Abstract
Purpose
In recent years, a greater emphasis has been placed on shared decision-making (SDM) techniques between providers and patients with the goal of helping patients make informed decisions about their care and subsequently to improve patient health outcomes. Previous research has shown variability in treatment decision-making among patients with colorectal cancer (CRC), and there is little comprehensive information available to help explain this variability. Thus, the purpose of this study was to evaluate the current state of the literature on factors that are influential in treatment decision-making among patients with CRC.
Method
A priori search terms using Boolean connectors were used to examine PubMed, PsycINFO, Web of Science, CINAHL, and MEDLINE for relevant studies. Eligibility criteria for inclusion in the study included patients with CRC and examination of influences on CRC treatment decision-making. All relevant data were extracted including, author, title and year, study methodology, and study results.
Results
Findings (n = 13) yielded influences in four areas: informational, patient treatment goals, patient role preferences, and relationship with provider. Quality of life and trust in physician were rated a high priority among patients when making decisions between different therapeutic options. Several studies found that patients wanted to be informed and involved but did not necessarily want to make autonomous treatment choices, with many preferring a more passive role.
Conclusions
Providers who initiate a dialog to better understand their patients’ treatment goals can establish rapport, increase patient understanding of treatment options, and help patients assume their desired role in their decision-making. Overall, there were a small number of studies that met all inclusion criteria with most used a cross-sectional design.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the third most commonly diagnosed form of cancer and the third leading cause of cancer death [17]. The 5-year survival rate as of 2005–2011 for patients with a CRC diagnosis is 64.9%. African Americans had higher mortality from colon cancer after controlling for sex, age, tumor stage, and grade [12]. For patients with a CRC diagnosis, the initial treatment for the majority without metastatic disease is complete surgical resection of the tumor [17, 34]. However, this varies for patients who have a colon cancer diagnosis versus a rectal cancer diagnosis such that patients in the latter group may begin treatment with radiation. Patient decision-making becomes critical following surgery when decisions must be made related to adjuvant chemotherapy. The decision to have adjuvant chemotherapy is complex and includes factors such as the patient’s disease staging, personal preferences, tumor type and characteristics, and other medical findings [34].
There are known differences in the quality and completion of treatment and that this varies significantly among patients of different sociodemographic groups and is influenced by patient knowledge, attitudes, and cultural beliefs. Previous findings show that Black patients are significantly less likely to receive adjuvant chemotherapy and that these differences are the highest among patients ages 66 to 70 [6]. Berry et al. (2009) found that there were patient, provider, and environmental factors that accounted for approximately 50% of the treatment disparity among this age group [5]. Among patients with high-risk stage II colon cancer, adherence to recommended treatment (i.e., surgery and adjuvant chemotherapy) was low (i.e., 36%). This was the highest for recommended adjuvant chemotherapy among patients who were older with comorbidities [8].
Patients often rely heavily on the recommendation of their providers. However, providers and patients often struggle with balancing the benefits of adjuvant chemotherapy with the risks which are often difficult for patients to fully understand or anticipate [24]. Patients’ decisions about how they proceed with treatment may be driven by various factors which may be different than their provider’s. Additionally, following diagnosis, patients also experience a substantial amount of psychosocial stress, making it even more difficult to comprehend the full volume of information related to their diagnosis, prognosis, and treatment options. As a result, patients may not be adequately equipped to make informed decisions about their care [2]. There are also numerous different factors at the individual, relationship, and systematic levels that may influence clinical decisions made by patients [23, 32].
The reasons behind variations in the uptake, quality, and completion of treatment are not well understood or documented among patients with colorectal cancer. However, over the last decade, there has been an increase in the amount of research dedicated to gaining a greater understanding of the patient-level, provider-level, and environmental influences on how patients make decisions regarding their cancer care. There has yet to be a synthesis of findings related to these influences among patient populations with CRC. Thus, the aim of this review was to evaluate the current state of the literature and synthesize current findings related to factors, which influence treatment decision-making among patients with CRC.
Method
A review of the scientific literature on treatment decision-making in CRC patients was conducted from December 2015–February 2016 in adherence with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [22].
Databases
The following databases were systematically searched for articles: PubMed, PsycINFO, Web of Science, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and MEDLINE. The searches were not limited by date, country of origin, or original published language.
Search
The following search terms were generated and connected using the Boolean search term “OR” in each database: “colorectal cancer,” “colon cancer,” “rectal cancer” and “AND” “decision making,” “medical decision making,” “informed decision making,” “treatment decision making,” and “hared decision making.” Given that this review was solely focused on influences on CRC treatment decision-making, the literature search was limited by also including the use of the Boolean term “NOT” in conjunction with the terms “screening” and “cancer screening” with each search term permutation listed above.
Study selection process
All retrieved studies were evaluated by title followed by a review of the abstract in order to determine whether full text review was necessary. All published studies from the targeted literary databases that met the designated inclusion criteria were included in the review: the study population must have been comprised of adults (18 years of age or older) with a CRC (i.e., cancer of the colon, rectum, or rectosigmoid junction) diagnosis. Studies that included patients with other cancer diagnoses (e.g., breast) were included in the analysis only if the authors provided sufficient subgroup information regarding patients with a CRC diagnosis. No other limitations were placed on study samples. Both qualitative and quantitative study designs were included. Both domestic and international studies were included if English translations were available.
Data extraction process
All relevant data elements were extracted from each article that was included in the review. Extracted data included author, title and year that the study was published, country of publication, demographic characteristics of the study sample, study methodology, and primary study results.
Results
Search results
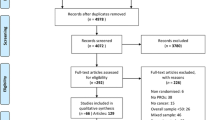
A search of the five databases yielded 2242 citations. Most titles were excluded because the study was on a topic that did not match the inclusion criteria for the review. Several studies investigated clinical decision-making methods (e.g., benefit of one therapeutic method versus another). Abstract reviews of 116 records resulted in 39 citations for full-paper review. As with the title review, the majority of excluded abstracts were studies based on clinical decision-making. Duplicates were also excluded at this stage. At the final stage of the selection process, 13 studies were ultimately included in the review. If the authors did not distinguish the results by cancer type, the study was excluded. Studies were also included if the sample population was made up of health care providers or considered the provider’s perspective on treatment decision-making. Included studies’ dates ranged from 1999 to 2015. Figure 1 illustrates the study selection process.
Participant and study characteristics
A total of 2237 participants were involved in the included studies. The majority (82.9%; n = 1855) of participants were patients with a CRC diagnosis. One study combined cancer types (i.e., breast and CRC) [1]. Patients with metastatic CRC accounted for 8% (n = 180) of the review population [13, 15].
Both qualitative and quantitative study designs were included in the review. Cross-sectional methodology was used most frequently (6/13 studies) [1, 2, 15, 18, 27, 31]. One study utilized a prospective, randomized controlled trial design [16] and one study used a prospective cohort study design [21]. Three studies used mixed methods, utilizing both qualitative interviews and cross-sectional survey techniques [28]. Several studies utilized a qualitative methodology (5/13) [13, 25, 26, 29]. Additional study details are displayed in Table 1.
Synthesis of results
The purpose of this review was to examine the literature on patient-level influences on treatment decision-making among patients with CRC. We chose to conduct a scoping review style of analysis, interpretation, and synthesizing of results [11, 20]. Commonalities among included studies were examined and grouped into thematic areas to represent the overarching tends present in the research. The results from this review yielded the following themes: (1) informational influences, (2) patient role and participation, (3) patient-level treatment goals, and (4) relationship and communication with providers. The distributions of included studies by thematic area are presented in Table 2.
Informational influences
Eight studies (62%) examined influences related to the type of information and method of delivery on patient treatment decision-making [1, 2, 4, 13, 15, 18, 26, 27]. The majority of studies used a cross-sectional study design with the exception of Sahay et al. (2000) and Beaver et al. (2005), which both utilized qualitative methodology [4, 26]. The type of information and method of delivery by physicians to patients was a commonly investigated theme. Several studies concluded that the way information is described to patients, including treatment options, potential side effects, and treatment regimens can influence how a patient arrives at a treatment decision [15, 18], satisfaction with their treatment decision, and subsequent adherence. Beaver and colleagues (2009) found that patients had a greater understanding of written information as opposed to verbal information given to them by providers [2]. However, it seems that the written information was most useful when used in conjunction with verbal information. Additionally, its usefulness increased when the written information reflected the verbal information provided by the physician. Previous research has indicated that depending on the conditions during the clinical encounter, patients forget 40–80% of the information presented to them almost immediately [19]. This might be especially important for patients who do not have a caregiver present during a clinical encounter.
With the increased availability of modern technology and methods for researching health information, more attention is being given to how and where patients access health information. One cross-sectional study [27] considered informational influences in the context of Internet searches among CRC patients. This study found that patients used basic search engines when researching medical information related to their treatment options. The search engines directed patients to websites and articles that may not have had accurate information or may have had information presented in a way that only brought more confusion to the patient. Findings showed that 59% of patients rated that the information they found during their Internet searches as unhelpful. Furthermore, an overwhelming number of patients (97%) were satisfied with the amount of information provided by their physicians, and they were found to be more dependent on the information from their medical care team than the information they sought on their own via the internet [27].
Patient role and participation
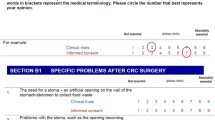
Several studies (8/13; 61.5%) investigated the influence of both patient and provider viewpoints towards the patient role in treatment decision-making [1, 2, 4, 13, 15, 18, 26, 27]. Several studies utilized the Control Preferences Scale (CPS) [10] to assess patient preferences for involvement in treatment decision-making [1, 13, 24, 28]. The CPS uses five statements that are indicative of an active, collaborative, or passive patient role. Among those studies that used the CPS, patients preferred a more passive role in decision-making and preferred that providers make the treatment decisions [1, 13, 18]. Beaver and colleagues (1999) found significant differences in the number of CRC patients that preferred a passive role (78%) compared with patients with breast cancer (52%) [2]. However, gender was not taken into consideration, in that the authors compared the frequency of role preferences as cancer groups, rather than demographic groups. Given that previous research has shown that women generally tend to prefer more collaborative decision-making, this could have potentially influenced these estimates [30].
Some studies found that patient involvement in treatment planning and decision-making was related to patients’ understanding of their diagnosis [25, 26]. Qualitative findings showed that patient experiences and perceptions related to participation in medical decision-making were mostly compliant in nature with two variations: (1) complying with participation and (2) complying without participation. Complying with participation included patient expressions of trust, self-confidence, competence in decision-making, and open dialog with providers. Compliance without participation was characterized as patients feeling that they lacked the ability to understand the information being presented to them and therefore could not effectively make treatment decisions [25]. Sahay et al. (2000) had a complementary finding among participants in their study that more information may have helped patients feel like they could be more active in the decision-making process. Findings showed that over time, patients began to realize that they did have a choice in their treatment and they began to ask more questions, when earlier in the process they had been more reserved [26].
Patient-level treatment goals
A small percentage of the studies in this review (3/13; 23.1%) considered patient goals as potential influences on their treatment decision-making process [16, 18, 28] A common theme among these studies was that patients placed great importance on QOL when considering treatment options. Hofmann et al. (2012) found that both healthy individuals and patients with CRC put greater emphasis on QOL outcomes (e.g., less negative side effects) versus reoccurrence rates when considering adjuvant treatment options [16]. A commonly reported goal of patients following treatment was “getting on with life” whereas disease reoccurrence was less frequently reported [28]. Patients were more concerned with moving past this event in their life and resuming a perceived normalcy (e.g., life prior to diagnosis). Among patients with recurrent disease, past experiences with treatment regimens played an influential role in patient treatment preferences [15]. Fu et al. (2015) found that patients were less willing to tolerate more common side effects (e.g., nausea, pain, fatigue) when considering treatment options compared to more clinically serious adverse events (e.g., heart attack, stroke). These findings also point towards a greater emphasis on the importance of daily QOL [15].
One study considered age group differences in influences on treatment decision-making [13, 18]. Jorgensen et al. (2013) found that both older (i.e., ≥65 years) and younger (i.e., <65 years) patients placed high importance on lowering their risk of reoccurrence and trust in their physician when considering their treatment options [18]. Additionally, “fear of dying” was rated highly among older patients which was unique in that fear of death is typically not shown in older populations and is more commonly reported as an influential factor in their decision to have chemotherapy [18].
Relationship and communication with provider
Several studies (5/13; 38.5%) considered provider-level influences on treatment decision-making among patients with CRC [2, 7, 18, 26, 28]. Previous research has indicated that providers believe that it is often difficult to explain all of the potential treatment options to patients because the information is too complex and clinical time too limited [3]. A couple studies (2/13; 15.3%) suggested that there is dissonance between health care providers acknowledging the importance of SDM and providers engaging in SDM practices with their patients. Elkin and colleagues (2007) found physician-patient role concordance to be only 44%. Physicians were shown to be more accurate in identifying patients who preferred a more passive role than those who preferred an active or collaborative role. This results in providers engaging with patients in ways that do not facilitate the desired level of SDM [13]. There is also evidence to suggest that patients do not feel like they can participate in decision-making because they feel they lack necessary knowledge, the provider is too busy to answer questions, or that they are not supposed to (even though there is a desire to be more active) [29].
The process of building rapport with patients is multifaceted. Facilitating open communication with patients regarding information related to their cancer diagnosis not only builds rapport and promotes information exchange but also empowers patients to ask questions and increases feelings of self-efficacy for the patient [9, 14]. Beaver and colleagues (2009) found 83.5% of patients indicated that talking to nursing staff helped them make sense of the information given by their doctor [2]. Results of this nature indicate that providers may not be adequately communicating information. Issues around communication may be due to limited time on part of the physician to counsel the patient or issues in the way the information is presented to the patient. Trust in provider was an influential factor for patients when considering treatment options [18, 28]. Jorgensen and colleagues (2013) found that trust in physician was an important factor when considering whether to have adjuvant chemotherapy following surgery among both younger and older patients [18]. Salkeld and colleagues (2004) echoed these findings that patients placed trust in the surgeon as the most important factor when considering treatment options. Trust was built on both a perceived expertise and that their surgeon was genuinely concerned about the patient’s well-being [28].
Discussion
Summary of evidence
The purpose of this review was to organize and evaluate the current state of the literature related to the factors of influence on treatment decision-making among patients with CRC. A review of the literature yielded 13 studies that were ultimately retained in the review. Findings showed informational influences could be categorized into four overall themes: (1) informational, (2) patient role and participation, (3) patient-level treatment goals, and (4) relationship and communication with provider.
For most patients with non-advanced CRC, the first decision-making point during treatment is whether they should seek a surgical treatment option. However previous research has shown that neither patients nor physicians believe this to be a decision point [4]. For providers, it is not generally considered to be an option, even though patients do have the ability to refuse surgery. It was often described as a required step towards survival and therefore not seen as being within the realm of choice for patients [4]. Patients often believed that there was a “right” choice to be made in regard to their cancer care and, as a result, believed that surgery was the “right” first step. Many of the patient narratives presented by Beaver et al. (2005) describe a disbelief that they had any options in order to engage in a decision-making process until after surgery [4]. Even though surgery is often the necessary first step, it can be argued that because patients do not see this as the most prominent medical decision-making point, a more pivotal point would involve post-surgical therapies.
There was a significant lack of published data considering the impact of both functional and health literacy on patient treatment decision-making. Only one study considered the impact of health literacy on adjuvant chemotherapy uptake among patients with CRC [7]. Busch et al. (2015) found that patients with lower reported health literacy were generally less likely to receive chemotherapy [7]. Furthermore, among patients with stage III CRC, for which adjuvant chemotherapy is a universally recommended treatment, those patients who were considered to be more health literate had a higher rate of adjuvant chemotherapy uptake. Additionally, it has been suggested that patients with lower levels of health literacy are more likely to prefer a more passive role in decision-making [7]. Research has also indicated health literacy as the pathway though which education impacts patient self-reported health status [33]. Other studies considered education level as a potential mediator; however, these results were non-significant [13].
Providing written information can address inconsistencies with how treatment-related information is described to patients. Sahay and colleagues (2000) found that patients had false impressions regarding their diagnosis and treatment options even after speaking with providers [26]. During qualitative interviews, one patient reported feeling shocked when she was diagnosed with recurrent disease because she believed her treatment was curative. The patient reported never knowing that reoccurrence was possible. Elkin and colleagues (2007) found that patients had overestimated expectations regarding the curative nature of chemotherapy and researchers believed that this finding could be attributed to patients’ selective memory during their clinical encounter [13]. Patients often had expectations that chemotherapy would be curative for advanced stage CRC when treatment was defined as palliative in nature [13]. Additionally, patients who sought more information regarding their prognosis were both more likely to receive it and also had an increased likelihood to have more realistic expectations regarding treatment efficacy [13]. Many studies highlighted that patients were satisfied with the amount of information given to them by their providers [27]. However, it is important to note that just because patients are satisfied with the amount of information provided does not mean that patients are satisfied with how it was presented. Additionally, this does not reflect the accuracy or amount of information that patients actually understand.
There are numerous implications from the findings of this review. Providers should consider that a patient who appears to be unengaged during a clinical encounter does not equate to a lack of personal responsibility for their health status. In these circumstances, additional steps should be taken by the provider to ensure that the patient understands the information being presented to them and encouraging them to ask any questions they may have. Clinically, findings from this review could have implications at both the provider and patient level. By increasing rapport and creating more effective methods for communicating information regarding treatment, patients may be more likely to adhere and have greater quality of life and more positive health outcomes. Future research on decision aid development should consider that written information is helpful for patients especially when presented in conjunction with verbal information given by their physician. Decision aids may be more effective for patients who are without a primary caregiver especially because patients experience false impressions about their diagnosis and treatment efficacy. This could be attributed to selective memory during the clinical encounter, and patients without caregivers are most likely at higher risk given that they do not have a second party who is paying attention to the information given by the physician. Providing written information to patients, which is meant to compliment what is told to them in a clinical encounter, may help alleviate some of the discordance in “take-home” information.
Strengths and limitations
This review has notable strengths and weaknesses that should be discussed. There were a relatively small number of studies that were eligible for inclusion in the review. Non-peer reviewed literature was not included in this review which may have increased the overall sample size. There were five additional studies that did not distinguish their results enough by cancer type to be included in this review, and it is unclear if they may have provided additional insights. The majority of included studies were conducted outside of the USA, suggesting varying cultural norms and standards of practice and differing medical care systems. It should be noted that there is some crossover between the four themes. None of these themes occur in a vacuum, and as a result in some aspects, they are intertwined. For example, issues of personal knowledge may complicate a patient’s relationship and communication with their provider. Regardless, these areas of influence still uniquely contribute to a patient’s treatment decision-making process. Lastly, it should also be taken into consideration that the culture surrounding medical decision-making and the progression towards SDM models and consumer-based medicine may impact potential influences into modern-day treatment decision-making versus research that was conducted over a decade ago.
Strengths of this review include that it is solely focused in on the CRC population, which is often overlooked and under researched outside of primary prevention-based studies. Studies were not limited by date for the purpose of having wide inclusion criteria, and despite the wide time frame of included studies in this review (i.e., 1999–2015), there is limited research into the area of patient-level treatment decision-making within the CRC population. This could have potentially impacted the results related to patient-level influences. Most importantly, this is the first review to consider influential factors on treatment decision-making among patients with CRC. This was also the first review to organize the literature relative to themes for both characterization as well as opportunities for further study.
Conclusions
Treatment decision-making among patients with CRC is a challenging process that is influenced by variables at various levels. Decision aid development is becoming more widespread to help with treatment decision-making in cancer populations, but in order to develop effective decision aids, there needs to be more foundational research into the influences on treatment decision-making that is cancer-population specific. This comprehensive review confirms that CRC is largely under researched in the area of decision-making and most research that has been conducted is largely focused on primary prevention. Results of this review also call into question the validity of the concept of SDM as it is currently defined and whether it is the best method for increasing patient satisfaction and bettering subsequent health outcomes.
References
Beaver K, Bogg J, Luker KA (1999) Decision-making role preferences and information needs: a comparison of colorectal and breast cancer. Health Expect 2:266–276
Beaver K, Campbell M, Craven O, Jones D, Luker KA, Susnerwala SS (2009) Colorectal cancer patients’ attitudes towards involvement in decision making. Health Expect 12:27–37
Beaver K, Craven O, Witham G, Tomlinson M, Susnerwala S, Jones D, Luker KA (2007) Patient participation in decision making: views of health professionals caring for people with colorectal cancer. J Clin Nurs 16:725–733
Beaver K, Jones D, Susnerwala S, Craven O, Tomlinson M, Witham G, Luker KA (2005) Exploring the decision-making preferences of people with colorectal cancer. Health Expect 8:103–113
Berry J, Bumpers K, Ogunlade V, Glover R, Davis S, Counts-Spriggs M, Kauh J, Flowers C (2009) Examining racial disparities in colorectal cancer care. J Psychosoc Oncol 27:59–83
Berry J, Caplan L, Davis S, Minor P, Counts-Spriggs M, Glover R, Ogunlade V, Bumpers K, Kauh J, Brawley OW, Flowers C (2010) A black-white comparison of the quality of stage-specific colon cancer treatment. Cancer 116:713–722
Busch EL, Martin C, DeWalt DA, Sandler RS (2015) Functional health literacy, chemotherapy decisions, and outcomes among a colorectal cancer cohort. Cancer Control 22:95–101
Chagpar R, Xing Y, Chiang YJ, Feig BW, Chang GJ, You YN, Cormier JN (2012) Adherence to stage-specific treatment guidelines for patients with colon cancer. J Clin Oncol 30:972–979
Charles C, Gafni A, Whelan T (2000) How to improve communication between doctors and patients. Learning more about the decision making context is important. BMJ 320:1220–1221
Degner LF, Sloan JA, Venkatesh P (1997) The Control Preferences Scale. Can J Nurs Res 29:21–43
Dijkers M (2015) What is a scoping review? In: editor (ed)^(eds) Book what is a scoping review? Center on knowledge translation for disability and rehabilitation Research, City.
Du XL, Fang S, Vernon SW, El-Serag H, Shih YT, Davila J, Rasmus ML (2007) Racial disparities and socioeconomic status in association with survival in a large population-based cohort of elderly patients with colon cancer. Cancer 110:660–669
Elkin EB, Kim SH, Casper ES, Kissane DW, Schrag D (2007) Desire for information and involvement in treatment decisions: elderly cancer patients’ preferences and their physicians’ perceptions. J Clin Oncol 25:5275–5280
Fallowfield LJ (2008) Treatment decision-making in breast cancer: the patient-doctor relationship. Breast Cancer Res Treat 112(Suppl 1):5–13
Fu AZ, Graves KD, Jensen RE, Marshall JL, Formoso M, Potosky AL (2015) Patient preference and decision-making for initiating metastatic colorectal cancer medical treatment. J Cancer Res Clin Oncol
Hofmann S, Vetter J, Wachter C, Henne-Bruns D, Porzsolt F, Kornmann M (2012) Visual AIDS for multimodal treatment options to support decision making of patients with colorectal cancer. BMC Med Inform Decis Mak 12:118
Institute NC SEER Cancer statistics factsheets: colon and rectum cancer. In: editor (ed)^(eds) book SEER cancer statistics factsheets: colon and Rectum cancer, City
Jorgensen ML, Young JM, Solomon MJ (2013) Adjuvant chemotherapy for colorectal cancer: age differences in factors influencing patients’ treatment decisions. Patient Prefer Adherence 7:827–834
Kessels RP (2003) Patients’ memory for medical information. J R Soc Med 96:219–222
Levac D, Colquhoun H, O’Brien K (2010) Scoping studies: advancing the methodology. Implement Sci 5:19
Mack JW, Cronin A, Fasciano K, Block SD, Keating NL (2015) Cancer treatment decision-making among young adults with lung and colorectal cancer: a comparison with adults in middle age. Psychooncology
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535
Mott-Coles S (2014) Patients’ cultural beliefs in patient-provider communication with African American women and Latinas diagnosed with breast cancer. Clin J Oncol Nurs 18:443–448
Ramfelt E, Lützen K, Nordström G (2005) Treatment decision-making in a group of patients with colo-rectal cancer before surgery and a one-year follow-up. Eur J Cancer Care (Engl) 14:327–335
Ramfelt E, Lützén K (2005) Patients with cancer: their approaches to participation in treatment plan decisions. Nurs Ethics 12:143–155
Sahay TB, Gray RE, Fitch M (2000) A qualitative study of patient perspectives on colorectal cancer. Cancer Pract 8:38–44
Sajid MS, Shakir AJ, Baig MK (2011) Information on the Internet about colorectal cancer: patient attitude and potential toward web browsing. A prospective observational study. Can J Surg 54:339–343
Salkeld G, Solomon M, Short L, Butow P (2004) A matter of trust—patient’s views on decision-making in colorectal cancer. Health Expectations 7:104–114
Sanders T, Skevington S (2003) Do bowel cancer patients participate in treatment decision-making? Findings from a qualitative study. Eur J Cancer Care (Engl) 12:166–175
Singh JA, Sloan JA, Atherton PJ, Smith T, Hack TF, Huschka MM, Rummans TA, Clark MM, Diekmann B, Degner LF (2010) Preferred roles in treatment decision making among patients with cancer: a pooled analysis of studies using the Control Preferences Scale. Am J Manag Care 16:688–696
Snijders HS, Kunneman M, Bonsing BA, de Vries AC, Tollenaar RA, Pieterse AH, Stiggelbout AM (2014) Preoperative risk information and patient involvement in surgical treatment for rectal and sigmoid cancer. Colorectal Dis 16:O43–O49
Tejeda S, Darnell JS, Cho YI, Stolley MR, Markossian TW, Calhoun EA (2013) Patient barriers to follow-up care for breast and cervical cancer abnormalities. J Women’s Health (Larchmt) 22:507–517
van der Heide I, Rademakers J, Schipper M, Droomers M, Sørensen K, Uiters E (2013) Health literacy of Dutch adults: a cross sectional survey. BMC Public Health 13:179
Wong AC, Stock S, Schrag D, Kahn KL, Salz T, Charlton ME, Rogers SO, Goodman KA, Keating NL (2014) Physicians’ beliefs about the benefits and risks of adjuvant therapies for stage II and stage III colorectal cancer. J Oncol Pract
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
There was no financial support for this study.
Rights and permissions
About this article
Cite this article
Cranley, N.M., Curbow, B., George, T.J. et al. Influential factors on treatment decision making among patients with colorectal cancer: A scoping review. Support Care Cancer 25, 2943–2951 (2017). https://doi.org/10.1007/s00520-017-3763-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-017-3763-z