Abstract
Purpose
The use of chemotherapy in the last month of life (CLML) of cancer patients is considered an aggressive approach to be avoided. We examined the practice of CLML in Lebanese cancer patients, and we investigated patient and tumor characteristics that justify this practice. To our knowledge, this is the first study describing CLML of Middle Eastern patients with advanced cancer.
Methods
We conducted this study at Hotel-Dieu de France University Hospital (HDF), Lebanon. Cases eligible for this study were all individuals diagnosed with cancer who died at HDF between the 1st of January and the 31st of December 2014. Demographic and clinical characteristics of the patients were obtained from the hospital registration records. Data concerning the management plan, primary malignancy and stage, chemo-sensitivity, line, type, and timing of chemotherapy in the last month of life were also obtained.
Results
Among the 130 cancer patients who were enrolled, CLML was administered to a total of 55 patients (42.3 %), of whom 26 patients (50 %) received more than one cytotoxic drug. Oral drug was only given to 9 patients (16.4 %). Interestingly, CLML increased the risk of death in the last month of life (p = 0.02), yet progression of disease constituted the major cause of death in this subgroup (54.6 %). The only variable to have statistical significant correlation with CLML was performance status (p = 0.03). The type of tumor and recent diagnosis of less than 2 months were also correlated to CLML (p = 0.03 and 0.024, respectively).
Conclusion
The high percentage of patients receiving CLML underlines the difficulty of end-of-life discussions in patients from Middle Eastern societies. This is true in the context of a country with little availability of palliative care resources, where health policies should be more focused on incorporating palliative medicine in all medical strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Most practitioners, particularly oncologists, are in the habit of continuously administering treatments at advanced stages of the disease where the chances of response are uncertain [1]. Over-treatment is a major concern when physicians disregard this concept for religious and social reasons and overestimate survival through wishful optimism. Another concern is the possible adverse effects from the administered treatment that sometimes accelerate the patient’s degradation process. An alternative option to the curative approach is to rationalize the purpose of treatment into a palliative approach [2]. Effectively, it is through rigorous communication between the physician and their patients that a balance between the expected advantages and disadvantages of cytotoxic treatment should be assessed.
Unfortunately, physicians often come to face the difficult decision of referring these patients to a hospice/palliative care program in the absence of clear recommendations guiding these decisions [3]. The only studies assessing patient characteristics for eligibility to receive cytotoxic therapy go back to the 1980s, where the patients’ performance status and response to previous evidence-based interventions were the only determinants of future therapeutic approaches [4]. Several other possible indicators were suggested, but these are often overlooked by the attending physician who is more concerned with the impact of his actions as they are perceived by the patients and their families [2]. As shown in the literature, this results in a wide variation in the percentage of patients receiving chemotherapy in the last month of life (CLML) among different populations, since most of the studied indicators underestimate the psychological, social, and religious beliefs of both physicians and patients.
Recently, the concept of mortality within 30 days of chemotherapy has been considered as an indicator of the quality of care, and even more studies emerged to assess its actual status. Interestingly, numbers varied significantly between different countries, with rates of CLML ranging between 4.4 and 55.6 % [5]. Such variations highlight the fundamental role of social awareness in accepting the palliative concept whereby physicians are assisted in taking on a rational management plan. In this context, family dynamics play a major role in the practical and emotional aspects of patient care. Emerging social analysis suggests that management planning, which should involve the patient together with his physician and loved ones, is essential for cancer care despite being burdensome in the last days of life [6]. Another major intervening factor comes in the form of religious beliefs that also affect care decision, as most patients erroneously believe that treatment will most definitely be curative owing to the intervention of a certain deity [7, 8].
The Lebanese society, located in the Mediterranean shores, is traditionally conservative with strong religious beliefs and even stronger family bonds where cultural ideals assume positive intergenerational relations. Analysis of the social status of the Lebanese population demonstrated a link between family relations and overall well-being. These particular characteristics underline very interesting family dynamics that affect the management plan in dying patients [9]. Moreover, palliative care medicine is not yet well accepted in the Lebanese society, especially since most hospitals lack such departments and most universities leave out this discipline from their curriculum [10]. Consequently, a patient diagnosed with terminal cancer is often unknowingly alienated from the management plan of his own disease, leaving the final decision to the “family unit,” which is often more concerned with maintaining life, rather than quality of life, in hope of restoring their loved one to his former self through chemotherapy and providence.
To our knowledge, the use of CLML in the Middle Eastern societies was never assessed. Therefore, the purpose of this study is to determine the characteristics of the patients receiving CLML. Included in this assessment is the medical aspect of the patient only.
Patients, materials, and methods
Study design and setting
We conducted our study at Hotel Dieu de France University Hospital (HDF), Lebanon, a multidisciplinary tertiary hospital serving in a rural area. This hospital is affiliated to the Faculty of Medicine of Saint Joseph University, one of the leading medical universities in Lebanon and the first to inaugurate the palliative concept in the medical curriculum. Hospital records of all admitted patients are available.
Participants
Eligible patients included Lebanese patients with an end-stage cancer diagnosis that died at our hospital between the 1st of January and the 31st of December 2014. We defined end-stage cancer by distant metastasis or disease refractory to ≥1 line of chemotherapy. Participants should be at least 18 years old with an estimated life expectancy of ≤6 months. We only excluded foreign patients, those with missing data, and those younger than 18 years of age. An approval of the institutional review board of the Faculty of Medicine of Saint Joseph University was obtained.
Data source and variables
Demographic and clinical characteristics of the patients were obtained from the hospital registration records. We retained information on age, gender, associated co-morbidities, performance status, cause of death, and time spent in hospital in the last month of life. Data concerning the management plan, primary malignancy with its stage at diagnosis and at the last month of life, chemo-sensitivity and line of treatment, and type and timing of chemotherapy in the last month of life were also obtained. We defined chemo-sensitivity by a response rate of 50 % or more with first-line chemotherapy for lymphomas, small cell of the lung, colorectal, ovarian, breast, and germ cell cancers. All other tumor types were considered chemo-resistant. Patients diagnosed with a malignancy in the last 2 months were included in the “newly diagnosed” subgroup. The change of the tumor burden was assessed via the revised RECIST version 1.1 guideline [11].
Statistical methods
SPSS 20.0 software was used for statistical analysis. Our clinical data is expressed in mean ± standard deviation (SD), median, or percentage. The relationships between each of the variables are assessed by t test, chi–square, and exact Fisher correlation. Multivariate analysis was assessed by a binary logistic regression [Method ENTER]. A p value <0.05 is considered significant.
Results
Characteristics of the population
One hundred thirty cases fulfilled the eligibility criteria and were included in this study. Sixty-seven were males (51.5 %) and 63 were females (48.5 %). The mean age was 65 ± 13 years (Table 1). Lung, colorectal, and breast cancer are the most common tumors with 16.9 % (22 patients), 16.2 % (21 patients), and 10.8 % (14 patients), respectively (Table 2). Only 5 patients (3.8 %) had chemo-sensitive tumors, whereas 125 patients (96.2 %) had chemo-resistant tumors. One hundred six patients (92.2 %) had stage IV disease followed by stage III in 8 patients (7.8 %). Newly diagnosed tumor was found in 18 patients (13.8 %).
Description of the management plan in the last month of life
Among the 130 patients, 52 patients (40.2 %) had imaging investigations in the last month of life with CT scan being the most frequent imaging modality in 33 patients (64.7 %). Progression of disease was the most common cause of death in 66 patients (50.8 %) followed by septic shock in 29 patients (22.3 %). Ninety-three patients (71.5 %) spent more than 14 days of their last month in hospital and only 9 patients (6.9 %) were admitted to the intensive care unit (Table 3).
Overall, CLML was administered to a total of 55 patients (42.3 %). The duration between death and the first day of chemotherapy administration had a mean of 16 ± 9 days (range 1–30 days). As for type of therapy, 26 patients (47.3 %) were given more than one cytotoxic drug. Oral drug, including oral 5 FU and targeted therapies, was given to 9 patients (16.4 %), whereas drug administration by intravenous injection was given to 46 patients (83.6 %) (Table 4). Interestingly, CLML increased the risk of death in the last month of life (OR = 1.6; CI = 95 % [1.1–2.4] p = 0.02), yet progression of disease constituted the major cause of death in this subgroup (54.6 %).
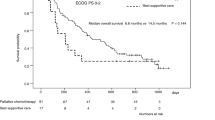
Correlations between the characteristics of the population and management plan
Our data demonstrated that the aggressive management plan was only significantly correlated to the performance status (PS) of the individuals (p = 0.03). Moreover, the tumor characteristics correlated to CLML were the type of tumor and the recent diagnosis of less than 2 months (p = 0.03 and 0.024, respectively). While hematological tumors compared to solid tumors were more likely to receive CLML (OR: 0.299; CI 95 %: 0.096–0.932), patients diagnosed with cancer in the last 2 months had an increased chance of receiving CLML (p = 0.02). Multivariate analysis concluded to the statistical significance of the ECOG-PS score only.
Discussion
During the last two decades, cancer therapeutics have provided remarkable improvements in terms of survival and quality of life for otherwise severely ill patients. The advent of such efficient therapeutic approaches has led to the administration of successive lines of therapy to patients who would scarcely be considered for more than one line of cytotoxic therapy in the past. Despite these monumental advances, an increased frequency and aggressiveness of CLML might not always be a sound decision since most patients diagnosed at an advanced stage will eventually die from their disease and cytotoxic therapy might even contribute to that demise through sheer toxicity, an act that goes against our primary directive as physicians: “Primum Non Nocere” [1, 12]. This poses a moral dilemma for practitioners particularly in Middle Eastern societies where social and religious beliefs hamper the implementation of western models of autonomy and patient-centered care [13, 14].
In comparison with similar data from other countries, the mean age at diagnosis, the types of cancer, and the gender ratios for patients receiving CLML are comparable (Table 5). Unfortunately, most of these studies did not report the performance status of their participants although it is considered the major determinant of CLML. Our study shows that 42.3 % of cancer patients received CLML with 18.5 % receiving chemotherapy within the last 2 weeks of their life. These numbers exceed most of the reported percentages except for Spain and the USA that attribute their findings to cultural and social constraints that are similar to those observed in Middle Eastern societies. The high rates of CLML were attributed to the younger age of the involved patients, denial, refusal of accepting the terminal diagnosis, and lack of proper palliative management that resulted in such [15]. All of the elements being applicable to our own patient population, it is arguable that a Mediterranean, rather than a Middle Eastern, cultural background is mostly to blame for such unwavering refusal of palliative care. It is noteworthy that our findings may exceed those of other countries because of a time bias defined by the increased worldwide trend to administer CLML in the era of notable therapeutic advances [1, 12, 16].
In line with literature, our experience reports lung, colorectal, and breast cancer as the most common neoplasia receiving CLML (Table 5). This finding is supported by a previous work by Weeks et al. who demonstrated that this subgroup of patients believes erroneously that chemotherapy will cure them [17]. Moreover, one sound basis for the high percentage of CLML in our series would be the case of hematological malignancies, which often present with widespread disease and are more likely to respond to chemotherapy, thus providing patients with a longer survival. Our patients did have an increased likelihood of receiving CLML when diagnosed with a hematological malignancy for the same scientific reasons as patients in other parts of the world [16]. Although patients with severely debilitating lymphoproliferative and myeloproliferative syndromes might present with markedly altered general status, chances are that a good proportion of these patients will benefit from an aggressive initial approach rather than succumb to it, provided that there are no other interfering co-morbidities.
Tumor sensitivity to chemotherapy is another possible determinant of CLML that is often unrecognized in published data. Interestingly, our data demonstrates tumor sensitivity in 3.8 % of patients receiving CLML and thus highlights the disregard to guidelines that would dissuade physicians from administering therapy whenever resistance occurs [18]. This finding could be explained by the higher performance status and percentage of newly diagnosed patients in our series. Nevertheless, imaging feedback used in 64.7 % of our patients may also affect the management plan although it was not statistically significant.
Despite the fact that disease progression was cited as the primary cause of death in more than half of the patients receiving CLML, our study demonstrates that administering CLML significantly increases the risk of death. Such an elevated rate of disease progression accounting for the primary cause of death constitutes a plausible rationale for justifying CLML. Effectively, one study of CLML in colorectal cancer advocated for a stabilization of the quality of life and psychosocial symptoms, but more robust evidence is needed before definite conclusions can be made [19]. Moreover, it would be naive to assume that the physical stress endured after chemotherapy does not contribute in any way to the patient’s demise. Debilitating fatigue and limited physical activity secondary to chemotherapy usually result in increased morbidity and altered quality of life [20]. It is noteworthy that the majority of our patients received more than one cytotoxic agent and, surprisingly, chemotherapy-naive patients were not subjected to more aggressive treatment regimens since performance status was ultimately taken into consideration. Unfortunately, very few patients received oral agents despite patient preferences to avoid hospitalizations [21]. However, oral chemotherapy is only approved for few types of cancer and not all patients are likely to benefit from this approach, which also carries the risk of added toxicity [22]. Furthermore, patients in the palliative care settings have seen a decrease in the administration of intravenous chemotherapy but not oral chemotherapy during at the end of life, thus providing somewhat of a measure as to the preferences of “lighter” therapeutic interventions in terminally ill patients [23].
Our results demonstrated that a good PS, the diagnosis of hematological malignancies, and a recent diagnosis of less than 2 months are relevant determinants of CLML. These factors seem to differ between countries where age, tumor chemosensitivity, and mode of treatment administration seem to affect the decision of CLML [24–27]. Nevertheless, all these studies undermined the psychosocial/religious effect and the presence of a palliative approach on the management plan at end of life.
Our study has several strength points including the real-world description of our sample. We also report a comprehensive assessment of patient demographics and physical and clinical characteristics in their last month of life. Moreover, we report the details of the management plan taking into consideration imaging tests as well as type and mode of administration of chemotherapy not analyzed in other reported studies. On the other hand, our study is limited by its retrospective status. This also restrained an analysis of the psychosocial determinants and the quality of life of our participants.
Conclusion
Our analysis of the demographic and clinical and physical characteristics failed to establish a complete assessment of the determinants of CLML, but a good PS, hemoproliferative disorders, and a recent diagnosis of less than 2 months seem to be consistently associated with this practice. The cultural specs of our Middle Eastern country, based on family ties and religious values, may also add to the high percentage of patients receiving CLML. Such over-treatments remain frequent despite the current recommendations to limit CLML as it seems to cause more harm that benefit even in the palliative settings. Published reports to date describe an increased frequency of CLML with wide variations of its use between countries and examine variable determinants of CLML. Therefore, it is fundamental that these recommendations be tailored according to each society and more specifically to each patient in this era of personalized medicine.
References
Earle CC, Neville BA, Landrum MB, Ayanian JZ, Block SD, Weeks JC (2004) Trends in the aggressiveness of cancer care near the end of life. J Clin Oncol Off J Am Soc Clin Oncol 22(2):315–321
Braga S (2011) Why do our patients get chemotherapy until the end of life? Ann Oncol Off J Eur Soc Med Oncol 22(11):2345–2348
Tanneberger S, Malavasi I, Mariano P, Pannuti F, Strocchi E (2002) Planning palliative or terminal care: the dilemma of doctors’ prognoses in terminally ill cancer patients. Ann Oncol Off J Eur Soc Med Oncol 13(8):1320–1322, author reply 1322–3
Schnipper LE, Smith TJ, Raghavan D, Blayney DW, Ganz PA, Mulvey TM et al (2012) American Society of Clinical Oncology identifies five key opportunities to improve care and reduce costs: the top five list for oncology. J Clin Oncol Off J Am Soc Clin Oncol 30(14):1715–1724
O’Brien MER, Borthwick A, Rigg A, Leary A, Assersohn L, Last K et al (2006) Mortality within 30 days of chemotherapy: a clinical governance benchmarking issue for oncology patients. Br J Cancer 95(12):1632–1636
van Eechoud IJ, Piers RD, Van Camp S, Grypdonck M, Van Den Noortgate NJ, Deveugele M et al (2014) Perspectives of family members on planning end-of-life care for terminally ill and frail older people. J Pain Symptom Manag 47(5):876–886
Jaul E, Zabari Y, Brodsky J (2014) Spiritual background and its association with the medical decision of, DNR at terminal life stages. Arch Gerontol Geriatr 58(1):25–29
Mack JW, Walling A, Dy S, Antonio ALM, Adams J, Keating NL et al (2015) Patient beliefs that chemotherapy may be curative and care received at the end of life among patients with metastatic lung and colorectal cancer. Cancer 121(11):1891–1897
Ajrouch KJ, Abdulrahim S, Antonucci TC (2015) Family relations and health over the life course. A Lebanese perspective. J Méd Liban 63(1):8–14
Naifeh Khoury M (2008) Palliative care education in Lebanon: past endeavors and future outlook. J Méd Liban 56(2):83–85
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R et al. (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer Oxf Engl 1990;45(2):228–47
Lee HS, Chun KH, Moon D, yeon HK, Lee S, Lee S (2015) Trends in receiving chemotherapy for advanced cancer patients at the end of life. BMC Palliat Care [Internet]. [cited 2015 Aug 11];14. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4365766/
Doumit MAA, Abu-Saad Huijer H, Kelley JH (2007) The lived experience of Lebanese oncology patients receiving palliative care. Eur J Oncol Nurs 11(4):309–319
Hamadeh GN, Adib SM (1998) Cancer truth disclosure by Lebanese doctors. Soc Sci Med 47(9):1289–1294
Sanz Ortiz J (2012) Chemotherapy at the end of life: up until when? Clin Transl Oncol Off Publ Fed Span Oncol Soc Natl Cancer Inst Mex 14(9):667–674
Ho TH, Barbera L, Saskin R, Lu H, Neville BA, Earle CC (2011) Trends in the aggressiveness of end-of-life cancer care in the universal health care system of Ontario, Canada. J Clin Oncol Off J Am Soc Clin Oncol 29(12):1587–1591
Weeks JC, Catalano PJ, Cronin A, Finkelman MD, Mack JW, Keating NL et al (2012) Patients’ expectations about effects of chemotherapy for advanced cancer. N Engl J Med 367(17):1616–1625
Ahn DH, Bekaii-Saab T (2014) Ampullary cancer: an overview. Am Soc Clin Oncol Educ Book ASCO Am Soc Clin Oncol Meet. 112–5
Mayrbäurl B, Giesinger JM, Burgstaller S, Piringer G, Holzner B, Thaler J (2015) Quality of life across chemotherapy lines in patients with advanced colorectal cancer: a prospective single-center observational study. Support Care Cancer Off J Multinatl Assoc Support Care Cancer
Gilliam LAA, St Clair DK (2011) Chemotherapy-induced weakness and fatigue in skeletal muscle: the role of oxidative stress. Antioxid Redox Signal 15(9):2543–2563
Liu G, Franssen E, Fitch MI, Warner E (1997) Patient preferences for oral versus intravenous palliative chemotherapy. J Clin Oncol Off J Am Soc Clin Oncol 15(1):110–115
Gandara DR, Gumerlock PH (2005) Epidermal growth factor receptor tyrosine kinase inhibitors plus chemotherapy: case closed or is the jury still out? J Clin Oncol 23(25):5856–5858
Greer JA, Pirl WF, Jackson VA, Muzikansky A, Lennes IT, Heist RS et al (2012) Effect of early palliative care on chemotherapy use and end-of-life care in patients with metastatic non-small-cell lung cancer. J Clin Oncol Off J Am Soc Clin Oncol 30(4):394–400
Sezgin Goksu S, Gunduz S, Unal D, Uysal M, Arslan D, Tatlı AM et al (2014) Use of chemotherapy at the end of life in Turkey. BMC Palliat Care 13(1):51
Kao S, Shafiq J, Vardy J, Adams D (2009) Use of chemotherapy at end of life in oncology patients. Ann Oncol Off J Eur Soc Med Oncol 20(9):1555–1559
Prigerson HG, Bao Y, Shah MA, Paulk ME, LeBlanc TW, Schneider BJ. et al. (2015) Chemotherapy Use, Performance Status, and Quality of Life at the End of Life. JAMA Oncol
Mohammed AA, Al-Zahrani AS, Ghanem HM, Farooq MU, El Saify AM, El-Khatib HM (2015) End-of-life palliative chemotherapy: where do we stand? J Egypt Natl Cancer Inst 27(1):35–39
Martoni AA, Tanneberger S, Mutri V (2007) Cancer chemotherapy near the end of life: the time has come to set guidelines for its appropriate use. Tumori 93(5):417–422
Keam B, Oh D-Y, Lee S-H, Kim D-W, Kim MR, Im S-A et al (2008) Aggressiveness of cancer-care near the end-of-life in Korea. Jpn J Clin Oncol 38(5):381–386
Acknowledgments
None.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Assi, T., El Rassy, E., Tabchi, S. et al. Treatment of cancer patients in their last month of life: aimless chemotherapy. Support Care Cancer 24, 1603–1608 (2016). https://doi.org/10.1007/s00520-015-2959-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-015-2959-3