Abstract
Purpose
Professional organizations provide no guidelines regarding assessment and management of opioid abuse risk in cancer. Universal precautions (UP) developed for non-cancer pain, include assessments for aberrant behavior, screening questionnaires, and urine drug screens (UDS). The role of UDS for identifying opioid abuse risk in cancer is uncertain. Our aim is to characterize inappropriate UDS, and identify a potential role for UDS in therapeutic decision-making.
Methods
An observational retrospective chart review of 232 consecutive supportive care clinic patients were seen during the study. Twenty-eight of the two hundred thirty-two did not meet inclusion criteria. One hundred fifty of the two hundred four had active cancer, while 54 had no evidence of active disease. Clinicians ordered UDS based on their clinical judgment of patients’ substance misuse risk. Edmonton symptom assessment scores, history of substance abuse, alcohol use, tobacco use, aberrant behavior, and morphine equivalent daily dose (MEDD) were obtained.
Results
Pain scores and MEDD were higher (p = 0.021; p < 0.001) in the UDS group vs non-UDS. Forty percent of the patients (n = 82/204) had at least one UDS and 70% (60/82) had an inappropriate result. Thirty-nine percent (32) were inappropriately negative, showing no prescribed opioids. Forty-nine of the eighty-two were positive for non-prescribed opioids, benzodiazepine, or illicit substance. Eleven of the forty-nine had only cannabis metabolites in their urine. There were no significant differences between appropriate and inappropriate UDS groups regarding pain scores, MEDD or referral to psychology, psychiatry, or substance abuse specialists.
Conclusions
UDS on the 82 oncology patients at high risk for substance misuse were frequently positive (46%) for non-prescribed opioids, benzodiazepines or potent illicit drugs such as heroin or cocaine, and 39% had inappropriately negative UDS, raising concerns for diversion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A comprehensive opioid risk assessment is advocated for patients with cancer to improve prescribing practices [1]. An adaptation of Universal Precautions (UP) initially developed for patients with non-cancer pain, has been proposed for cancer pain [2, 3]. These include assessments of substance abuse risk, monitoring of aberrant behavior, and the use of additional assessments such as urine drug screens (UDS). Some studies in non-cancer pain suggest UDS assist in identifying illicit drug use or opioid prescription misuse. Data from more than 900,000 urine samples revealed up to 75% of patients did not use their medications as prescribed [4]. In the primary care setting, aberrant results were found for 30% of UDS in chronic pain patients on opioid therapy, largely because of prescribed opioid non-detection and cannabis [5]. Despite increasing concerns that patients with cancer are also at high risk of opioid abuse, [6] reports of UDS from cancer centers are very rare [7, 8]. Professional organizations have no guidelines regarding screening for opioid risk in cancer and a U.S. survey of palliative care programs found the majority had no substance abuse or diversion policies [9].
In this retrospective review, our aims were to
-
1.
Characterize ambulatory cancer patients with abnormal UDS.
-
2.
Describe the non-prescribed opioids and illicit drugs identified by UDS.
-
3.
Identify a potential role for UDS in therapeutic decision–making.
Methods
An observational retrospective chart review of 232 consecutive supportive care clinic patients were seen at a NCI center during an 18-month period from July 2012 to December 2013. Patients with at least one urine drug screen ordered by the palliative clinic were included (n = 82). Patients were excluded if they had a UDS ordered by another service (n = 3), were only seen by ancillary staff without a palliative physician or nurse practitioner visit (n = 13), or had no diagnosis of cancer (n = 12).
Patient characteristics included sex, race, age, diagnosis, and disease status (No Evidence of Disease (NED) vs Active Cancer (AC)). ECOG Performance Status, Edmonton Symptom Assessment Scores (ESAS), history of aberrant behavior, alcohol use (remote or current), and tobacco use (remote or current) were collected. Management characteristics included referral for psychiatry/psychology/substance abuse evaluation, opioid requirements measured as a morphine equivalent daily dose (MEDD), opioid type, and compliance with follow-up. The number of UDS obtained, results, and the appropriateness of the results were documented. If a patient had multiple UDS, then data were collected from the first abnormal UDS. If a patient had multiple UDS with no abnormality, then data were collected from the first UDS. All UDS were analyzed by mass spectrometry. The UDS evaluation in our clinic initially involves an enzyme immunoassay screen, which has the potential to detect compounds that can produce a “false” positive drug result. The UDS evaluation then proceeds with definitive testing, mass spectrometry, to positively identify drugs and/or drug metabolites present, providing more detailed information on opioids or illicit substances.
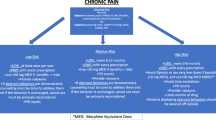
Palliative care physicians or nurse practitioners used clinical judgment to order UDS, based on patients’ aberrant behavior ( lost prescriptions, request for early refill, prescriptions obtained from multiple providers, demands for inappropriate dose escalation), or past history of chemical coping (illicit drug use, CAGE questionnaire scores ≥2) [10]. This clinical approach for detecting and avoiding harm to patients is similar to the universal precautions suggested for managing opioid risk in patients with non-malignant pain. However, even the guidelines for managing non-malignant pain have no clear criteria for obtaining UDS [11] and there were no mandatory “triggers” or care pathways in place for ordering a UDS in our clinic.
Statistical methods
All measures were summarized using frequencies and percentages, means and standard deviations, and medians and interquartile ranges, where appropriate. The demographic and additional characteristics were summarized separately and compared using exact Pearson’s chi-square tests (due to small expected cell counts), two-sample t tests and Kruskal-Wallis tests. Similar tests were used to compare subjects that had an appropriate and inappropriate UDS result. All inference was performed at the 0.05 level.
Results
Patient characteristics and demographics were compared between patients without UDS and those with at least one UDS (Table 1). One hundred fifty patients had active cancer, 54 cancer patients had no evidence of active disease. Characteristics and demographics were compared between patients with appropriate or expected UDS results to patients with inappropriate/unexpected results (Table 2). Patients in the non-UDS population were significantly younger, Caucasian, and more likely to active cancer. The non-UDS population were less likely to have a documented history of aberrant behavior, tobacco use, or alcohol use and had significantly (p = 0.021) lower pain scores (5.6/10) and MEDD (95 mg) compared to the UDS group (6.5/10; 248 mg). Patients with an inappropriate UDS result were more likely to be younger, non-white, and have multiple UDS ordered. Compared to patients with an appropriate UDS, those with inappropriate UDS showed a trend toward lower sustained release opioid: immediate release opioid ratio (p = 0.051).
Of the 204 patients seen in the outpatient palliative care clinic during the study period, 40% (n = 82) of patients had at least one UDS (Fig. 1). For patients with at least one UDS, 73% (n = 60) had an inappropriate UDS. Forty-nine of the eighty-two (60%) were positive for a non-prescribed opioid, benzodiazepine, or illicit substance. Eleven of the forty-nine patients with an inappropriately positive UDS had only cannabis metabolites in their urine. All other patients with inappropriately positive UDS (38/49) had non-prescribed opioids, benzodiazepines, cocaine or heroin with 21 patients demonstrating polysubstance abnormalities (≥1 urine abnormality). Thirty-two patients (39%) had an inappropriately negative UDS, showing none of their prescribed opioids (Fig. 2). Eighteen of these 32 patients had active cancer while 14 no longer had evidence of cancer (Table 2). Eleven (13%) of the 82 patients with a UDS were negative for the prescribed opioid while 21(26%) patients had both inappropriately positive and negative UDS.
Clinical interventions and management were comparable between the two groups (Table 3). Subjects with inappropriate UDS results were more likely to have multiple UDS screenings than those with appropriate results.
Discussion
UDS abnormalities were common in our ambulatory patients with cancer. Remarkably, almost half of patients tested were positive for non-prescribed opioids or potent illicit drugs such as heroin or cocaine and only 1 in 5 had cannabis as the sole substance of misuse. In addition, 39% of those tested, had inappropriately negative UDS, raising concerns for diversion or hoarding of opioids. Although only 40% of outpatients underwent UDS, the abnormal results accounted for almost 30% of all patients seen in an 18 month period. To our knowledge, these high rates of inappropriate UDS results have not been reported in palliative care populations. Only two studies have reported UDS results in ambulatory patients with cancer. One study obtained UDS in less than 5% of patients, while another found a high prevalence of abnormal UDS, but identified cannabis as the sole abnormality in 62% of abnormal UDS [8]. Our rates are closer to those reported in non-malignant chronic pain populations where 38% of patients were found to have no detectable level of their prescribed medication and 29% had a non-prescribed medication present in their urine [4]. We did find a trend for patients with inappropriate UDS to have a lower sustained release to immediate release ratio. The greater use of immediate release opioids may be consistent with diversion tendencies or binge use [12, 13].
We were conscious of the potential for misinterpreted or falsely “inappropriate” UDS results harming patients or patient-provider relationships. The UDS in our clinic were analyzed by mass spectrometry, a relatively expensive assay that provides a high level of accuracy and sensitivity, definitively identifying the drug of interest, and eliminating the potential for “false” positive screening results. Expected drug doses consistent with measured assay levels were reported, and a toxicologist was also available for additional discussion and interpretation of any equivocal results. Based on the high percentage of abnormal UDS results in our clinic, one could argue that testing should be extended to all patients. However, a less expensive assay would be necessary for screening because of the prohibitive cost associated with mass spectrometry. We have not yet implemented any changes in our clinic because of concerns that a less accurate test would increase the level of clinician uncertainty and increase the risk of opioids being inappropriately withheld in an especially vulnerable population. Strategies adopted in our clinic for managing patients with abnormal UDS include shorter intervals between clinic visits, the use of more sustained release vs IR opioids, brief motivational interviewing, and co-management with substance abuse clinicians. Opioid prescriptions are not provided to patients under special circumstances e.g. when the UDS is negative for all prescribed opioids and the result is confirmed to be accurate by the toxicologist.
Prior studies using screening questionnaires to assess for chemical coping in patients with cancer, found “positive” screens were associated with increased pain scores and opioid use [14,15,16]. Similarly, our patients selected for UDS (based on a past history of alcohol or drug use, positive risk questionnaires, or aberrant behavior) had higher pain scores and MEDD. However, there were no differences in ESAS scores or MEDD whether UDS were inappropriate or appropriate, and our therapeutic decisions were similar. There may be a number of reasons to explain the similar management: Patients with appropriate UDS may also have been chemical copers, but were able to avoid abuse of illicit drugs or non-prescribed opioids. Some of these “chemical copers” with appropriate UDS may have been the recipients of clinician opioid prescription “overtreatment” [17]. Also, clinicians may have identified a need among both UDS groups for referral to psychiatry or to our embedded psychologist for management of maladaptive coping, existential suffering or psychological distress. Finally, we did not clearly distinguish the reasons for psychosocial referral in our clinical records.
Our preliminary findings indicate there is a need for future prospective studies. The scope of opioid and drug misuse in oncology patients should be evaluated by UDS in larger populations. Evaluating the extent of the problem may be helpful for resource allocation and in raising the awareness of clinicians and hospital administrators. There are also extra costs associated with UDS and the potential for harm to the physician-patient relationship because of implied mistrust. Therefore, studies to determine whether UDS provide useful additional information to existing assessments for opioid risk such as questionnaires (e.g. CAGE-AID, SOAPP), prescription monitoring programs and clinician evaluation of aberrant behavior are needed.
Our single center, retrospective study has several limitations, including a relatively small sample size. The high prevalence of inappropriate UDS may be influenced by the referral of highly selected patients with complex psychosocial needs to our specialist palliative care team. Additional research needs to be done in other ambulatory oncology and palliative care clinics before our findings can be generalized. Our rates of illicit drug use may also be elevated because the supportive care clinic operates in a safety-net hospital that provides care for a large proportion of underserved patients; however, Virginia ranks in the lower quartile for prescription opioids and for drug overdose rates among states [18].
Conclusion
Our preliminary findings suggest that substance misuse is frequent in ambulatory supportive care patients exhibiting aberrant behavior or high risk for chemical coping. Although we believe inappropriate UDS results may be helpful for individualized management and therapeutic decision making, our results indicate subsequent clinical interventions were not significantly different between inappropriate and appropriate UDS groups. Future research should determine whether UDS are helpful for risk stratification and improving clinical outcomes such as pain control, function, opioid dose reduction, and mortality in patients with cancer.
References
Del Fabbro E (2014) Assessment and management of chemical coping in patients with cancer. J Clin Oncol 32(16):1734–1738. doi:10.1200/JCO.2013.52.5170
Gourlay DL, Heit HA, Almahrezi A (2005) Universal precautions in pain medicine: a rational approach to the treatment of chronic pain. Pain Med 6(2):107–112. doi:10.1111/j.1526-4637.2005.05031.x
Modesto-Lowe V, Girard L, Chaplin M (2012) Cancer pain in the opioid-addicted patient: can we treat it right? J Opioid Manag 8(3):167–175. doi:10.5055/jom.2012.0113
Couto JE, Romney MC, Leider HL, Sharma S, Goldfarb NI (2009) High rates of inappropriate drug use in the chronic pain population. Popul Health Manag 12(4):185–190. doi:10.1089/pop.2009.0015
Turner JA, Saunders K, Shortreed SM, Rapp SE, Thielke S, LeResche L et al (2014) Chronic opioid therapy risk reduction initiative: impact on urine drug testing rates and results. J Gen Intern Med 29(2):305–311. doi:10.1007/s11606-013-2651-6
Rauenzahn S, Del Fabbro E (2014) Opioid management of pain: the impact of the prescription opioid abuse epidemic. Curr Opin Support Palliat Care 8(3):273–278. doi:10.1097/SPC.0000000000000065
Childers JW, King LA, Arnold RM (2015) Chronic pain and risk factors for opioid misuse in a palliative care clinic. Am J Hosp Palliat Care 32(6):654–659. doi:10.1177/1049909114531445
Barclay JS, Owens JE, Blackhall LJ (2014) Screening for substance abuse risk in cancer patients using the opioid risk tool and urine drug screen. Support Care Cancer 22(7):1883–1888. doi:10.1007/s00520-014-2167-6
Tan PD, Barclay JS, Blackhall LJ (2015) Do palliative care clinics screen for substance abuse and diversion? Results of a National Survey. J Palliat Med 18(9):752–757. doi:10.1089/jpm.2015.0098
Dev R, Parsons HA, Palla S, Palmer JL, Del Fabbro E, Bruera E (2011) Undocumented alcoholism and its correlation with tobacco and illegal drug use in advanced cancer patients. Cancer 117(19):4551–4556. doi:10.1002/cncr.26082
Chou R, Fanciullo GJ, Fine PG, Adler JA, Ballantyne JC, Davies P et al (2009) Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain 10(2):113–130. doi:10.1016/j.jpain.2008.10.008
Morton T, Kostenbader K, Montgomery J, Devarakonda K, Barrett T, Webster L (2014) Comparison of subjective effects of extended-release versus immediate-release oxycodone/acetaminophen tablets in healthy nondependent recreational users of prescription opioids: a randomized trial. Postgrad Med 126(4):20–32. doi:10.3810/pgm.2014.07.2780
Shram MJ, Sathyan G, Khanna S, Tudor IC, Nath R, Thipphawong J et al (2010) Evaluation of the abuse potential of extended release hydromorphone versus immediate release hydromorphone. J Clin Psychopharmacol 30(1):25–33. doi:10.1097/JCP.0b013e3181c8f088
Parsons HA, Delgado-Guay MO, El Osta B, Chacko R, Poulter V, Palmer JL et al (2008) Alcoholism screening in patients with advanced cancer: impact on symptom burden and opioid use. J Palliat Med 11(7):964–968. doi:10.1089/jpm.2008.0037
Koyyalagunta D, Bruera E, Aigner C, Nusrat H, Driver L, Novy D (2013) Risk stratification of opioid misuse among patients with cancer pain using the SOAPP-SF. Pain Med 14(5):667–675. doi:10.1111/pme.12100
Kwon JH, Hui D, Chisholm G, Bruera E (2013) Predictors of long-term opioid treatment among patients who receive chemoradiation for head and neck cancer. Oncologist 18(6):768–774. doi:10.1634/theoncologist.2013-0001
Paice JA, Von Roenn JH (2014) Under- or overtreatment of pain in the patient with cancer: how to achieve proper balance. J Clin Oncol 32(16):1721–1726. doi:10.1200/JCO.2013.52.5196
Paulozzi LJ, Mack KA, Hockenberry JM (2014) Division of Unintentional Injury Prevention NCfIP, Control CDC. Vital signs: variation among States in prescribing of opioid pain relievers and benzodiazepines–United States, 2012. MMWR Morb Mortal Wkly Rep 63(26):563–568
Acknowledgment
Teri-Dulong Rae in preparation of the manuscript
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Rauenzahn, S., Sima, A., Cassel, B. et al. Urine drug screen findings among ambulatory oncology patients in a supportive care clinic. Support Care Cancer 25, 1859–1864 (2017). https://doi.org/10.1007/s00520-017-3575-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-017-3575-1