Abstract
Purpose
There is clinical need to predict risk of febrile neutropenia before a specific cycle of chemotherapy in cancer patients.
Methods
Data on 3882 chemotherapy cycles in 1089 consecutive patients with lung, breast, and colon cancer from four teaching hospitals were used to construct a predictive model for febrile neutropenia. A final nomogram derived from the multivariate predictive model was prospectively confirmed in a second cohort of 960 consecutive cases and 1444 cycles.
Results
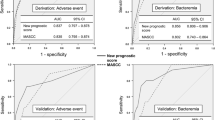
The following factors were used to construct the nomogram: previous history of febrile neutropenia, pre-cycle lymphocyte count, type of cancer, cycle of current chemotherapy, and patient age. The predictive model had a concordance index of 0.95 (95 % confidence interval (CI) = 0.91–0.99) in the derivation cohort and 0.85 (95 % CI = 0.80–0.91) in the external validation cohort. A threshold of 15 % for the risk of febrile neutropenia in the derivation cohort was associated with a sensitivity of 0.76 and specificity of 0.98. These figures were 1.00 and 0.49 in the validation cohort if a risk threshold of 50 % was chosen.
Conclusions
This nomogram is helpful in the prediction of febrile neutropenia after chemotherapy in patients with lung, breast, and colon cancer. Usage of this nomogram may help decrease the morbidity and mortality associated with febrile neutropenia and deserves further validation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Febrile neutropenia is an important risk factor for morbidity and mortality in patients with cancer and may lead to a reduction in the dose of chemotherapy delivered [1–4]. Even when a standard dose of chemotherapy is used, febrile neutropenia may be a non-rare event in daily practice in different settings, for example an incidence rate of 9 % after adjuvant chemotherapy with vinorelbine and cisplatin in patients with non-small cell lung cancer (NSCLC) as shown in the ANITA trial, or more than 20 % for docetaxel and trastuzumab chemotherapy in patients with metastatic breast cancer [5, 6]. Thus, primary or secondary prevention, in particular, through the administration of colony-stimulating factor (CSF) is recommended by various guidelines when there is a considerable risk of febrile neutropenia [7, 8].
Although there exist models to predict the risk of febrile neutropenia, they are either derived from groups of solid cancer patients mixed with cases of hematological malignancy or have not been prospectively validated [4, 9–12]. For these reasons, the 2006 ASCO update on the use of hematopoietic CSFs underlines the need for further studies to develop and prospectively validate an accurate risk model to improve the efficacy and cost-effectiveness of growth factor prophylaxis [8]. At the present time, the criteria for the use of CSF and/or other measures to minimize the risk of febrile neutropenia are to some extent arbitrary and based on low quality evidence. Moreover, they have not been fully validated. In this study, we aimed to develop a clinically useful model to predict the individual risk of febrile neutropenia in patients with solid tumors only and validate this model both internally and externally.
Materials and methods
Patients and data collection
Patients with three types of common cancer (breast, lung, and colorectal cancer) who were receiving any line and any cycle of chemotherapy and were at any stage of disease were prospectively and consecutively entered into the study from two institutions over a course of 8 months between May 2010 and January 2011 for the initial cohort (model derivation cohort) and from four institutions during November 2011 and December 2011 for the external validation cohort. The local ethical committee of Akdeniz University approved the study protocol, prior to the onset of the study. Outpatients receiving chemotherapy at the outpatient chemotherapy units and inpatients receiving chemotherapy in the oncology wards were both enrolled. Disease and patient characteristics, as well as details of present and past treatment, specifics of the chemotherapy protocol, number of cycles, any history of febrile neutropenia, and use of CSF were recorded. Chemotherapy regimens administered during the study were categorized with respect to their risk of inducing febrile neutropenia as previously described [7]. Each patient was carefully observed after each cycle for the development of febrile neutropenia. Febrile neutropenia was defined as the occurrence of a fever of 38.3 °C orally or 38.0 °C for over an hour and a neutrophil count <500 or 500–999/mm3 with a predicted decline to <500/mm3 over the next 48 h [13]. Regular telephone meetings with the investigators from other participating centers were carried out to ensure timely and accurate data management. Our main reason to use a predictive model to estimate the risk of febrile neutropenia was to be able to initiate some preventive measures: CSF, dose reduction, or prophylactic antibiotics. For example, CSF can be initiated in patients without CSF coverage, or dose reduction and/or prophylactic antibiotics can be started in cases that are already on CSF. All data were entered daily into the main database by the participating centers. The outcome of each febrile neutropenia episode was carefully followed or queried. Two centers (Akdeniz University, Department of Medical Oncology and Antalya Training and Research Hospital, Department of Medical Oncology, both in the city of Antalya) recruited patients for model derivation and four centers recruited for validation (Necmettin Erbakan University, Meram Faculty of Medicine, Dept. of Medical Oncology, Konya, and Süleyman Demirel University, Department of Medical Oncology, Isparta, in addition to the two listed above).
Statistical analysis
Derivation of the model
The main outcome variable was the development of febrile neutropenia after a specific cycle of chemotherapy. As the unit of analysis is the cycle of chemotherapy and not the patient, and data are dependent within the same patient, we used univariate and multivariate generalized estimating equation (GEE) models, taking into account the correlation structure within patients. Any factor with a P value <0.10 in the univariate analysis was entered into multivariate analysis. A P value <0.05 was considered necessary for statistical significance.
Validation of the model
External validation was performed to test the robustness of the model in a separate validation cohort of patients who were prospectively recruited from four centers. The risk of febrile neutropenia before a specific cycle of chemotherapy in the validation cohort was calculated using a nomogram of the initial model obtained from the derivation cohort. If score calculated with the use of nomogram prior to a specific cycle of chemotherapy exceeded a certain threshold for the risk of febrile neutropenia, for example 15 %, then it was assumed that the predicted and the actual outcomes for febrile neutropenia were in accordance.
Performance of the model
After applying different threshold levels for the risk of febrile neutropenia, the sensitivity and specificity values of each scenario were calculated. Concordance index (CI) was determined to assess the discrimination of the model.
Results
General characteristics
The derivation cohort comprised 1089 patients and 3880 chemotherapy cycles from two centers. The median age was 55 years (range, 26 to 86), 44.8 % had stage 4 disease, and 25.6 % were using CSF prior to a cycle. Most of the cycles (62.1 %) consisted of a chemotherapy protocol that had a 10–20 % risk of febrile neutropenia. During the study duration, a total of 59 episodes of febrile neutropenia were observed (1.5 % of total cycles) (Table 1). With respect to the cycle of chemotherapy administered, 2.7 % of the first cycle, 1 % of the second cycle, 1.6 % of the third, 1.2 % of the fourth and the fifth, and 0.6 % of the sixth cycles and beyond were effected by febrile neutropenia.
The external validation cohort consisted of 960 patients and 1444 cycles of chemotherapy from four centers. The characteristics of this cohort were similar to those of the derivation cohort with a 25.3 % lung cancer frequency, 17.4 % CSF usage rate for prophylaxis, and 18 episodes of febrile neutropenia (1.2 % of total cycles) (Table 2).
Derivation of the generalized estimating equations model
In the univariate analysis, 16 of the 36 factors tested were associated with the occurrence of febrile neutropenia. Five of these 16 factors retained their significance in the multivariate analysis: four factors had significant P values; cycle of current chemotherapy, previous history of febrile neutropenia, type of cancer, and pre-cycle lymphocyte count. In addition, because patient age had a marginal significance in the multivariate model, and previous literature suggested it might be a significant factor, it was also incorporated into the final multivariate model. The specifics of the predictors of febrile neutropenia in the derivation cohort are presented in Table 3.
The resultant coefficients of this final model were then used to construct a nomogram. Please refer to the table in Fig. 1 for details of the nomogram.
Nomogram for the risk of febrile neutropenia after standard dose chemotherapy in common solid tumors. 1Any episode of febrile neutropenia with the current protocol or a previous protocol; 2based on precycle blood counts; 3current cycle of chemotherapy with the present protocol; omega (Ω) symbol indicates breast or colorectal cancer. In order to calculate risk of febrile neutropenia, add up individual points (on the individual point line) to find total points (on the total point line) which correspond to a risk of febrile neutropenia (on the risk of febrile neutropenia line)
External validation of the model
The validity of the derived model and the nomogram was tested in a second prospective cohort of consecutive patients from four centers. When a cut off threshold of 0.50 for the risk of febrile neutropenia was chosen, sensitivity and specificity values were 1.00 and 0.49, respectively. The performance details of external validation are shown in Table 4.
Performance of the model
If a cut off level of 0.15 for febrile neutropenia was specified, the sensitivity and specificity values in the derivation cohort were 0.76 and 0.98, respectively (see Table 4 for details of the performance of the model). The predictive model had a concordance index of 0.95 (95 % confidence interval (CI) = 0.91–0.99) in the derivation cohort, and 0.85 (95 % CI = 0.80–0.91) in the external validation cohort. Also, in the derivation cohort, for patients who did not use CSF, the concordance index was 0.96 (95 % CI = 0.92–0.99), as opposed to 0.93 (95 % CI = 0.84–1.00) in patients that did use CSF, and these figures were very close.
Discussion
This is an externally validated predictive model to define the risk of febrile neutropenia after chemotherapy in patients with common cancers. This model thus allows pretreatment identification of patients who are likely to develop febrile neutropenia after a specific cycle of chemotherapy. Thus, we think that the nomogram derived from our model will be helpful in daily clinical practice to guide efforts for the prophylaxis of febrile neutropenia. Previous predictive models for febrile neutropenia are either derived from mixed populations including patients with hematological malignancies or have not been externally validated [4, 9–15]. Although Bley et al. prospectively tested their model in two cohorts, the data were very limited for patients with solid tumors; among the 104 patients prospectively tested, only 53 had heterogeneous solid tumors [16]. For these reasons, we believe that the current model represents significant progress in predicting febrile neutropenia and optimizing protection against it. Usage of growth factors, dose reduction or prophylactic antibiotics are among the potential preventive measures in this setting.
The cycle number of the current chemotherapy is two important factors of the current model, and our results indicate that earlier cycles of chemotherapy have a greater risk of febrile neutropenia. This is in accordance with previous studies, in which various investigators have shown that the first cycle of chemotherapy in particular has a greater risk for the development of febrile neutropenia compared with subsequent cycles [17, 18]. The reduced risk of febrile neutropenia after subsequent cycles might be because the nadir of blood counts and clinical characteristics of a patient while on chemotherapy give the clinician extra time and opportunity to lessen the risk, such as by decreasing the chemotherapy drug dosages and/or starting CSF. For example, current guidelines suggest the use of CSF as a secondary prophylaxis in patients who develop febrile neutropenia on the same or equitoxic chemotherapy protocol, taking into consideration a patient’s previous tolerance to chemotherapy [2, 7]. Thus, a history of febrile neutropenia in a patient is a widely recognized risk factor for the development of other febrile neutropenia episodes and was also the most significant factor associated with febrile neutropenia in our analysis.
In our model, a higher baseline lymphocyte count appears to be protective against febrile neutropenia. We believe that higher lymphocyte counts may reflect higher resistance to infection, as these patients may have the potential to activate their humoral or cellular immunity more readily. The precise role of lymphocytes in the development of febrile neutropenia remains to be determined. Interestingly, it has also been demonstrated that baseline or fifth-day lymphocyte counts independently predict the risk of febrile neutropenia [15, 16]. In addition, we found that lung cancer patients had a higher rate of developing febrile neutropenia than breast and colorectal cancer patients. This may be related to the more aggressive nature of this disease, as reflected by poorer survival figures in advanced disease, and/or the more toxic nature of some of the chemotherapy protocols used in our cohort.
We had enriched our model with an additional variable: patient age. Clinicians are aware of the fact that myelosuppression is more common in the elderly cancer patient population. Indeed, this factor was significant in the univariate analysis, with a borderline significance in the multivariate analysis, as well. It is also well known that use of CSF decreases the risk of febrile neutropenia [7, 19]. Numerous analyses have estimated the protective effect of CSF to be around 50 %. In our study, CSF usage was also associated with a reduced risk of febrile neutropenia, although this was not statistically significant. This statistical nonsignificance may stem from the fact that CSF use for prophylaxis was already more frequent in our cohort than expected.
One shortcoming in our study is the low prevalence of febrile neutropenia episodes in the derivation and validation cohorts: 1.5 and 1.2 %, respectively, of the chemotherapy cycles administered. Secondly, the rate of CSF use prior to a cycle, either for primary or secondary prophylaxis, appears to be high in both the derivation and validation cohorts: 25.6and 17.4 %, respectively. We believe that these two shortcomings reflect a highly cautious strategy to minimize the risk of febrile neutropenia. We showed the validity of our nomogram in patients with breast, lung, and colorectal cancers. However, using our nomogram in different patient populations with different cancers, or treated with different approaches or strategies, may yield slightly different results and could affect the generalizability of our findings. Thus, our results preferably need to be replicated by other investigators and in different settings.
It is to be kept in mind that the decision of growth factors was not guided in this study. Although this may be regarded as a limitation of the nomogram as it should also be a tool for guiding the decision to use or not growth factors, we used data on the use of growth factors as they are used in the real clinical life from four hospitals; thus, this approach to some extent reflects applicability to daily clinical routine.
Nomograms have been used in the field of oncology for many years [20, 21]. In the construction of our nomogram, we used the most recent methodology [22], and we believe that this is the first validated nomogram to estimate the risk of febrile neutropenia in three common cancers. The performance of the model underlying this nomogram and the potential to reduce the morbidity and mortality associated with febrile neutropenia make this model a candidate for clinical use at oncology clinics to estimate the risk of febrile neutropenia.
In short, we describe in this paper a prospectively validated model to estimate the risk of febrile neutropenia. Using this model, it may be possible to take additional preventive measures against the development of febrile neutropenia and consequently decrease the associated morbidity and mortality. Application of this nomogram in daily practice may help with the risk stratification and the prevention of febrile neutropenia. Thus, our nomogram deserves further validation by other groups.
References
Herbst C, Naumann F, Kruse EB et al (2009) Prophylactic antibiotics or G-CSF for the prevention of infections and improvement of survival in cancer patients undergoing chemotherapy. Cochrane Database Syst Rev 1:CD007107
Aapro MS, Cameron DA, Pettengell R et al (2006) European organisation for research and treatment of cancer (EORTC) granulocyte colony-stimulating factor (G-CSF) guidelines working party. EORTC guidelines for the use of granulocyte-colony stimulating factor to reduce the incidence of chemotherapy-induced febrile neutropenia in adult patients with lymphomas and solid tumours. Eur J Cancer 42:2433–2453
Kelly S, Wheatley D (2009) Prevention of febrile neutropenia: use of granulocyte colony stimulating factors. Br J Cancer 101:6–10
Aapro M, Crawford J, Didier K (2010) Prophylaxis of chemotherapy induced febrile neutropenia with granulocyte colony stimulating factors: where are we know? Support Care Cancer 18:549–541
Douillard JY, Rosell R, De Lena M et al (2006) Adjuvant vinorelbine plus cisplatin versus observation in patients with completely resected stage IB-IIIA non-small-cell lung cancer (Adjuvant Navelbine International Trialist Association [ANITA]): a randomised controlled trial. Lancet Oncol 7(9):719–727
Marty M, Cognetti F, Maraninchi D et al (2005) Randomised phase II trial of the efficacy and safety of trastuzumab combined with docetaxel in patients with epidermal growth factor receptor-2 positive metastatic breast cancer administered as first line treatment. The M77001 Study Group. J Clin Oncol 23:4265–4274
NCCN Guidelines. Myeloid growth factors. Version 1 (2013) (http://www.nccn.org/professionals/physician_gls/pdf/myeloid_growth.pdf)
Smith TJ, Khatcheressian J, Lyman GH et al (2006) 2006 update of the recommendations for the use of white blood cell growth factors: an evidence-based clinical practice guideline. J Clin Oncol 24(19):3187–3205
Lynman GH, Lynman CH, Agboola O (2005) Risk models for chemotherapy-induced neutropenia. Oncologist 10:427–437
Dranisatris G, Rayson D, Vincent M et al (2008) Identifying patients at high risk for neutropenic complications during chemotherapy for metastatic breast cancer with doxorubicin or pegylated liposomal doxorubicin: the development of a prediction model. Am J Clin Oncol 31:369–374
Pettengell R, Bosly A, Szucs TD et al (2009) Multivariate analysis of febrile neutropenia occurrence in patients with non-Hodgkin lymphoma: data from the INC-EU prospective observational European Neutropenia Study. Br J Haematol 144:677–685
Ziepert M, Schmits R, Trumper L et al (2008) Prognostic factors for hematotoxicity of chemotherapy in aggressive non-Hodgkin’s lymphoma. Ann Oncol 19:752–762
Lynman GH, Kuderer NM (2003) Epidemiology of febrile neutropenia. Support Cancer Ther 1:23–35
Morrison VA, Caggiano V, Fridman M et al. (2004) A model to predict chemotherapy-related severe or febrile neutropenia in cycle one among breast cancer or lymphoma patients. Proc Am Soc Clin Oncol 23 (abstr 742)
Ray-Coquard I, Borg C, Bachelot T et al (2003) Baseline and early lymphopenia predict for the risk of febrile neutropenia after chemotherapy. Br J Cancer 88:181–186
Blay JY, Chauvin F, Le Cesne A et al (1996) Early lymphopenia after cytotoxic chemotherapy as a risk factor for febrile neutropenia. J Clin Oncol 14:636–643
Gomez H, Hidalgo M, Casanova L et al (1986) Risk factors for treatment-related death in early patients with aggressive non-Hodgkin’s lymphoma: results of a multivariate analysis. J Clin Oncol 16:2065–2069
Crawford J, Dale DC, Lyman GH (2004) Chemotherapy induced neutropenia. Cancer 100:228–237
Gridelli C, Aapro MS, Barni S et al (2007) Role of colony stimulating factors in solid tumors: results of an expert panel. Crit Rev Oncol Hematol 53:53–64
Kattan MW, Scardino PT (2007) Evidence for the usefulness of nomograms. Nat Clin Pract Urol 4:638–639
Andrews JV, Cronin AM (2010) Everything you always wanted to know about evaluating prediction models. Urology 76(6):1298–1301
Iasanos A, Schrag D, Raj GV, Panageas K (2008) How to build and interpret a nomogram for cancer prognosis. J Clin Oncol 26:1364–1370
Acknowledgments
This paper was professionally edited by BioScience Writers. We thank Prof. Dr. Mustafa Özdoğan, MD (medical oncologist) and Prof. Dr. Rabin Saba, MD (specialist in infectious diseases) for their suggestions on the design of this study.
All named authors have read the manuscript, have agreed to the submission and have participated in the study to a sufficient extent to be named as authors.
Conflict of interest
Authors do not have any conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bozcuk, H., Yıldız, M., Artaç, M. et al. A prospectively validated nomogram for predicting the risk of chemotherapy-induced febrile neutropenia: a multicenter study. Support Care Cancer 23, 1759–1767 (2015). https://doi.org/10.1007/s00520-014-2531-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-014-2531-6