Abstract
Purpose
This study evaluated the efficacy of a self-guided Web-based cognitive behaviour therapy (CBT) intervention compared to an attention control in improving cancer-related distress, health-related quality of life (HRQOL), and maladaptive coping, among people recently diagnosed with cancer.
Methods
Sixty individuals with cancer diagnosed in the previous 6 months and receiving treatment with curative intent were randomised to receive either the 6-week intervention Cancer Coping Online (CCO: n = 30) or the 6-week Web-based attention control (n = 30). Outcome measures, including cancer distress (the Posttraumatic Stress Scale—Self-Report), general distress (Depression Anxiety Stress Scale), quality of life (EORTC QLQ-C30), and coping (mini-MAC), were administered at baseline, immediately post-intervention, and at 3 and 6 months post-intervention.
Results
Significant main effects for time were found for cancer distress, global QOL, physical function, role function, social function, and anxious preoccupation. Post hoc between-group comparisons showed CCO participants had statistically significantly higher physical functioning compared to controls at 3 months of follow-up (d = −0.52, p = 0.02). Furthermore, compared to controls, post hoc comparisons found moderate between-group effect sizes favouring CCO post-intervention for cancer distress (d = 0.43) and anxious preoccupation (d = 0.38), and at 6 months of follow-up for global QOL (d = −0.43).
Conclusions
These results provide preliminary support for the potential efficacy of a self-guided Web-based CBT programme in improving aspects of HRQOL, cancer-related distress, and anxious preoccupation after cancer diagnosis. This paper provides justification for, and will help inform the development of, subsequent larger multi-site studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Despite the demonstrable evidence base supporting the use of psychosocial treatments for cancer distress [1, 2], many barriers to their success in traditional face-to-face settings exist. These range from geographic barriers, particularly for those living in rural or remote areas [3], to personal and illness-related barriers, including the ongoing stigma associated with seeking mental health assistance [4, 5] and service barriers, with the demand exceeding the current level of funding for psycho-oncologists [4, 6]. As a result, researchers have started investigating the Internet as a treatment delivery modality for cancer distress [4, 5, 7], and there is a growing evidence base for self-guided Web-based interventions for physical health complaints [5, 7].
Given that 84 % of Australians have access to the Internet [8], Web-based interventions are a logical format for the wide dissemination of evidence-based psychological treatment for cancer patients. However, the evidence base for self-guided Web-based psychological therapy specific to cancer distress is only now emerging, with four pilot/preliminary randomised controlled trials (RCTs) [9–12] and one case series study [13] published to date. All studies investigated curatively treated cancer patients or survivors, including early-stage breast cancer [9, 11], localised prostate cancer [12], and heterogeneous cancer survivors [10, 13]. Of the RCTs, two were pilot studies [10, 11] that were limited by small sample sizes (31 and 62 participants, respectively) and were therefore underpowered to detect statistically significant effects; however, moderator analyses found significant intervention effects for those with poor perceived baseline health status [11] or high baseline distress [10].
The other two RCTs were large [9, 12] and sufficiently powered to find intervention effects. Carpenter et al. [9] found that although the discussion forum component was not well utilised, their programme improved self-efficacy for coping with breast cancer, regulating negative mood, and reducing cancer-related post-traumatic symptoms [9]. In contrast, Wootten et al. [14] found their programme significantly reduced distress among men with prostate cancer who had access to the programme combined with an asynchronous discussion forum, when compared to a forum-only condition (a third programme-only condition did not significantly differ from the other two conditions).
In contrast to the above RCTs which contained asynchronous group support as a key feature of their programmes, our group tested a purely self-guided Web-based intervention (i.e. no forum) for newly diagnosed cancer patients in 2011 [13]. The decision to omit a forum was primarily due to the currently conflicting evidence base for its inclusion in health populations [5]. Our small case series study of 12 participants found that the intervention reduced distress and maladaptive coping at post-treatment as evidenced by the small-to-moderate effect sizes.
Collectively, these five studies demonstrate the promise of Web-based formats for delivering psychosocial programmes for cancer; however, they all suffer from either (a) being small, underpowered, or uncontrolled feasibility studies or (b) not evaluating the longer-term impact of the intervention. Therefore, the present study aimed to extend our earlier findings testing the feasibility of the Cancer Coping Online (CCO) intervention [13] by conducting an RCT evaluating the efficacy of CCO compared to an attention control over a 6-month follow-up period.
Methods
Participants
Participants were cancer patients receiving treatment at a single institution who met the following eligibility criteria: (i) cancer being treated with curative intent, (ii) aged 18+ years, (iii) receiving active treatment or were within 6 months of diagnosis, (iv) spoke sufficient English for informed consent and programme use, and (v) had Internet access. Participants were recruited between 1 March 2011 and 15 November 2012, with data collection completed on 30 June 2013.
Procedure
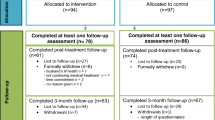
Procedural elements of this study conformed to the CONSORT statement and checklist [15, 16]. Participants were recruited via local media advertisements and referrals from cancer clinicians. Interested patients were contacted by the research team, provided with detailed information about the study, and directed to the Website to enrol (comprised of an eligibility screen, information sheet and consent form, and baseline assessment). Informed consent was obtained from all individual participants included in the study. After enrolment, participants were randomised in blocks of 2 to receive either the intervention or the Web-based control condition. Randomisation occurred via a computer-generated block random allocation where the sequence was concealed until conditions were assigned. Participants worked through the six intervention modules sequentially (new modules were released weekly with an email reminder to use the programme). After completing module 6, participants were automatically directed to the post-treatment assessment. Participants who did not immediately complete the post-treatment assessment were sent email reminders 1 and 2 weeks later, with a single telephone reminder used 3 weeks later for non-responders. This same procedure was adopted for the 3- and 6-month assessments. Figure 1 illustrates the flow of participants through the study. Ethics approval was obtained from the Southern Adelaide Clinical Human Research Ethics Committee, and the study is registered with the Australian New Zealand Clinical Trials Registry (registration number: ACTRN12613001170718).
Intervention conditions
CCO is a six-module password-protected cognitive behaviour therapy (CBT) programme, where each module is comprised of three key elements: (a) psycho-education, (b) CBT-based activities, including worksheets, quizzes, and relaxation and meditation exercises, and (c) written survivor testimonials and quotes [13]. Designed for patients currently receiving treatment for curatively treated cancer, the programme was adapted from an evidence-based print workbook [17]. CCO addresses the most commonly reported physical, psychological, and social concerns experienced during treatment, with the six modules addressing (i) starting treatment—working with your medical team, covering assertive communication and decision-making; (ii) coping with physical symptoms and side effects—including fatigue, pain, and insomnia—and providing activity pacing worksheets and relaxation audio tracks; (iii) coping with emotional distress—which covers depression, anxiety, anger, and stress—and providing cognitive restructuring diaries and mindfulness audio tracks; (iv) body image, identity, and sexuality—with psychosexual worksheets and therapeutic writing activities; (v) your family and friends—comprising further assertive communication and needs assessment worksheets; and (vi) completing treatment, which includes self-management strategies to facilitate healthy lifestyles. CCO also contains an online personal journal/blog and a resources section with links to reputable cancer-related organisations and other health websites.
Web-based control condition
An information-only version of CCO was developed for this study to provide an appropriate control for demand characteristics and participant expectancies. The control condition contained the same six information topics as the intervention but none of the worksheets, activities, relaxation/meditation exercises, or journal. Previous research indicates that an information-only control condition does not significantly reduce distress [17], and having a Web-based control is the recommended strategy for testing the efficacy of Internet interventions [18].
Measures
Participants were emailed links to the online assessments at baseline (pre-treatment), post-treatment (immediately upon completing the programme), 3 months post-treatment, and 6 months post-treatment. The battery was comprised of the following measures, which all have excellent psychometric properties.
Participant characteristics (baseline only)
Demographic measures included age, marital status, occupational status, annual gross income, level of educational attainment, area of residence (rural, urban, state), and contact details. Medical treatment measures included cancer type, date of diagnosis, treatment received (surgery, chemotherapy, radiotherapy, hormonal therapy, other), and any other chronic health conditions.
Distress
Two measures of distress were evaluated: cancer-specific distress and general distress. The 17-item Posttraumatic Stress Scale—Self Report (PSS-SR) [19] was utilised as a measure of cancer-specific distress. This scale measures the severity of each DSM-IV post-traumatic stress disorder symptom criterion. Participants indicate how often they experienced each symptom in the previous week. Total scores range from 0 to 51, with higher scores indicating higher PTSD symptomatology. In the present study, the PSS-SR had a strong internal consistency reliability, α = 0.90. General distress was measured using the total scale score of the Depression Anxiety Stress Scale short form (DASS) [20]. This 21-item scale assesses symptoms of anxiety, depression, and stress over the previous week. Scores range from 0 to 126, with higher scores indicating higher distress. In the present study, the DASS had a strong internal consistency reliability, α = 0.94.
HRQOL
Five QOL domains with acceptable internal consistency reliability were assessed using the European Organisation for Research and Treatment of Cancer quality of life core questionnaire (EORTC QLQ-C30: [21]): global QOL (α = 0.86), physical functioning (α = 0.80), role functioning (α = 0.89), emotional functioning (α = 0.87), and social functioning (α = 0.86). Total scores range from 0 to 100, with higher scores indicating better functioning.
Coping
Three coping styles with acceptable internal reliability (helplessness/hopelessness, α = 0.81; anxious preoccupation, α = 0.89; and cognitive avoidance, α = 0.75) were assessed using the mini-Mental Adjustment to Cancer Scale (mini-MAC) [22]. Participants indicate on a 4-point scale how much each statement applies to them currently, and scores are calculated by summing items for each respective domain, with higher scores indicating more use of that coping style.
Adherence
Multiple measures of adherence were monitored within the website: the number of modules and worksheets completed, the number of visits to the website, and length of time logged in.
Statistical methods
Power calculation
An a priori sample size calculation was conducted using a programme by Hedeker [14]. With three follow-up assessment points, two groups, power set at 0.80, statistical significance set at α = 0.05 (two tailed), and an effect size set at moderate (0.50), 55 participants per group were required (total N = 110 patients), allowing for 20 % attrition over the course of the study in line with previous Web-based studies [9, 12]. Due to the constraints of completing the trial within the duration of a funded fellowship, a stopping rule was introduced, such that recruitment ceased after a 20-month recruitment window. This resulted in a final sample of 60 participants (30 per condition), with the study therefore being underpowered for moderate or small effect sizes.
Analytic strategy
Group differences at baseline were investigated using t tests for continuous variables or χ 2 tests of independence for categorical variables. Intervention effects for each outcome variable were assessed using linear mixed model (LMM) analyses with restricted maximum likelihood (REML). Baseline observations were used as covariates to eliminate the influence of baseline variability, resulting in a 2 (group: intervention, control) × 3 (time: post-programme, 3 months of follow-up, 6 months of follow-up) fixed effects model for each outcome variable, with random effects accounting for individual variation. This approach effectively equalises conditions at baseline and consequently allows for direct comparison between conditions at each follow-up point. In this context, (a) interactions between condition and time, (b) main effects of group, and (c) post hoc pairwise comparisons at each follow-up point are all indicators of intervention effects. LMM analyses are robust with respect to handling missing data and unbalanced designs in longitudinal research as all participants with at least one observed data point (i.e. one completed follow-up assessment) are included in analyses. As the baseline assessment was operating as a covariate only for analysis of intervention effects, any participants who withdrew prior to the post-intervention assessment—and subsequently only gave baseline data—were not included in the initial LMM (n = 5). To correct for this and ensure a true intention-to-treat design was utilised, a separate LMM including the five dropouts was therefore conducted for each outcome variable, by conducting estimation maximisation imputation at post-treatment [23, 24].
Because of the limitations that small sample sizes pose to significance testing, between-group effect sizes (Cohen’s d) were calculated as another indicator of intervention effects. These were calculated from the post hoc pairwise comparisons, using the difference in means between conditions (control − CCO) divided by the pooled standard deviation, with a bias correction applied to account for the small sample size [25]. Cohen’s d = 0.20 is considered small, 0.50 moderate, and 0.80 large. All analyses were conducted using the statistical software SPSS for Windows version 19.0 (SPSS Inc., Chicago, IL, USA).
Results
Participants
As Fig. 1 demonstrates, 145 patients were approached/screened for eligibility; 21 (14.5 %) were unable to be contacted, and 29 (20 %) did not meet eligibility criteria. Of the remaining 95 eligible patients, 60 consented to participate (n = 30 control; n = 30 intervention), resulting in an uptake rate of 63.2 %.
On average, participants were 52.73 (SD = 9.78) years of age (median = 50.50 years; range 30–84) and had been diagnosed on average 2.65 months prior to study enrolment, and the vast majority were females (95 %) with breast cancer (82 %). As there had been no a priori plans to stratify on sex, the three male participants were randomly assigned to the intervention condition. Table 1 summarises the sample’s demographic and medical characteristics and demonstrates that there were no significant baseline differences between control and intervention participants. Importantly, no significant group differences at baseline were found for any of the psychosocial outcome measures.
Dropouts
All five dropouts were women, with breast cancer, and married. Reasons for dropout were as follows: n = 2 withdrew due to technical difficulties with their computers; n = 2 withdrew due to time restraints; and n = 1 withdrew due to the programme not being what she was after (support group, in person). No significant differences were found between dropouts and treatment completers on baseline demographic, medical characteristics, or outcome variables, with the exception of significantly lower levels of anxious preoccupation (dropouts: M = 12.80, SD = 7.46; completers: M = 19.93; SD = 6.36; t(58) = −2.37, p = 0.02) and helplessness/hopelessness (dropouts: M = 8.20, SD = 0.45; completers: M = 11.87, SD = 4.47; t(58) = 2.15, p = 0.001) in dropouts.
Programme usage
As Table 1 shows, there were no significant differences between intervention and control participants in terms of number of logins, session length, or average number of modules completed. However, a significant difference emerged in the pattern of how participants used the programme: Control participants had a bimodal pattern of usage, either not completing a single module (17 %) or completing five to six modules (63.3 %). In contrast, all intervention participants completed at least one module, with the distribution across modules being even.
Repeated measures
Table 2 displays the estimated marginal means, standard errors, and between-group effect sizes at each assessment time point.
Distress
No statistically significant group × time interactions or main effects for group were obtained for either measure. A significant main effect for time was found for cancer distress (F 2, 48.35 = 5.982, p = 0.005), and post hoc analysis shows a trend towards significantly lower scores at post-treatment for CCO participants (F 1, 51.65 = 2.73, p = 0.10). This was supported by the moderate between-group effect size (d = 0.43).
QOL
No statistically significant interactions or main effects for group were obtained for either measure. Two trends approaching significance were obtained: (i) an interaction for global QOL (F 2, 48.30 = 2.45, p = 0.097), with covariate-adjusted scores demonstrating that CCO leads to greater improvements over time than controls, and (ii) a main effect for group for physical function (F 1, 51.40 = 2.92, p = 0.09), with covariate-adjusted scores indicating that CCO participants experienced higher physical functioning across all follow-up assessments compared to controls. Significant main effects for time were found for physical functioning (F 2, 47.86 = 8.48, p = 0.001), global QOL (F 2, 48.30 = 9.46, p < 0.001), role function (F 2, 48.09 = 8.44, p = 0.001), and social function (F 2, 45.59 = 17.80, p < 0.001).
As shown in Fig. 2, post hoc group comparisons at each follow-up, controlling for baseline levels, found significantly higher physical functioning in CCO participants at 3 months of follow-up (F 1, 47.77 = 6.08, p = 0.02), with a moderate between-group effect size (d = −0.52). This effect was somewhat reduced, but still moderate, at 6 months of follow-up (d = −0.40). Post hoc analyses also showed a trend towards a significant group difference in global QOL at 6 months of follow-up (F 1, 49.02 = 2.63, p = 0.10), with a moderate between-group effect size (d = −0.43).
Coping
No significant interactions or main effects for group were obtained. A significant main effect for time was found for anxious preoccupation (F 2, 49.22 = 7.14, p = 0.002). Post hoc pairwise comparisons showed a trend towards lower anxious preoccupation levels in CCO participants compared to controls at post-treatment (F 1, 51.88 = 3.26, p = 0.08), with a small-to-moderate associated effect size. A non-significant trend towards lower cognitive avoidance among CCO participants was also found at 3 months of follow-up (F 1, 48.43 = 3.02, p = 0.09), with a small associated effect size.
Intention-to-treat
An intention-to-treat analysis to manage missing data was then applied, using EM maximisation at post-treatment for the five participants with missing data, with no significant changes to results obtained.
Gender
Given only three men participated in the study and were all randomised to the intervention condition, LMM analyses were re-run excluding them to determine whether they were influential in the results. No changes in results occurred.
Conclusions
Overall, while results were promising, they must be interpreted with caution, given the lack of power to detect statistically significant interactions. Several notable findings emerged. First, extending the findings of our feasibility study [13], statistically significant main effects for time were obtained in six of the ten outcomes evaluated, with post hoc pairwise comparisons and/or between-group effect sizes demonstrating that CCO was driving the changes observed for four of these six outcomes. That is, there were (i) statistically significantly higher levels of physical functioning at 3 months of follow-up, with a moderate between-group effect size (d = 0.52); (ii) a trend towards a significant group × time interaction for global QOL; (iii) immediate post-treatment reductions in cancer distress; and (iv) immediate post-treatment reductions in anxious preoccupation compared to controls, as evidenced by the small-to-moderate between-group effect sizes.
Second, while not statistically significant, group differences with small-to-moderate effect sizes favouring CCO were obtained at 3 and 6 months of follow-ups for general distress and emotional function, and at 3 months for cognitive avoidance. However, this pattern of findings must be balanced against the three outcomes where no group differences at any follow-up emerged: role function, social function, and helplessness/hopelessness. This lack of group differences over time for helplessness/hopelessness contrasts with both our prior feasibility study [13] and our RCT evaluation of the original print workbook that CCO was adapted from [17]. These results clearly need to be substantiated with statistically significant results in a larger-scale adequately powered RCT.
Of interest, there were differing patterns of programme usage between groups: 17 % of control participants were non-users (i.e. did not access a single module), while all intervention participants accessed at least one module. This difference is noteworthy given that attempts were made to reduce allocation bias: the conditions were described as two different versions of the same programme that were being compared to establish which one is more helpful. Neither condition was posited as being superior, and the terms ‘control’ and ‘intervention’ were deliberately not used. Whether this non-usage therefore related to treatment allocation, individual/personal factors, or chance cannot be determined. Conversely, nearly two thirds of control participants were high-users (i.e. they completed five to six out of the six available modules), while the number of modules completed was evenly distributed for CCO participants. It is interesting that fewer CCO participants were categorised as high-users compared to Web-based controls; whether this indicates that participants found the intervention condition less engaging or too demanding to complete warrants further investigation. This finding is not novel: other non-cancer online interventions have found control group membership to be associated with higher adherence [26–28]; however, non-usage or treatment attrition evaluations for cancer interventions are only now emerging [29]. Our adherence results compare favourably to a recent usage analysis of a Web-based breast cancer survivor intervention RCT [29] which classified 9 of their 70 intervention participants (13 %) as non-users, 43 % as low-users, and 44 % as high-users. It was beyond the scope of the current paper to conduct in-depth analyses of within-programme usage, such as whether specific modules were qualitatively less well received than others or whether the various programme ingredients (such as specific CBT worksheets) were well utilised or could be omitted in future iterations. Qualitatively, previous research suggests that adherence is reduced when participants have negative experiences with specific programme components [30]; therefore, these analyses are planned for future dissemination and publication. Further sub-analysis of variables that quantitatively predict programme adherence is also warranted which will further inform this research area.
The current study should be interpreted in the context of the following limitations: First, the small sample size and resulting lack of power limited our ability to obtain statistically significant intervention effects. This resulted from a slower than anticipated recruitment rate at the study site, rather than from a low uptake rate. Second, our sample reported overall low baseline levels of distress; therefore, floor effects were operating, reducing our likelihood of detecting intervention effects. While other studies have implemented distress cut-offs as an eligibility criteria, we elected not to do this in order to increase the potential recruitment pool. A third limitation related to the over-representation of breast cancer in our sample, therefore reducing the generalisability of these results to other curatively treated cancer patients. Whether the fact that this intervention was standardised (that is, it was not tailored to specific cancer types) was a factor in the reduced uptake of non-breast cancer patients warrants consideration. Interventions tailored to cancer types are likely to be more desirable, and qualitative research suggests that more personalised interventions may also yield higher levels of adherence [26, 30, 31]. This, however, must be balanced against the cost-effectiveness of developing a single intervention that can have a broader reach (across cancer types). Fourth, given the pilot nature of this RCT, we did not stratify gender at randomisation, and all three male participants were allocated to the intervention condition. Therefore, this study cannot comment on the benefits of online self-help for men. The fact that only seven men were approached for the study indicates a potential screening bias among recruiters. This gender imbalance is consistent with the online-intervention research literature [32]. Finally, whether users received other formal psychological services during the study was not monitored and therefore could not be controlled for in the analyses.
A strength of this study was the methodology utilised: it was the first to evaluate an Internet intervention for cancer using a Web-based control rather than a waitlist control [9, 11] or second active-treatment group/no control group [10, 13]. This is an important distinction as using a Web-based control provides a more stringent test of the intervention compared to waitlist-control conditions [7], and one would expect to obtain smaller effect sizes when using an active-control condition [18]. While this is a methodological strength in study design, it may have limited our ability to detect significant effects, as the Web-based control may have performed better than predicted. The fact that CCO obtained promising trends compared with our Web-based control, with moderate between-group effect sizes for four outcomes, is therefore indicative of its potential and provides justification for a larger RCT to be conducted.
In conclusion, while limited by its small sample size, this study adds to the emerging Web-based cancer distress intervention literature [9–11, 13] and suggests that CCO holds promise for improving distress, coping, and aspects of health-related quality of life in cancer patients. It will be important for all future studies to conduct usage as well as efficacy analyses to continue to more appropriately tailor interventions to the users they are designed for, and to incorporate longer-term follow-up assessments in order to evaluate whether intervention effects are sustained.
References
Osborn RL, Demoncada AC, Feuerstein M (2006) Psychosocial interventions for depression, anxiety, and quality of life in cancer survivors: meta-analyses. Int J Psychiatry Med 36(1):13–34
Zimmermann T, Heinrichs N, Baucom DH (2007) “Does one size fit all?” Moderators in psychosocial interventions for breast cancer patients: a meta-analysis. Ann Behav Med 34:225–239
Cancer Council SA, Government of South Australia (2011) Statewide cancer control plan 2011–2015. Adelaide
Christensen H (2010) Increasing access and effectiveness: using the internet to deliver low intensity CBT. In: Bennett-Levy J, Richards DA, Farrand P, et al. (eds) Oxford guide to low intensity CBT interventions. Oxford University Press, New York, pp. 53–68
Beatty L, Lambert S (2013) A systematic review of internet-based self-help therapeutic interventions to improve distress and disease-control among adults with chronic health conditions. Clin Psychol Rev 33:609–622
Yates PM, Edwards HE, Nash RE, Walsh AM, Fentiman BJ, Skerman HM, McDowell JK, Najman JM (2001) Barriers to effective cancer management: a survey of hospitalised cancer patients. J Pain Symptom Manag 23:393–405
Cuijpers P, van Straten A, Andersson G (2008) Internet-administered cognitive behavior therapy for health problems: a systematic review. J Behav Med 31(2):169–177. doi:10.1007/s10865-007-9144-1
Australian Bureau of Statistics (2006) Household use of information technology. Australian Bureau of Statistics (No. 8146.0),
Carpenter KM, Stoner SA, Schmitz K, McGregor BA, Doorenbos AZ (2012) An online stress management workbook for breast cancer. J Behav Med. doi:10.1007/s10865-012-9481-6
Duffecy J, Sanford S, Wagner L, Begale M, Nawacki E, Mohr DC (2013) Project onward: an innovative e-health intervention for cancer survivors. Psycho-Oncology 22:947–951
Owen JE, Klapow JC, Roth DL, Shuster Jr JL, Bellis J, Meredith R, Tucker DC (2005) Randomized pilot of a self-guided internet coping group for women with early-stage breast cancer. Ann Behav Med 30(1):54–64
Wootten AC, Abbott J-AM, Meyer D, Chisholm K, Austin DW, Klein B, McCabe M, Murphy DG, Costello AJ Preliminary results of a randomised controlled trial of an online psychological intervention to reduce distress in men treated for localised prostate cancer. European Urology (0). doi:http://dx.doi.org/10.1016/j.eururo.2014.10.024
Beatty L, Koczwara B, Wade T (2011) ‘Cancer Coping Online’: a pilot trial of a self-guided CBT internet intervention for cancer-related distress. Electron.J.Appl.Psychol 7(2):17–25
Hedeker D, Gibbons RD, Waternaux C (1999) Sample size estimation for longitudinal studies with attrition: comparing time related contrasts between two groups. J Educ Behav Stat 24:70–93
Boutron I, Moher D, Altman DG, Schulz K, Ravaud P (2008) Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Ann Intern Med 148:295–309
Schulz K, Altman D, Moher D, CONSORT Group (2010) CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 340:698–702
Beatty L, Koczwara B, Rice J, Wade T (2010) A randomised controlled trial to evaluate the effects of a self-help workbook intervention on distress, coping and QOL after breast cancer diagnosis. Med.J.Aust 193:S68–S73
Danaher B, Seeley J (2009) Methodological issues in research on web-based behavioral interventions. Ann Behav Med 38(1):28–39. doi:10.1007/s12160-009-9129-0
Foa EB, Riggs DS, Dancu CV, Rothbaum BO (1993) Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. J Trauma Stress 6(4):459–473. doi:10.1007/bf00974317
Lovibond SH, Lovibond PH (1995) Manual for the Depression Anxiety Stress Scales (DASS). University of New South Wales, Sydney
Klee M, Groenvold M, Machin D (1997) Quality of life of Danish women: population-based norms for the EORTC QLQ-C30. Qual Life Res Int J Qual Life Asp Treat Care Rehab 6(1):27–34
Watson M, Law M, dos Santos M, Greer S, Baruch J, Bliss J (1994) The mini-MAC: further development of the Mental Adjustment to Cancer Scale. J Psychosoc Oncol 12(3):33–46
Enders CK (2001) A primer on maximum likelihood algorithms available for use with missing data. Structural Equation Modeling: A Multidisciplinary Journal 8(1):128–141. doi:10.1207/S15328007SEM0801_7
Scheffer J (2002) Dealing with missing data. Res.Lett.Inf.Math.Sci 3:153–160
Hedges LV (1981) Distribution theory for Glass’s estimator of effect size and related estimators. J Educ Behav Stat 6(2):107–128. doi:10.3102/10769986006002107
Andersson G, Stromgren T, Strom L, Lyttkens L (2002) Randomized controlled trial of internet-based cognitive behavior therapy for distress associated with tinnitus. Psychosom Med 64(5):810–816
Bewick BM, West R, Gill J, O’May F, Mulhern B, Barkham M, Hill AJ (2010) Providing web-based feedback and social norms information to reduce student alcohol intake: a multisite investigation. J.Med.Internet.Res 12(5) e59
Geraghty AW, Wood AM, Hyland ME (2010) Attrition from self-directed interventions: investigating the relationship between psychological predictors, intervention content and dropout from a body dissatisfaction intervention. Soc Sci Med 71(1):30–37
van den Berg S, Peters E, Kraaijeveld J, Gielissen M, Prins J (2013) Usage of a generic web-based self-management intervention for breast cancer survivors: substudy analysis of the BREATH trial. J.Med.Internet.Res 15(8) e170. doi:10.2196/jmir.2566
Gerhards S, Abma T, Arntz A, de Graaf L, Evers S, Huibers M, Widdershoven G (2011) Improving adherence and effectiveness of computerised cognitive behavioural therapy without support for depression: a qualitative study on patient experiences. J Affect Disord 129(1–3):117–125
Scott K, Beatty L (2013) A feasibility study of a self-guided CBT internet intervention for cancer carers. Aust.J.Prim.Health 19:270–274
Brouwer W, Oenema A, Raat H, Crutzen R, de Nooijer J, de Vries NK, Brug J (2010) Characteristics of visitors and revisitors to an Internet-delivered computer-tailored lifestyle intervention implemented for use by the general public. Health Educ Res 25(4):585–595. doi:10.1093/her/cyp063
Acknowledgments
Thanks to the men and women who participated in this pilot study and for the helpful feedback; we hope you found the programme beneficial. Thanks are due to Ms. Melissa Atkinson for your assistance with study coordination; to the Cancer Care Coordinator, Ms. Caroline Richards; and to Breast Care Nurses Jan. Rice, Merralyn Briskham, and Rachel Buder for your assistance with patient recruitment from Flinders Medical Centre. The Cancer Council of South Australia supported and assisted with advertising this study.
The Cancer Coping Online website was funded by the South Australian Department of Health Australian Better Health Initiative Cancer Coordination Project Grant. Dr. Lisa Beatty’s postdoctoral research fellowship was co-funded by the South Australian Department of Health, the Cancer Council South Australia, and Flinders University. She is currently funded by the National Health and Medical Research Council Project Grant #1042942.
Compliance with ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Beatty, L., Koczwara, B. & Wade, T. Evaluating the efficacy of a self-guided Web-based CBT intervention for reducing cancer-distress: a randomised controlled trial. Support Care Cancer 24, 1043–1051 (2016). https://doi.org/10.1007/s00520-015-2867-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-015-2867-6