Abstract
Purpose
Hydration is needed before and after cisplatin infusion for reducing the risk of nephrotoxicity. Even though there is no standard regimen, patients receive mostly intravenous hydration before and after cisplatin leading hospitalization during at least one night. Since the feasibility has been published, oral hydration after cisplatin was implemented in our practice. The safety of this new way of hydration needs to be assessed in clinical practice.
Methods
We collected medical records from patients treated by cisplatin for lung cancer in our unit between 2010 and 2016. We retrospectively analyzed the incidence of cisplatin induced nephrotoxicity between after and before the change of hydration regimen.
Results
Our patient cohort included 241 patients hydrated by intravenous regimen (IV/IV group) and 276 patient hydrated by intravenous and oral regimen (IV/PO group). Grade ≥ 1 nephrotoxicity occurred in 39.4 and 25.7% in the IV/IV and IV/PO groups respectively (p = 0.001). Age over 70 at baseline was a predictive factor for nephrotoxicity, but not estimated glomerular filtration rate nor cisplatin-associated drugs. After a multivariate analysis, age remained a predictive factor for nephrotoxicity and IV/PO hydration associated with a decrease in nephrotoxic risk.
Conclusion
The implementation of oral hydration in our practice was not associated with an increase in nephrotoxicity. Our observation based on large data from clinical practice shows that oral hydration after cisplatin is safe.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cisplatin is a widely used cytotoxic drug for a broad spectrum of malignancies, including lung cancer. Although new drugs have been introduced such as angiogenesis inhibitors, tyrosine kinase inhibitors, or immunotherapy, cisplatin remains the basis of many combinations as a first-line treatment for both non-small cell and small cell lung cancer [1,2,3].
Like other cytotoxic agents, cisplatin has a narrow therapeutic index and can induce neurotoxicity, ototoxicity, nausea and emesis, or nephrotoxicity. Nephrotoxicity is the main dose-limiting effect of cisplatin, since it occurs in about one third of patients receiving cisplatin [4]. Nephrotoxicity arises as an acute reduction in glomerular filtration rate, an increase in serum creatinine and long-term renal failure [5]. Nephrotoxicity is partly explained by tubular re-absorption that causes accumulation of cisplatin leading to renal tubular cell death [6].
Active hydration before, during, and after cisplatin infusion is accepted as the standard of care for reducing the cisplatin-associated nephrotoxic risk since it decreases tubular uptake by expanding volume [7, 8]. Various hydration regimens have been proposed, but none is the gold standard. The most frequently used hydration regimens in France consist of intravenous (IV) pre-hydration with 1–2 L of normal saline for 6 h before cisplatin infusion, and IV post-hydration with 1–2 L after cisplatin infusion. These long-duration hydration regimens require patients to stay at least one night at hospital. Since anticancer drugs are now mostly administered in outpatient units, this lengthy hydration regimen is less feasible in current oncology practice.
Since aggressive hydration regimens (i.e., high hydration volume) do not seem to reduce the nephrotoxicity risk [9], some authors have suggested that patients could receive shorter IV hydration regimens without increasing the nephrotoxicity risk. Since the 2012 publication of a retrospective non-comparative study documenting the feasibility of oral hydration after cisplatin infusion [10], we changed our practice: while IV hydration is still performed before cisplatin infusion, patients are advised to drink a large quantity of water during the days following cisplatin infusion.
The aim of our study was to assess the safety of oral hydration post-cisplatin 3 years after it was implemented in our unit by comparing the incidence of nephrotoxicity before and after this change in practice.
Patients and method
This was a single-center, retrospective study based on data extracted from the existing database of our prescription software for anticancer drugs at the University Hospital of Toulouse.
Patients
Data from patients treated with any cisplatin-based regimen for lung cancer (no matter the histology grade) or malignant mesothelioma in our outpatient lung cancer unit between 2010 and 2016 were evaluated retrospectively. We selected patients who received cisplatin either as post-operative or first-line metastatic treatment. To be included in the analysis, patients must have been treated with at least one course of cisplatin combination and had their renal function determined before and after the cisplatin treatment.
Since the mode of hydration after cisplatin changed in 2013, the patients were divided into two groups: patients treated between 2010 and 2012 were in the IV/IV hydration group and those treated between 2014 and 2016 were in the IV/PO hydration group.
Data collected were the patients’ demographic parameters (age, sex), morphology parameters (weight, body surface area, body mass index), laboratory test results (serum creatinine (SCr), estimated glomerular filtration rate (eGFR)), and treatment parameters (dose of cisplatin by course, number of cisplatin courses, combination regimen, history of switch from cisplatin to carboplatin).
Hydration regimen
All patients were prehydrated with 2 L of NaCl 0.9%, 1 g/L KCl, and 1 g/L MgSO4 for 6 h before the cisplatin infusion. Patients in the IV/IV group (i.e., treated between 2010 and 2012) were hydrated after the cisplatin infusion with 1 L of NaCl 0.9%, 1 g/L KCl, and 1 g/L MgSO4 for 2 h. Patients in the IV/PO group (i.e., treated between 2014 and 2016) were advised to drink as much water as they could (at least 1 L per day) on the days following cisplatin infusion. Neither diuretics nor mannitol were administered in any group.
Nephrotoxicity evaluation
Serum creatinine levels before each course were measured from the first cisplatin infusion until the last cisplatin infusion or the first carboplatin infusion, as the case may be. The eGFR was calculated using the MDRD formula [11]. The primary outcome was the occurrence of nephrotoxicity at any time during the follow-up period defined using and the Common Terminology for Criteria for Adverse Event (CTCAE) version 4.0 and the RIFLE (risk, injury, failure, loss, and end stage) criteria [12].
-
Grade ≥ 1 nephrotoxicity was defined as follows: decrease in eGFR of > 25% or increase in serum creatinine level of ≥ 1.5 times the baseline level.
-
Grade ≥ 2 nephrotoxicity was defined as follows: decrease in eGFR of > 50% or increase in serum creatinine level of ≥ 2 times the baseline level.
-
Grade ≥ 3 nephrotoxicity was defined as follows: decrease in eGFR of > 75% or increase in serum creatinine level of ≥ 3 times the baseline level.
Since carboplatin is an alternative to cisplatin in case of emerging or potential toxicity (nephrotoxicity, neurotoxicity, ototoxicity, etc.), the incidence of switching from cisplatin to carboplatin was a secondary outcome to assess cisplatin toxicity.
Statistical analyses
Most quantitative variables were converted into categorical variable using the median as the cutoff point; a more clinically relevant cutoff point was used for baseline eGFR (90 mL/min/1.73 m2) and age (70 years old). Association between incidence of grade ≥ 1 nephrotoxicity and categorical variables (patient characteristics, treatment parameters, or baseline eGFR) was assessed with the chi2 test or Fisher’s exact test if necessary. All significant variables in the univariate analyses (p value < 0.1) were introduced in a multivariate logistic regression; then, a stepwise backward elimination of variables was performed to retain only variables with a p value < 0.01 in the final model. All analyses were carried out using R software version 3.3.1 (R Core team 2013).
Results
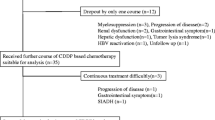
Patients
In the first group, 241 patients treated by cisplatin as first-line therapy between 2010 and 2012 were assessed for nephrotoxicity among the 258 selected (93.4%), whereas in the second group, 276 patients among the 296 (93.2%) treated between 2014 and 2016 were assessed. The patients’ characteristics are shown in Table 1. The two groups were comparable in terms of patient demographics, morphology, and laboratory test results. A median of three cisplatin course (range 1–6) was administered for each group. The body surface area used to calculate the dose of cisplatin was capped at 2 m2, which explains why the cisplatin dosage was low (< 70 mg/m2) in the largest patients. Pemetrexed- and/or bevacizumab-based regimens were more common in the 2014–2016 treatment period, but the number of cisplatin courses and the cisplatin dosage were comparable across the two groups.
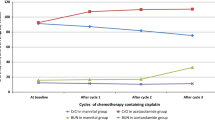
Nephrotoxicity
Grade ≥ 1 nephrotoxicity occurred in 39.4% of patients of the IV/IV hydration group and 25.7% of patients in the IV/PO hydration group (p = 0.001). Grade ≥ 2 nephrotoxicity occurred in 3.7% of patients of the IV/IV hydration group and 1.8% of patients in the IV/PO hydration group (p = 0.27). Grade ≥ 1 nephrotoxicity occurred in a median of 65 days in the IV/IV hydration group and 60 days in the IV/PO hydration group. When nephrotoxicity was observed, it was not reversible, since no improvement of eGFR occurred during the treatment period.
The predictors of grade ≥ 1 nephrotoxicity based on the univariate analysis are shown in Table 2. Hydration group, a pemetrexed-based regimen, age and dosage were included in the multivariate analysis. Only hydration group and age were retained in the final model (Table 2). The IV/PO hydration group was associated with a decrease in the risk of nephrotoxicity and being more than 70 years of age was associated with an increase.
Switch from cisplatin to carboplatin
A switch from cisplatin to carboplatin (no matter the reason) occurred in 32.8% of patients in the IV/IV hydration group and 32.2% of patients the IV/PO hydration group (p = 0.9). Predictors of a switch to carboplatin based on the univariate analysis are shown in Table 3. Only being more than 70 years old and having baseline eGFR < 90 mL/min/1.73 m2 were correlated with the need to switch to carboplatin. These two variables remained significant in the multivariate logistic regression model (Table 3); thus, both were associated with an increased need to switch to carboplatin.
Discussion/conclusion
Among the 517 patients evaluated, 32% had grade ≥ 1 nephrotoxicity and 2.7% had grade ≥ 2; no grade 3 nephrotoxicity was observed. These results are consistent with those published previously [4]. Our multivariate analysis showed that changing the hydration regimen did not increase the incidence of nephrotoxicity. Moreover, patients who hydrated using the IV/PO regimen had a significant decrease in nephrotoxicity. Since volume of water consumed was not monitored, we cannot explore if this was due to a difference of volume between the two hydration regimens. The protective effect of oral magnesium supplementation [13, 14] has been described. So we may hypothesize that patients advised to drink the days following cisplatin infusion should have a better dietary electrolyte intake that could explain this decrease in nephrotoxicity. The prevention of chemotherapy-induced nausea and vomiting could indirectly influence the nephrotoxicity by facilitating the oral hydration [15], but since the antiemetic regimen was the same during our observation period, a better nausea and vomiting control could not be considered as confounding factor.
The other factor associated with an increasing risk of nephrotoxicity was being more than 70 years of age. The age effect was expected since it has already been identified as a predictive factor for cisplatin nephrotoxicity [4]; however, it could also be the result of a poor performance status or associated comorbidity. Since full clinical data for our patients were not available, we could not conclude that age is an independent predictive factor for nephrotoxicity. Nevertheless, it suggests that frail patients are more susceptible to nephrotoxicity.
Unexpectedly, we found no relationship between altered eGFR at baseline and nephrotoxicity, neither in the univariate nor in the multivariate analysis, although it has been shown as a predictive factor for nephrotoxicity [16]. Since altered eGFR was associated with a higher rate of switching from cisplatin to carboplatin, we can presume that carboplatin was used to replace cisplatin earlier for patients with low eGFR before they experienced nephrotoxicity. Interestingly, the IV/PO hydration regimen was not associated with carboplatin use; hence, the benefit of oral hydration is not due to the protective effect of switching to carboplatin.
Age > 70 was also associated with carboplatin use. Despite careful use of cisplatin in older patients with an early switch to carboplatin, the nephrotoxicity rate was higher. This could be explained by confounding factors that influence nephrotoxicity in older patients, independent of whether carboplatin is used or not.
No influence of the treatment associated with cisplatin was observed on nephrotoxicity. Recent drugs such as pemetrexed or bevacizumab—while suspected to be nephrotoxic [17]—were not associated with an increase in cisplatin nephrotoxicity. It should be noted that the nephrotoxic risk was not evaluated during the maintenance period after cisplatin, only during the combination period.
In the multivariate analysis, we found no significant correlation between the cisplatin dose and nephrotoxicity, whereas it is known to be a dose-dependent side effect [18]. Indeed, a dose > 75 mg/m2 was associated with a 1.5-fold increasing risk of nephrotoxicity, but not at a significant level. In our population, cisplatin regimens were relatively homogenous with very low between-patient dose variation, which may explain the lack of correlation between dose and toxicity.
The main limitation of our study is the lack of clinical data such as performance status, cancer stage, comorbidity, and associated treatment that can influence cisplatin nephrotoxicity (such as use of non-steroidal anti-inflammatory drugs [19]. Nevertheless, the available characteristics were comparable between the two hydration regimen groups. Clinical practice did not change between the two hydration regimens except for combination treatments, but the multivariate analysis did not find any effect of cisplatin-associated drugs on nephrotoxicity. While this is not truly a comparative study since patients were not treated during the same period, the multivariate analysis allowed us to conclude that an IV/PO hydration regimen is not associated with worse safety outcomes.
Other studies explored the feasibility of short-duration hydration regimens, most of them performed on non-Caucasian patients. Tiseo et al. [20] in a non-comparative retrospective study were the first to report the feasibility of a short IV hydration (normal saline 2 h before and 2 h after cisplatin) with a decrease in creatinine clearance ranged between 11 and 39.9% in 40% of patients. Ouchi et al. [21] and Yamaguchi et al. [22] in two similar retrospective studies compared short IV hydration (2 L of normal saline infused over 4 h started before and ended after cisplatin) to continuous hydration (normal saline over 24 h). They observed no difference in nephrotoxicity between the two hydration regimens but the numbers of patients were limited. Three prospective studies demonstrated the feasibility of short-term and low volume hydration [23,24,25]. The incidence of nephrotoxicity was below 4% but they only looked at nephrotoxicity after the first cisplatin infusion. Sato et al. [26] tried to add oral hydration solution to short IV hydration in a 47 patient’s non-comparative prospective study. Our study was based on the publication of Lavolé et al. [10]. In this study, patients were prehydrated with 2 L of 5% dextrose with 4 g/L NaCl, 2 g/L KCl, 1 g/L MgCl2, and 1 g/L CaCl2, and advised to drink large quantities of liquid during the days following chemotherapy. In this non-comparative retrospective study, they showed only 20% of patients with a decrease in creatinine clearance over than 20 mL/min. Given the large number of Caucasian patients followed during the entire cisplatin treatment period in our study, our findings reinforce previous suggestions that a less aggressive hydration regimen could be implemented in outpatient units without increasing cisplatin nephrotoxicity. This approach represents a way to decrease medical cost since day hospital care is cheaper than inpatient care [27]. This also could represent a clinical benefit for patients. Cisplatin and carboplatin are two options as first-line therapy in lung cancer [1]. Cisplatin is slightly superior in efficacy to carboplatin [28] but carboplatin may have less toxicity; thus, clinicians must take individual patient factors into consideration when recommending cisplatin or carboplatin. Azuma et al. [29] showed that quality of life score was significantly better in outpatients receiving chemotherapy with short hydration than inpatients receiving the same chemotherapy with long hydration. This observation could lead to recommending carboplatin on quality of life criteria, but our study shows that IV/PO hydration allows clinicians to recommend cisplatin without impairing quality of life.
Conclusion
Based on our retrospective analysis, we showed that the change in cisplatin hydration regimen did not lead to an increasing risk of nephrotoxicity. Thus, this study validates the safety of oral hydration after cisplatin infusion that allows clinicians to administer cisplatin in outpatient units.
References
Masters GA, Temin S, Azzoli CG, Giaccone G, Baker S Jr, Brahmer JR, Ellis PM, Gajra A, Rackear N, Schiller JH, Smith TJ, Strawn JR, Trent D, Johnson DH, American Society of Clinical Oncology Clinical Practice (2015) Systemic therapy for stage IV non–small-cell lung cancer: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol 33(30):3488–3515. https://doi.org/10.1200/JCO.2015.62.1342
Facchetti G, Petrella F, Spaggiari L, Rimoldi I (2017) Malignant pleural mesothelioma: state of the art and advanced cell therapy. Eur J Med Chem 142:266–270. https://doi.org/10.1016/j.ejmech.2017.07.063
Kalemkerian GP (2014) Advances in pharmacotherapy of small cell lung cancer. Expert Opin Pharmacother 15(16):2385–2396. https://doi.org/10.1517/14656566.2014.957180
Miller RP, Tadagavadi RK, Ramesh G, Reeves WB (2010) Mechanisms of cisplatin nephrotoxicity. Toxins 2(11):2490–2518. https://doi.org/10.3390/toxins2112490
Pabla N, Dong Z (2008) Cisplatin nephrotoxicity: mechanisms and renoprotective strategies. Kidney Int 73(9):994–1007. https://doi.org/10.1038/sj.ki.5002786
Oh G-S, Kim H-J, Shen A, Lee SB, Khadka D, Pandit A, So HS (2014) Cisplatin-induced kidney dysfunction and perspectives on improving treatment strategies. Electrolyte Blood Press E BP 12(2):55–65. https://doi.org/10.5049/EBP.2014.12.2.55
Launay-Vacher V, Rey J-B, Isnard-Bagnis C, Deray G, Daouphars M (2008) European Society of Clinical Pharmacy Special Interest Group on Cancer Care. Prevention of cisplatin nephrotoxicity: state of the art and recommendations from the European Society of Clinical Pharmacy Special Interest Group on Cancer Care. Cancer Chemother Pharmacol 61(6):903–909. https://doi.org/10.1007/s00280-008-0711-0
Fukushima K, Okada A, Oe H, Hirasaki M, Hamori M, Nishimura A, Shibata N, Sugioka N (2018 Apr) Pharmacokinetic-pharmacodynamic analysis of cisplatin with hydration and mannitol diuresis: the contribution of urine cisplatin concentration to nephrotoxicity. Eur J Drug Metab Pharmacokinet 43(2):193–203. https://doi.org/10.1007/s13318-017-0436-8
Stewart DJ, Dulberg CS, Mikhael NZ, Redmond MD, Montpetit VA, Goel R (1997) Association of cisplatin nephrotoxicity with patient characteristics and cisplatin administration methods. Cancer Chemother Pharmacol 40(4):293–308. https://doi.org/10.1007/s002800050661
Lavolé A, Danel S, Baudrin L et al (2012) Routine administration of a single dose of cisplatin ≥75mg/m2 after short hydration in an outpatient lung-cancer clinic. Bull Cancer (Paris) (4):43–48. https://doi.org/10.1684/bdc.2012.1555
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of diet in renal disease study group. Ann Intern Med 130(6):461–470
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P (2004) Acute dialysis quality initiative workgroup. Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care Lond Engl 8(4):R204–R212. https://doi.org/10.1186/cc2872
Willox JC, McAllister EJ, Sangster G, Kaye SB (1986) Effects of magnesium supplementation in testicular cancer patients receiving cis-platin: a randomised trial. Br J Cancer 54(1):19–23
Bodnar L, Wcislo G, Gasowska-Bodnar A, Synowiec A, Szarlej-Wcisło K, Szczylik C (2008) Renal protection with magnesium subcarbonate and magnesium sulphate in patients with epithelial ovarian cancer after cisplatin and paclitaxel chemotherapy: a randomised phase II study. Eur J Cancer Oxf Engl 1990 44(17):2608–2614. https://doi.org/10.1016/j.ejca.2008.08.005
Furukawa N, Kawaguchi R, Kobayashi H (2012) Use of high-dose cisplatin with aprepitant in an outpatient setting. Eur J Cancer Care (Engl) 21(4):436–441. https://doi.org/10.1111/j.1365-2354.2011.01284.x
Reece PA, Stafford I, Russell J, Khan M, Gill PG (1987) Creatinine clearance as a predictor of ultrafilterable platinum disposition in cancer patients treated with cisplatin: relationship between peak ultrafilterable platinum plasma levels and nephrotoxicity. J Clin Oncol 5(2):304–309. https://doi.org/10.1200/JCO.1987.5.2.304
Sassier M, Dugué AE, Clarisse B, Lesueur P, Avrillon V, Bizieux-Thaminy A, Auliac JB, Kaluzinski L, Tillon J, Robinet G, le Caer H, Monnet I, Madroszyk A, Boza G, Falchero L, Fournel P, Egenod T, Toffart AC, Leiber N, Do P, Gervais R (2015) Renal insufficiency is the leading cause of double maintenance (bevacizumab and pemetrexed) discontinuation for toxicity to advanced non-small cell lung cancer in real world setting. Lung Cancer 89(2):161–166. https://doi.org/10.1016/j.lungcan.2015.05.005
Madias NE, Harrington JT (1978) Platinum nephrotoxicity. Am J Med 65(2):307–314
Sato K, Watanabe S, Ohtsubo A et al (2016) Nephrotoxicity of cisplatin combination chemotherapy in thoracic malignancy patients with CKD risk factors. BMC Cancer 16(1). https://doi.org/10.1186/s12885-016-2271-8
Tiseo M, Martelli O, Mancuso A, Sormani MP, Bruzzi P, di Salvia R, de Marinis F, Ardizzoni A (2007) Short hydration regimen and nephrotoxicity of intermediate to high-dose cisplatin-based chemotherapy for outpatient treatment in lung cancer and mesothelioma. Tumori 93(2):138–144
Ouchi A, Asano M, Aono K, Watanabe T, Kato T (2014) Comparison of short and continuous hydration regimen in chemotherapy containing intermediate- to high-dose cisplatin. J Oncol 2014:1–4. https://doi.org/10.1155/2014/767652
Yamaguchi T, Uozu S, Isogai S, Hayashi M, Goto Y, Nakanishi T, Imaizumi K (2017) Short hydration regimen with magnesium supplementation prevents cisplatin-induced nephrotoxicity in lung cancer: a retrospective analysis. Support Care Cancer 25(4):1215–1220. https://doi.org/10.1007/s00520-016-3512-8
Hotta K, Takigawa N, Hisamoto-Sato A, Ichihara E, Kudo K, Uchida K, Yanase-Nakamura K, Tanaka H, Kato Y, Tabata M, Tanimoto M, Kiura K (2013) Reappraisal of short-term low-volume hydration in cisplatin-based chemotherapy: results of a prospective feasibility study in advanced lung Cancer in the Okayama Lung Cancer Study Group Trial 1002. Jpn J Clin Oncol 43(11):1115–1123. https://doi.org/10.1093/jjco/hyt128
Ninomiya K, Hotta K, Hisamoto-Sato A, Ichihara E, Gotoda H, Morichika D, Tamura T, Kayatani H, Minami D, Kubo T, Tabata M, Tanimoto M, Kiura K (2016) Short-term low-volume hydration in cisplatin-based chemotherapy for patients with lung cancer: the second prospective feasibility study in the Okayama Lung Cancer Study Group Trial 1201. Int J Clin Oncol 21(1):81–87. https://doi.org/10.1007/s10147-015-0860-1
Horinouchi H, Kubota K, Itani H, Taniyama TK, Nakamichi S, Wakui H, Kanda S, Nokihara H, Yamamoto N, Sekine I, Tamura T (2013) Short hydration in chemotherapy containing cisplatin (>=75 mg/m2) for patients with lung cancer: a prospective study. Jpn J Clin Oncol 43(11):1105–1109. https://doi.org/10.1093/jjco/hyt122
Sato J, Morikawa N, Nitanai H et al (2016) Feasibility study of short hydration using oral rehydration solution in cisplatin including chemotherapy of lung cancer. J Pharm Health Care Sci 2(1). https://doi.org/10.1186/s40780-016-0041-z
Mor V, Stalker MZ, Gralla R, Scher HI, Cimma C, Park D, Flaherty AM, Kiss M, Nelson P, Laliberte L, Schwartz R, Marks PA, Oettgen HF (1988) Day hospital as an alternative to inpatient care for cancer patients: a random assignment trial. J Clin Epidemiol 41(8):771–785
Azzoli CG, Baker S, Temin S et al (2009) American Society of Clinical Oncology Clinical Practice Guideline update on chemotherapy for stage IV non-small-cell lung cancer. J Clin Oncol Off J Am Soc Clin Oncol 27(36):6251–6266. https://doi.org/10.1200/JCO.2009.23.5622
Azuma T, Matayoshi Y, Sato Y, Sato Y, Nagase Y, Oshi M (2016) The safety and effect of chemotherapy with short hydration for urothelial cancer on patients’ quality of life. Jpn J Clin Oncol 46(10):958–963. https://doi.org/10.1093/jjco/hyw097
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was performed in the respect for ethical consideration of research involving human participant. Since it was a retrospective study based on existing data, formal consent is not required.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Puisset, F., Bigay-Game, L., Paludetto, M.N. et al. Safety of oral hydration after cisplatin infusion in an outpatient lung cancer unit. Support Care Cancer 27, 1679–1686 (2019). https://doi.org/10.1007/s00520-018-4415-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4415-7