Abstract
Purpose
This study aims to investigate the comparison of effectiveness between stellate ganglion block (SGB) and complex decongestive physiotherapy (CDT) in breast cancer-related lymphedema (BCRL) patients.
Methods
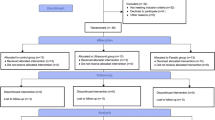
The study is a retrospective matched cohort study. A total of 60 subjects who had secondary lymphedema after breast cancer treatments were included in this study. Thirty subjects who had SGB were matched with other 30 subjects treated with CDT, which is the standard therapy for BCRL. The groups were matched for age, duration of lymphedema, type of surgery, and history of lymph node dissection. SGB subjects received SGB three times, once every 2 weeks and CDT subjects were treated for 2 weeks. The circumferences of the forearm and upper arm were used as the outcome variable. These parameters were measured with baseline value before each treatment and repeated the evaluation after the treatments. We investigated the difference of circumferences within each treatment and compared the clinical effect between treatments.
Results
Sixty subjects (mean age 58.2 ± 8.7) were treated with CDT and SGB each. There was no significant difference in demographic data including cancer treatment. The mean circumferences of the forearm and upper arm after CDT significantly reduced; forearm from 24.91 to 23.87 cm and upper arm from 30.52 to 29.58 cm (p < 0.001). And the clinical effect of SGB was also significant; forearm from 24.90 to 23.64 cm and upper arm from 30.96 to 29.16 cm (p < 0.001). The differences of the forearm between CDT and SGB was not significant, but the circumference of the upper arm was more reduced after SGB treatment (1.81 ± 1.21 cm) than CDT (0.94 cm ± 0.78 cm) (p < 0.01).
Conclusions
SGB is an effective treatment which can reduce the circumference of arm in breast cancer-related lymphedema patients and could be an alternative treatment for lymphedema.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lymphedema is a progressive pathologic condition of localized body fluid retention and subcutaneous tissue swelling caused by a lymphatic obstruction or compromised lymphatic system [1]. If the lymphatic system is damaged, transportation of lymph fluid is reduced, and water and protein is accumulated within the tissue organization. As a result, this high protein concentration cause colloid osmotic pressure in the tissue to increase, and it cause lymphedema by increasing the movement of water [2, 3]. This kind of lymphedema is caused by secondary complications of malignant tumors, infections, trauma, and filariasis, etc. However, most of them have been reported to be associated with malignant tumor and treatments [2]. Secondary lymphedema of the upper extremity usually occurs after breast cancer treatments and the frequency was reported 24–49 % after total mastectomy and 4–17 % after sentinel lymph node biopsy with radiation [4, 5]. In Korea, it is reported that 22 % of patients have developed secondary lymphedema in the upper extremity after breast cancer treatments [1].
The standard treatment for lymphedema is well known for complex decongestive physiotherapy (CDT). CDT is a treatment consisting of skin care, manual lymph drainage massage, non-elastic bandage therapy, and exercise therapy [6]. The reduction of lymphedema after CDT was around 30–60 % on average and has been reported to be maintained after 1 year [7]. However, there are some disadvantages such as differing results of edema reduction within each patient and the high risk of recurrent edema if the patient’s compliance is poor. In addition, CDT is sometimes criticized for being time consuming and can be a burden for the rest of the patient’s life [8–10]. Therefore, complementary and alternate treatment is required to manage breast cancer-related lymphedema (BCRL).
In recent years, consequentially, new alternative therapies have been tried using extracorporeal shock wave therapy (ESWT) and microsurgical lymph node transplantation [11, 12]. The authors reported these therapies were good alternative methods. In addition, previous studies tried the cervical stellate ganglion block (SGB) and reported a good result for the reduction of lymphedema on the upper extremity after breast cancer treatments [13, 14]. However, these new trials are limited to case or case-series studies. Therefore, a comparison between CDT and new clinical therapies is needed.
The main purpose of this study, therefore, is to compare the effectiveness between CDT and SGB in BCRL patients and to determine whether SGB can be applied as much as CDT in the clinic.
Subjects and methods
Subjects
A total of 60 subjects who were diagnosed with secondary lymphedema after breast cancer treatment and who underwent CDT or SGB were retrospectively recruited based on their medical record. Subjects who had (1) a mastectomy due to breast cancer, (2) no history of physical therapy except self-manual lymph drainage massage in the last 6 months, and (3) lymphedema defined as a circumference of the affected arm of 2 cm or more compared with the unaffected arm were recruited. Women were ruled ineligible for the study according to the following exclusion criteria: (1) bilateral lymphedema, (2) breast reconstruction, (3) infection or cellulitis, (4) severe pain in the axillary operation scar, (5) venous thrombosis, (6) difficulties in participating in the study, and (7) irregular attendance. We preferentially included the SGB subjects who were small in number because patients preferred the less invasive CDT. Therefore, 30 patients who received SGB were retrospectively included from March 2012 to February 2013. From the same period, we randomly included 30 CDT subjects who were matched to age, duration of lymphedema, and type of surgery and history of lymph node dissection. Eight subjects in the SGB group were previously treated with CDT more than 6 months before the SGB. However, CDT was ineffective and the patients performed self-manual drainage massage during that period. The present study was approved by the Institutional Review Board of Seoul National University Hospital [H-1305-052-488].
Methods
Demographics
Demographic information including age (year), body mass index (BMI, kg/m2), duration of lymphedema (month), time since mastectomy (month), laterality (right or left), type of surgery (modified radical mastectomy, breast conserving surgery, or total mastectomy), experience of reconstruction surgery and lymph node dissection, the presence of lymph node metastasis, and whether having radiotherapy and chemotherapy, were collected retrospectively with a medical record.
SGB
Thirty subjects underwent consecutive SGB three times, once every 2 weeks by the same physician at the outpatient clinic [13, 15]. The procedure was performed while the subject was in the supine position with the head slightly extended on a pillow. Sternocleidomastoid muscle around cricoid cartilage was retracted laterally using two fingers which could pull the internal carotid artery and the internal jugular vein. Next, the needle was inserted between the cricoid cartilage and the fingers under aseptic ultrasonographic guidance. After contact with the anterior tubercle of the C6 transverse process, the needle was withdrawn from the periosteum and 4 ml of 1 % lidocaine and 1 ml of 40 mg triamcinolone mixture were injected into the stellate ganglion [13]. Figure 1 shows a lateral axis view of an ultrasound image of the neck. All SGB patients were educated self-massage and CDT was not done by therapists.
Lateral axial view of ultrasound neck image at the C6 vertebral level. TR trachea, CA carotid artery, AS anterior scalene muscle, SCM sternocleidomastoid muscle, MS middle scalene muscle, AT anterior tubercle, PT posterior tubercle, C6 C6 nerve root, SC sympathetic chain, LC longus coli muscle, and VB vertebral body
CDT
The other 30 subjects with secondary lymphedema had ten sessions of CDT (2 weeks, from Monday to Friday of the next week) with a physical therapist in an outpatient clinic. One session (40 min) was comprised of manual lymphatic drainage (15 min) of stimulating the movement of fluid in the tissue, bandaging (15 min) in compression garments, and exercise (10 min).
Outcome variable
The circumferences of the forearm and upper arm were used as an outcome variable which was measured by a tape measure without any pressure and placed perpendicular at the vertical axis in the forearm and upper arm. The forearm was measured at 10 cm below the cubital crease between the medial and lateral epicondyle and the upper arm was measured at 10 cm above the cubital crease (Fig. 2). In the CDT group, the circumferences were initially measured with a baseline value before CDT, and the measurements were repeated 2 weeks after the first treatment. In the SGB group, the baseline circumferences were initially measured before SGB and were reevaluated three times: 2 weeks after the first block, 2 weeks after the second block (4 weeks after the first block) and 4 weeks after the third block (8 weeks after the first block) that was regarded as the primary outcome variable. In addition, we compared the effects of each treatment and investigated the serial effect of SGB.
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics version 19.0 for Windows. Demographic data was analyzed using an independent t test and chi-square test according to the number of possible responses for each item. Also, we investigated the difference of circumference within each treatment using a paired t test, and compared the circumferences between treatments using an independent t test. In addition, we analyzed the serial effect of SGB with a paired t test. To evaluate the factor affecting the decrement of lymphedema in demographics, the chi-square test was used. P values of <0.05 were taken to represent statistical significance.
Results
Demographics
Table 1 showed the demographic information of 60 subjects who had SGB (30 subjects, mean age 58.70 ± 10.36) and CDT (30 subjects, mean age 57.73 ± 6.92). All subjects had lymph node dissection and chemotherapy but no reconstructive surgery. Twenty-seven subjects (90 %) in the SGB group and 24 subjects (80 %) in the CDT group received radiation therapy (p = 0.472). The demographic information showed an even distribution between the SGB and CDT groups, including cancer treatments and the baseline circumferences of the forearm and upper arm.
Effect of CDT
The baseline circumferences of the forearm and upper arm were 24.91 cm (±2.34) and 30.52 cm (±2.67) and the circumferences after treatment were 23.87 cm (±2.26) and 29.58 cm (±2.43), which showed a significant reduction in each (p < 0.001) (Table 2). However, there was no significant demographic factor to influence the reduction of the circumference with factor analysis.
Effect of SGB
The circumferences of the forearm and upper arm were 24.90 cm (±3.64) and 30.96 cm (±3.57) at baseline and the circumferences of 8 weeks after the first block were significantly reduced to 23.64 cm (±3.24) and 29.16 cm (±3.45) (p < 0.001) (Table 2). However, there was no significant demographic factor affecting the decrement of lymphedema.
Serial effect of SGB
Of 30 subjects in the SGB group, 15 subjects had serial circumferences on medical record (Fig. 3). In three consecutive blocks, the circumferences of the forearm after the first and second blocks did not show a significant reduction, but the circumference after the third block significantly decreased from 25.47 cm (±3.28) to 24.66 cm (±3.11) (p < 0.05), which is also a significant reduction from baseline (26.21 ± 3.64 cm) (p < 0.01).
The serial effect of SGB. a The circumference of forearm after third block significantly decreased from 25.47 cm (±3.28) to 24.66 cm (±3.11) (p < 0.05) which is also a significant reduction from baseline (26.21 ± 3.64 cm) (p < 0.01). b Baseline circumference was 32.32 cm (±3.28) and the circumference after second block was 31.52 cm (±3.29) (p < 0.01). Additionally, there was a significant reduction after the third block which is from 31.52 cm (±3.28) to 30.11 cm (±2.69) (p < 0.001). *<0.05, †<0.01, ‡<0.001
The circumferences of the upper arm, on the other hand, showed a significant decrease after the second block. The baseline circumference was 32.32 cm (±3.28) and the circumference after the second block was 31.52 cm (±3.29) (p < 0.01). In addition, there was a significant reduction after the third block, from 31.52 cm (±3.28) to 30.11 cm (±2.69) (p < 0.001).
Effect between CDT and SGB
The effects of lymphedema treatments on the forearm were 1.03 cm (±0.85) and 1.26 cm (±1.23), which is not a significant difference between the CDT and SGB groups (Fig. 4). The effects of treatment on the upper arm, however, showed 0.94 cm (±0.78) and 1.81 cm (±1.21) which is a significant reduction in each group, but more so for the SGB group than CDT (p < 0.01).
Discussion
Secondary lymphedema, in contrast with primary lymphedema, is much more common and can develop after any surgical, traumatic, inflammatory, or neoplastic disruption or obstruction of lymphatic pathways [16]. A reduction of the lymph node can cause lymphostasis in the interstitial fluid and lymph collectors or precollectors to become engorged and fibrotic, eventually causing lymphatic hypertension. If one of the collector valves is interrupted due to lymphatic hypertension, the other valves around it could become damaged in consequence [17]. As a result, a reduction or destruction of lymphatic transport can develop the lymphedema after cancer treatments.
Manual lymph drainage massage is a gentle and rhythmic manipulation of the lymphatic ducts to stimulate the flow of lymph into collectors and precollectors [18]. Bandage therapy with exercise or daily activities can enhance the pumping action of the lymph vessels by providing increased resistance for them to push against [19]. So, CDT is well known as a primary method of treatment in lymphedema management and many studies have reported a reduction of circumference on extremity [6, 7, 20]. Yamamoto et al. reported the median reduction was 328.7 ml and the median rate of reduction was 58.9 % after CDT in the upper extremity for lymphedema patients [7]. In addition, Karadibak et al. showed that the mean reduction of volume was 415 ml and the mean rate of reduction was 25.8 % after CDT in the upper extremity for cancer-related lymphedema patients [20]. The present study shows enough decrement of circumference after CDT and this is a significant reduction of subcutaneous volume compared to previous studies.
SGB resulted in a marked reduction of volume after 8 weeks from the first block [13, 15]. Kim et al. performed SGB on ten patients with the same protocol as this study and showed a significant decrement of circumferences in the forearm and upper arm which is similar to the results of this study [13]. Our result also showed significant improvement of lymphedema.
Interestingly, the three treatments of SGB appear to have an accumulative effect. There was a significant reduction in the forearm circumferences after the third block compared with the second block. In the upper arm, we identified a significant decrement after the second and third blocks, respectively. Unfortunately, there is no standard protocol for SGB because it is not a widely accepted treatment for lymphedema. No one knows how many SGBs are needed, when it works, or whether it has a long-term effect, so we did it three times, every 2 weeks, like previous small-sized studies about cervical SGB at BCRL [13, 15]. Recently, Woo et al. reported that three treatments of lumbar sympathetic ganglion block (LSGB) at 2-week intervals were effective in treating secondary lymphedema after gynecologic cancer [21].
We expected the effect of SGB might be similar to CDT, but there was a bigger reduction of circumference in the upper arm. The reason is unclear, but the authors suggest cervical SGB might have a stronger effect on proximal than distal extremity.
Still, the mechanism of SGB is unclear. The previous researchers explained that this phenomenon was the result of autonomic regulation block by SGB. Smooth muscles which are innervated by the autonomic nervous system envelop the lymphatic channel-like vessels [22, 23]. In case of peripheral vascular disease, blocking the sympathetic nervous system causes a vascular dilatation, improving microvascular response [23, 24]. The effect of this sympathetic block may also happen in the lymphatic circulation [23]. The other possible mechanism of SGB is the effect of immune modulation in lymphedema. In subcutaneous tissue of lymphedema, chronic inflammation was observed in some studies [25, 26]. Yokoyama et al. reported a significant alteration in immune activity by SGB, in which the local sympathetic nerve block may modulate the immune response [27]. They used lidocaine only but we used the lidocaine with triamcinolone acetate, which has a strong anti-inflammatory effect; this suggests steroids can help to reduce lymphedema. To verify the effects of steroids on lymphedema, further randomized, controlled studies with various injectates are therefore needed.
Our study has certain limitations. First, the data is retrospective. Despite the significant results of the current study, we could not recommend cervical SGB for BCRL patients with strong evidence. Therefore, further randomized, controlled studies should follow to establish cervical SGB as an effective modality for BCRL patients. Second, although 60 subjects were included, this study had a limitation stemming from its small sample size. Finally, there is no widely accepted protocol of SGB concerning the number of blocks, blocking medicines, and solutions. Precise protocol such as injection times and injectates should be evaluated in a further study.
In conclusion, the results of the present study show that SGB is an effective treatment which can reduce the circumference of the arm in breast cancer-related lymphedema patients. SGB might be an alternative treatment for lymphedema after further studies are followed.
References
Kim KS, Ko HY (1992) Upper extremity lymphedema secondary to breast cancer. J Korean Acad Rehab Med 16:94–100
Warren AG, Brorson H, Borud LJ, Slavin SA (2007) Lymphedema: a comprehensive review. Ann Plast Surg 59:464–472
Bennett Britton TM, Wallace SM, Wilkinson IB, Mortimer PS, Peters AM, Purushotham AD (2009) Sympathetic nerve damage as a potential cause of lymphoedema after axillary dissection for breast cancer. Br J Surg 96:865–869
Hinrichs CS, Watroba NL, Rezaishiraz H, Giese W, Hurd T, Fassl KA, Edge SB (2004) Lymphedema secondary to postmastectomy radiation: incidence and risk factors. Ann Surg Oncol 11:573–580
Querci della Rovere G, Ahmad I, Singh P, Ashley S, Daniels IR, Mortimer P (2003) An audit of the incidence of arm lymphoedema after prophylactic level I/II axillary dissection without division of the pectoralis minor muscle. Ann R Coll Surg Engl 85:158–161
Moseley AL, Carati CJ, Piller NB (2007) A systematic review of common conservative therapies for arm lymphoedema secondary to breast cancer treatment. Ann Oncol 18:639–646
Yamamoto R, Yamamoto T (2007) Effectiveness of the treatment-phase of two-phase complex decongestive physiotherapy for the treatment of extremity lymphedema. Int J Clin Oncol 12:463–468
Boris M, Weindorf S, Lasinkski S (1997) Persistence of lymphedema reduction after noninvasive complex lymphedema therapy. Oncology (Williston Park) 11:99–109, discussion 110, 113–4
Casley-Smith JR, Boris M, Weindorf S, Lasinski B (1998) Treatment for lymphedema of the arm—the Casley-Smith method: a noninvasive method produces continued reduction. Cancer 83:2843–2860
Casley-Smith JR, Morgan RG, Piller NB (1993) Treatment of lymphedema of the arms and legs with 5,6-benzo-[alpha]-pyrone. N Engl J Med 329:1158–1163
Bae H, Kim HJ (2013) Clinical outcomes of extracorporeal shock wave therapy in patients with secondary lymphedema: a pilot study. Ann Rehabil Med 37:229–234
Becker C, Assouad J, Riquet M, Hidden G (2006) Postmastectomy lymphedema: long-term results following microsurgical lymph node transplantation. Ann Surg 243:313–315
Kim HG, Kim K, Seo HG, Im CY, Kim TU, Chung SG, Noh DY, Seo KS (2009) Clinical outcomes of cervical stellate ganglion block in patients with secondary lymphedema: a pilot study. J Korean Acad Rehabil Med 33:297–303
Swedborg I, Arnér S, Meyerson B (1983) New approaches to sympathetic blocks as treatment of postmastectomy lymphedema. Report of a successful case. Lymphology 16:157–163
Kim HR, Kim K, Kim HG, Lim CY, Chun SW, Seo KS (2011) Predicting the effect of stellate ganglion block on the lymphoscintigraphic findings for lymphedema in post-mastectomy patients. J Korean Acad Rehabil Med 35:214–223
Rockson S (2001) Lymphedema. Am J Med 110:288–295
Olszewski WL (2003) Pathophysiological aspects of lymphedema of human limbs: I. Lymph protein composition. Lymphat Res Biol 1:235–243
Liao SF, Huang MS, Li SH, Chen IR, Wei TS, Kuo SJ, Chen ST, Hsu JC (2004) Complex decongestive physiotherapy for patients with chronic cancer-associated lymphedema. J Formos Med Assoc 103:344–348
Szuba A, Achalu R, Rockson SG (2002) Decongestive lymphatic therapy for patients with breast carcinoma-associated lymphedema. A randomized, prospective study of a role for adjunctive intermittent pneumatic compression. Cancer 95:2260–2267
Karadibak D, Yavuzsen T, Saydam S (2008) Prospective trial of intensive decongestive physiotherapy for upper extremity lymphedema. J Surg Oncol 97:572–577
Woo JH, Park HS, Kim SC, Kim YH (2013) The effect of lumbar sympathetic ganglion block on gynecologic cancer-related lymphedema. Pain Physician 16:345–352
Planas-Paz L, Lammert E (2013) Mechanical forces in lymphatic vascular development and disease. Cell Mol Life Sci 70:4341–4354
Mignini F, Sabbatini M, Coppola L, Cavallotti C (2012) Analysis of nerve supply pattern in human lymphatic vessels of young and old men. Lymphat Res Biol 10:189–197
Langley JN (1903) The autonomic nervous system. Brain 26:1–26
Tabibiazar R, Cheung L, Han J, Swanson J, Beilhack A, An A, Dadras SS, Rockson N, Joshi S, Wagner R, Rockson SG (2006) Inflammatory manifestations of experimental lymphatic insufficiency. PLoS Med 3:e254
Piller NB (1990) Macrophage and tissue changes in the developmental phases of secondary lymphoedema and during conservative therapy with benzopyrone. Arch Histol Cytol 53(Suppl):209–218
Yokoyama M, Nakatsuka H, Itano Y, Hirakawa M (2000) Stellate ganglion block modifies the distribution of lymphocyte subsets and natural-killer cell activity. Anesthesiology 92:109–115
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, JG., Bae, S.O. & Seo, K.S. A comparison of the effectiveness of complex decongestive physiotherapy and stellate ganglion block with triamcinolone administration in breast cancer-related lymphedema patients. Support Care Cancer 23, 2305–2310 (2015). https://doi.org/10.1007/s00520-014-2593-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-014-2593-5