Abstract
Purpose
In the oncology population where malnutrition prevalence is high, more descriptive screening tools can provide further information to assist triaging and capture acute change. The Patient-Generated Subjective Global Assessment Short Form (PG-SGA SF) is a component of a nutritional assessment tool which could be used for descriptive nutrition screening. The purpose of this study was to conduct a secondary analysis of nutrition screening and assessment data to identify the most relevant information contributing to the PG-SGA SF to identify malnutrition risk with high sensitivity and specificity.
Methods
This was an observational, cross-sectional study of 300 consecutive adult patients receiving ambulatory anti-cancer treatment at an Australian tertiary hospital. Anthropometric and patient descriptive data were collected. The scored PG-SGA generated a score for nutritional risk (PG-SGA SF) and a global rating for nutrition status. Receiver operating characteristic curves (ROC) were generated to determine optimal cut-off scores for combinations of the PG-SGA SF boxes with the greatest sensitivity and specificity for predicting malnutrition according to scored PG-SGA global rating.
Results
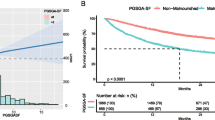
The additive scores of boxes 1–3 had the highest sensitivity (90.2 %) while maintaining satisfactory specificity (67.5 %) and demonstrating high diagnostic value (AUC = 0.85, 95 % CI = 0.81–0.89). The inclusion of box 4 (PG-SGA SF) did not add further value as a screening tool (AUC = 0.85, 95 % CI = 0.80–0.89; sensitivity 80.4 %; specificity 72.3 %).
Conclusions
The validity of the PG-SGA SF in chemotherapy outpatients was confirmed. The present study however demonstrated that the functional capacity question (box 4) does not improve the overall discriminatory value of the PG-SGA SF.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
It is well documented that the prevalence of malnutrition in the oncology population is high, yet malnutrition remains under-diagnosed and under-treated [1]. The diagnosis of a patient’s nutritional status usually consists of a detailed investigation that takes into account medical and nutritional history, as well as an anthropometric assessment [2]. Evidence-based practice guidelines recommend the use of the Scored Patient-Generated Subjective Global Assessment (PG-SGA) for nutrition assessment within the oncology patient population [1]. However, comprehensive nutrition assessment is not practical for routine use for all oncology patients in large tertiary hospitals due to time and human resource limitations [3]. It is therefore appropriate to consider a more simplified yet accurate screening process to identify patients at nutritional risk. Evidence-based practice guidelines for the nutritional management of patients receiving anti-cancer treatment [1, 4, 5] recommend routine malnutrition screening of all patients to quickly identify those at nutritional risk who would benefit from comprehensive nutritional assessment and management [6].
A number of nutrition screening tools have been developed [7–9]; however, it is the Malnutrition Screening Tool (MST) [7] that is considered the most widely used within the Australian oncology setting. Despite the speed and ease of administration of the MST, it offers limited clinically relevant information beyond weight change and appetite loss [10]. The Patient-Generated Subjective Global Assessment Short Form (PG-SGA SF), also referred to as the abridged PG-SGA, is gaining momentum as a detailed screening tool [10]. The PG-SGA SF eliminates the physical examination, disease/condition and metabolic demand assessment components of the PG-SGA but retains the medical history component (comprising weight history, food intake, nutrition impact symptoms, as well as activities and function) [10]. The PG-SGA SF has demonstrated comparable sensitivity and specificity to that of the full-length scored tool [10]. In patients with advanced non-small cell lung or gastrointestinal cancer, higher scores (≥9) from the PG-SGA SF were associated with increased hospital length of stay, decreased anthropometric measures, decreased physical measures such as handgrip and leg strength and increased mortality [11].
Previously, our group validated screening tools (including a novel, automated nutrition screening system) against the global PG-SGA category rating (i.e. SGA A, SGA B, SGA C) in the ambulatory oncology population [12]. In this study, none of the novel screening tools or the MST reached the accepted professional standard for sensitivity to identify nutritional risk. This paper is a secondary analysis of the data from that study assessing the validity of the PG-SGA SF score and deconstructed scores from components of the PG-SGA SF against the global PG-SGA category rating.
Subjects and methods
Study design
This is a secondary analysis of a single-site, cross-sectional, observational study [12]. A written informed consent was obtained from all participants. The protocol (HREC/13/QPAH/110) received was approved by the Metro South Human Research Ethics Committee.
Participants
Consecutive patients at an Australian tertiary hospital were offered study entry. Eligibility criteria included the following: aged 18 years or greater, prescribed anticancer treatment (chemotherapy, targeted therapies ± radiation therapy) received on an outpatient basis, English literate and able to provide written consent. Data were collected from April to May 2013 during routine scheduled anticancer treatment appointments by an Accredited Practising Dietitian.
Global PG-SGA category rating
The Scored PG-SGA (© FD Ottery, 2001) was developed for use with cancer patients and has been validated in ambulatory oncology settings [2, 13, 14]. This tool generates a global PG-SGA category rating for nutritional status which is analogous to the SGA rating [15] (i.e. A, well-nourished; B, moderate/suspected malnutrition; and C, severely malnourished) and a total PG-SGA score used for triaging the intensity of nutritional intervention.
PG-SGA SF scores
The PG-SGA SF generates a total score sourced from the first four boxes of the Scored PG-SGA: box 1 describes current weight, weight history and acute weight changes (scores 0–5); box 2 describes any changes in food intake over the past month (scores 0–4); box 3 lists any nutrition impact symptoms experienced over the previous 2 weeks (scores 0–23) and box 4 indicates any changes to activities and functions over the previous month (scores 0–4). The anthropometric data for box 1 were obtained from the patient medical records, where possible. As in clinical practice, if these were unavailable, self-reported data were used. All global ratings and scores were checked by a researcher (JA). Where there was any disagreement, the final decision was provided by a third researcher (EI) who independently reviewed the global PG-SGA rating and PG-SGA SF score from the source data.
Data analysis
The global PG-SGA category rating was the reference standard for validity (i.e. PG-SGA A, well-nourished, versus PG-SGA B or C, malnourished). Each box of the PG-SGA SF was scored separately to give a total score per box. These scores were analysed per box or combined with other boxes in every combination. Receiver operating characteristic (ROC) curves were used to compare sensitivity versus specificity across the PG-SGA SF box combinations for their ability to predict malnutrition at the accepted professional standard of 80 and 60 %, respectively. Higher sensitivity (percentage of malnourished correctly identified as such) is deemed more desirable in a nutritional screening tool than specificity (percentage of well-nourished correctly identified as such) [16, 17]. The results are reported only if these criteria were met. The area under the curve (AUC) is an indicator of diagnostic performance and was used to compare the test performance of the PG-SGA SF and deconstructed box scores in identifying malnutrition risk. Statistical analyses were conducted using STATA (version 13.0, 2013, StataCorp LP) [18] with statistical significance reported at P < 0.05.
Results
Three hundred participants consented to the study (96.2 % participation rate). Reasons for non-participation included treatment-associated fatigue and minimal remaining time of the chemotherapy infusion. Patient characteristics have been described elsewhere [12]. Briefly, mean age was 58.6 ± 13.4 years and 51.7 % were male. The most common cancer diagnoses were haematological (31.3 %), followed by gastrointestinal (21 %) and breast cancers (19.7 %). Overall, 83 % (n = 249) of participants were well-nourished and 17 % (n = 51) were malnourished. Data collected from box 3 (nutrition impact symptoms) reveals that 59 % of patients had problems with eating (i.e. at least one nutrition impact symptom). The most commonly reported nutrition impact symptoms included ‘no appetite,’ ‘feeling full quickly’ and ‘taste changes’ (Table 1). Malnourished patients experienced significantly more nausea, vomiting, taste changes, feeling full quickly and loss of appetite compared to well-nourished patients (Table 1).
Validity
The combinations of box scores that met the sensitivity and specificity criteria are described in Table 2. Different cut-off scores were used for these variables within the boxes of the PG-SGA SF to determine the best sensitivity, specificity and accuracy compared to the global PG-SGA category rating. Scores from boxes 1–4, 1–3 and 1 + 3 provided the best accuracy (AUC = 0.85) while meeting the sensitivity and specificity criteria at a score of ≥2.
Discussion
This study demonstrates that the PG-SGA SF is an accurate, highly sensitive and specific screening tool for malnutrition in the ambulatory oncology population, consistent with Gabrielson [10]. However, compared with the optimal cut-off score of the PG-SGA SF reported by Gabrielson (≥6, AUC = 0.96) [10], this study demonstrated a lower cut-off score of ≥3 (AUC = 0.85). This disparity may be due to the different administration methods, as scores from patient- versus dietitian-administered PG-SGA SF may not be comparable. Within Australia, where much of the validation work has been conducted, it is a standard practice for clinicians to administer the PG-SGA SF. However, the original intent was that the PG-SGA SF was to be self-administered by the patient. The authors speculate that patients are likely to over-report symptom scores based on presence alone, irrespective of their impact on nutritional intake. This would account for the higher PG-SGA SF cut-off scores reported in studies conducted outside, e.g. ≥6 Gabrielson et al. [10], versus within Australia, e.g. ≥3 Campbell et al. [19].
Compared with previous reports, the current study offers the advantage of a larger sample size, higher participation rate and more diverse oncological and haematological diagnoses, representative of the mixed diagnoses seen in the ambulatory outpatient population. Hence it mirrors actual clinical practice. The prevalence of malnutrition in this cohort, according to the global rating of the PG-SGA, was 17 %. Other studies of chemotherapy outpatients have reported malnutrition prevalence around 25 % [10, 20]. Reasons for a lower prevalence were suggested in our previous work [12]. Nutrition impact symptoms (Table 2) were common, with 59 % of patients experiencing at least one of these symptoms in the 2 weeks preceding nutritional assessment. This is comparable with previous studies by Isenring et al. [3], which found that 48 % of participants (N = 191) had at least one nutrition impact symptom, and Khalid et al. [21], who reported that 62 % (N = 161) of patients had at least one nutrition impact symptom.
There were a number of components (i.e. boxes) of the PG-SGA SF that in isolation, or when combined, provided similar accuracy (Table 2). This indicates that some of the information elicited by the PG-SGA SF might not improve its overall discriminatory ability. The additive score of boxes 1–3 and box 1 + 3 had comparable accuracy to the PG-SGA SF. The score of box 3 and the additive score of box 2 + 3 had comparable accuracy with previously reported Malnutrition Screening Tool (MST) values (AUC = 0.77) [12]. Despite comparable accuracy, the sensitivity analyses showed better performance for box 3 (82.4 %) and box 2 + 3 (82.4 %) when compared with the previously reported MST data (70.6 %) [12], indicating that these tools may be more preferable for screening purposes. The specificity analysis (Table 2) yielded >60 % for these boxes. With any screening tool, there will always be a trade-off between sensitivity and specificity. As previously stated, higher sensitivity is more desirable in nutritional screening tools than higher specificity [16, 17].
Implications for practice
It can be challenging to implement routine nutritional screening in large oncology outpatient settings. In busy, resource-stretched units, nutritional screening is not necessarily a priority and may be limited to those with visible signs of malnutrition [2]. Therefore, nutrition screening tools must be quick and simple [22]. Simple screening tools offer the benefit of not requiring the administrator to perform any calculations beyond simple addition, which is an advantage in busy clinical situations. Conversely, the PG-SGA SF provides additional clinical information that requires the calculation of percentage loss of body mass (box 1) and therefore involves additional resources. However, the food intake (box 2) plus symptom (box 3) score or symptom (box 3) score alone has acceptable sensitivity and specificity to be used for nutrition screening, eliminating the calculation from the weight history question.
Implications for research
The findings of this study indicate that PG-SGA SF and combinations of various box scores within the PG-SGA SF (Table 2) are potentially sensitive and specific malnutrition screening tools. The Scored PG-SGA and PG-SGA SF recently became available as an application on smart devices, with the intent to support health care professionals to implement easy and systematic nutritional assessment and facilitate consistent scoring and use of validated multilingual translations (Pt-Global 2014 [23]). This application uses an algorithm to generate scores and global ratings. An updated paper-based version of the Scored PG-SGA (version 3.22.15) has also been released with additions and interpretive differences which have implications for scoring that have yet to be validated. Future studies should investigate the validity of the tool in its electronic form and its updated paper-based form.
The strengths of this study include the use of a valid and reliable nutrition assessment tool to assess nutritional status for comparison and a large representative sample with an excellent participant response rate. Limitations of this study include the following: (1) this study was a secondary analysis of data collected for our primary study [12] and (2) the PG-SGA SF score and the global SGA category rating (nutritional status) are not independent as the PG-SGA SF also generates data used for decision-making regarding the global SGA category rating.
Conclusion
Nutritional screening enables the proactive identification of patients at risk of malnutrition and the opportunity to act prior to malnutrition onset to prevent further deterioration in nutritional status [22]. Our study supports the implementation of the PG-SGA SF as a simple and accurate method to detect malnutrition risk when administered by the dietitian. The PG-SGA SF and additive score combinations of the first three boxes all had higher sensitivity than the MST and the automated tool in our previous analyses [12]. Where resources allow, the PG-SGA SF is useful in assisting clinicians in the identification of patients at malnutrition risk who warrant comprehensive nutrition assessment.
References
Isenring E, Zabel R, Bannister M, Brown T, Findlay M, Kiss N, Loeliger J, Johnstone C, Camilleri B, Davidson W, Hill J, Bauer J (2013) Updated evidence-based practice guidelines for the nutritional management of patients receiving radiation therapy and/or chemotherapy. Nutr Dietetics 70(4):312–324. doi:10.1111/1747-0080.12013
Bauer J, Capra S, Ferguson M (2002) Use of the Scored Patient-Generated Subjective Global Assessment (PG-SGA) as a nutrition assessment tool in patients with cancer. Eur J Clin Nutr 56(8):779–785. doi:10.1038/sj.ejcn.1601412
Isenring E, Cross G, Kellett E, Koczwara B, Daniels L (2010) Nutritional status and information needs of medical oncology patients receiving treatment at an Australian public hospital. Nutr Cancer 62(2):220–228. doi:10.1080/01635580903305276
Evidence based practice guidelines for the nutritional management of malnutrition in adult patients across the continuum of care (2009). Nutrition & Dietetics 66:S1-S34. doi:10.1111/j.1747-0080.2009.01383.x
Bauer JD, Ash S, Davidson WL, Hill JM, Brown T, Isenring EA, Reeves M (2006) Evidence based practice guidelines for the nutritional management of cancer cachexia. Nutr Dietetics 63:S3–S32. doi:10.1111/j.1747-0080.2006.00099.x
Skipper A, Ferguson M, Thompson K, Castellanos VH, Porcari J (2012) Nutrition screening tools: an analysis of the evidence. JPEN J Parenter Enteral Nutr 36(3):292–298. doi:10.1177/0148607111414023
Ferguson ML, Bauer J, Gallagher B, Capra S, Christie DR, Mason BR (1999) Validation of a malnutrition screening tool for patients receiving radiotherapy. Australas Radiol 43(3):325–327
Rubenstein LZ, Harker JO, Salva A, Guigoz Y, Vellas B (2001) Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). J Gerontol A Biol Sci Med Sci 56(6):M366–M372
Kondrup J, Rasmussen HH, Hamberg O, Stanga Z (2003) Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr 22(3):321–336
Gabrielson DK, Scaffidi D, Leung E, Stoyanoff L, Robinson J, Nisenbaum R, Brezden-Masley C, Darling PB (2013) Use of an abridged Scored Patient-Generated Subjective Global Assessment (abPG-SGA) as a nutritional screening tool for cancer patients in an outpatient setting. Nutr Cancer 65(2):234–239. doi:10.1080/01635581.2013.755554
Vigano AL, di Tomasso J, Kilgour RD, Trutschnigg B, Lucar E, Morais JA, Borod M (2014) The abridged Patient-Generated Subjective Global Assessment is a useful tool for early detection and characterization of cancer cachexia. J Acad Nutr Diet 114(7):1088–1098. doi:10.1016/j.jand.2013.09.027
Abbott J, Teleni L, McKavanagh D, Watson J, McCarthy A, Isenring E (2014) A novel, automated nutrition screening system as a predictor of nutritional risk in an oncology day treatment unit (ODTU). Support Care Cancer 22(8):2107–2112. doi:10.1007/s00520-014-2210-7
Bauer J, Capra S (2003) Comparison of a malnutrition screening tool with subjective global assessment in hospitalised patients with cancer–sensitivity and specificity. Asia Pac J Clin Nutr 12(3):257–260
Isenring E, Bauer J, Capra S (2003) The Scored Patient-Generated Subjective Global Assessment (PG-SGA) and its association with quality of life in ambulatory patients receiving radiotherapy. Eur J Clin Nutr 57(2):305–309. doi:10.1038/sj.ejcn.1601552
Detsky AS, McLaughlin JR, Baker JP, Johnston N, Whittaker S, Mendelson RA, Jeejeebhoy KN (1987) What is subjective global assessment of nutritional status? JPEN J Parenter Enteral Nutr 11(1):8–13
Healy E, Yaxley A, Isenring E, Bannerman E, Miller M (2014) Ability of existing malnutrition screening tools to identify risk of starvation, sarcopenia and cachexia: a systematic review. e-SPEN. Journal 9(3):e109–e122. doi:10.1016/j.clnme.2014.04.005
Isenring EA, Banks M, Ferguson M, Bauer JD (2012) Beyond malnutrition screening: appropriate methods to guide nutrition care for aged care residents. J Acad Nutr Diet 112(3):376–381. doi:10.1016/j.jada.2011.09.038
Stata Statistical Software (2013) Release, 13 edn. StataCorp LP, TX
Campbell KL, Bauer JD, Ikehiro A, Johnson DW (2013) Role of nutrition impact symptoms in predicting nutritional status and clinical outcome in hemodialysis patients: a potential screening tool. J Ren Nutr 23(4):302–307. doi:10.1053/j.jrn.2012.07.001
Davidson W, Teleni L, Muller J, Ferguson M, McCarthy AL, Vick J, Isenring E (2012) Malnutrition and chemotherapy-induced nausea and vomiting: implications for practice. Oncol Nurs Forum 39(4):E340–E345. doi:10.1188/12.onf.e340-e345
Khalid U, Spiro A, Baldwin C, Sharma B, McGough C, Norman AR, Eisen T, O’Brien ME, Cunningham D, Andreyev HJ (2007) Symptoms and weight loss in patients with gastrointestinal and lung cancer at presentation. Support Care Cancer 15(1):39–46. doi:10.1007/s00520-006-0091-0
Davies M (2005) Nutritional screening and assessment in cancer-associated malnutrition. Eur J Oncol Nurs 9(Suppl 2):S64–S73. doi:10.1016/j.ejon.2005.09.005
Pt-Global (2014) Pt-Global innovation in nutritional care. http://pt-global.org/. Accessed January 8 2015
Acknowledgments
This project was funded by the Dietitians Association of Australia (DAA) Small Grant 2013 and the Queensland Health Practitioner Research Grant Scheme 2013–2014.
Author’s contribution
All authors read and approved the final manuscript. JA carried out the study and prepared the manuscript. JA and LT were responsible for the conception and study design, statistical analysis and interpretation. DM advised on Charm software. EI, LT, AM, and DM provided interpretation and critical revision of the article. JA and JW participated in the acquisition of data and literature review. EI supervised the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
A written informed consent was obtained from all participants. The protocol (HREC/13/QPAH/110) received was approved by the Metro South Human Research Ethics Committee.
Conflict of interest
The authors declare that we have no conflicts of interest. We acknowledge that we have full control of all primary data and agree to allow the journal to review the data if requested.
Rights and permissions
About this article
Cite this article
Abbott, J., Teleni, L., McKavanagh, D. et al. Patient-Generated Subjective Global Assessment Short Form (PG-SGA SF) is a valid screening tool in chemotherapy outpatients. Support Care Cancer 24, 3883–3887 (2016). https://doi.org/10.1007/s00520-016-3196-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-016-3196-0