Abstract
Purpose
Reasons for the social gradient in cancer survival are not fully understood yet. Previous studies were often only able to determine the socio-economic status of the patients from the area they live in, not from their individual socio-economic characteristics.
Methods
In a multi-centre cohort study with 1633 cancer patients and 10-year follow-up, individual socio-economic position was measured using the indicators: education, job grade, job type, and equivalence income. The effect on survival was measured for each indicator individually, adjusting for age, gender, and medical characteristics. The mediating effect of health behaviour (alcohol and tobacco consumption) was analysed in separate models.
Results
Patients without vocational training were at increased risk of dying (rate ratio (RR) 1.5, 95% confidence interval (CI) 1.1–2.2) compared to patients with the highest vocational training; patients with blue collar jobs were at increased risk (RR 1.2; 95% CI 1.0–1.5) compared to patients with white collar jobs; income had a gradual effect (RR for the lowest income compared to highest was 2.7, 95% CI 1.9–3.8). Adding health behaviour to the models did not change the effect estimates considerably. There was no evidence for an effect of school education and job grade on cancer survival.
Conclusions
Patients with higher income, better vocational training, and white collar jobs survived longer, regardless of disease stage at baseline and of tobacco and alcohol consumption.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Disparities in cancer incidence and survival still exist in high-income countries. The Multinational Association of Supportive Care in Cancer (MASCC) Education Study Group therefore has recently published a call for further research and action in this area [1].
One challenge of understanding the relationship of socio-economic position (SEP) and cancer survival is that many studies investigating this relationship have been conducted with area level data [2]. This approach means that researchers determine patients’ SEP not by their individual characteristics, but by socio-economic indicators of the area they live in. Individual level studies, in contrast, ascertain the SEP of each patient from individual characteristics.
The area level approach is used far more often because area information is frequently the only information possible to obtain from cancer registry data. Such area level comparisons are important to understand context-based factors driving the social gradient in health [3]. However, area SEP is not simply a proxy for individual SEP; using aggregated indicators may introduce an ecological bias because the area level SEP may not correspond with the patient’s individual SEP [4, 5].
Individual level studies can examine the effects of individual SEP on health in more detail and without ecological bias. They also enable the investigation of the different SEP aspects—education, income, and job separately [6], which is crucial to better understand their individual role in driving the social gradient in health. While they are correlated with each other, they represent different phenomena and affect different causal mechanisms between SEP and health [7, 8].
Evidence from area [9–13] and individual [8, 14, 15] level studies suggests that low SEP is associated with poor survival in a variety of cancers. Moreover, socio-economic inequalities in survival have been widening for many adult cancers [10, 16–19]. Gains in survival due to progress in medicine are less marked among the more deprived than among the more affluent groups [10]. The causal mechanisms for this social gradient are not yet entirely understood [2, 20, 21]. One explanation is that clinical factors such as stage at diagnosis and treatment are associated with SEP. Indeed, socially deprived patients more often present with advanced disease [2]. However, studies have found that stage at diagnosis explains part but not all of the deprivation gap in breast [16, 22], lung [9, 23], oral [9], laryngeal [24], and colorectal [9] cancer survival. There is also evidence that patients with low income receive different treatment compared to more affluent patients [19, 23, 25, 26].
A second explanation is that the patient’s health behaviour differs according to SEP [27]. Such behaviour does not only include smoking, alcohol consumption, exercise, and diet, but also the time patients wait before they see a doctor. Delays in access to health care occur more frequently in patients with lower SEP, resulting in the fact that they present with more advanced disease [2, 17, 25, 28, 29]. A recent review [2] also showed that patient with good social support has better survival.
In summary, evidence suggests that low SEP is associated with poor survival in cancer patients, but the role of the different SEP factors is still unclear because studies with individual patient SEP data are sparse. With the present study, we ascertained the different SEP factors in a large group of cancer patients on an individual level in order to answer the question as to which SEP factors—education, job grade, and income drive the social gradient in cancer survival.
Methods
Enrolment
Over a period of 2 years, all patients admitted for diagnosis or treatment of cancer to the Leipzig University Medical Centre, to St. Elisabeth Hospital Leipzig, and to St. Georg Hospital Leipzig, Germany, were eligible for this study. Exclusion criteria were the following: age below 18 years and inability to complete a questionnaire. After giving written informed consent, the participants received a questionnaire to be completed on their first days in the hospital. Personal interviews were conducted after completion of the questionnaires by trained psychologists and study nurses to ascertain health behaviour with a structured interview (see below).
The study was approved by the institutional ethics committee of Leipzig University.
Ascertainment of survival
All patients treated in Leipzig for malignant diseases are documented in a regional Cancer Registry. The Registry documents stage at diagnosis, date of diagnosis, and the starting date of treatment. It follows up every patient and documents the date of death. For this purpose, information from local census bureaus, health authorities, and from health care providers are collected and merged. In addition, data on date of death are exchanged with other cancer registries within Germany on a regular basis so that patients moving to other areas can be followed up as well.
Ascertainment of socio-economic position
Education was assessed by the highest level of (a) academic education and (b) vocational training. Academic education was classified as compulsory (or below), post-compulsory, and higher secondary school. When grouping the educational degrees, we had to take into account that the education system in Germany is (and was) not homogeneous. The participants of our study grew up in the former German Democratic Republic (eastern Germany), in the former Federal Republic of Germany (western Germany), and in pre-war Germany, and each had its own education system. Patients were considered to have compulsory education or less if they had attended 6 years of schooling in pre-war Germany or 8 years in post-war Germany. Depending on the federal state and the school type attended, higher secondary school degrees are obtained after 11 to 13 years. These degrees (called “Abitur” or “Fachhochschulreife”) enable the students to attend universities. All degrees between these two types were considered post-compulsory in our study. After school, vocational training is another important part of education in Germany. We asked the patients whether they had completed no vocational training, apprenticeship, higher vocational education, or vocational college/university.
Job grade was defined by the patient’s position within a certain job category. First, the patient reported the job category (e.g., worker). Then the job grade according to this category was enquired. For example, the grade levels for workers were unskilled, skilled, and skilled with a leading position.
Whether patients had a white or blue collar job was documented, and this variable is called job type.
To ascertain the equivalence income, participants were asked to indicate their net household income, i.e., the sum of all incomes in the household minus taxes. They also reported the number of persons living in their household and how many of them were under the age of 18 years. We then adopted the OECD-modified equivalence scale [30], assigning each household type a value in proportion to its needs.
All socio-economic variables were assessed according to the guidelines of the German Rehabilitation Research Association [31].
Covariates
The patient’s stage of disease at presentation was documented by the medical team and reported to the Cancer Registry. There, it was classified according to the Union Internationale Contre le Cancer (UICC), 4th edition, by experienced data managers specifically trained for this task.
Tumour site was documented according to the International Classification of Diseases (ICD-10).
Cohabitation was defined from two items. Firstly, we asked the patients whether they currently had a partner. Secondly, the number of people in the household was documented. If a patient neither had a partner nor lived together with someone in the household, he or she was classified as “lives alone”.
Alcohol, nicotine, and drug consumption were evaluated in personal interviews by trained interviewers using the Structured Clinical Interview (SCID) [32]. The interviewer asked about the amount consumed with pre-defined questions and the response options were open.
Statistical analysis
The outcome of interest was all-cause mortality. Survival time was defined as the interval between the date of presentation and the date of death or end of follow-up. Mortality rates were computed by dividing the number of deaths by the sum of person-years (py) at risk, per 100 py.
Univariate Poisson regression models were used to estimate the crude rate ratio (RR) for dying in relation to SEP categories with 95% confidence intervals (CI). To avoid duplication, the CIs are presented in the tables but not repeated in the text.
In addition, rate differences (RD) and attributable fractions (AF) were calculated.
Multivariable Poisson regression models estimated the RR again, now adjusted for sex, age at diagnosis, UICC stage at diagnosis, tumour site, and cohabitation. In order to assess whether the association between SEP categories and survival was modified by gender, tests of interaction were performed using likelihood ratio tests comparing the fully adjusted model with the same model with an interaction term. No such interactions were found.
To understand the potential mediating effect of health behaviour, the regression models were repeated while adding current tobacco and alcohol consumption to the set of covariables. We did not enter health behaviour in the first (main) model because we assumed it to be a factor on the causal pathway. For example, a person may have little academic education which may result in poor knowledge about the negative effects of smoking, hence this person may smoke more than others and, consequently, the survival is worse. Such mediating factors should not be used as a covariate in regression models to avoid over-adjustment.
Finally, to understand the joint effects of the individual SEP variables, they all were entered simultaneously into one regression model. This final model was computed again separately for the three largest disease groups in this study.
The statistical analyses were performed using STATA version 12 (StataCorp, Texas, USA).
Results
Sample
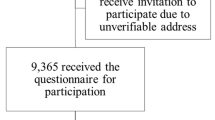
A total of 2913 patients were admitted to the hospital during the study duration. 147 (5%) of them were excluded because they had recurrent disease and 85 (3%) because of a second primary, leaving 2681 patients potentially eligible for this study. Five hundred forty-nine (20%) of them were unable to participate because of cognitive deficits (n = 60), physical weakness (n = 130), mental health problems (n = 299), organisational problems (n = 56), or because they died before the first contact (n = 4). Another 499 patients (19%) declined participation. Hence, 1633 patients (77% of all eligible) were enrolled into this study, contributing 11,926py together.
Survival
In total, 665 (41%) study participants died within follow-up. The mortality rate was 5.6 per 100py (95% CI 5.2; 6.0). Compared to the study participants, the mortality rate in non-participants was somewhat higher, with 6.3 per 100py (95% CI 5.8; 6.9).
The median follow-up time was 10 years (mean 7 years, minimum 3 days, maximum 12 years).
Sample characteristics
Twenty six percent of the patients had a university or college degree. Six percent had an equivalence income of less than 500 euros per month. The most frequent tumour sites were breast (14%) and prostate (17%). In 12% of the cases, the disease was metastatic (Table 1 for more details).
Health behaviour could be assessed in 624 patients. Of them, 78 (13%) currently smoked, and 363 (58%) had ever smoked. Fifty (8%) patients currently abused alcohol, and 276 (44%) had ever consumed alcohol in dangerous amounts.
Survival by socio-economic position
Death rates were higher in patients with post-compulsory and compulsory school education compared to patients with college education (Table 2). Patients with compulsory school education lived 2 years fewer than patients with higher secondary school education (RR 1.5). However, when we adjusted for demographic and clinical characteristics, this effect decreased (Table 3).
The level of vocational training was associated with survival. Patients with the highest vocational training lived 4 years longer than patients without vocational training (AF 47%). After adjustment for demographic and clinical variables, the RR decreased slightly, but there was still evidence for an effect of vocational training on survival. Compared to patients with the highest vocational training, death rates were higher in patients with apprenticeship (RR 1.2) and with no vocational training (RR 1.5) (Table 3, Fig. 1). When health behaviour was added to the model, the RRs did not change considerably.
There was no evidence for an effect of job grade on survival (Tables 2 and 3).
Patients with blue-collar jobs had a 1.4 times increased risk of dying compared to those with white-collar jobs (RD 1.9, AF 28%). This effect did not disappear after adjustment for confounders, but it decreased to 1.2. When we entered health behaviour into the model, it remained at the same level.
The risk of dying in the lowest income group was more than double compared to the highest income group (RR 2.5, RD 5.1, AF 60%; see Table 2 for details). This effect did not decrease after adjusting for age, sex, cohabitation, tumour site, and stage of disease. It was still present when entering health behaviour into the model (Table 3 and Fig. 1).
To estimate the independent contribution of the socio-economic characteristics regarding the social gradient in survival, a joint regression model was built with all previously separately tested SEP factors and all covariates combined. It appeared that patients without vocational training were at a 1.7 times increased risk of dying while adjusting for all the other factors. Low income remained a strong predictor of poor survival (Table 3). Comparable results were found in the three subgroups calculated separately (see online supplementary Table).
Discussion
This study aimed to answer the question as to which factors of SEP drive the social gradient in cancer survival. We found that, in contrast to patients with coronary heart disease, cancer patients with a low job grade did not have poorer survival rates compared to those with higher job grades. School education was also not related to survival, yet, vocational education was. Patients without vocational training had a 90% increased risk of dying compared to patients with a vocational college or university degree; 47% of all cancer deaths in patients without vocational training were attributable to this fact. It should be noted that the word “attributable” does not imply that vocational training is “causal” for cancer death or survival. This association could have been spurious because of confounding factors, for example the stage of disease at presentation. In the UK, deprived patients are more likely to be diagnosed in an advanced stage for melanoma, prostate, endometrial, and breast cancers: The odds ratios for the most versus least deprived quintile ranged from 2.2 for melanoma to 1.3 for breast cancer [33]. In Germany, patients with low income presented 2.6 times as often with advanced disease compared to patients with higher income [34]. However, even after controlling for characteristics known to be related to survival, the association of vocational training with survival remained. A potential mediating factor could have been the patient’s health behaviour [27]. For example, patients with no vocational training could be more prone to tobacco smoking, which in turn would lead to poor survival. Health behaviour would then be a factor on the causal pathway, and hence a mediating factor rather than a confounder. Therefore, we added health behaviour separately to the model. As the relationship between vocational training and survival did not change by this, we assume that the effect of vocational training on survival must be explained by different mechanisms. One explanation would be that patients without vocational training are older and therefore die earlier. This was accounted for in the model which adjusted for age, and indeed the rate ratio decreased, but it did not disappear.
Could it be that patients without vocational training work in more hazardous jobs and are therefore more exposed to carcinogenic substances? We did not have enough information to investigate this point. The fact that blue collar workers had an increased risk of dying in our study would underline this notion. However, in the joint model, where vocational training and job type were considered together, the effect of training was still prevalent. We do assume that there must be other causal mechanisms in place here as well, for example that these patients receive different treatment than others [35, 36]. Unfortunately, we do not have the data to check these assumptions. Moreover, only 80 patients in our sample were without vocational training, thus further research is needed here before firm conclusions can be drawn. Our findings, however, emphasise the need to document not only school education in such epidemiological studies, but vocational education as well.
The second SEP factor related to cancer survival in our study was income. Across all income levels, there was a clear social gradient in cancer survival. This result is in line with results obtained from area-level studies, where the most deprived group often has a death excess of 30–50% compared to that of the most affluent one [2]. In our study, the risk was even three times increased. Not only survival is associated with poverty, but also cancer incidence [37]. The sites most strongly associated with higher poverty in the United States are Kaposi sarcoma, larynx, cervix, penis, and liver; those most strongly associated with lower poverty are melanoma, thyroid, and testis. These results are relevant for survival as well because it was shown that sites associated with higher poverty had lower incidence and higher mortality than those associated with lower poverty [37].
How can it be explained that income is related to cancer survival in a country like Germany, with supposedly equal access to health care for all? There are several explanations possible. The first goes back to Victora [38] who hypothesised that new interventions will initially reach those of higher SEP and only later affect the poor. This is underlined by research from the UK showing that the deprivation gap in survival has decreased between 1973 and 2004 from 10 to 6% in female breast cancer patients but increased from 5 to 11% in male rectum cancer patients [18]. The most likely explanation for these diverging trends in cancer survival is, according to the authors, the speed of dissemination of treatments.
The second explanation is based on psychological theories. It is known from diseases other than cancer that poor health among disadvantaged people results not just from lack of material resources but also from non-material factors such as autonomy and self-efficacy [39].
A third explanation is that poor patients may have more delays in cancer diagnosis, resulting in more advanced stage of disease at presentation [34]. However, this hypothesis is not likely to explain our results because the UICC stage was accounted for. Moreover, Arndt et al. found that, amongst breast cancer patients in Germany, the delay was even higher in those with high SEP [40].
The results of our study should be interpreted while bearing its limitations in mind. First, comorbidity was not assessed, which most likely had an impact on overall survival [41]. Secondly, health behaviour was measured only once, and this could change over time as a cancer diagnosis often leads to cessation of smoking, especially in patients with tobacco-related cancers [42–45]. We were also not able to assess the patients’ physical activity and diet because we had to keep the questionnaire brief.
The major strength of this study is that the SEP indicators were collected individually from each patient. Another advantage is that a variety of SEP indicators were included, making it possible for example to find the different effects of school education versus vocational training.
Finally, the median follow-up was 10 years, enabling us to look at the long-term consequences of SEP. Previous studies found that the deprivation gap was largest shortly after diagnosis, especially within the first 3 months [9, 23]. We see in our study that the gap is still existent many years after the diagnosis.
Our findings imply that better cancer survival could potentially be achieved by socio-economic interventions and by political decisions in addition to the medical care. Survival rates in the upper SEP groups show what is possible. We should strive to achieve such survival for all cancer patients, not only for the wealthy and well educated.
References
Dixit N, Crawford GB, Lemonde M, Rittenberg CN, Fernandez-Ortega P (2016) Left behind: cancer disparities in the developed world. Support Care Cancer 24:3261–3264
Quaglia A, Lillini R, Mamo C, Ivaldi E, Vercelli M, SEIH (Socio-Economic Indicators HWG (2013) Socio-economic inequalities: a review of methodological issues and the relationships with cancer survival. Critical Reviews in Oncology and Hematology 85:266–277
Diez Roux AV, Nieto FJ, Muntaner C, Tyroler HA, Comstock GW, Shahar E, Cooper LS, Watson RL, Szklo M (1997) Neighborhood environments and coronary heart disease: a multilevel analysis. Am J Epidemiol 146:48–63
Robert SA, Strombom I, Trentham-Dietz A, Hampton JM, McElroy JA, Newcomb PA, Remington PL (2004) Socioeconomic risk factors for breast cancer—distinguishing individual-and community-level effects. Epidemiology 15:442–450
Diez Roux A, Merkin SS, Arnett D, Chambless L, Massing M, Nieto FJ, Sorlie P, Szklo M, Tyroler HA, Watson RL (2001) Neighborhood of residence and incidence of coronary heart disease. N Engl J Med 345:99–106
Geyer S, Hemström O, Peter R, Vågerö D (2006) Education, income, and occupational class cannot be used interchangeably in social epidemiology. Empirical evidence against a common practice. J Epidemiol Community Health 60:804–810
Akinyemiju TF, Soliman AS, Johnson NJ, Altekruse SF, Welch K, Banerjee M, Schwartz K, Merajver S (2013) Individual and neighborhood socioeconomic status and healthcare resources in relation to black-white breast cancer survival disparities. Journal of cancer epidemiology 2013: Article ID 490472
Shariff-Marco S, Yang J, John EM, Sangaramoorthy M, Hertz A, Koo J, Nelson DO, Schupp CW, Shema SJ, Cockburn M, Satariano WA, Yen IH, Ponce NA, Winkleby M, THM K, Gomez SL (2014) Impact of neighborhood and individual socioeconomic status on survival after breast cancer varies by race/ethnicity: the neighborhood and breast cancer study. Cancer Epidemiol Biomark Prev 23:793–811
Jansen L, Eberle A, Emrich K, Gondos A, Holleczek B, Kajuter H, Maier W, Nennecke A, Pritzkuleit R, Brenner H (2014) Socioeconomic deprivation and cancer survival in Germany: an ecological analysis in 200 districts in Germany. Int J Cancer 134:2951–2960
Rachet B, Woods LM, Mitry E, Riga M, Cooper N, Quinn MJ, Steward J, Brenner H, Esteve J, Sullivan R, Coleman MP (2008) Cancer survival in England and Wales at the end of the twentieth century. Br J Cancer 99:S2–S10
Brusselaers N, Ljung R, Mattsson F, Johar A, Wikman A, Lagergren P, Lagergren J (2013) Education level and survival after oesophageal cancer surgery: a prospective population-based cohort study. British Medical Journal Open 3:e003754. doi:10.1136/bmjopen-2013-003754
Hastert TA, Beresford SAA, Sheppard L, White E (2015) Disparities in cancer incidence and mortality by area-level socioeconomic status: a multilevel analysis. J Epidemiol Community Health 69:168–176
Hystad P, Carpiano RM, Demers PA, Johnson KC, Brauer M (2013) Neighbourhood socioeconomic status and individual lung cancer risk: evaluating long-term exposure measures and mediating mechanisms. Soc Sci Med 97:95–103
CC W, Hsu TW, Chang CM, CH Y, Wang YF, Lee CC (2014) The effect of individual and neighborhood socioeconomic status on gastric cancer survival. PLoS One 9(2):e89655
Chang TS, Chang CM, Hsu TW, Lin YS, Lai NS, YC S, Huang KY, Lin HL, Lee CC (2013) The combined effect of individual and neighborhood socioeconomic status on nasopharyngeal cancer survival. PLoS One 8(9):e73889
Kaffashian F, Godward S, Davies T, Solomon L, McCann J, Duffy SW (2003) Socioeconomic effects on breast cancer survival: proportion attributable to stage and morphology. Br J Cancer 89:1693–1696
Schrijvers CTM, Mackenbach JP, Lutz JM, Quinn MJ, Coleman MP (1995) Deprivation and survival from breast-cancer. Br J Cancer 72:738–743
Lyratzopoulos G, Barbiere JM, Rachet B, Baum M, Thompson MR, Coleman MP (2011) Changes over time in socioeconomic inequalities in breast and rectal cancer survival in England and Wales during a 32-year period (1973-2004): the potential role of health care. Ann Oncol 22:1661–1666
Thomson CS, Hole DJ, Twelves CJ, Brewster DH, Black RJ (2001) Prognostic factors in women with breast cancer: distribution by socioeconomic status and effect on differences in survival. J Epidemiol Community Health 55:308–315
Ahnquist J, Wamala SP, Lindstrom M (2012) Social determinants of health—a question of social or economic capital? Interaction effects of socioeconomic factors on health outcomes. Soc Sci Med 74:930–939
Schrijvers CTM, Mackenbach JP, Lutz JM, Quinn MJ, Coleman MP (1995) Deprivation, stage at diagnosis and cancer survival. Int J Cancer 63:324–329
Rutherford MJ, Hinchliffe SR, Abel GA, Lyratzopoulos G, Lambert PC, Greenberg DC (2013) How much of the deprivation gap in cancer survival can be explained by variation in stage at diagnosis: an example from breast cancer in the east of England. Int J Cancer 133:2192–2200
Berglund A, Lambe M, Luchtenborg M, Linklater K, Peake MD, Holmberg L, Moller H (2012) Social differences in lung cancer management and survival in south East England: a cohort study. British Medical Journal Open 2:e001048. doi:10.1136/bmjopen-2012-001048
Groome P, Schulze KM, Keller S, Mackillop WJ, O’Sullivan B, Irish JC, Bissett RJ, Dixon PF, Eapen LJ, Gulavita SP, Hammond JA, Hodson DI, Mackenzie RG, Schneider KM, Warde PR (2006) Explaining socioeconomic status effects in laryngeal cancer. Clinical Oncology (R Coll Radiol) 18:283–292
O'Malley CD, Le GM, Glaser SL, Shema SJ, West DW (2003) Socioeconomic status and breast carcinoma survival in four racial/ethnic groups—a population-based study. Cancer 97:1303–1311
Polednak AP (2002) Survival of breast cancer patients in Connecticut in relation to socioeconomic and health care access indicators. Journal of Urban Health-Bulletin of the New York Academy of Medicine 79: 211–218
Woods LM, Rachet B, Coleman MP (2006) Origins of socio-economic inequalities in cancer survival: a review. Ann Oncol 17:5–19
Macleod U, Ross S, Gillis C, McConnachie A, Twelves C, Watt GCM (2000) Socio-economic deprivation and stage of disease at presentation in women with breast cancer. Ann Oncol 11:105–107
Brewster DH, Thomson CS, Hole DJ, Black RJ, Stroner PL, Gillis CR (2001) Relation between socioeconomic status and tumour stage in patients with breast, colorectal, ovarian, and lung cancer: results from four national, population based studies. Br Med J 322:830–831
Hagenaars A, de Vos K, Zaidi MA (1994) Poverty statistics in the late 1980s: research based on micro-data. Office for Official Publications of the European Communities, Luxembourg
Verband deutscher Rentenversicherungsträger (1999) Förderschwerpunkt “Rehabilitationswissenschaften”. Empfehlungen der Arbeitsgruppen “Generische Methoden”, “Routinedaten” und “Reha-Ökonomie”. DRV-Schriften ed. VDR, Frankfurt am Main
First M, Spitzer R, Gibbon M, Williams J (1997) Structured clinical interview for DSM-IV Axis I disorders (SCID-I), clinician version. American Psychiatric Press, Washington, DC
Lyratzopoulos G, Abel GA, Brown CH, Rous BA, Vernon SA, Roland M, Greenberg DC (2013) Socio-demographic inequalities in stage of cancer diagnosis: evidence from patients with female breast, lung, colon, rectal, prostate, renal, bladder, melanoma, ovarian and endometrial cancer. Ann Oncol 24:843–850
Singer S, Roick J, Briest S, Stark S, Gockel I, Boehm A, Papsdorf K, Meixensberger J, Müller T, Prietzel T, Schiefke F, Dietel A, Bräunlich J, Danker H (2016) Impact of socio-economic position on cancer stage at presentation: findings from a large hospital-based study in Germany. Int J Cancer 139:1696–1702
Doubeni C, Rustgi A (2015) Racial disparities in colorectal cancer survival: is elimination of variation in care the cure? J Natl Cancer Inst 107:djv229. doi:10.1093/jnci/djv229
Bristow RE, Chang J, Ziogas A, Campos B, Chavez LR, Anton-Culver H (2015) Sociodemographic disparities in advanced ovarian cancer survival and adherence to treatment guidelines. Obstet Gynecol 125:833–842
Boscoe FP, Johnson CJ, Sherman RL, Stinchcomb DG, Lin G, Henry KA (2014) The relationship between area poverty rate and site-specific cancer incidence in the United States. Cancer 120:2191–2198
Victora CG, Vaughan JP, Barros FC, Silva AC, Tomasi E (2000) Explaining trends in inequities: evidence from Brazilian child health studies. Lancet 356:1093–1098
Marmot M (2006) Health in an unequal world: social circumstances, biology and disease. Clinical Medicine 6:559–572
Arndt V, Sturmer T, Stegmaier C, Ziegler H, Becker A, Brenner H (2003) Provider delay among patients with breast cancer in Germany: a population-based study. J Clin Oncol 21:1440–1446
Backemar L, Lagergren P, Johar A, Lagergren J (2015) Impact of co-morbidity on mortality after oesophageal cancer surgery. Br J Surg 102:1097–1105
Westmaas JL, Newton CC, Stevens VL, Flanders WD, Gapstur SM, Jacobs EJ (2015) Does a recent cancer diagnosis predict smoking cessation? An analysis from a large prospective US cohort. J Clin Oncol 33:1647
Sitas F, Weber MF, Egger S, Yap S, Chiew M, O'Connell D (2014) Smoking cessation after cancer. J Clin Oncol 32:3593–3595
Danker H, Keszte J, Singer S, Thomä J, Täschner R, Brähler E, Dietz A (2011) Alcohol consumption after laryngectomy. Clin Otolaryngol 36:336–344
Singer S, Keszte J, Thiele A, Klemm E, Täschner R, Oeken J, Meister EF, Danker H, Guntinas-Lichius O, Lautermann J, Meyer A, Dietz A (2010) Rauchverhalten nach Laryngektomie. Laryngo-Rhino-Otologie 89:146–150
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by a grant from the German Federal Ministry of Education and Research (grant number 01ZZ0106) to Prof. Reinhold Schwarz for baseline data collection. The mortality follow-up received no funding.
Conflicts of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
ESM 1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Singer, S., Bartels, M., Briest, S. et al. Socio-economic disparities in long-term cancer survival—10 year follow-up with individual patient data. Support Care Cancer 25, 1391–1399 (2017). https://doi.org/10.1007/s00520-016-3528-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-016-3528-0