Summary
Background
The therapeutic effects of music have been known for thousands of years. Recently, studies with music interventions in patients with cardiovascular diseases yielded controversial results. The aim of this review is to provide an overview of the effects of receptive music intervention on the cardiovascular system.
Methods
We searched in PubMed, SCOPUS and CENTRAL for publications between January 1980 and May 2018. Primary endpoints were heart rate, heart rate variability and blood pressure. Secondary endpoints comprised respiratory rate, anxiety and pain. The quality of the studies was assessed by using the CONSORT statement and the Cochrane risk of bias assessment tool. A meta-analysis and subgroup analyses concerning music style, gender and region were planned.
Results
A total of 29 studies comprising 2579 patients were included and 18 studies with 1758 patients investigated the effect of music on patients undergoing coronary angiography or open heart surgery. Other studies applied music to children with congenital heart diseases, pregnant women with hypertension or patients with unstable angina. Due to high methodological study heterogeneity, a meta-analysis was not performed. The study quality was assessed as medium to low. In ten studies with higher quality comprising 1054 patients, music intervention was not associated with significant changes in the cardiovascular endpoints compared to the control group. The subgroup analyses did not demonstrate any relevant results.
Conclusion
Currently no definite effect of receptive music intervention on the cardiovascular system can be verified. Further research is needed to assess music as an inexpensive and easy applicable form of therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The therapeutic effects of music have been known for thousands of years [1]; however, it remains unclear how music affects the human body. Most hypotheses assume that music, in addition to its conscious perception, influences the autonomic and central nervous system at subcortical levels and that the limbic system plays a crucial role in the processing of musical elements [2]. The influences on the limbic system also explain the strong effect on mood which may result in changes of cardiovascular parameters mediated by the autonomic nervous system.
The majority of previous studies focused on the anxiolytic and stress-reducing effects of music rather than on the direct impact on cardiovascular outcomes [3], although it is well acknowledged that a close connection exists between the psychological processes and functional parameters, such as blood pressure, heart rate and heart rate variability. Therefore, the application of music as an adjuvant therapy for various diseases has been expanded over the past few years [4]. The aim of this review is to specifically focus on the effect of music in patients with cardiovascular diseases and during cardiovascular interventions.
Methods
Two reviewers (CH and CS) independently searched three electronic databases (PubMed, SCOPUS, CENTRAL) between June 2018 and February 2019 for the following predefined terms: “influence of music”, “music, cardiovascular system” , “music, heart”, “music, cardiac”, “music, hypertension”, “music, heart rate”, “music, newborns”, “arrhythmia, music”, “music, catheterization”, “music, coronary angiography”, “music, myocardial infarction”, “music, cardiac surgery”, “music, sudden death”, “music, coronary artery disease” , “music, catheter ablation”, “music, coronary intervention”, “music, pacemaker”, “music, defibrillator”, “music, congenital heart disease”. A screening of the titles and abstracts of the publications between 1 January 1980 and 31 May 2018 was performed according to predefined inclusion and exclusion criteria (Table 1). Studies with one or more exclusion criteria and those that did not meet all inclusion criteria were excluded. To identify further publications, bibliographic lists of relevant studies or reviews were searched.
The primary outcomes were heart rate, heart rate variability and blood pressure. The secondary outcomes included respiratory rate, oxygen saturation, skin temperature, hormone levels, and psychological parameters (anxiety, stress, depression, pain, quality of life).
The following data were extracted: general information (title and author of the study, year and country of publication), information on study design, type of randomization, music intervention, duration of music exposure, music genre, control intervention, setting, participants (number of patients, gender, age, ethnicity) and the outcome parameters.
The consolidated standards of reporting trials (CONSORT) checklist was used to assess the quality of randomized controlled trials [5]. The risk of bias (RoB), which is classified into selection, attrition, detection, performance and reporting bias, was assessed as low risk, high risk, or unclear risk by using the Cochrane risk of bias assessment tool [6].
Discrepancies concerning the results of the search as well as the quality assessment were carefully documented.
Statistical analyses were performed and graphics were generated by using the software Review Manager 5.3 of the Cochrane Collaboration [7]. Additional subgroup analyses were carried out by gender, age, cardiovascular diseases/interventions or cardiac surgery, time of the music intervention, music selection, setting, region, study duration and type of music.
This review was completed as part of a diploma thesis. The institutional review board of the community of Vienna considered no necessity of an approval for the present study.
Results
Results of the search
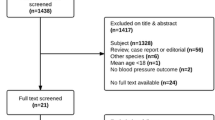
The search of the electronic databases PubMed, SCOPUS and CENTRAL delivered a total of 20,910 results. After the exclusion of double entries (n = 16,688), 38 potentially relevant publications were identified from the remaining 4222 papers (Fig. 1). Searching the reference lists of the included studies did not reveal any additional studies. Attempts were made to access the full text of nine of these 38 publications that were not readily available and five authors immediately replied providing the full text. The remaining four studies were excluded as no full text was available. Five further publications were excluded as indicated in Fig. 1. There were no discrepancies between both reviewers with respect to the screening and inclusion of the studies.
Included studies
A total of 29 studies were selected for inclusion in this review, reporting a total of 2579 patients (Table 2; [8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36]). The sample size varied between 30 and 240 patients and the duration of each music intervention between 15 min and 1h. The majority of studies (n = 20) examined the influence of music within a single intervention. Kunikullaya et al. [24] conducted a study for three months, representing the study with the longest duration and eight other publications applied more than one single music intervention [12, 13, 16, 19, 31, 32, 34, 35].
A total of 18 studies were found, comprising 1758 patients undergoing elective coronary angiography, coronary artery bypass grafting (CABG) and/or aortic valve replacement (AVR) [9,10,11,12, 14, 15, 17, 18, 20, 21, 23, 26,27,28,29, 31, 33]. Music was applied to pregnant women in three [16, 32, 35] and to children with congenital heart diseases in two further studies [8, 22]. Three further studies investigated the changes in physiological parameters in (pre)hypertensive patients [13, 24, 34], two studied the effect of receptive music intervention in patients with unstable angina [19] or acute myocardial infarction [36]. In one study, music had been applied during coronary computed tomography (Table 2; [25]).
A great variety of music styles was used in the studies, including Turkish [13, 35], Indian [24], classical [19, 22, 34, 36] and relaxing music [10, 18, 21, 26,27,28, 30, 32] as well as nature-based sounds [9, 23, 29]. In 11 studies, the music applied was not transparent [8, 11, 12, 14,15,16,17, 20, 25, 31, 33]. Overall, only ten studies provided a clear description of the musical structures such as rhythm, tempo and melody [18, 21,22,23, 26,27,28, 31, 34, 36].
Quality assessment
The included studies fulfilled between 24% and 69% of the criteria of the CONSORT statement (Table 2). None of the studies could achieve more than 75% of the CONSORT aspects. For ten studies, the percentage of fulfilled CONSORT aspects was below 50%.
Overall, 21 discrepancies with respect to the assessment based on the CONSORT statement (mostly regarding the aspects abstract, eligibility criteria and discussion) were resolved through discussion between the two reviewers.
Concerning the RoB, only two studies with a low RoB were identified (Figs. 2 and 3; [8, 9]). The highest RoB was found in the study by White [36]. Performance bias and detection bias of subjective outcomes (anxiety, pain) were found to be particularly high. In contrast, attrition and detection bias of objective outcomes (heart rate, blood pressure, heart rate variability) were assessed as low risk in most cases. Overall, a predominance of studies with high or unclear RoB was found.
A statistical analysis and graphical depiction of publication bias could not be performed due to missing data (e.g. missing mean values and standard deviations of the reported outcomes) and extensive methodological heterogeneity among the studies (e.g. different patient groups and the great variety of music selected in the experiments).
Study results and meta-analysis
Overall, 11 studies of higher quality, defined as publications that achieved more than 50% of the aspects in the CONSORT statement and were assessed with a high RoB in three or less categories, were identified [9, 11, 18, 23,24,25,26,27,28, 30, 35]. Only one of these 11 studies reported a significant reduction of blood pressure in the music group compared to the control arm [35]. In the remaining ten studies of higher quality comprising 1054 patients, music intervention was not associated with significant changes in the cardiovascular endpoints compared to the control group (Table 2; [9, 11, 18, 23,24,25,26,27,28, 30]). In three of these ten studies, though, heart rate and blood pressure demonstrated a decreasing trend in the music group [18, 23, 27]. Interestingly, Kunikullaya et al. observed significant reductions of diastolic blood pressure only in both the interventional and control group as well as an increasing trend in parasympathetic parameters of heart rate variability, although not statistically significant [24]. Regarding the psychological outcomes, significantly greater anxiolytic effects in the music group compared to the control arm were found in three studies [9, 18, 23]. Kunikullaya et al. reported a reduction of anxiety in both the intervention and control group, indicating that both lifestyle modification and music intervention have anxiety relieving effects in patients with hypertension [24]. Furthermore, although psychological outcomes were not statistically significant in six studies [11, 25, 26, 28, 30, 35], two studies reported that the music intervention had a calming effect on and was highly appreciated by the patients during the procedure [11, 25].
However, due to the high methodological heterogeneity mentioned above, it was difficult to compare the study results in general. A statistical meta-analysis was, therefore, considered as inappropriate and was not performed.
Results of subgroup analyses
The studies were classified into subgroups by gender, age, cardiovascular diseases/interventions or cardiac surgical procedures, time of the music intervention, selection of music, setting, region, study duration and type of music. For each of these subgroup analyses, only the findings of those 11 studies with higher quality were summarized [9, 11, 18, 23,24,25,26,27,28, 30, 35].
The detailed results of the subgroup analyses are presented in Table 3. Due to the small number of studies of comparatively higher quality in each subgroup, no relevant information could be derived to answer the questions regarding choice of music, time of music intervention, patient group and gender-specific differences.
Discussion
According to the CONSORT statement and the risk of bias assessment, the overall quality of the studies was perceived as medium to low. An analysis of the studies with higher quality, defined as publications that fulfilled more than 50% of the aspects in the CONSORT statement and were assessed with a high RoB in three or less categories, revealed that most of the publications could not demonstrate any statistically significant changes in the physiological and psychological parameters. Some studies, however, showed a decreasing trend in heart rate or blood pressure in the music group [18, 23, 27], or reported that the music was positively accepted by the patients in the intervention group [11, 25] indicating that there still might be an effect which was not significant due to low statistical power; however, the great methodological variety and the small number of included studies led to difficulties in comparing the study results in general. In order to verify the significant findings of individual experiments, such as the anxiolytic or blood pressure-reducing effects of music [18, 23, 35], further studies of high quality are needed.
Besides low statistical power, the study duration could be another important aspect that accounts for the predominantly insignificant results. Whether the length and number of music interventions have an impact on the cardiovascular system remained unanswered as only nine of the included 29 studies with more than one single music intervention or a music exposure longer than 1h were found [12, 13, 16, 19, 24, 31, 32, 34, 35]. It is possible that the effect of music arises only after a certain period of time. The long-term effect should thus be examined in more detail when exploring the influence of music on chronic cardiovascular diseases; however, a single application of music as a therapeutic agent may be sufficient when the focus is on the (acute) effect in the context of cardiovascular examinations and/or interventions.
Another aspect that needs to be discussed is the way music is applied. The patients listened to music via headphones [8,9,10,11,12,13, 15,16,17,18,19,20,21,22,23,24,25, 29, 31, 33,34,35,36], speakers [14, 28] or music pillows [26, 27, 30] in the included studies. The advantage of headphones is that the participants are not distracted by the noise from medical devices. On the other hand, the question arises whether prerecorded music has a different impact than live music. Thus, it would be interesting to measure the changes in cardiovascular parameters in patients who listen to music which is performed live using an instrument. The implementation of such a music intervention during cardiovascular procedures could pose a challenge, though. To our knowledge, this has not been investigated in previous studies.
Furthermore, it is crucial to consider the type of music. The music applied in the studies included Turkish [13, 35], Indian [24], classical [19, 22, 34, 36] and relaxing music [10, 18, 21, 26,27,28, 30, 32] as well as nature-based sounds [9, 23, 29]. A clear description of the musical structures was only found in ten studies [18, 21,22,23, 26,27,28, 31, 34, 36]. Different cultural backgrounds, early experiences and generational influences by which personal preferences for a certain type of music is shaped must be taken into consideration. Listening to one’s favorite music can trigger different changes in the human body in comparison to unfamiliar melodies that could implicate a lower patient adherence, reducing the possible therapeutic effects of music. For instance, in two of the included studies it was reported that patients withdrew from the intervention for dislike of the preselected music [17, 21]. On the other hand, Chang et al. found that a higher music preference was associated with lower posttest anxiety [18]. Preexisting moods and different personalities pose further challenges to the selection of the appropriate music. In addition, a general distinction must also be made between ergotropic and trophotropic types of music. It can be reasonably assumed that relaxing music has a calming effect during cardiac catheterization (directly or indirectly through anxiolytic processes) and therefore leads to reductions of blood pressure and/or heart rate. On the other hand, encouraging rhythms could facilitate faster mobilization e.g. after myocardial infarction [37]; however, since none of the studies to our knowledge has made such distinctions, no conclusions could be derived.
There are several studies that specifically investigated the effect of different styles of music on the cardiovascular system, mostly in healthy volunteers. Trappe and Voit conducted a randomized controlled trial with 120 healthy subjects who listened to music by Wolfgang Amadeus Mozart, Johann Strauss Jr. and ABBA [38]. Reductions of blood pressure and heart rate were reported when listening to Mozart or Strauss whereas the music by ABBA did not lead to any significant results. In the study by Bernardi et al. 24 healthy subjects were included and exposed to different styles of music [39]. A crescendo in music was associated with vasoconstriction and an increase in heart rate whilst uniform music induced vasodilatation and reductions of heart rate and blood pressure.
It can be concluded that the great variety of music with its complex elements which trigger different effects poses a great challenge to selecting the “right” music and that the fact that only ten studies provided a clear description of the music applied explains the difficulties in identifying homogeneous comparable trials. Therefore, an interdisciplinary cooperation between music therapists/musicologists and physicians is necessary. On 1 July 2009, the Austrian government officially recognized the music therapy profession by passing the Music Therapy Law [40], supporting the importance of incorporating musical specialists with their expertise into the studies.
Finally, it is important to underline that only studies which primarily investigated the cardiovascular system were included. Several literature reviews concluded that music might lead to a reduction of anxiety and pain [41,42,43,44,45,46]. Similar findings were reported in three of the included studies [9, 18, 23]. Therefore, it can be hypothesized that the focus of therapeutic effects of music is not on the cardiovascular system, but on psychological parameters; however, these effects might account for the subsequent changes in cardiovascular parameters.
Implications for further research
To minimize performance and detection bias, blinding is necessary. Headphones should be used for the experiments as they not only minimize the noise and distraction from outside, but also allow the blinding of the investigators and study participants during an intervention with the patient under general anesthesia or intubated patients in the intensive care unit who are not aware of the music played. This would therefore allow an objective analysis of the subconscious effects of music. Additionally, physiological changes are continuously measured in these settings and can be directly documented, thereby minimizing detection bias. In the case that double blinding is not possible, single blinded studies should still be preferred.
A further interesting field of investigation would be to examine patients with cardiac arrhythmia as nowadays arrhythmias can be easily detected by wearables, loop recorders or a 24‑h electrocardiogram [47]. Patients could be continuously monitored on an outpatient basis to investigate the influence of music on the occurrence of atrial fibrillation or other types of arrhythmia.
As the influence of music is modified by personal preferences, it would be interesting to perform studies on newborns who might not have yet developed personal tastes and thus could provide information that helps us to discern biological from cultural effects. Since it is presumed that music might only have an effect on cardiovascular diseases when applied with a certain regularity and length, future studies should also consider performing a series of music interventions with several follow-up sessions; however, as mentioned earlier, these questions regarding the choice of music as well as the length and number of music sessions should rather be discussed with music therapists/musicologists and documented in the study protocol. Moreover, the cooperation with music specialists helps defining and including a clear classification of the music style in the study protocol. This would result in more homogeneous studies and enable meta-analyses.
Finally, a careful and precise documentation of the patient’s medical history and the music interventions can minimize confounders, such as underlying diseases and medication administered; however, obtaining a statistically significant number of homogeneous patients for an interindividual comparison indeed poses a great challenge. Focusing on the analysis of intraindividual changes over several music interventions can be perceived as a further approach to investigating music and its efficacy as an adjuvant therapy in medicine.
Limitations
One limitation is that only publications in English or German were searched. Another limitation involves the issue that only studies with receptive music intervention were included. Music therapy that incorporates active participation of the patient by singing, dancing, clapping and musical improvisation has not been explored in the present review. It is conceivable, though, that active music therapy induces greater effects compared to the passive form since a close connection between music and movement has been described in the literature [48].
Moreover, the number of analyzed studies was relatively low, mostly explained by the strict inclusion criteria. In addition, the number of comparable findings was further reduced due to high methodological heterogeneity among the studies. Thus, generalizability of the trial results remains unclear.
Conclusion
This review included 29 studies with 2579 patients. An extensive full text and subgroup analysis as well as a precise quality assessment revealed that currently no definite effect of receptive music intervention on the cardiovascular system can be verified; however, it cannot be ruled out that music during medical interventions for instance can contribute to a relief of anxiety and tension by reducing the stress response of the autonomic nervous system. The world of music and its connection to medicine remains an interesting topic. Further research is needed to assess music as an inexpensive and easy applicable form of therapy.
References
Gasenzer ER, Neugebauer EAM. The relations between music and medicine in history and present. Dtsch Med Wochenschr. 2011;136:2644–51.
Juslin PN, Västfjäll D. Emotional responses to music: the need to consider underlying mechanisms. Behav Brain Sci. 2008;31:559–75.
Bradt J, Dileo C, Grocke D, Magill L. Music interventions for improving psychological and physical outcomes in cancer patients. Cochrane Database Syst Rev. 2011;8:CD6911.
Trappe H‑J. The effects of music on the cardiovascular system and cardiovascular health. Heart. 2010;96:1868–71.
Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c869.
Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. 2011. Available from: http://handbook-5-1.cochrane.org/.
The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre; 2014.
Abd-Elshafy SK, Khalaf GS, Abo-Kerisha MZ, Ahmed NT, Abd El-Aziz MA, Mohamed MA. Not all sounds have negative effects on children undergoing cardiac surgery. J Cardiothorac Vasc Anesth. 2015;29:1277–84.
Aghaie B, Rejeh N, Heravi-Karimooi M, Ebadi A, Moradian ST, Vaismoradi M, et al. Effect of nature-based sound therapy on agitation and anxiety in coronary artery bypass graft patients during the weaning of mechanical ventilation: a randomised clinical trial. Int J Nurs Stud. 2014;51:526–38.
Argstatter H, Haberbosch W, Bolay HV. Study of the effectiveness of musical stimulation during intracardiac catheterization. Clin Res Cardiol. 2006;95:514–22.
Bally K, Campbell D, Chesnick K, Tranmer JE. Effects of patient-controlled music therapy during coronary angiography on procedural pain and anxiety distress syndrome. Crit Care Nurse. 2003;23:50–8.
Barnason S, Zimmerman L, Nieveen J. The effects of music interventions on anxiety in the patient after coronary artery bypass grafting. Heart Lung. 1995;24:124–32.
Bekiroğlu T, Ovayolu N, Ergün Y, Ekerbiçer HÇ. Effect of Turkish classical music on blood pressure: a randomized controlled trial in hypertensive elderly patients. Complement Ther Med. 2013;21:147–54.
Buffum MD, Sasso C, Sands LP, Lanier E, Yellen M, Hayes A. A music intervention to reduce anxiety before vascular angiography procedures. J Vasc Nurs. 2006;24:68–73. quiz 74.
Cadigan ME, Caruso NA, Haldeman SM, McNamara ME, Noyes DA, Spadafora MA, et al. The effects of music on cardiac patients on bed rest. Prog Cardiovasc Nurs. 2001;16:5–13.
Cao S, Sun J, Wang Y, Zhao Y, Sheng Y, Xu A. Music therapy improves pregnancy-induced hypertension treatment efficacy. Int J Clin Exp Med. 2016;9(5):8833–8.
Chan MF. Effects of music on patients undergoing a C-clamp procedure after percutaneous coronary interventions: a randomized controlled trial. Heart Lung. 2007;36:431–9.
Chang H‑K, Peng T‑C, Wang J‑H, Lai H‑L. Psychophysiological responses to sedative music in patients awaiting cardiac catheterization examination: a randomized controlled trial. J Cardiovasc Nurs. 2011;26:E11–E8.
Elliott D. The effects of music and muscle relaxation on patient anxiety in a coronary care unit. Heart Lung. 1994;23:27–35.
Forooghy M, Mottahedian Tabrizi E, Hajizadeh E, Pishgoo B. Effect of music therapy on patients’ anxiety and hemodynamic parameters during coronary angioplasty: a randomized controlled trial. Nurs Midwifery Stud. 2015;4:e25800.
Hamel WJ. The effects of music intervention on anxiety in the patient waiting for cardiac catheterization. Intensive Crit Care Nurs. 2001;17:279–85.
Hatem TP, Lira PIC, Mattos SS. The therapeutic effects of music in children following cardiac surgery. J Pediatr (Rio J). 2006;82:186–92.
Heidari S, Babaii A, Abbasinia M, Shamali M, Abbasi M, Rezaei M. The effect of music on anxiety and cardiovascular indices in patients undergoing coronary artery bypass graft: a randomized controlled trial. Nurs Midwifery Stud. 2015;4:e31157.
Kunikullaya KU, Goturu J, Muradi V, Hukkeri PA, Kunnavil R, Doreswamy V, et al. Music versus lifestyle on the autonomic nervous system of prehypertensives and hypertensives—a randomized control trial. Complement Ther Med. 2015;23:733–40.
Ng MY, Karimzad Y, Menezes RJ, Wintersperger BJ, Li Q, Forero J, et al. Randomized controlled trial of relaxation music to reduce heart rate in patients undergoing cardiac CT. Eur Radiol. 2016;26:3635–42.
Nilsson U. The effect of music intervention in stress response to cardiac surgery in a randomized clinical trial. Heart Lung. 2009;38:201–7.
Nilsson U. Soothing music can increase oxytocin levels during bed rest after open-heart surgery: a randomised control trial. J Clin Nurs. 2009;18:2153–61.
Nilsson U, Lindell L, Eriksson A, Kellerth T. The effect of music intervention in relation to gender during coronary angiographic procedures: a randomized clinical trial. Eur J Cardiovasc Nurs. 2009;8:200–6.
Rejeh N, Heravi-Karimooi M, Tadrisi SD, Jahani A, Vaismoradi M, Jordan S. The impact of listening to pleasant natural sounds on anxiety and physiologic parameters in patients undergoing coronary angiography: a pragmatic quasi-randomized-controlled trial. Complement Ther Clin Pract. 2016;25:42–51.
Ripley L, Christopoulos G, Michael TT, Alomar M, Rangan BV, Roesle M, et al. Randomized controlled trial on the impact of music therapy during cardiac catheterization on reactive hyperemia index and patient satisfaction: the functional change in endothelium after cardiac catheterization, with and without music therapy (FEAT) study. J Invasive Cardiol. 2014;26:437–42.
Sendelbach SE, Halm MA, Doran KA, Miller EH, Gaillard P. Effects of music therapy on physiological and psychological outcomes for patients undergoing cardiac surgery. J Cardiovasc Nurs. 2006;21:194–200.
Sundar S, Ramesh B, R A. Effect of relaxing music on blood pressure and heart rate in hospitalized pre-hypertensive women in 3rd trimester of pregnancy: a randomized control study. Asian J Pharm Clin Res. 2015;8:186–8.
Taylor-Piliae RE, Chair S‑Y. The effect of nursing interventions utilizing music therapy or sensory information on Chinese patients’ anxiety prior to cardiac catheterization: a pilot study. Eur J Cardiovasc Nurs. 2002;1:203–11.
Teng XF, Wong MYM, Zhang YT. The effect of music on hypertensive patients. Annu Int Conf IEEE Eng Med Biol Soc. 2007;2007:4649–51.
Toker E, Komurcu N. Effect of Turkish classical music on prenatal anxiety and satisfaction: a randomized controlled trial in pregnant women with pre-eclampsia. Complement Ther Med. 2017;30:1–9.
White JM. Music therapy: an intervention to reduce anxiety in the myocardial infarction patient. Clin Nurse Spec. 1992;6:58–63.
Decker-Voigt H‑H. Mit Musik ins Leben. Wie Klänge wirken: Schwangerschaft und frühe Kindheit. Kreuzlingen, München: Ariston-Verlag; 1999.
Trappe H‑J, Voit G. The cardiovascular effect of musical genres. Dtsch Arztebl Int. 2016;113:347–52.
Bernardi L, Porta C, Casucci G, Balsamo R, Bernardi NF, Fogari R, et al. Dynamic interactions between musical, cardiovascular, and cerebral rhythms in humans. Circulation. 2009;119:3171–80.
RIS. Musiktherapiegesetz – Bundesrecht konsolidiert. 2020. https://www.ris.bka.gv.at/GeltendeFassung.wxe?Abfrage=Bundesnormen&Gesetzesnummer=20005868#header. Accessed 24 Sept 2020.
Bradt J, Dileo C, Magill L, Teague A. Music interventions for improving psychological and physical outcomes in cancer patients. Cochrane Database Syst Rev. 2016;8:CD6911.
Aalbers S, Fusar-Poli L, Freeman RE, Spreen M, Ket JC, Vink AC, et al. Music therapy for depression. Cochrane Database Syst Rev. 2017;11:CD4517.
Kühlmann AYR, de Rooij A, Kroese LF, van Dijk M, Hunink MGM, Jeekel J. Meta-analysis evaluating music interventions for anxiety and pain in surgery. Br J Surg. 2018;105:773–83.
Baylan S, Swann-Price R, Peryer G, Quinn T. The effects of music listening interventions on cognition and mood post-stroke: a systematic review. Expert Rev Neurother. 2016;16:1241–9.
Zhang Y, Cai J, An L, Hui F, Ren T, Ma H, et al. Does music therapy enhance behavioral and cognitive function in elderly dementia patients? A systematic review and meta-analysis. Ageing Res Rev. 2017;35:1–11.
Jayakar JP, Alter DA. Music for anxiety reduction in patients undergoing cardiac catheterization: a systematic review and meta-analysis of randomized controlled trials. Complement Ther Clin Pract. 2017;28:122–30.
Sana F, Isselbacher EM, Singh JP, Heist EK, Pathik B, Armoundas AA. Wearable devices for ambulatory cardiac monitoring: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75:1582–92.
Amrhein F. Musik und Bewegung. In: Hartogh T, Wickel HH, editors. Handbuch Musik in der Sozialen Arbeit. Weinheim: Beltz Juventa; 2004. pp. 231–44.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
C.-Y. Ho, P. Wexberg, B. Schneider, and C. Stöllberger declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ho, CY., Wexberg, P., Schneider, B. et al. Effect of music on patients with cardiovascular diseases and during cardiovascular interventions. Wien Klin Wochenschr 133, 790–801 (2021). https://doi.org/10.1007/s00508-020-01782-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-020-01782-y