Summary
Background
Nosocomial pneumonia (NP) and ventilator associated pneumonia (VAP) have been associated with financially significant economic burden and increased case fatality rate in adult intensive care units (ICUs). This study was designed to evaluate case fatality rate among patients with NP and VAP in a respiratory ICU.
Methods
In 2008–2013, VAP and NP in the ICUs were included in this retrospective single-centre cohort study. Data on demographics, co-morbidities, severity of illness, mechanical ventilation, empirical treatment, length of hospital stay and laboratory findings were recorded in each group, as were case fatality rate during ICU admission and after discharge including short-term (28-day) and long-term (a year) case fatality rate.
Results
A total of 108 patients with VAP (n = 64, median (IQR) age: 70 (61–75) years, 67.2 % were men) or NP (n = 44, median (IQR) age: 68 (62–74) years, 68.2 % were men) were found. Appropriate empirical antibiotic therapy was identified only in 45.2 and 42.9 % of patients with VAP and NP, respectively. Overall case fatality rate in VAP and NP (81.3 vs 84.1), ICU case fatality rate (42.2 vs 45.5 %), short-term case fatality rate (15.6 vs 27.3 %) and long-term case fatality rate (23.4 vs 11.4 %) were similar between VAP and NP groups along with occurrence 50 % of case fatality rate cases in the first 2 months and 90 % within the first year of discharge. Multivariate analysis showed that chronic obstructive pulmonary disease (COPD) (HR: 3.15, 95 % CI: 1.06–9.38; p = 0.039) and presence of septic shock (HR: 3.83, 95 % CI: 1.26–11.60; p = 0.018) were independently associated with lower survival.
Conclusion
In conclusion, our findings in a retrospective cohort of respiratory ICU patients with VAP or NP revealed high ICU, short- and long-term case fatality rates within 1 year of diagnosis, regardless of the diagnosis of NP after 48 h of initial admission or after induction of ventilator support. COPD and presence of septic shock are associated with high fatality rate and our findings speculate that as increasing compliance with infection control programs and close monitoring especially in 2 months of discharge might reduce high-case fatality rate in patients with VAP and NP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nosocomial pneumonia (NP), defined as the pneumonia that occurs more than 48 h after a patient’s admission to hospital [1], is the second most common infection acquired among hospitalized patients [2–4] and the primary cause of death in intensive care units (ICUs) [3, 4]. Ventilator-associated pneumonia (VAP) is a subset of NP occurring 48 h or more after endotracheal intubation [1, 5], while NPs including ventilator-associated subtype have been considered to be a major public health problem associated with financially significant economic burden, increased length of hospital stays along with increased case fatality rate that ranges from 33 to 72 % [5–10].
Besides adverse impact on patients’ safety and quality of healthcare systems [10], NPs have also been associated with potential risk of fatality due to emergence of resistant pathogens and scarcity of available novel antimicrobial agents [11]. Accordingly, NP has become a priority in patient safety policies at the national and international levels and determination of the VAP-associated epidemiology in each medical institution has been considered important for developing effective prophylactic and therapeutic strategies for prevention and control of NP and VAP [12–18].
In studies, attributable case fatality rates have included only patients with ventilator-associated pneumonia. So, these data may not be directly comparable with studies evaluating the attributable case fatality rate of NP overall because these differences may be explained by differences in diagnostic criteria for pneumonia and study design using different matching criteria [19]. Our single-centre retrospective study was designed to evaluate long- and short-term case fatality rate among patients with NP and VAP in a respiratory ICU.
Methodology
This study was done in a tertiary teaching hospital for Chest and Thoracic Surgery Hospital of 22 beds Level III medical non-surgical, nonobstetrical adult intensive care unit between January 2008 and July 2013. This study was designed a single-centre cohort study and was approved by the local ethical committee of the government teaching hospital (Sureyyapasa Chest Diseases and Thoracic Surgery Teaching Hospital-Istanbul-Turkey, 05/02/2014–2015) and it was conducted in accordance with the ethical principles stated in the Declaration of Helsinki. Inform consent was not obtained from all patients due to retrospective study design.
Study population
Patients who were diagnosed as the definition of NP or VAP as below were included in to the study. Patients group were named as NP and VAP.
Study parameters
Data on patient demographics, co-morbidities, The Acute Physiologic Score and Chronic Health Evaluation (APACHE II) scores at ICU admission, application of non-invasive and invasive mechanical ventilation, diagnosis day of NP/VAP, culture findings, appropriateness of empirical treatment (appropriate, not appropriate, partially appropriate), length of ICU and hospital stay and laboratory findings (leucocyte count, platelet count, C-reactive protein (CRP) and albumin levels) were recorded in each group, as case fatality rate during ICU admission and after discharge including short-term (28-day) and long-term (a year) periods.
VAP and NP definitions
VAP was defined as a new chest infiltration after 2 days of invasive mechanical ventilation (patients ventilated mechanically via endotracheal tube by ICU ventilators) accompanied with leucocytosis (white blood cell count (WBC) > 10 × 109/l) or leucopenia (WBC < 4 × 109/l) and fever (> 38 or < 36 °C). Patients with new chest infiltration after 2 days of hospital admission who did not meet VAP criteria were classified into the NP group [1, 5, 20].
Microbiological assessments
Endotracheal aspirate or sputum cultures with two sets of blood cultures were performed for each of patient for isolation of the causative microorganisms after the 2 days of admission of ICU either intubated or not. In hypoxemic patients, closed suctioning system attached between the ETT and ventilatory tubing, allowing introduction of the suctioning catheter into the airways without disconnecting the patient from the ventilator was used for aspiration procedure [21]. The thresholds for quantitative cultures were 104 colony-forming units/mL for endotracheal aspirate and 104 colony-forming units/mL for bronchoalveolar lavage and non–bronchoscopic lavage. All microorganisms isolated were identified by standard laboratory methods.
Statistical analysis
All statistical analyses were performed using SPSS 20.0 portable. A descriptive analysis was used to investigate patient demographics and ICU data. Groups were compared with Mann–Whitney U-tests for non-parametric continuous variables or Student’s t-tests for parametric continuous variables. Chi-square tests and Fisher’s exact tests (if n ≤ 5) were employed for dichotomous variables. The median with interquartile range (IQR) was employed for non-parametric continuous variables, and mean ± standard deviation (SD) was used for parametric continuous variables. Count and percentage were used when applicable. Kaplan–Meier test was performed to assess the time to event. Multivariate regression analysis was used to access independent prognostic factors which are associated with case fatality, p-value < 0.05 was accepted as statistically significant.
Results
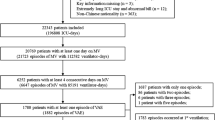
A total of 108 patients with VAP (n = 64, median (IQR) age: 70 (61–75) years, 67.2 % were men) and NP (n = 44, median (IQR) age: 68 (62–74) years, 68.2 % were men) were found.
Patient demographics and comorbidities in study groups
As shown in Table 1, VAP and NP groups were homogenous in terms of patient demographics and co-morbidities.
ICU data in study groups
VAP and NP groups were similar in terms of mean (SD) APACHE II scores (24.0 (7.0) vs 21.0 (7.0)), median duration of invasive mechanical ventilation (15 vs 7 days), rate of non-invasive mechanical ventilation (66.7 vs 66.8 %) as well as laboratory findings including leucocyte count, CRP levels at admission and albumin levels. Median (IQR) duration of non-invasive mechanical ventilation (5 (2–9) vs 12 (8–18) days, p = 0.001) and platelet count (235,000 (107,000) vs 285,000 (132,000) × 106/L, p = 0.034) were significantly lower, while the rate of invasive mechanical ventilation (100 vs 65.9 %, p = 0.001) and mean (SD) body temperature (37.6 (0.8) vs 37.3 (0.8) °C, p = 0.036) were significantly higher in VAP than in NP patients (Table 2).
Pneumonia and hospitalisation-related characteristics in study groups
VAP and NP groups were similar in terms of mean (SD) pneumonia severity index (101 (30.0) vs 196 (37.0)) and the rate of culture positivity (95.2 % for each), while Acinobacter baumannii was the most commonly identified pathogen in 63.3 and 35 % of VAP and NP patients, respectively and significantly higher in VAP than NP (p = 0.005) (Table 3).
Percentage of patients with appropriate empirical treatment (45.2 vs 42.9 %), antibiotic use in the last 3 months (54.7 vs 68.2 %) and the rate of late onset disease (62.5 vs 61.4 %) were also similar between VAP and NP groups, while the rate of multiple organ failure was significantly higher in VAP than in NP group (67.2 vs 51.2 %, p = 0.01). No significant difference was noted between VAP and NP groups in terms of median (IQR) length of ICU stay (20 (14–31) vs 14 (10–24) days) as well as length of hospital stay after the diagnosis (14 (6–23) vs 10 (5–21) days) (Table 3).
Short- and long-term case fatality rates in study groups
Overall case fatality rate was similar between groups with death of 52 of 64 (81.3 %) patients with VAP and 37 of 44 (84.1 %) patients with NP at the end of the study period. Case fatality rate during ICU admission (42.2 vs 45.5 %), short-term case fatality rate within 28 days of discharge (15.6 vs 27.3 %), long-term case fatality rate within a year of discharge (23.4 vs 11.4 %), time to death during ICU stay (6 vs 5 days) as well as survival after discharge (3.8 (4.8) vs 4.8 (7.7) months) were similar between VAP and NP groups.
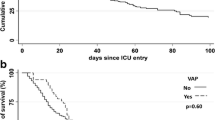
Kaplan–Meier survival analysis revealed that two groups were similar in terms of long-term survival (p > 0.67) with occurrence 50 % of case fatality rate cases in the first 2 months and 90 % within the first year of discharge (Fig. 1).
We analysed variables that included the co-morbid diseases, age, gender, type of mechanical ventilation, APACHE II on the admission to the ICU, C-reactive protein, prognostic index of surgical infections, multiple organ failure and presence of septic shock to access independent prognostic factors which are associated with case fatality. In the multivariate analysis, chronic obstructive pulmonary disease (COPD) (HR: 3.15, 95 % CI: 1.06–9.38; p = 0.039) and presence of septic shock (HR: 3.83, 95 % CI: 1.26–11.60; p = 0.018) were independent prognostic factors for case fatality rate (Table 4).
Discussion
Our findings from a retrospective cohort of ICU patients with VAP and NP revealed high overall rates of case fatality rate including case fatality rate during ICU stay and within 28 days or later following discharge, with no significant difference between VAP and NP groups. Apart from significantly higher rate for multiple organ failure, tendency for length of ICU stay as well as higher rate for invasive mechanical ventilation in VAP than in NP patients and significantly higher duration of non-invasive mechanical ventilation in NP than in VAP patients, VAP and NP groups were similar not only in case fatality rate but also in terms or demographic characteristics, co-morbid disorders, laboratory findings and the rates for late-onset pneumonia, appropriate empirical treatment and culture positivity.
In our cohort, ICU case fatality rate in VAP and NP patients seems comparable to ICU case fatality rates of 48.3 % [16] and 47.3 % [22] associated with VAP and crude ICU case fatality rate in patients with NP (41 %) [23] reported in the past studies. Short-term case fatality rates were also consistent with the 28-day case fatality rate in appropriately treated VAP patients that varies from 18 to 29 % in literature [24, 25].
Given the range of crude (24–76 %) and attributable (20–30 %) case fatality rates reported in developed countries [17, 26–28], our findings seems notable by providing data on overall case fatality rates within 1 year of diagnosis as well as on timing of case fatality rate indicating that most of case fatality rate cases to occur during ICU stay or within 2 months of hospital discharge.
In agreement with indication of certain co-morbidities to significantly affect prognosis in NP/VAP patients and thereby lead high case fatality rates [27], case fatality rate due to terminal illness composed one-third of case fatality rates occurred during ICU admission in our study groups.
Data from a first prospective study of targeted surveillance of healthcare-associated infections in 13 ICUs from 12 Turkish hospitals revealed that during the 3-year study, VAP comprised 47.4 % of all device-associated infections and associated with the highest risk, while Acinetobacter spp. (26.7 %), Pseudomonas spp. (24.2 %) and Staphylococcus aureus (14.9 %) were the most commonly identified causative agents [29]. Accordingly, identification of A. baumannii, P. aeruginosa and S. aureus as the most frequent causative pathogens in our cohort consistent with the statement that P. aeruginosa, Acinetobacter spp., and S. aureus were among the most frequent multidrug resistant (MDR) pathogens found in VAP [17, 30–32] and notable given that their frequencies were also reported to be significantly associated with increased case fatality rate with rates of up to 70 % [17, 33]. In present study A. baumannii was the major causative agent in VAP and NP, however, VAP group had two times higher rate of that agent than NP.
Indeed, increasing detection of MDR in association with VAP in the hospital setting has been considered to be a threat for the treatment of the patients [34] being attributed to the widespread use of antimicrobials, prolonged use of invasive mechanical ventilation in the ICU, prolonged stay in the hospital and prior antibiotic therapy due to presence of late-onset disease and co-morbidities [12, 30, 34–36].
In this regard, given the high case fatality rates despite isolation of aetiological agent in 95 % of cultures, our findings emphasise the contribution of certain factors such as emergence of MDR pathogens, co-morbidities, severity of illness, appropriate antibiotic therapy, prior antibiotic therapy, duration of mechanical ventilation and length of ICU stay, in the prognosis of VAP patients [11, 27, 30, 37–40].
Timely administration of appropriate antibiotic therapy has been considered essential element in successful management of NP and shown to significantly influence outcome, yielding survival rates of 70–80 % [41, 42]. In this regard it is worth noting that in our cohort administration of appropriate empirical antibiotic therapy was identified only in 45.2 and 42.9 % of patients with VAP and NP, respectively.
Underlying disease of the patient has also been related with death as much as the infection sites and antibiotic susceptibility of pathogen [43]. Therefore, it should be noted that the majority of patients in our cohort had co-morbidities, a factor which is known to influence long-term outcomes [44, 45].
Besides, administration of broad spectrum antibiotics in the preceding 7 days was reported to be associated with increased rate of VAP especially forms caused by P. aeruginosa and Acinetobacter spp. [16, 46, 47]. In this regard, use of antibiotic therapy within the last 3 months in our cohort seems to be in line with the identification of A. baumannii and P. aeruginosa in most of the cultures and emphasize the crucial importance of determination of antibiotic sensitivity patterns and administration of appropriate empirical antibiotic therapy in such cases [30, 48].
NP has been suggested to independently increase case fatality rate risk in patients with moderately severe (APACHE scores of 20–29) illness, while case fatality rate in more severely (APACHE scores > 30) or less severely (APACHE scores < 20) ill patients have been considered to occur secondary to the underlying disease, regardless of the presence of NP [10, 49]. Our cohort indicating moderate severity of the illness at admission according to APACHE II score, and NP/VAP seems to have substantial influence on death as the outcome which seems consistent with identification of pneumonia as the primary cause of death in two-thirds of ICU mortalities in our study.
Higher rate of invasive mechanical ventilation in patients with VAP than NP in the present cohort is in agreement with the fact that mechanical ventilation increases the risk of pneumonia by 6–20 times and associated with case fatality rates of up to 50 % [50, 51], while non-invasive methods of ventilation were associated with reduced rates of VAP in patients with acute respiratory failure [5]. Likewise, data from a past study in Turkey revealed that overall higher incidence of nosocomial infection in medical/surgical than in neurological ICUs was associated with greater use of invasive devices in medical/surgical ICUs [52].
Up to 1–3 % increase in the risk of VAP has been indicated for each day requirement for mechanical ventilation in intubated patients [39, 53], along with the contribution of longer ICU stay and thereby increased risk of ICU-related complications such as other nosocomial infections and complications related to invasive procedures to the attributable case fatality rate [49]. In this regard, our findings emphasise the likely benefit of strategies of reducing need for ventilation, reducing colonisation and reducing aspiration in prevention of VAP [5] and support the statement that implementation of rational protocols for the rational of use of empirical antibacterial agents and having knowledge on MDR organisms may help in decreasing VAP-related case fatality rates by MDR bacteria in the ICU and in reducing length of hospital stay and healthcare costs [6, 17, 34, 41].
Presence of diagnosis of COPD and septic shock are associated with high fatality rate in our study after multivariate analysis. In a prospective study conducted in mix ICU, COPD diagnosis and presence of shock found also to be related with high fatality rate in patients with VAP [54]. Presence of COPD was also found as fatality risk factor for NP in previous studies [55].
Certain limitations to this study should be considered. First, due to retrospective single-centre design of the present study, establishing the temporality between cause and effect as well as generalising our findings to overall VAP/NP population seems difficult. Second, due to lack of a selection protocol, each physician might have used a different choice of antibiotic for treatment of a specific organism. Nevertheless, despite these certain limitations, given the paucity of the solid information available on this area despite the importance of regional and local surveillance data, our findings could represent a valuable contribution to the literature.
Conclusion
In conclusion, our findings in a retrospective cohort of respiratory ICU patients with VAP or NP revealed high ICU, short- and long-term case fatality rates within 1 year of diagnosis, regardless of the diagnosis of NP after 48 h of initial admission or after induction of ventilator support. Additionally, use of mechanical ventilation, predominance of MDR causative pathogens, insufficient use of appropriate antibiotic therapy, late-onset disease and thus use of previous antimicrobial therapy along with moderate severity of illness and co-morbidities in substantial percentage of patients in our cohort seem to contribute to the outcome. Our findings indicate the importance of not only ICU admission but also first 2 months after hospital discharge in terms of case fatality rate associated with VAP and NP in respiratory ICU and speculate that increasing compliance with infection control programmes and close monitoring especially in 2 months of discharge might reduce the high case fatality rates in patients with VAP and NP.
Author contributions
M. Yalçınsoy, Z. Karakurt, C. Salturk, G. Gungor, M. Balcı designed research and performed interpretation of data, drafting the article and revising it; O. Y. Mocin, E. Aksoy, N. Adıguzel performed drafting the article; F. Kargın, H. B. Takır, A. Oguz, performed analysis and interpretation of data; S. B. Kutlu, Z. Karakurt provided intellectual content of critical importance to the work, M. Yalçınsoy, Z. Karakurt had primary responsibility for final content. All authors read and approved the final manuscript
Conflict of interest
The authors declare that there are no actual or potential conflicts of interest in relation to this article.
References
Torres A, Ferrer M, Badia JR. Treatment guidelines and outcomes of hospital-acquired and ventilator-associated pneumonia. Clin Infect Dis. 2010;51:48–53.
Cook DJ, Walter SD, Cook RJ, Griffith LE, Guyatt GH, Leasa D, et al. Incidence of and risk factors for ventilator-associated pneumonia in critically ill patients. Ann Intern Med. 1998;129:433–40.
Efrati S, Deutsch I, Antonelli M, Hockey PM, Rozenblum R, Gurman GM. Ventilator-associated pneumonia: current status and future recommendations. J Clin Monit Comput. 2010;24:161–8.
Melsen WG, Rovers MM, Bonten MJ. Ventilator-associated pneumonia and mortality: a systematic review of observational studies. Crit Care Med. 2009;37:2709–18.
Majumdar SS, Padiglione AA. Nosocomial infections in the intensive care unit. Anaesth Intens Care Med. 2012;13:204–8 (Review).
Japoni A, Vazin A, Davarpanah MA, Afkhami Ardakani M, Alborzi A, Japoni S, Rafaatpour N. Ventilator-associated pneumonia in Iranian intensive care units. J Infect Dev Ctries. 2011;5:286–93.
Fagon JY, Chastre J, Vuagnat A, Trouillet JL, Novara A, Gibert C. Nosocomial pneumonia and mortality among patients in intensive care units. JAMA. 1996;275:866–9.
Heyland DK, Cook DJ, Griffith L, Keenan SP, Brun-Buisson C. The attributable morbidity and mortalityof ventilator-associated pneumonia in the critically ill patient. The Canadian Critical Trials Group. Am J Respir Crit Care Med. 1999;159:1249–56.
Umscheid CA, Mitchell M, Doshi J, Agarwal R, Williams K, Brennan P. Estimating the proportion of healthcare-associated infections that are reasonably preventable and the related mortality and costs. Infect Control Hosp Epidemiol. 2011;32:101–14.
Guzmán-Herrador B, Díaz Molina C, Allam MF, Fernández-Crehuet Navajas R. Underlying illness severity and outcome of nosocomial pneumonia: prospective cohort study in intensive care unit. J Hosp Infect. 2014;86:53–6.
Behnia M, Logan SC, Fallen L, Catalano P. Nosocomial and ventilator-associated pneumonia in a community hospital intensive care unit: a retrospective review and analysis. BMC Res Notes. 2014;7:232.
American Thoracic Society Documents. Guidelines for the management of adults with hospital-acquired ventilator-associated pneumonia. Am J Respir Crit Care Med. 2005;171:388–416.
Tablan OC, Anderson LJ, Besser R, Bridges C, Hajjeh R. Guidelines for preventing health-care-associated pneumonia, 2003: recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee. MMWR Recomm Rep. 2004;53:1–36.
Díaz E1, Martín-Loeches I, Vallés J. Nosocomial pneumonia. Enferm Infecc Microbiol Clin. 2013;31:692–8.
Rello J, Sa-Borges M, Correa H, Leal SR, Baraibar J. Variations in etiology of ventilator-associated pneumonia across four treatment sites: implications for antimicrobial prescribing practices. Am J Respir Crit Care Med. 1999;160:608–13.
Ranjan N, Chaudhary U, Chaudhry D, Ranjan KP. Ventilator-associated pneumonia in a tertiary care intensive care unit: analysis of incidence, risk factors and mortality. Indian J Crit Care Med. 2014;18:200–4.
Resende MM, Monteiro SG, Callegari B, Figueiredo PM, Monteiro CR, Monteiro-Neto V. Epidemiology and outcomes of ventilator-associated pneumonia in northern Brazil: an analytical descriptive prospective cohort study. BMC Infect Dis. 2013;13:119.
Charles MP, Kali A, Easow JM, Joseph NM, Ravishankar M, Srinivasan S, et al. Ventilator-associated pneumonia. Australas Med J. 2014;31(8):334–44.
Rosenthal VD, Guzman S, Migone O, Safdar N. The attributable cost and length of hospital stay because of nosocomial pneumonia in intensive care units in 3 hospitals in Argentina: a prospective, matched analysis. Am J Infect Control. 2005;33:157–61.
Mietto C, Pinciroli R, Patel N, Berra L. Ventilator associated pneumonia: evolving definitions and preventive strategies. Respir Care. 2013;58(6):990–1007.
Rabitsch W, Köstler WJ, Fiebiger W, Dielacher C, Losert H, Sherif C, Staudinger T, Seper E, Koller W, Daxböck F, Schuster E, Knöbl P, Burgmann H, Frass M. Closed suctioning system reduces cross-contamination between bronchial system and gastric juices. Anesth Analg. 2004;99:886–92.
Mukhopadhyay C, Bhargava A, Ayyagari A. Role of mechanical ventilation and development of multidrug resistant organisms in hospital acquired pneumonia. Indian J Med Res. 2003;118:229–35.
Bercault N, Boulain T. Mortality rate attributable to ventilator-associated nosocomial pneumonia in an adult intensive care unit: a prospective case-control study. Crit Care Med. 2001;29:2303–9.
Combes A, Luyt CE, Fagon JY, Wolff M, Trouillet JL, Chastre J. Early predictors for infection recurrence and death in patients with ventilator-associated pneumonia. Crit Care Med. 2007;35:146–54.
Luna CM, Aruj P, Niederman J, Garzón J, Violi D, Prignoni A, Ríos F, Baquero S, Gando S; the Grupo Argentino de Estudio de la Neumonia Asociada al Respirador (GANAR) group. Appropriateness and delay to initiate therapy in ventilator associated pneumonia. Eur Res J. 2006;27:158–64.
Arabi Y, Al-Shirawi N, Memish Z, Anzueto A. Ventilator-associated pneumonia in adults in developing countries: a systematic review. Int J Infect Dis. 2008;12:505–12.
Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002;165:867–903.
Rodrigues PM, Carmo Neto E, Santos LR, Knibel MF. Ventilator-associated pneumonia: epidemiology and impact on the clinical evolution of ICU patients. J Bras Pneumol. 2009;35:1084–91.
Leblebicioglu H, Rosenthal VD, Arikan OA, Ozgültekin A, Yalcin AN, Koksal I, Usluer G, Sardan YC, Ulusoy S; Turkish Branch of INICC. Device-associated hospital-acquired infection rates in Turkish intensive care units. Findings of the International Nosocomial Infection Control Consortium (INICC). J Hosp Infect. 2007;65:251–7.
Depuydt PO, Vandijck DM, BekaertMA, Decruyenaere JM, Blot SI, Vogelaers DP, Benoit DD. Determinants and impact of multidrug antibiotic resistance in pathogens causing ventilator-associated-pneumonia. Crit Care. 2008;12:R142.
Giantsou E, Liratzopoulos N, Efraimidou E, Panopoulou M, Alepopoulou E, Kartali-Ktenidou S, Minopoulos GI, Zakynthinos S, Manolas KI. Both early-onset and late-onset ventilator-associated pneumonia are caused mainly by potentially multiresistant bacteria. Intensive Care Med. 2005;31:1488–94.
Guimaraes MM, Rocco JR. Prevalence of ventilator-associated pneumonia in a university hospital and prognosis for the patients affected. J Bras Pneumol. 2006;32:339–46.
Fagon JY, Chastre J, Hance AJ, Montravers P, Novara A, Gibert C. Nosocomial pneumonia in ventilated patients: a cohort study evaluating attributable mortality and hospital stay. Am J Med. 1993;94:281–8.
Charles MP, Easow JM, Joseph NM, Ravishankar M, Kumar S, Sivaraman U. Aetiological agents of ventilator-associated pneumonia and its resistance pattern—a threat for treatment. Australas Med J. 2013;6:430–4.
Chien JY, Hsueh PR, Yu CJ, Yang PC. The evolution of drug-resistant microorganisms in patients with prolonged mechanical ventilation. Am J Infect Control. 2009;37:231–6.
Trouillet JL, Chastre J, Vuagnat A, Joly-Guillou ML, Combaux D, Dombret MC, Gibert C. Ventilator-associated pneumonia caused by potentially drug-resistant bacteria. Am J Respir Crit Care Med. 1998;157:531–9.
Hartzell JD, Kim AS, Kortepeter MG, Moran KA. Acinetobacter pneumonia: a review. MedGenMed. 2007;9:4.
Teixeira PJZ, Seligman R, Hertz FT. Inadequate treatment of ventilator-associated pneumonia; risk factors and impact on outcomes. J Hosp Infect. 2007;65:361–367.
Lahoorpour F, Delpisheh A, Afkhamzadeh A. Risk factors for acquisition of ventilator-associated pneumonia in adult intensive care units. Pak J Med Sci. 2013;29:1105–7.
Gursel G, Aydogdu M, Ozyilmaz E, Ozis TN. Risk factors for treatment failure in patients with ventilator-associated pneumonia receiving appropriate antibiotic therapy. J Crit Care. 2008;23:34–40.
Harmanci A, Harmanci O, Akova M. Hospital-acquired pneumonia: challenges and options for diagnosis and treatment. J Hosp Infect. 2002;51:160–7. Review.
Iregui M, Ward S, Sherman G, Fraser VJ, Kollef MH. Clinical importance of delays in the initiation of appropriate antibiotic treatment for ventilator-associated pneumonia. Chest. 2002;122:262–8.
Ozdemir H, Kendirli T, Ergun H, Ciftci E, Tapisiz A, Guriz H, et al. Nosocomial infections due to Acinetobacter baumannii in a pediatric intensive care unit in Turkey. Turk J Pediatr. 2011;53:255–60.
Erdem H, Inan A, Altındis S, Carevic B, Askarian M, Cottle L, et al. Surveillance, control and management of infections in intensive care units in Southern Europe, Turkey and Iran—a prospective multicenter point prevalence study. J Infect. 2014;68:31–140.
Rubenfeld GD. Interventions to improve long-term outcomes after critical illness. Curr Opin Crit Care. 2007;13:476–81.
Nakaviroj S, Cherdrungsi R, Chaiwat O. Incidence and risk factors for ventilator-associated pneumonia in the surgical intensive care unit, Siriraj Hospital. J Med Assoc Thai. 2014;97:61–8.
Fagon JY, Chastre J, Domart Y, Trouillet JL, Pierre J, Darne C, Gibert C. Nosocomial pneumonia in patients receiving continuous mechanical ventilation. Prospective analysis of 52 episodes with use of a protected specimen brush and quantitative culture techniques. Am Rev Respir Dis. 1989;139:877–84.
Japoni A, Vazin A, Hamedi M, Davarpanah MA, Alborzi A, Rafaatpour N. Multidrug-resistant bacteria isolated from intensive-care-unit patient samples. Braz J Infect Dis. 2009;13:118–22.
Melsen WG, Rovers MM, Groenwold RH, Bergmans DC, Camus C, Bauer TT, et al. Attributable mortality of ventilator-associated pneumonia: a meta-analysis of individual patient data from randomised prevention studies. Lancet Infect Dis. 2013;13:665–71.
Kollef MH. Clinical characteristics and treatment patterns among patients with ventilator-associated pneumonia. Chest. 2006;129:1210–8.
Craven DE, Hjalmarson KI. Ventilator-associated tracheobronchitis and pneumonia: thinking outside the box. Clin Infect Dis. 2010;51:59–66.
Guclu E, Ogutlu A, Kaya G, Karaba O. Invasive device usage and relationship between nosocomial infections. Int J Infect Dis. 2014;21:137.
Apostolopoulou E, Bakakos P, Katostaras T, Gregorakos L. Incidence and risk factors for ventilator-associated pneumonia in 4 multidisciplinary intensive care units in Athens, Greece. Respir Care. 2003;48:681–8.
Makris D, Desrousseaux B, Zakynthinos E, Durocher A, Nseir S. The impact of COPD on ICU mortality in patients with ventilator-associated pneumonia. Respir Med. 2011;105(7):1022–9.
Torres A, Aznar R, Gatell JM, Jimenez P, Gonzalez J, Ferrer A, et al. Incidence, risk, and prognosis factors of nosocomial pneumonia in mechanically ventilated patients. Am Rev Respir Dis. 1990;142:528.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yalçınsoy, M., Salturk, C., Takır, H. et al. Case fatality rate related to nosocomial and ventilator-associated pneumonia in an ICU: a single-centre retrospective cohort study. Wien Klin Wochenschr 128, 95–101 (2016). https://doi.org/10.1007/s00508-015-0884-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-015-0884-6