Abstract
The assessment of constipation symptoms is based on history and physical examination. However, the experience is highly subjective perhaps explaining why palliative medicine doctors continue to use plain abdominal radiographs as part of routine assessment of constipation. Previous studies have demonstrated poor agreement between clinicians with this work in palliative care, limited further by disparity of clinicians’ experience and training. The aim of this work was to explore whether there was less variation in the assessments of faecal shadowing made by more experienced clinicians compared to their less experienced colleagues. This pragmatic study was conducted across six palliative care services in Sydney (NSW, Australia). Doctors of varying clinical experience were asked to independently report their opinions of the amount of shadowing seen on 10 plain abdominal radiographs all taken from cancer patients who self-identified themselves as constipated. There were 46 doctors of varying clinical experience who participated including qualified specialists, doctors in specialist training and lastly, doctors in their second- and third post-graduate years. Poor agreement was seen between the faecal shadowing scores allocated by doctors of similar experience and training (Fleiss’s kappa (FK): RMO 0.05; registrar 0.06; specialist 0.11). Further, when the levels of agreement between groups were considered, no statistically significant differences were observed. Although the doctors did not agree on the appearance of the film, the majority felt they were able to extrapolate patients’ experiences from the radiograph’s appearance. As it remains challenging in palliative care to objectively assess and diagnose constipation by history and imaging, uniform and objective assessment and diagnostic criteria are required. It is likely that any agreed criteria will include a combination of imaging and history. The results suggest the use of radiographs alone to diagnose and assess constipation in palliative care represents low value care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Recommended approaches to diagnosing constipation include a detailed patient assessment focusing on changes in bowel habits, identification of potentially contributing factors and physical examination [1]. A history of infrequent stools, hard stools that are difficult to pass; excessive straining, feeling of incomplete evacuation, or use of manual manoeuvres should be sufficient to establish the diagnosis [2]. In reality, it is often more complicated. People’s experiences are highly subjective [3] with diary studies demonstrating that individual’s recall of the frequency of their bowel movements is often poor [4]. Additionally, clinicians do not universally agree on symptoms or criteria which might lead to a diagnosis of constipation [5]. These uncertainties reiterate the importance of objective approaches to assess and diagnose constipation.
In gastroenterology, this issue has been addressed by the universally accepted gold-standard diagnostic criteria, the symptom-based Rome criteria [6]. A similar agreement in palliative care is lacking [7]. This gap may explain why some palliative care guidelines still recommendation a role for abdominal radiographs in the assessment and diagnosis of constipation in some situations [8, 9]. These recommendations are in contrast to constipation assessment in other populations where radiographs are no longer routinely recommended [10, 11].
In the general population, estimates suggest that up to 30% of people experience constipation symptoms. In contrast, up to 85% of palliative care patients will experience bowel symptoms at one or more points in their disease trajectory [12, 13]. There are likely to be numerous factors that affect the bowel including a past history of functional constipation; medications; disorders of the endocrine system (hypothyroidism, long term diabetes mellitus); metabolic abnormalities (hypercalcemia or hypocalcemia, hypokalemia, renal impairment and under hydration), neuropathic or myopathic pathologies; reduced mobility and mechanical or pseudo-obstructions [14, 15]. Aside from opioids [2, 16] and possibly anti-cholinergic load [17, 18], the actual clinical effects of other factors on the gut and its supporting structures have not been extensively studied in palliative care. These knowledge deficits complicate the assessment and diagnosis of constipation and provide an explanation for why palliative care clinicians continue to rely on radiographs.
However, there is a lack of objective evidence to support this test’s diagnostic accuracy for this purpose. Acknowledging this, a recent study was undertaken to explore the role for plain abdominal radiographs in the assessment of constipation in palliative care patients [19]. This research by Clark et al. was based on work previously undertaken in functionally constipated patients [20]. The results demonstrated poor levels of agreement between palliative care clinicians’ reports with no relationship seen between reports of faecal shadowing and the patient’s self-assessed symptoms [19]. An acknowledged limitation of this work was that the four participating clinicians possessed differing levels of clinical experience.
This current study was undertaken with the aim of exploring if the level of a clinician’s training and experience affected the levels of agreement when palliative care practitioners were asked to report their assessments of the degree of faecal shadowing visible on plain abdominal radiographs in palliative care patients who had identified themselves as constipated.
Aim
To explore whether there was less variation in the assessments of faecal shadowing made by more experienced clinicians compared to their less experienced colleagues.
Methods
Study design and setting
A pragmatic observational study was undertaken with the aim of comparing the radiology reports voluntarily made by doctors of varying clinical experience working in palliative care settings.
Settings and participants
Doctors from six palliative care services across New South Wales (Australia) were approached to participate. With the approval of their respective institution’s human research ethics committees, a convenience sample of palliative care doctors of varying experience was recruited including palliative medicine specialists (consultants), registrars (fellows; postgraduate years three or more) and Resident Medical Officers (RMO) (house staff; postgraduate year two or three).
In an Australian context, a palliative medicine specialist is a doctor who is recognised as a fellow of the Royal Australasian College of Physician’s Chapter of Palliative Medicine [21]. Registrars are medical practitioners who are undertaking an accredited course of study leading to a higher medical qualification. Resident medical officers are usually within their second or subsequent years of practical experience after eligibility for full registration as a medical practitioner prior to progressing to further training [22].
Data collection
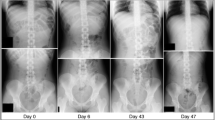
Each of the consenting doctors individually and without consultation reviewed 10 abdominal radiographs, blinded to any clinical details. This was done in order not to influence the doctors’ reports. The participating doctors were asked to provide their assessments of the amount of faecal shadowing they observed in the three sections of the colon, namely the right colon, left colon and sigmoid colon. This was undertaken according to previously published recommendations which require a 0–5 score to be assigned for each colonic section where 0 = no shadowing and 5 = severe shadowing with dilated bowel. The scores of each section are totalled to give a final numerical score of between 0 and 15 with higher scores reflective of more shadowing [23].
Based on these scores, the clinicians were then asked to assess the degree that they were able to predict the problems might be experiencing based on the appearance of the radiograph.
These 10 radiographs were previously taken from consenting patients with advanced cancers who had self-identified themselves as constipated and requiring regular laxatives.
Analysis
De-identified demographic details and clinician’s opinions regarding the use of radiographs were summarised using summary statistics. Fleiss’s kappa (FK) was used to evaluate concordance between multiple raters within each group with this technique evaluating the reliability of agreement amongst greater than one rater, with 0–0.2 reflecting a slight association and 0.8–1 reflecting almost perfect agreement. The regression co-efficient was calculated for pair-wise comparisons amongst groups. This was performed with the registrar as the reference group and included Specialists versus Registrars as well as RMOs vs Registrars. Lastly, a two by two table was constructed to explore the degree to which doctors felt they could extrapolate from the radiograph appearance the clinical experience of each subject’s experience.
Results
Demographics
The demographics of the patients whose abdominal radiographs were used in this study are detailed in Table 1 and the demographics of the 46 participating doctors are summarised in Table 2. Of the latter group, over half of these doctors (62%, n = 28) were women with nearly half less than 35 years of age (n = 19). There were similar numbers of participants in each of the three groups by level of experience.
Agreement regarding the degree of faecal shadowing within and between sub-groups
As is summarised in Table 3, poor agreement was seen between the faecal shadowing scores allocated by doctors of similar experience and training. Further, when the levels of agreement between RMOs and registrars were compared, and when the levels of agreement between specialists and registrars were compared, no real differences were seen (Table 4).
Doctors perceived diagnostic value of the radiographs
For each radiograph, the doctors were asked to comment about whether the radiological features present allowed them to diagnose constipation (yes/no); and predict a patient’s symptoms (yes/no) based on the appearance of the abdominal film. The results suggest that if a doctor believed that a patient was likely to be constipated based on the radiograph, the doctor was more likely to feel confident that they could predict symptoms based on the appearance of the radiograph (OR 96.5) (Table 5).
Discussion
The ability to diagnose and manage constipation is considered a core component of palliative care doctors’ clinical practice. Currently, the use of radiographs to assess this issue is clinically widespread and in fact, recommended in clinical guidelines. These observations highlight the real need to understand the reliability and repeatability of this investigation.
The alternative hypothesis that the concordance between more experienced clinicians’ assessments of degrees of faecal shadowing on abdominal radiographs would differ from that of more junior staff was not upheld. The study’s results suggest only faint levels of agreement amongst the most experienced doctors with this lack of agreement also apparent in the other two groups of less experienced clinicians. When the levels of agreement seen within each group were compared, no differences were seen. From this work, it seems that experience appears to have no impact on palliative care clinicians’ assessments of the degrees of faecal shadowing on abdominal radiographs in advanced cancer patients who were all constipated.
These findings compare and contrast with other work that has been conducted to document the degree of agreement amongst clinicians reporting radiographs in other settings [24,24,25,27]. In one such study, specialists, registrars and RMO’s were asked to report chest radiographs with the main finding on these films being a pneumothorax. There were significant differences in diagnostic accuracy between the groups with the study concluding that the skill of interpretation of radiographs increases with experience [24]. However, the major difference between the pneumothorax study and the one presented here is that unlike a radiological diagnosis of a pneumothorax, there are no agreed criteria to diagnose constipation on plain films. The only exception to this is when plain radiographs are combined with radio-opaque markers to assess whether colon transit times are prolonged based on the number of markers visible, not the appearance of shadowing [28].
Even though the clinicians were not reliably able to agree on the extent of visible shadowing, many still felt that they could both establish a diagnosis of constipation and predict specific symptoms, e.g. cramping or bloating based on the appearance of the radiograph. This observation confirms the widespread belief that there is a high concordance between clinical and radiographic constipation. This raises a number of issues which include the observation that the sensitivity and specificity of plain radiographs to diagnose constipation in palliative care has not previously been examined and is unlikely to change in the near future given the ongoing absence of gold standard diagnostic criteria for constipation in palliative care. Further, while clinicians felt that they were able to predict patient’s symptoms based on the radiograph’s appearance, previous studies have failed to correlate radiographs with patient’s objective symptoms [20] including studies involving palliative populations [19, 29].
Continued reliance on radiographs raises the possibility of search-satisficing bias and confirmation bias. Search-satisficing bias is most simply defined as the action of calling off a search once a clinician believes they have a positive result, whereas confirmation bias refers to a situation when the clinician has an initial or a preconceived idea about a problem and interprets subsequent information to confirm the diagnoses [30]. A patient presenting with cramping pain and based on their assessment of moderate shadowing on abdominal radiograph may lead the clinician to end the decision-making process and conclude that constipation is the diagnosis. However, this could be erroneous given the variability seen between clinicians’ reports, the lack of objective diagnostic criteria and the fact that a plain radiograph is taken at single time point with many factors influencing its appearance.
Reliance on a test of unproven value potentially exposes patients to harm and increases health care costs. This may be either in the form of unnecessary investigations or the possibility of either over- or under-treatment or missed diagnoses. Within current evidence in palliative care, the use of radiographs to assess constipation is an example of low-value health care [31], an issue that has been raised in other parts of medicine. Systematic reviews have highlighted that the evidence to support plain radiographs as a useful tool to assess childhood constipation is insufficient and this practice is seen as over-utilisation of an investigation that is potentially detrimental not only to patients but health care systems as well [11].
Strengths of this study include that this is the only study that has compared the opinions of a reasonable number of palliative care doctors drawn from different stages of experience to document the level of agreement when radiographs are reported when the main issue is the assessment of constipation. As such, this work has highlighted that before radiographs can be accepted as a validated tool in the assessment of constipation in palliative care, more work is required. Another strength is that the abdominal radiographs are taken from patients with advanced malignancy so would represent the palliative care patient population in whom this investigation is likely to be done.
The weaknesses of this work include the fact that it was a small, pragmatic study. Clinicians were not provided with patient histories, a deliberate choice in order not to influence the final reports. This is despite the fact that there is likely to be merit in providing clinical information in order to improve the diagnostic accuracy of investigations [32]. The decision not to include history was considered pivotal to the study as the aim was to compare the agreement between clinicians’ assessments of visible faecal shadowing. It is important that this be highly consistent if the premise is accepted that a plain abdominal radiograph can be used to diagnose constipation. However, all the patients had symptomatic constipation meaning that no radiographs were included from non-constipated patients to act as distractors. Another weakness is that the scores of the palliative medicine doctors were not compared with radiologists. In many clinical settings, it is necessary for doctors to have the necessary skills and expertise to act upon investigations. In addition, although future studies will include radiologists, it is also of note that other studies have included such experts with no improvement in agreement [20, 33]. Finally, the impact of clinician bias on the results cannot be ignored. This may have impacted the results in a number of ways including embedded ways of thinking or disparate learning experiences.
Future work
This study is not claiming plain abdominal radiographs have no role in palliative care. It is however suggesting that even with the limitations of this work, relying on a plain radiographs appearance to assess and manage constipation requires much more consideration. Comprehensive history and physical examination is required [9] with radiographs imperative to exclude bowel obstruction, gut perforation, volvulus or paralytic ileus. It may be in the future possible to readdress whether plain radiographs provide important information to help palliative care clinicians to assess and manage their patients’ constipation symptoms. However, this requires, at the very minimum, development and testing of an agreed diagnostic gold standard against which to assess the specificity and positive predictive capacity of plain radiographs.
Conclusion
As it remains challenging in palliative care to objectively assess and diagnose constipation by history and imaging, uniform and objective assessment and diagnostic criteria are required. It is likely that any agreed criteria will include a combination of imaging and history. The considerable variation between observers seen in this work when assessing faecal loading and the previously identified poor correlation of faecal loading with objective assessments of constipation such as colon transit time suggest that plain radiographs are not a sufficiently reliable method of diagnosing constipation. However, this must not preclude the use of radiographs in specific situations.
References
Tian H, Ding C, Gong J, Ge X, McFarland LV, Gu L, Chen Q, Ma C, Zhu W, Li J, Li N (2016) An appraisal of clinical practice guidelines for constipation: a right attitude towards to guidelines. BMC Gastroenterol 16(1):52. https://doi.org/10.1186/s12876-016-0466-8
Wald A (2016) Constipation: advances in diagnosis and treatment. JAMA 315(2):185–191. https://doi.org/10.1001/jama.2015.16994
Alame AM, Bahna H (2012) Evaluation of constipation. Clin Colon Rectal Surg 25(1):5–11. https://doi.org/10.1055/s-0032-1301753
Bharucha AE, Seide BM, Zinsmeister AR, Melton LJ 3rd (2008) Insights into normal and disordered bowel habits from bowel diaries. Am J Gastroenterol 103(3):692–698. https://doi.org/10.1111/j.1572-0241.2007.01631.x
Herz MJ, Kahan E, Zalevski S, Aframian R, Kuznitz D, Reichman S (1996) Constipation: a different entity for patients and doctors. Fam Pract 13(2):156–159
Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC (2006) Functional bowel disorders. Gastroenterology 130(5):1480–1491. https://doi.org/10.1053/j.gastro.2005.11.061
Clark K, Currow DC (2013) Constipation in palliative care: what do we use as definitions and outcome measures? J Pain Symptom Manag 45(4):753–762. https://doi.org/10.1016/j.jpainsymman.2012.03.016
Anon (2010) Tasmanian Goverment. http://www.dhhs.tas.gov.au/__data/assets/pdf_file/0003/36939/Care_Management_Guidelines_-_Constipation_-_20160622.pdf. Accessed 17th July 2017
Larkin PJ, Sykes NP, Centeno C, Ellershaw JE, Elsner F, Eugene B, Gootjes JR, Nabal M, Noguera A, Ripamonti C, Zucco F, Zuurmond WW, European Consensus Group on Constipation in Palliative C (2008) The management of constipation in palliative care: clinical practice recommendations. Palliat Med 22(7):796–807. https://doi.org/10.1177/0269216308096908
Bharucha AE, Dorn SD, Lembo A, Pressman A (2013) American Gastroenterological Association medical position statement on constipation. Gastroenterology 144(1):211–217. https://doi.org/10.1053/j.gastro.2012.10.029
Ferguson CC, Gray MP, Diaz M, Boyd KP (2017) Reducing unnecessary imaging for patients with constipation in the pediatric emergency department. Pediatrics 140:e20162290. https://doi.org/10.1542/peds.2016-2290
Kamal AH, Nipp RD, Bull J, Stinson CS, Abernethy AP (2015) Symptom burden and performance status among community-dwelling patients with serious illness. J Palliat Med 18(6):542–544. https://doi.org/10.1089/jpm.2014.0381
Clark K, Smith JM, Currow DC (2012) The prevalence of bowel problems reported in a palliative care population. J Pain Symptom Manag 43(6):993–1000. https://doi.org/10.1016/j.jpainsymman.2011.07.015
Connolly M, Larkin P (2012) Managing constipation: a focus on care and treatment in the palliative setting. Br J Community Nurs 17(2):60, 62–64, 66-67. https://doi.org/10.12968/bjcn.2012.17.2.60
Basilisco G, Coletta M (2013) Chronic constipation: a critical review. Dig Liver Dis 45(11):886–893. https://doi.org/10.1016/j.dld.2013.03.016
Sykes NP (1996) An investigation of the ability of oral naloxone to correct opioid-related constipation in patients with advanced cancer. Palliat Med 10(2):135–144. https://doi.org/10.1177/026921639601000208
Clark K, Lam L, Currow DC, Agar M (2014) A prospective study to investigate contributory factors that lead to constipation in palliative care patients. Journal of Pain & Symptom Management 47(6):e1–e4. https://doi.org/10.1016/j.jpainsymman.2014.01.005
Clark K, Lam LT, Agar M, Chye R, Currow DC (2010) The impact of opioids, anticholinergic medications and disease progression on the prescription of laxatives in hospitalized palliative care patients: a retrospective analysis. Palliat Med 24(4):410–418. https://doi.org/10.1177/0269216310363649
Clark K, Lam LT, Talley NJ, Quinn J, Blight A, Byfieldt N, Currow DC (2016) Assessing the presence and severity of constipation with plain radiographs in constipated palliative care patients. J Palliat Med 19(6):617–621. https://doi.org/10.1089/jpm.2015.0451
Cowlam S, Vinayagam R, Khan U, Marsden S, Minty I, Moncur P, Bain I, Yiannakou YJ (2008) Blinded comparison of faecal loading on plain radiography versus radio-opaque marker transit studies in the assessment of constipation. Clin Radiol 63(12):1326–1331. https://doi.org/10.1016/j.crad.2008.06.011
AIHW (2012) Palliative care services in Australia 2012. Australian Institue of Health and Welfare Canberra
AMA (2010) Becoming a doctor. Australian medical association Accessed 23rd July 2017
Leech SC, McHugh K, Sullivan PB (1999) Evaluation of a method of assessing faecal loading on plain abdominal radiographs in children. Pediatr Radiol 29(4):255–258. https://doi.org/10.1007/s002470050583
Kelly BS, Rainford LA, Darcy SP, Kavanagh EC, RJ Toomey (2016) The development of expertise in radiology: in chest radiograph interpretation, “expert” search pattern may predate “expert” levels of diagnostic accuracy for pneumothorax identification. Radiology 280
Henriksson L, Sundin A, Smedby O, Albrektsson P (1990) Assessment of congestive heart failure in chest radiographs. Observer performance with two common film-screen systems. Acta Radiol 31(5):469–471
Tudor GR, Finlay D, Taub N (1997) An assessment of inter-observer agreement and accuracy when reporting plain radiographs. Clin Radiol 52(3):235–238
Test M, Shah SS, Monuteaux M, Ambroggio L, Lee EY, Markowitz RI, Bixby S, Diperna S, Servaes S, Hellinger JC, Neuman MI (2013) Impact of clinical history on chest radiograph interpretation. J Hosp Med 8(7):359–364. https://doi.org/10.1002/jhm.1991
Rao SS, Camilleri M, Hasler WL, Maurer AH, Parkman HP, Saad R, Scott MS, Simren M, Soffer E, Szarka L (2011) Evaluation of gastrointestinal transit in clinical practice: position paper of the American and European Neurogastroenterology and Motility Societies. Neurogastroenterol Motil 23(1):8–23
Nagaviroj K, Yong WC, Fassbender K, Zhu G, Oneschuk D (2011) Comparison of the constipation assessment scale and plain abdominal radiography in the assessment of constipation in advanced cancer patients. J Pain Symptom Manag 42(2):222–228. https://doi.org/10.1016/j.jpainsymman.2010.11.019
Pines JM (2006) Profiles in patient safety: confirmation bias in emergency medicine. Acad Emerg Med 13(1):90–94. https://doi.org/10.1197/j.aem.2005.07.028
Cassel CK, Guest JA (2012) Choosing wisely: helping physicians and patients make smart decisions about their care. JAMA 307(17):1801–1802
Loy CT, Irwig L (2004) Accuracy of diagnostic tests read with and without clinical information: a systematic review. JAMA 292(13):1602–1609
Kokke FT, Sittig JS, de Bruijn A, Wiersma T, Van Rijn RR, Limpen JL, Houwen RH, Fischer K, Benninga MA (2010) Starreveld scoring method in diagnosing childhood constipation. Pediatr Radiol 40(11):1789–1793. https://doi.org/10.1007/s00247-010-1725-4
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Clark, K., Lam, L., Talley, N.J. et al. A pragmatic comparative study of palliative care clinician’s reports of the degree of shadowing visible on plain abdominal radiographs. Support Care Cancer 26, 3749–3754 (2018). https://doi.org/10.1007/s00520-018-4238-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4238-6