Abstract
Purposes
Patient Generated Index (PGI) is designed to both ask and document quality of life (QOL) concerns. Its validity with respect to standard QOL measures has not been fully established for advanced cancer when QOL concerns predominate. The specific objective of this study is to identify, for people with advanced cancer, similarities and differences in ratings of global QOL between personalized and standard measures.
Methods
A total of 192 patients completed five QOL measures at study entry: PGI, generic measures (SF-6D, EQ-5D), and cancer-specific measures of QOL (McGill Quality of Life Questionnaire and Edmonton Symptoms Assessment Scale). Comparisons among total scores were compared using Generalized Estimating Equations (GEE).
Results
Patients voiced 114 areas of QOL concerns by the PGI with the top three being fatigue, sleep, and pain (39.2, 22.6, and 21.6 %, respectively). PGI total QOL score was 25 to 30 percentage points lower than those documented by the other measures, particularly when QOL was poor. Correlations between PGI and other measures were low.
Conclusion
PGI allowed patients to express a wide range of QOL concerns, many that were not assessed by other QOL measures. If only one QOL measure is to be included, either in a clinical setting or for research, the PGI would satisfy many of the criteria for “best choice.” PGI could be considered a cancer-specific QOL measure.
Implications for cancer
This study provides evidence that the PGI would be a good measure for patients and clinicians to use together to identify areas of concern that require attention and monitor changing needs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Worldwide, in 2012, there were 14.1 million people living with cancer, 7.4 million in men and 6.7 million in women [1]. By 2035, an estimated, 24 million individuals will be diagnosed with cancer [1]. Technological advances have played a key role in improving survival through early detection and better treatment [2, 3]. As a result, approximately 75 % of people with cancer will now live 5 years or more [2, 3], but still many will experience a wide range of physical and psychological sequelae from the disease process itself and its treatment [4, 5]. These sequelae matter to patients and impact negatively on their quality of life (QOL).
It remains a challenge in a busy clinical setting to systematically obtain information on the different symptoms, functions, and health aspects of QOL. As a result, these concerns are often not systematically queried nor documented despite the fact that this information is important to guide patient-centered care.
One measurement technology designed specifically to obtain personalized information on areas of concerns to patients is personalized QOL measures [6–10]. The literature indicates that multi-item questionnaires [11–13] correlate only moderately with personalized measures indicating that standardized measures may not capture what is important to individuals. One such measure constructed to capture important concerns of the patient is the Patient Generated Index (PGI).
PGI is a personalized measure designed to both query and document QOL concerns and, thus, could potentially be a valuable clinical and research tool to evaluate changes in health outcomes in patients undergoing cancer care. However, its validity with respect to more standard QOL measures has not been fully established in the context of advanced cancer when QOL concerns predominate. The global objective of this study is to contribute evidence to validate the PGI as quality of life measure in people with advanced cancer. The specific objective is to identify similarities and differences in ratings of global quality of life between personalized and standard measures.
Methods
Subjects
The data for this study comes from a study of anorexia/cachexia in people with advanced cancer, and the data collection included a comprehensive assessment of factors contributing to overall quality of life [14].The target population of this study was people with advanced cancer of any origin. The sample was recruited from two tertiary care university hospitals. This was a cross-sectional study using data from the first assessment post-diagnosis, before start of oncology treatment.
The sample included people with unresectable stage 3A, 3B, or 4 non-small cell lung cancer (NSCLC); stage 3 or 4 upper gastrointestinal (GI) cancer; stage 4 colorectal, hepatobiliary, or head and neck (ENT) cancers; breast and prostate cancers with visceral metastases; all stages of pancreatic cancers; an estimated life expectancy of 3 months or more; and an Eastern Cooperative Oncology Group performance status score of 0 to 3 [15, 16]. People with symptomatic brain metastases were excluded from the study as well as those who were not able to follow the instructions.
Measures
The measurement framework for this study was based on the Wilson-Cleary model [17] of health-related quality of life. In addition to the personalized measure, both generic and cancer-specific QOL measures were used. Measures were chosen based on brevity, comprehensiveness, and inclusion of items on quality of life in addition to symptoms and function.
Personalized measure
The PGI, a personalized measure to identify the impact of specific conditions on QOL [7], has been used and validated in both noncancer populations [7, 18] and a variety of cancer populations [9, 10, 19–21].
PGI is completed in three steps: (1) patients identify the most important five areas of their life affected by cancer; (2) patients rate how much each area has been affected using a scale from 0 to 10, where 0 is the worst imaginable and 10 exactly as they would like it to be and how much; (3) patients now imagine that they have 12 tokens to spend to improve on the selected areas and they allocate these tokens to the areas according to their own priority. A global index is calculated by multiplying the ratings for each area in step 2 by the proportion of tokens given to that area in step 3, which are then summed to produce an index from 0 to 100 with higher scores indicating higher QOL. According to Ruta [7], the final score indicates the extent to which the reality falls short of patient’s hopes and expectations for those areas of life for which they would most value an improvement [7, 22].
Generic health-related quality of life measures
Two measures were used: the EQ-5Dindex from the EuroQoL group [23, 24] and the SF-6D derived from the comprehensive SF-36 Health Survey. The EQ-5D™ is a brief generic measure that provides a descriptive system consisting of five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression). Each dimension has three levels of response: no problems, some problems, and extreme problems. The EQ-5D™ describes 243 health states each with a unique index value calculated using country-specific weights [25–27] with values for EQ-5Dindex ranging from −0.6 to 1.0 [25, 28]. The EQ-5Dindex has been used extensively in population health and cancer research [29–32].
The SF-6D is a generic measure (39, 40) with six multi-level dimensions covered by the SF-36 Health Survey: physical functioning, role limitation ((combined role-physical and role-emotional)), social functioning, bodily pain, and mental health. Each dimension contains four to six levels of function or limitation. Therefore, the SF-6D index classifies 18,000 unique health states. The SF-6D index is calculated using preference weights obtained from a sample of the general population using the standard gamble and ranges from 0.3 (worst health state) to 1.0 (best health state) [33]. The SF-6D has been widely used and validated in cancer population [34–39].
Cancer-specific quality of life measures
Two single-item and one multi-item measures were used. The single items were: (1) Edmonton Symptoms Assessment Scale (ESAS-Version 1) [40] QOL, with a rating scale from 0 to 10 with 10 being the worst possible QOL, and (2) McGill Quality of Life Questionnaire (MQOL) [15, 41–44], also with a 0 to 10 rating scale with 10 being the best QOL. The multi-item questionnaire was the existential subscale from the MQOL with six items, each rated on 0 to 10, scale with 0 meaning the worst and 10 being the best. The ESAS is a brief cancer-specific measure of symptom severity and it is a valid and reliable tool to help in the assessment of nine symptoms commonly experienced by cancer patients (pain, fatigue, nausea, depression, anxiety, drowsiness, appetite, itching, and shortness of breath) and one item for overall quality of life [45, 46].
McGill QOL questionnaire was developed to measure QOL at all stages of the disease trajectory for people with a life-threatening illness such as cancer [15, 41–44]. There are five MQOL sub-domains: physical symptoms (items 1–3), physical well-being (item 4), psychological symptoms (items 5–8), existential (items 9–14), and support (items 15 and 16). The existential sub-domain captured aspects related to meaning of life considering the last 2 days. Many studies have shown that the total score and the sub-domain scores of the MQOL have a good validity (construct validity) and reliability (internal consistency reliability) for people with cancer and other palliative populations [15, 41–43, 47].
All of the measures used in this study, with the exception of the ESAS and the MQOL, have legitimate total scores [48] based on weighting the dimensions before summing. Therefore, from the ESAS and MQOL, we chose the two single items for QOL and the one sub-domain (existential) of the MQOL.
Procedure
This study was approved by the Institutional Review Board of the Faculty of Medicine of McGill University. People who met the study criteria were approached by a member of their primary oncology and medical team in order to obtain verbal consent. Once consent was granted, study personnel contacted the patients to explain the goals and procedures of the study. All participants gave written informed consent. At the first assessment, patients were interviewed on all study measures by trained research personnel.
Analysis
The first step was to identify the most frequently nominated areas using the PGI measure and to calculate the PGI score. Secondly, scores were calculated for all the measures and comparisons between personalized measure (PGI), generic measures (SF-6D, EQ-5Dindex), and the cancer-specific measures (ESAS-qol, MQOL single items, and MQOL existential) made using generalized estimating equations (GEE) to account for the clustering of the questionnaire scores within person. All measures were transformed to range from 0 to 100 with 100 being the best QOL.
Spearman’s correlation coefficient was used to measure the strength of the association between the PGI and the other QOL measures. The regression coefficients from the GEE model were used to calculate the difference between measures and the corresponding 95 % CIs, accounting for the correlation among measures. Also calculated from the regression coefficients were effect sizes (β/SE).
The Bland-Altman plot was used to depict differences between the measures under study here: the PGI and the EQ-5Dindex, and the PGI and the SF-6D. While developed to depict agreement, in this context, the graphic representation permits a visualization of the variability in the magnitude of the latent variable QOL arising from using different measures of the latent construct. The latent construct is represented, on the x-axis, by the average of the scores of the two measures. The unique contribution to the latent construct from the different measures is shown on the y-axis as the difference between the two measures. If both measures equally represent the latent construct throughout its range, there will be no discernible pattern to the distribution of the difference along the latent construct.
Results
A total of 192 persons completed the PGI at baseline, and their characteristics are shown in Table 1. Table 2 lists the 11 most frequent areas of QOL affected by advanced cancer, at time of diagnosis, as documented using the PGI. Also indicated is whether or not the areas of QOL concern are present in the other study measures: EQ-5Dindex, the SF-6D, the MQOL, and the ESAS. Overall, participants nominated 114 areas of QOL concern, using the PGI.
Participants nominated a wide range of QOL concern affected by cancer with fatigue being the most common, nominated by 39 % of participants, to mobility, nominated by 3.5 %. Fatigue was present as an item in the SF-6D, the MQOL, and the ESAS but not in the EQ-5Dindex. Sleep function, the second most frequent area, was found only in the MQOL. Pain was the only area that was included in all of the measures. In the five top commonly nominated areas, the MQOL included all the areas (five areas) important to the people with advanced cancer, followed by the ESAS (four areas), the SF-6D (three areas), and then the EQ-5Dindex (two areas).
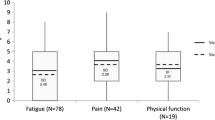
The average rating from the PGI was substantially lower (37 ± 25) than the average QOL ratings from generic measures (EQ-5Dindex (mean 66 ± 17) and SF-6D (mean 65 ± 14)). The correlations between the PGI and the generic measures were low (0.16 and 0.22 for EQ-5Dindex and SF-6D, respectively); the correlation between the two generic measures was moderate (0.53). The magnitude of the difference between the PGI and generic measure ranged from −28.5 to −27.5; effect size estimates ranged from −14.3 to −13.4 (see Fig. 1a). The results comparing the PGI with the cancer-specific QOL measures are shown in Fig. 1b. Correlations between the PGI and these measures were also low (range 0.12 to 0.18), and the magnitude of differences were similar for the MQOL single item (−26.7) and the ESAS single item (−26.1) and larger for the MQOL existential single item (−43.3).
Figure 2 represents the relationship between the PGI and the generic measures (EQ-5Dindex and SF-6D) using the Bland-Altman plot. The y-axis represents the difference between the PGI and each measure, EQ-5Dindex (Fig. 2a) and SF-6D (Fig. 2b). The x-axis represents the latent construct of QOL as the average between the two measures. The gray line, which is parallel to the x-axis, represents the line of equality (0 differences between measures). The middle red line represents the mean difference between the two measures. The upper and lower red lines represent the corresponding 95 % CI. The black dots represent the score of each participant on both measures. At the left end of the x-axis when the participant’s QOL was poor, the score from the PGI was lower (except for one observation) than the score obtained from the EQ-5Dindex (Fig. 2a). This was also observed for the middle range (shown in rectangle), where the majority of the observations were below the line of equality. However, at the right end of the x-axis, when the participant’s QOL was good, there was no discernible pattern to the difference between the two measures. Similar results were found for the comparison between the PGI and SF-6D (Fig. 2b).
Discussion
The PGI identified a total of 114 areas of QOL concern, with the top three, fatigue, sleep disruptions, and pain. Other studies that have used the PGI in cancer samples also found this wide range of areas [9, 19]. Our findings are concordant with the literature on the importance of fatigue, sleep, and pain to QOL, as the most recent systematic reviews endorsed their importance [48–53].
This heterogeneity in QOL contributors is not reflected in standard QOL measures, either generic or cancer specific, as the combined measures used in our study queried only nine areas. All of the measures used in this study except the EQ-5Dindex included fatigue; sleep was only included in the MQOL. Pain, the third most frequently endorsed area, was the only domain that was included in all of the measures. In contrast, two of the ten top areas identified using the PGI (eating, family relationships; see Table 2) were not represented in any of the standard measures used here. ESAS, a symptom measure, captured all the important symptoms identified by the participants, except sleep disruption.
One of the most frequently used cancer-specific measures is the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-C30 (EORTC QLQ-C30) [54]. While we did not include this 30-item measure, its content has been shown to capture 25 domains related to symptoms and function and also includes three questions, one each on health perception, overall QOL rating, and financial impact of cancer [55]. The functional domains on the EORTC were all nominated using the PGI and are present as items in the measures chosen for this study (see Table 2). Another widely used measure the Functional Assessment on Cancer Therapy—General Scale (FACIT-G) [56] comprises 27 items that capture 6 emotional impairments and 4 physical impairments (pain, fatigue, nausea, and insomnia); 2 items for work; 1 for role; and the remaining 14 items reflect aspects of QOL, general health, and environmental factors. These areas were all identified in the PGI.
This study found that the PGI consistently produced values for QOL that were lower than standard generic or cancer-specific measures of QOL. One reason for this is the scoring system which not only rates the severity of the impact of nominated areas but also weighs them in terms of their priority for intervention. For example, a person would get a low QOL score if an area has a large negative impact and receives a lot of “tokens,” therefore identified as a very important priority. Another reason is that the PGI allows patients to mention important QOL contributors that may not be captured by other measures. The other measures that use weights to derive total scores (EQ-5Dindex and SF-6D) have obtained these from the general population, not from people with cancer [57]. The consequence is that QOL is overestimated if measurement relies only on standard “one-size-fits-all” measures and/or weights. The PGI could be useful in the clinical setting as the combination of weight and priority for each contributor would probably be more effective in orientating interventions to improve overall QOL.
There was a low correlation between the PGI and the other study measures. This finding is supported by earlier studies that found low to moderate correlation between the PGI and EORTC and the PGI and the SF-36 [9, 19]. Also, our finding is in line with a study done in multiple sclerosis using the same methodology [58]. This further supports the importance of exploring the priority attached by the patient to the QOL contributors.
This was a study of a unique sample compromised entirely of people with advanced cancer before any oncological treatment for whom QOL is of primordial concern for making treatment and life decisions. Because a restricted number of QOL measures were included in the study based on the fewest items per questionnaire, in order not over burden the participants, direct comparisons with the well-known 30-item EORTC and the 27-item FACIT could not be performed.
The PGI may be an interesting instrument to evaluate the impact of clinical trials that target QOL. The standard measures tend to yield higher QOL ratings, and hence, comparisons with baseline may be disappointing as there is limited room for improvement with intervention. It would not be unusual for a cancer clinical trial to use the SF-6D or EQ-5D as an outcome [59]. If so, the effect of the intervention in a sample of patients with similar QOL as our study, considering a ½ SD effect size [60], would mean that the SF-6D would need to improve from a mean of 66 to a mean of 75 (and the EQ-5Dindex, from 65 to 72), whereas the same effect size on PGI would require a change from 37 to 49, a more achievable change. For the cancer-specific measures, the SDs were as high as the PGI but the means were also higher indicating an important change would be difficult to achieve.
Conclusion
PGI is a personalized measure and was developed to identify the impact of a health condition on QOL. This study showed that, in comparison to commonly used generic and cancer-specific QOL measures, the PGI covers the widest spectrum of health concepts as it allows respondents to nominate, weigh, and prioritize any areas that are important to their QOL, not just those presented to them. The PGI has additional advantages in that it is short and easy to administer and yields a value farther away from the ceiling and with a lower standard error in comparison to standard measures. If only one QOL measure is to be included, either in a clinical setting or for research, the PGI would satisfy many of the criteria for “best choice” [61]. When used in a cancer population, the PGI could be considered a cancer-specific QOL measure.
Financial disclosure
None.
Funding
This study received funding from the Terry Fox Research Institute.
Conflict of interest
The authors declare that they have no competing interests.
References
WCRF International (2015) Cancer worldwide data. [cited 5/3]; Available from: http://www.wcrf.org/int/cancer-facts-figures/worldwide-data
de Boer AG et al (2008) Work ability and return-to-work in cancer patients. Br J Cancer 98(8):1342–1347
Hoffman B (2005) Cancer survivors at work: a generation of progress. CA Cancer J Clin 55:271–280
Lehmann JF et al (1978) Cancer rehabilitation: assessment of need, development, and evaluation of a model of care. Arch Phys Med Rehabil 59(9):410–419
Ness KK et al (2006) Physical performance limitations and participation restrictions among cancer survivors: a population-based study. Ann Epidemiol 16(3):197–205
O’Boyle CA et al (1992) Individual quality of life in patients undergoing hip replacement. Lancet 339(8801):1088–1091
Ruta DA et al (1994) A new approach to the measurement of quality of life. The Patient-Generated Index. Med Care 32(11):1109–1126
Broadhead JK, Robinson JW, Atkinson MJ (1998) A new quality-of-life measure for oncology: The SEIQoL. J Psychosoc Oncol 16(1):21–35
Tavernier SS et al (2011) Validity of the Patient Generated Index as a quality-of-life measure in radiation oncology. Oncol Nurs Forum 38(3):319–329
Tavernier SS, Totten AM, Beck SL (2011) Assessing content validity of the patient generated index using cognitive interviews. Qual Health Res 21(12):1729–1738
Frick E, Tyroller M, Panzer M (2007) Anxiety, depression and quality of life of cancer patients undergoing radiation therapy: a cross-sectional study in a community hospital outpatient centre. Eur J Cancer Care 16(2):130–136
Montgomery C et al (2002) Individual quality of life in patients with leukaemia and lymphoma. Psychooncology 11(3):239–243
Waldron D et al (1999) Quality-of-life measurement in advanced cancer: assessing the individual. J Clin Oncol 17(11):3603–3611
Rodriguez AM, Mayo NE, Gagnon B (2013) Independent contributors to overall quality of life in people with advanced cancer. Br J Cancer 108(9):1790–1800
Cohen SR et al (1997) Validity of the McGill Quality of Life Questionnaire in the palliative care setting: a multi-centre Canadian study demonstrating the importance of the existential domain. Palliat Med 11(1):3–20
Osoba D, King M (2005) Meaningful differences. In: Fayers PM, Hays RD (eds) Assessing quality of life in clinical trials, 2 edn. Oxford University Press, New York, pp. 243–257 p. 5 A.D. 251
Wilson IB, Cleary PD (1995) Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA 273(1):59–65
Ruta DA, Garratt AM, Russell IT (1999) Patient centred assessment of quality of life for patients with four common conditions. Qual Health Care 8(1):22–29
Camilleri-Brennan J, Ruta DA, Steele RJ (2002) Patient generated index: new instrument for measuring quality of life in patients with rectal cancer. World J Surg 26(11):1354–1359
Lewis S et al (2002) Quality of life issues identified by palliative care clients using two tools. Contemp Nurse 12(1):31–41
Llewellyn CD, McGurk M, Weinman J (2006) Head and neck cancer: to what extent can psychological factors explain differences between health-related quality of life and individual quality of life? Br J Oral Maxillofac Surg 44(5):351–357
Calman KC (1984) Quality of life in cancer patients—an hypothesis. J Med Ethics 10(3):124–127
EuroQOL Group (1990) EuroQol—a new facility for the measurement of health-related quality of life. Health Policy 16(3):199–208
Gudex C et al. (1996) Health state valuations from the general public using the visual analogue scale. Qual Life Res 5(6):521–531
Dolan P (1997) Modeling valuations for EuroQol health states. Med Care 35(11):1095–1108
Bansback N et al (2012) Canadian valuation of EQ-5D health states: preliminary value set and considerations for future valuation studies. PLoS One 7(2):e31115
Oremus M et al (2014) Health utility scores in Alzheimer’s disease: differences based on calculation with American and Canadian preference weights. Value Health 17(1):77–83
Shaw JW, Johnson JA, Coons SJ (2005) US valuation of the EQ-5D health states: development and testing of the D1 valuation model. Med Care 43(3):203–220
Lee JA et al (2014) Comparison of health-related quality of life between cancer survivors treated in designated cancer centers and the general public in Korea. Jpn J Clin Oncol 44(2):141–152
Shim EJ et al (2011) Comprehensive needs assessment tool in cancer (CNAT): the development and validation. Support Care Cancer 19(12):1957–1968
Glick HA et al (1998) Empirical criteria for the selection of quality-of-life instruments for the evaluation of peripheral blood progenitor cell transplantation. Int J Technol Assess Health Care 14(3):419–430
Pickard AS et al (2007) Health utilities using the EQ-5D in studies of cancer. PharmacoEconomics 25(5):365–384
Brazier J, Roberts J, Deverill M (2002) The estimation of a preference-based measure of health from the SF-36. J Health Econ 21(2):271–292
Hever, N.V., et al (2014) Health related quality of life in patients with bladder cancer: a cross-sectional survey and validation study of the Hungarian version of the bladder cancer index. Pathol Oncol Res
Gallop K et al (2015) A qualitative evaluation of the validity of published health utilities and generic health utility measures for capturing health-related quality of life (HRQL) impact of differentiated thyroid cancer (DTC) at different treatment phases. Qual Life Res 24(2):325–338
Teckle P et al (2013) Mapping the FACT-G cancer-specific quality of life instrument to the EQ-5D and SF-6D. Health Qual Life Outcomes 11:203
Lee L et al (2013) Valuing postoperative recovery: validation of the SF-6D health-state utility. J Surg Res 184(1):108–114
Barton GR et al (2008) An assessment of the discriminative ability of the EQ-5D index, SF-6D, and EQ VAS, using sociodemographic factors and clinical conditions. Eur J Health Econ 9(3):237–249
Hornbrook MC et al (2011) Complications among colorectal cancer survivors: SF-6D preference-weighted quality of life scores. Med Care 49(3):321–326
Bruera E et al (1991) The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. J Palliat Care 7(2):6–9
Cohen SR et al (2001) Changes in quality of life following admission to palliative care units. Palliat Med 15(5):363–371
Cohen SR, Mount BM (2000) Living with cancer: “good” days and “bad” days—what produces them? Can the McGill quality of life questionnaire distinguish between them? Cancer 89(8):1854–1865
Cohen SR et al (1995) The McGill Quality of Life Questionnaire: a measure of quality of life appropriate for people with advanced disease. A preliminary study of validity and acceptability. Palliat Med 9(3):207–219
Cohen SR et al (1996) Existential well-being is an important determinant of quality of life. Evidence from the McGill Quality of Life Questionnaire. Cancer 77(3):576–586
Nekolaichuk CL et al (1999) Assessing the reliability of patient, nurse, and family caregiver symptom ratings in hospitalized advanced cancer patients. J Clin Oncol 17(11):3621–3630
Chang VT, Hwang SS, Feuerman M (2000) Validation of the Edmonton Symptom Assessment Scale. Cancer 88(9):2164–2171
Cohen SR et al (1996) Quality of life in HIV disease as measured by the McGill quality of life questionnaire. AIDS 10(12):1421–1427
Glare PA et al (2014) Pain in cancer survivors. J Clin Oncol 32(16):1739–1747
Denlinger CS et al (2014) Survivorship: sleep disorders, version 1.2014. J Natl Compr Cancer Netw 12(5):630–642
Dickerson SS et al (2014) Sleep-wake disturbances in cancer patients: narrative review of literature focusing on improving quality of life outcomes. Nat Sci Sleep 6:85–100
Moens K, Higginson IJ, Harding R (2014) Are there differences in the prevalence of palliative care-related problems in people living with advanced cancer and eight non-cancer conditions? A systematic review. J Pain Symptom Manag 48(4):660–677
Olson K (2014) Sleep-related disturbances among adolescents with cancer: a systematic review. Sleep Med 15(5):496–501
Otte JL et al (2015) Systematic review of sleep disorders in cancer patients: can the prevalence of sleep disorders be ascertained? Cancer Med 4(2):183–200
Aaronson NK et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85(5):365–376
Letellier, M.E., D. Dawes, and N. Mayo (2014) Content verification of the EORTC QLQ-C30/EORTC QLQ-BR23 with the International Classification of Functioning, Disability and Health. Qual Life Res
Cella DF et al (1993) The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol 11(3):570–579
Dolan P (1999) Whose preferences count? Med Decis Mak 19(4):482–486
Kuspinar A, Mayo NE (2013) Do generic utility measures capture what is important to the quality of life of people with multiple sclerosis? Health Qual Life Outcomes 11:71
Garratt A et al (2002) Quality of life measurement: bibliographic study of patient assessed health outcome measures. BMJ 324(7351):1417
Norman GR, Sloan JA, Wyrwich KW (2003) Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care 41(5):582–592
McHorney CA, Tarlov AR (1995) Individual-patient monitoring in clinical practice: are available health status surveys adequate? Qual Life Res 4(4):293–307
Compliance with ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Statement of informed consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aburub, A.S., Gagnon, B., Rodríguez, A.M. et al. Using a personalized measure (Patient Generated Index (PGI)) to identify what matters to people with cancer. Support Care Cancer 24, 437–445 (2016). https://doi.org/10.1007/s00520-015-2821-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-015-2821-7