a desire to know friends and family members’ experiences regarding their use of integrative therapies, and discussed a preference of receiving advice from family and friends primarily with respect to nutrition and supplements. The majority of participants stated that they received more nutrition and supplement advice from family and friends than from their health care providers; these findings are consistent with previous studies [22, 23]. Our participants reported that 41% used some sort of natural product, which correlates closely with a recent survey reporting 35% of responding patients were using natural products [22]. Many participants took commonly used supplements (e.g., multivitamin, vitamin C, calcium, vitamin D, glucosamine) prior to their cancer diagnosis and continued to do so afterwards. In the current study, motivation and interest in integrative therapeutic modalities more commonly came from patients themselves or personal contacts, rather than the healthcare team. This is consistent with the findings of King and colleagues [22] who studied the perspective of HCPs as well as the patients. Receiving information and support from family and friends may hold a deep merit and value through the social connection; yet, it is imperative that the information provided is specific, accurate, and appropriate to the cancer patient.
Participants discussed the importance of being able to trust in their healthcare providers and reported a desire to have more discussion with their HCPs regarding their use of integrative therapeutic modalities; interestingly, these findings are in contrast to previous studies demonstrating that patients did not disclose their use of integrative therapies at all with their health care providers [22]. Reasons for lack of disclosure are unclear; however, it is important for patients to have an opportunity to discuss these aspects of their cancer care with their healthcare providers as part of ongoing routine office visits. Previous studies suggest that patient-physician communication about the use of integrative therapies may reinforce the potential benefits and prevent dangerous side effects from unproven therapies [24]. Given the conflicting benefits and risks associated with different integrative therapeutic modalities, communication between patients and physicians must be improved to maximize the benefits in cancer care [25].
Limitations
Our study has several limitations. Our sample was small and self-selected from one cancer center, which limits generalizability of the findings. The qualitative methods do not provide a determination of the exact proportions of a certain perspective held; however, the themes prevailed strongly across all focus groups. We have confidence these themes reflect the patient perception for the need and utility of integrative therapeutic strategies in their cancer care. We are also missing the perspective of the HCPs, which is vital to this discourse. We focused on the types of modalities patients were engaged with and why, and less on what benefits they were receiving from these strategies. Further exploration of these aspects will lead to examination of the outcomes that are being achieved for cancer patients, for which so much is at stake. Lastly, the voluntary participation of these participants’ suggests engagement and interest in integrative therapeutic modalities and may not represent the general cancer population.
Future directions/conclusion
Many cancer patients reported using integrative therapeutic modalities alongside conventional medicines, yet these strategies are frequently not discussed with oncologists and health care providers. Lack of pertinent communication may increase potential negative interactions and preventable harms; suitability and usage of integrative therapeutic modalities should be included in ongoing cancer care. Specific physician training may best support a robust approach to improve communication and coordination among patients and healthcare teams.
Clearly, there is a well-documented need for increased education and communication regarding integrative therapeutic modalities and strategies for cancer patients and healthcare teams. Patients and providers may benefit greatly from programs designed to support a more inclusive and holistic method to cancer care. Collaborative efforts to understand preferences regarding the use of integrative therapeutic modalities in cancer patients may provide the necessary framework for a more comprehensive recovery treatment plan as well as the potential for short- and long-term increased quality of life.
References
Sohl SJ, Borowski LA, Kent EE, Smith AW, Oakley-Girvan I, Rothman RL, Arora NK (2015) Cancer survivors’ disclosure of complementary health approaches to physicians: the role of patient-centered communication. Cancer 121(6):900–907. https://doi.org/10.1002/cncr.29138
American CS (2009) Cancer Facts & Figures 2009. American Cancer Society, Atlanta
Deng G, Cassileth B (2014) Integrative oncology: an overview. Am Soc Clin Oncol Educ Book 34:233–242. https://doi.org/10.14694/EdBook_AM.2014.34.233
Hu XY, Lorenc A, Kemper K, Liu JP, Adams J, Robinson N (2015) Defining integrative medicine in narrative and systematic reviews: a suggested checklist for reporting. Eur J Integr Med 7(1):76–84. https://doi.org/10.1016/j.eujim.2014.11.006
Gansler T, Kaw C, Crammer C, Smith T (2008) A population-based study of prevalence of complementary methods use by cancer survivors: a report from the American Cancer Society’s studies of cancer survivors. Cancer 113(5):1048–1057. https://doi.org/10.1002/cncr.23659
Ernst E, Cassileth BR (1998) The prevalence of complementary/alternative medicine in cancer: a systematic review. Cancer 83(4):777–782. https://doi.org/10.1002/(SICI)1097-0142(19980815)83:4<777::AID-CNCR22>3.0.CO;2-O
Sparber A, Bauer L, Curt G, Eisenberg D, Levin T, Parks S, Steinberg SM, Wootton J (2000) Use of complementary medicine by adult patients participating in cancer clinical trials. Oncol Nurs Forum 27(4):623–630
Molassiotis A, Fernadez-Ortega P, Pud D, Ozden G, Scott JA, Panteli V, Margulies A, Browall M, Magri M, Selvekerova S, Madsen E, Milovics L, Bruyns I, Gudmundsdottir G, Hummerston S, Ahmad AM, Platin N, Kearney N, Patiraki E (2005) Use of complementary and alternative medicine in cancer patients: a European survey. Ann Oncol 16(4):655–663. https://doi.org/10.1093/annonc/mdi110
Molassiotis A, Bardy J, Finnegan-John J, Mackereth P, Ryder DW, Filshie J, Ream E, Richardson A (2012) Acupuncture for cancer-related fatigue in patients with breast cancer: a pragmatic randomized controlled trial. J Clin Oncol 30(36):4470–4476
Buffart LM, Van Uffelen JG, Riphagen II, Brug J, van Mechelen W, Brown WJ, Chinapaw MJ (2012) Physical and psychosocial benefits of yoga in cancer patients and survivors, a systematic review and meta-analysis of randomized controlled trials. BMC Cancer 12(1):559
Matthews AK, Sellergren SA, Huo D, List M, Fleming G (2007) Complementary and alternative medicine use among breast cancer survivors. J Altern Complement Med 13(5):555–562. https://doi.org/10.1089/acm.2007.03-9040
Brauer JA, El Sehamy A, Metz JM, Mao JJ (2010) Complementary and alternative medicine and supportive care at leading cancer centers: a systematic analysis of websites. J Altern Complement Med 16(2):183–186. https://doi.org/10.1089/acm.2009.0354
Cassileth BR, Deng G (2004) Complementary and alternative therapies for cancer. Oncologist 9(1):80–89
Horneber M, Bueschel G, Dennert G, Less D, Ritter E, Zwahlen M (2012) How many cancer patients use complementary and alternative medicine: a systematic review and metaanalysis. Integr Cancer Ther 11(3):187–203. https://doi.org/10.1177/1534735411423920
Eisenberg DM, Kessler RC, Van Rompay MI, Kaptchuk TJ, Wilkey SA, Appel S, Davis RB (2001) Perceptions about complementary therapies relative to conventional therapies among adults who use both: results from a national survey. Ann Intern Med 135(5):344–351
Braun V, Clarke V (2006) Using thematic analysis in psychology. Qual Res Psychol 3(2):77–101
Eliot & Associates(2005) Guidelines for Conducting a Focus Group. Available at: http://assessment.aas.duke.edu/documents/How_to_Conduct_a_Focus_Group.pdf. Last accessed 30 April 2017.
Creswell JW (2009) Research design : qualitative, quantitative, and mixed methods approaches, 3rd edn. Sage Publications, Thousand Oaks
Campbell JL, Quincy C, Osserman J, Pedersen OK (2013) Coding in-depth Semistructured interviews:problems of unitization and intercoder reliability and agreement. Sociol Methods Res 42(3):294–320. https://doi.org/10.1177/0049124113500475
Deng G, Cassileth BR (2005) Integrative oncology: complementary therapies for pain, anxiety, and mood disturbance. CA Cancer J Clin 55(2):109–116
Chen KW, Berger CC, Manheimer E, Forde D, Magidson J, Dachman L, Lejuez C (2012) Meditative therapies for reducing anxiety: a systematic review and meta-analysis of randomized controlled trials. Depress Anxiety 29(7):545–562
King N, Balneaves LG, Levin GT, Nguyen T, Nation JG, Card C, Truant T, Carlson LE (2015) Surveys of cancer patients and cancer health care providers regarding complementary therapy use, communication, and information needs. Integr Cancer Ther. https://doi.org/10.1177/1534735415589984
Vapiwala N, Mick R, Hampshire MK, Metz JM, DeNittis AS (2006) Patient initiation of complementary and alternative medical therapies (CAM) following cancer diagnosis. Cancer J 12(6):467–474
Davis EL, Oh B, Butow PN, Mullan BA, Clarke S (2012) Cancer patient disclosure and patient-doctor communication of complementary and alternative medicine use: a systematic review. Oncologist 17(11):1475–1481. https://doi.org/10.1634/theoncologist.2012-0223
Deng GE, Frenkel M, Cohen L, Cassileth BR, Abrams DI, Capodice JL, Courneya KS, Dryden T, Hanser S, Kumar N, Labriola D, Wardell DW, Sagar S, Society for Integrative O (2009) Evidence-based clinical practice guidelines for integrative oncology: complementary therapies and botanicals. J Soc Integr Oncol 7(3):85–120
Acknowledgements
The authors dedicate this article to the memory of Julie McNulty, RN, PhD, CPHQ, who passed away prior to publication. The authors gratefully acknowledge her contribution in developing this article. Her passion for and dedication to improving health and wellness for patients with cancer and survivors will be remembered.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The Mayo Clinic Institutional Review Board approved the study and patients provided written informed consent.
Conflict of interest
The authors declare that that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Integrative Oncology Focus Group Questions
Engagement
-
1.
What 3 things made/are making the biggest difference in your healthcare during your cancer experience?
-
2.
What do you notice has made/is making a difference in other peoples’ healthcare cancer experience (e.g. friends, family, others in treatment at the same time as you)?
Exploration
-
3.
During your cancer experience, have you received consistent nutrition advice? What has been most helpful? What has been most confusing?
-
4.
Exercise:
-
a.
Did you exercise before diagnosis?
-
b.
Are you exercising now?
-
c.
Do you exercise how you want to (both type of exercise and movement)?
-
d.
How could it be better?
-
a.
-
5.
Natural Products (supplements and botanicals):
-
a.
Did you take natural products before diagnosis?
-
b.
Do you take natural products now?
-
c.
Where do you become educated on what to take?
-
d.
Do you share the use of these products with your providers?
-
a.
-
6.
Do you intentionally have strategies to manage your stress? What are they?
-
7.
Did you use Integrative Medicine modalities (see list from survey) during your cancer journey and experience?
-
a.
If yes, which were most important to your health and healing?
-
a.
-
8.
What Integrative Medicine modalities (see list) would you liked to have used in your cancer experience but did not? What were the barriers?
-
9.
What has been missing in your cancer experience at the Mayo Clinic?
Exit Question
-
10.
Is there anything else you would like to add?
Rights and permissions
About this article
Cite this article
Kim, W.(., James, D. & Millstine, D.M. Integrative medicine therapeutic approaches to cancer care: patient preferences from focus groups. Support Care Cancer 27, 2949–2955 (2019). https://doi.org/10.1007/s00520-018-4601-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4601-7



