Abstract
Purpose
Hydronephrosis is a frequently observed but understudied complication in patients with cervical cancer. To better characterize hydronephrosis in cervical cancer patients, the current study sought (1) to describe hydronephrosis-associated morbidity and (2) to analyze the prognostic effect of hydronephrosis in patients with a broad range of cancer stages over time.
Methods
The Mayo Clinic Tumor Registry was interrogated for all invasive cervical cancer patients seen at the Mayo Clinic from 2008 through 2013 in Rochester, Minnesota; these patients’ medical records were then reviewed in detail.
Results
Two hundred seventy-nine cervical cancer patients with a median age of 49 years and a range of cancer stages were included. Sixty-five patients (23 %) were diagnosed with hydronephrosis at some point during their disease course. In univariate analyses, hydronephrosis was associated with advanced cancer stage (p < 0.0001), squamous histology (p = 0.0079), and nonsurgical cancer treatment (p = 0.0039). In multivariate analyses, stage and tumor histology were associated with hydronephrosis. All but one patient underwent stent placement or urinary diversion; hydronephrosis-related morbidity included pain, urinary tract infections, nausea and vomiting, renal failure, and urinary tract bleeding. In landmark univariate survival analyses, hydronephrosis was associated with worse survival at all time points. In landmark multivariate analyses (adjusted for patient age, stage, cancer treatment, and tumor histology), hydronephrosis was associated with a trend toward worse survival over time (hazard ratios ranged from 1.47 to 4.69).
Conclusion
Hydronephrosis in cervical cancer patients is associated with notable morbidity. It is also associated with trends toward worse survival—even if it occurs after the original cancer diagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hydronephrosis develops when a blockage in the renal collecting system leads to distention of the renal calyces. Women with cervical cancer often develop this complication as a result of tumor or lymph node encroachment, inflammation, or scarring at the pelvic rim. In an effort to relieve obstructive symptoms, patients can undergo stent placement or urinary diversion procedures [1–8]. In addition, cervical cancer is often treated with nephrotoxic drugs, which are sometimes dose-modified or omitted when hydronephrosis is associated with renal insufficiency [8]. Such dose changes can compromise cancer treatment and potentially lead to compromised clinical outcomes, thus emphasizing the importance of studying hydronephrosis in patients with cervical cancer. Furthermore, this complication has been associated with pain related to inflammation of the kidney and surrounding structures.
At least two topics related to hydronephrosis continue to generate controversy. First, a dearth of studies has examined morbidity in cervical cancer patients who have been diagnosed with this complication. Lapitan and Buckley undertook a prospective quality of life assessment of cervical cancer patients with hydronephrosis and reported that quality of life did not change over 1 year [9]. However, this study did not specifically describe hydronephrosis-related morbidity, and it relied on a quality of life tool that was not highly germane to the issues patients with hydronephrosis encounter. The fact that a limited number of studies catalog hydronephrosis-related morbidity denotes one gap in the published literature. Second, previous studies report that hydronephrosis predicts compromised survival. Pradhan and others described that among 197 cervical cancer patients, hydronephrosis was associated with a statistically significant doubling of the risk for death [3]. Other investigators have reported similar prognostic outcomes in both univariate and multivariate analyses, although not consistently so [1, 2]. However, these studies are older, recounting a patient experience that might no longer be contemporaneous and relevant. These studies also focused exclusively on patients with stage III cancer, an approach which can be justified based on the fact that the FIGO staging of cervical cancer ascribes stage III disease to patients with tumor-related hydronephrosis [1–3]. Clearly, however, patients with cervical cancer can develop hydronephrosis later in their disease course, and those who develop hydronephrosis as a postcancer diagnosis complication also merit inclusion in prognostic studies. An updated clinical experience that includes an assessment of morbidity and that includes patients with various stages of cancer with hydronephrosis that occurred at various time points after cancer diagnosis would address both these salient gaps in the published literature.
In this context, the current study sought to capture the morbidity associated with hydronephrosis and to understand the prognostic implications of this cancer- and cancer treatment-related complication in patients of with a broad range of cancer stages and with hydronephrosis that occurred at various time points with respect to their cancer diagnosis. A more thorough understanding of both the morbidity and prognostic implications of hydronephrosis might lead to improvement in the palliative management of cervical cancer patients and to the identification of areas in need of further research.
Methods
Overview
The Mayo Clinic Institutional Review Board approved this study, and thereafter, the Mayo Clinic Tumor Registry provided a list of all patients with cervical cancer seen at the Mayo Clinic from 2008 through 2013 in Rochester, Minnesota. These dates were chosen in order to provide a contemporary experience with minimal overlap with previously published studies.
Information abstracted from the medical record
Each patient’s medical record was reviewed in detail. Abstracted information included patient date of birth; date of cancer diagnosis; cancer stage; cancer histology; cancer treatment modalities, such as surgery, chemotherapy, and radiation; and vital status. Vital status was acquired from the medical record and, via the Mayo Clinic Tumor Registry, from the Social Security Death Index. Additionally, date of diagnosis of hydronephrosis, method of diagnosis, whether bilateral or unilateral, management, and complications related to management were also abstracted from the medical record. Of note, this study did not attempt to determine the etiology of hydronephrosis, in view of the complexity and potential inaccuracies of such attribution attempts and in view of the heightened challenges of a retrospective study design. If an exact date was not available in the medical record, a midmonth or midyear date was imputed.
Data analyses
Data are presented descriptively with percentages, medians, and ranges as appropriate. The Wilcoxon rank-sum test was used to compare continuous variables between two-level categorical variables of interest. Chi-square tests were used to assess relationships between categorical variables, and univariate and multivariate logistic regression models were used to assess relationships between clinical variables and hydronephrosis. Cox proportional hazards models were used to assess relationships between clinical variables (including hydronephrosis) and overall survival. Overall survival was defined as the time from cancer diagnosis to death from any cause; patients still alive were censored at the date of last follow-up. Because hydronephrosis occurred at varying times during patients’ course of disease, a landmark analysis was performed at various times to assess the prognostic impact of hydronephrosis in univariate and multivariate Cox proportional hazards models. The inclusion of variables in both the logistic regression models and the Cox proportional hazards models was based on precedent in the published literature [1–3]. Because of the variability in approaches to cancer surveillance, cancer status was not used in the multivariate Cox proportional hazards models, although cancer stage was. A two-sided p value of <0.05 was considered statistically significant. Data were analyzed with JMP®, Cary, North Carolina, USA.
Results
Demographics
Two hundred seventy-nine cervical cancer patients were included in this study. Their median age at cancer diagnosis was 49 years (range 21–92). Sixty-five patients (23 %) were diagnosed with hydronephrosis at some point during their disease course. Compared to patients with no hydronephrosis, patients with this complication tended to be older at cancer diagnosis (median age 54 vs 47 years; p = 0.0295) with a higher rate of squamous histology (72 vs 58 %; p = 0.0373) and more advanced cancer stage at diagnosis (p < 0.0001) (Table 1).
Hydronephrosis rates
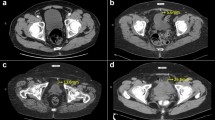
The rate of hydronephrosis is noted above. In 51 patients, the diagnosis of hydronephrosis occurred after the original diagnosis of cancer, and the median interval from cancer diagnosis to the diagnosis of hydronephrosis was 11 weeks. In the 30 hydronephrosis patients who underwent surgery, the hydronephrosis followed surgery in 22 patients, and the median time from surgery to diagnosis of hydronephrosis was 32 weeks (range 2 weeks–21 years). Hydronephrosis was diagnosed by computerized tomography (CT) scan alone in 48 patients, by ultrasound alone in 9, by CT scan and ultrasound in 4, by ultrasound and other imaging in 2, with unknown information available in the others. Hydronephrosis was bilateral in 22 patients (34 %).
Among the patients diagnosed with hydronephrosis, 35 were eventually diagnosed with cancer recurrence; the hydronephrosis followed the cancer recurrence in 16 patients (46 %), occurred at the same time in 6 (17 %), and preceded it in the remaining patients.
Hydronephrosis risk factors, management, and morbidity
Univariate logistic regression analyses showed that the development of hydronephrosis at any time point was directly associated with more advanced cancer stage (p < 0.0001), squamous histology (p = 0.0079), and nonsurgical treatment modalities (p = 0.0039) (Table 2). Multivariate analyses showed similar findings except treatment modality lost its statistical significance (Table 2).
Management consisted of stent placement in 48 patients (74 %), nephrostomy tube in 15 (23 %), ureterostomy tube in one (2 %), and no treatment in the remaining patient.
Seventeen patients suffered notable morbidity, which included pain, urinary tract infections, nausea and vomiting, renal failure, and urinary tract bleeding (Table 3). Seven patients experienced more than one type of morbidity.
Of note, 76 patients within this entire group of cervical cancer patients developed recurrent cancer, and 36 of these patients with recurrent cancer also developed hydronephrosis at some time point. Cumulative cancer therapy in patients who developed both recurrent cancer and hydronephrosis included chemotherapy alone (11), chemotherapy/radiation (9), surgery/radiation/chemotherapy (5), radiation alone (4), surgery alone (3), surgery/radiation (2), and no cancer treatment (2).
Prognosis and hydronephrosis
In the 278 patients with survival data, 221 were still alive at the time of this report with a median follow-up of 1.5 years (range 0.02–5.4 years). Among these 278 patients, 57 had died at the time of this report.
In univariate survival analyses, as assessed from the date of cancer diagnosis, patients who developed hydronephrosis at any point during their cancer course manifested a worse survival compared to those who did not develop this complication. Three-year survival rates were 37 % (95 % confidence interval (CI) 14–68 %) and 74 % (95 % CI 66–80 %), respectively, for those with and without hydronephrosis (hazard ratio (HR) = 4.00 (95 % CI 1.75, 8.01); p = 0.0021) (Table 4). However, this prognostic effect was no longer observed when patient age at cancer diagnosis, tumor stage, nonsurgical cancer treatment, and tumor histology were included in the multivariate model (p = 0.2097) (Table 4). In this multivariate model, cancer stage was the only statistically significant prognostic factor (p = 0.0036).
However, in landmark univariate survival analyses, hydronephrosis remained a statistically significant prognostic factor associated with worse survival at all time points (Table 5). In landmark multivariate analyses, after adjusting for patient age at cancer diagnosis, tumor stage, nonsurgical cancer treatment, and tumor histology, hydronephrosis was associated with worse survival from 9 to 18-month postcancer diagnosis (Table 5).
Discussion
This study undertook the twofold task of cataloging morbidity in cervical cancer patients who developed hydronephrosis and of better understanding the prognostic implications of this cancer- and cancer treatment-related complication. In terms of morbidity, 65 patients (23 %) developed hydronephrosis during their disease course, and 17 of these patients developed notable morbidity, which included pain, urinary tract infections, nausea and vomiting, renal failure, and urinary tract bleeding. In view of the fact that nearly all these patients underwent a stent or diversion procedure, it is challenging to distinguish between morbidity from the hydronephrosis and procedure-related morbidity. Nonetheless, the realization that a quarter of patients with hydronephrosis appear to suffer notable morbidity—which likely goes underreported to some extent in a retrospective study such as this one—speaks to the need to further study patient-reported outcomes in cervical cancer patients who develop this complication.
Second, from a prognostic standpoint, this study demonstrates that cervical cancer patients who develop hydronephrosis at any point during their cancer trajectory manifest a trend toward poor survival from the time they develop hydronephrosis. To our knowledge, this observation has not been previously investigated and reported in patients with various stages of cervical cancer and suggests a heightened concern for the implications of hydronephrosis. To analyze the impact of hydronephrosis on survival, with the use of more traditional survival analysis methods, longer survival itself will positively impact the possibility that patients will eventually develop hydronephrosis and thereby potentially lead to biased survival in favor of hydronephrosis patients. For this reason, we opted to conduct landmark analyses. These analyses included patients who were alive at well-demarcated time points; at the time of these well-demarcated time points, we compared outcomes among patients who had and had not developed hydronephrosis. The resulting trend is that hydronephrosis that occurs after a diagnosis of cervical cancer is associated with compromised survival. This observation raises the question of whether the hydronephrosis resulted in compromised cancer treatment perhaps because of the limited potential of prescribing nephrotoxic drugs or whether this complication is a manifestation of progressive, more aggressive cancer. Although it is difficult to make such distinctions, the prognostic effect of this cancer complication suggests that future clinical trials conducted in patients with metastatic cervical cancer should consider including hydronephrosis as a stratification factor to gain a more accurate understanding of survival-related endpoints. This observation also suggests that health care providers should consider counseling cervical cancer patients about the seriousness of this complication.
Admittedly, a growing literature shows that hydronephrosis can occur in patients after surgery for cervical cancer even under circumstances where no specific trauma to ureters was noted during the operation [10]. Under such circumstances, hydronephrosis is persistent at 3 months in only 15 % of patients, who initially sustained this complication, an observation that raises the question of whether this complication has any clinical implications in the majority of postoperative patients [10]. Simultaneously, a growing literature also suggests that stent placement reverses the negative prognostic effect of hydronephrosis [1]. Tension appears to exist as to whether to place a stent or not early on, but the morbidity observed in this study perhaps tips the scales toward not stenting as readily, particularly in a postoperative setting. This question of when to stent, how to stent, and when to observe, particularly in patients who may be candidates for impending cancer treatment with nephrotoxic drugs, is another area that perhaps merits further research.
In summary, this study adds to an extant published literature on hydronephrosis in patients with cervical cancer. It demonstrates that this cancer-related complication or cancer treatment-related complication is associated with notable morbidity and shortened survival. It also suggests that this complication merits further study with the goal of reducing this morbidity, understanding its prognostic effect, and ultimately improving survival in patients with cervical cancer.
References
Rose PG, Shamshad A, Whitney CW et al (2010) Impact of hydronephrosis on outcome of stage IIIB cervical cancer patients with disease limited to the pelvis, treated with radiation and courrent chemotherapy: a Gynecological Oncology Group study. Gynecol Oncol 117:270–275
Chao KSC, Leung W, Grigsby PW et al (1998) The clinical implications of hydronephrosis and the level of ureteral obstruction in stage IIIB cervical cancer. Int J Radiat Oncol Biol Phys 40:1095–1100
Pradham TS, Duan H, Katsoulakis E et al (2011) Hydronephrosis as a prognostic indicator of survival in advanced cervix cancer. Int J Gynecol Cancer 21:1091–1096
Wit EMK, Horenblas W (2014) Urological complications after treatment of cervical cancer. Nat Rev Urol 11:110–117
Atuhairwe S, Busingye RB, Sekikubo M, Nakimuli A, Mutyaba T (2011) Urologic complications among women with advanced cervical cancer at a tertiary referral hospital in Uganda. Int J Gynecol Obstet 115:282–284
Hazewinkel MH, Gietelink L, ven der Velden J et al (2012) Renal ultrasound to detect hydronephrosis: a need for routine imaging after radical hysterectomy? Gynecol Oncol 124:83–86
Paick SH, Oh SY, Kim HH (2003) The natural history of hydronephrosis after radical hysterectomy with no interoperatively recognizable injury to the ureter: a prospective study. BJU Int 92:748–750
Morris M, Eifel PJ, Grisby PW et al (1999) Pelvic radiation with concurrent chemotherapy compared with pelvic and para-aortic radiation for high-risk cervical cancer. N Engl J Med 340:137–143
Lapitan MC, Buckley BS (2011) Impact of palliative urinary diversion by percutaneous nephrostomy drainage and ureteral stenting among patients with advanced cervical cancer and obstructive uropathy: a prospective cohort. J Obstet Gynaecol Res 37:1061–1070
Suprasert P, Euathrongchit J, Suryachai P et al (2009) Hydronephrosis after radical hysterectomy: a prospective study. Asian Pac J Cancer Prev 10:375–378
Funding
This work was funded by 5K24CA131099.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Patel, K., Foster, N.R., Kumar, A. et al. Hydronephrosis in patients with cervical cancer: an assessment of morbidity and survival. Support Care Cancer 23, 1303–1309 (2015). https://doi.org/10.1007/s00520-014-2482-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-014-2482-y