Summary
Background
In April 2013, an outbreak of acute gastroenteritis was reported in a residential long-term care facility (LTCF) in Ljubljana. We carried out an outbreak investigation to describe the outbreak, identify factors associated with contracting infection and to recommend control measures.
Methods
We conducted descriptive epidemiology of the outbreak and a case-control study among residents; a case was a resident or staff member of the LTCF with acute diarrhoea and at least one of the following symptoms: fever, vomiting, nausea, fatigue, headache and abdominal pain between 11 and 23 April 2013. Controls had no gastrointestinal symptoms during the outbreak period. Stool specimens were tested for enteric pathogens, including Rotavirus.
Results
Of 244, 33 (13.5 %) and 4 of 106 staff (3.8 %) were affected. Twenty-eight (84.8 %; median age 85 years; range 71–95 years) among affected residents and four (100 %; median age 35 years; range 30–45 years) among affected staff were women. The main symptoms besides acute diarrhoea were fatigue (54.1 %) and nausea (45.9 %). The average duration of gastroenteritis symptoms was 3.6 days in residents and 1.3 days in staff. None of the affected persons was hospitalized. Rotavirus group A was detected in a single stool specimen. In the multivariable analysis, being ambulant (aOR = 12.3; 95 % CI: 1.14–133.1), and having more than two comorbidities (aOR = 4.7; 95 % CI: 1.14–19.0) were significantly associated with acute gastroenterocolitis.
Conclusions
Contact precautions of affected persons and controlled staff interactions between outbreak ward and unaffected ward are recommended in times of outbreak, with additional effort in targeting mobile residents and those with comorbidities.
Zusammenfassung
Grundlagen
Im April 2013 wurde ein Ausbruch von akuter Gastroenteritis in einer Langzeitpflege-Residenz in Ljubljana bekannt. Wir führten eine Untersuchung dieses Ausbruchs durch, um ihn zu beschreiben, um die Faktoren, die mit dem Erwerb der Infektion im Zusammenhang stehen zu identifizieren, und um Empfehlungen für Kontrollmaßnahmen zu erarbeiten.
Methoden
Wir führten eine deskriptive Epidemiologie des Ausbruchs und eine Fall-Kontrollstudie unter den Bewohnern des Residenzheims durch. Ein Fall war entweder ein Bewohner oder ein Angestellter des Residenzheims und musste folgende Kriterien erfüllen: akute Diarrhoe und zumindest eines der folgenden Symptome: Fieber, Erbrechen, Übelkeit, Müdigkeit, Kopfweh und Abdominalschmerzen zwischen 11. und 23. April 2013. Die Kontrollen hatten im Zeitraum des Ausbruchs keinerlei gastrointestinale Symptome. Stuhlproben wurden auf pathogene Darmkeime inklusive Rotaviren untersucht.
Ergebnisse
Bei 33 von 244 (13,5 %) Residenzbewohnern bzw. bei 4 von 106 (3,8 %) Angestellten trat die Erkrankung ein. Von den infizierten Bewohnern waren 28 (84,8 %) Frauen (mittleres Alter 85 Jahre; Bereich: 71–95 Jahre). Bei den 4 infizierten Angestellten handelte es sich durchwegs um Frauen (mittleres Alter 35; Bereich: 30–45 Jahre). Abgesehen vom Durchfall war Müdigkeit (54,1 %) und Übelkeit (45,9 %) das Hauptsymptom. Die durchschnittliche Dauer der gastrointestinalen Symptome war 3,6 Tage bei den Residenzbewohnern und 1,3 Tage bei den Angestellten. Keine der befallenen Personen wurde hospitalisiert. In der Multivarianzanalyse war die Gehfähigkeit (aOR = 12,3; 95 % CI: 1,14–133,1) und der Umstand, mehr als 2 Begleiterkrankungen zu haben (aOR = 4,7; 95 % CI: 1,14–19,0), signifikant mit der akuten Gastroenteritis assoziiert.
Schlussfolgerungen
Vorsichtsmaßnahmen im Kontakt mit betroffenen Personen und kontrollierte Interaktionen zwischen den Angestellten mit Infektion und denen ohne werden empfohlen. Besonders hingewiesen wird darauf, dass mobile Residenzheim-Bewohner und solche mit mehr als zwei Begleiterkrankungen besonders gefährdet sind.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rotavirus has been recognized as a major aetiological cause of acute diarrhoeal disease in preschool children. Rotavirus infection is usually characterized by watery diarrhoea, vomiting and fever, with incubation period ranging from 24 to 72 h [1–3]. Infection in adults is usually subclinical, as a result of immunologic tolerance evolving from repeated exposures in the past [4]. Rotavirus occasionally causes illness in parents of children with Rotavirus diarrhoea, immunocompromised persons, the elderly and travellers [2, 5]. The predominant way of transmission is by person-to-person contact via the faecal–oral way, although spread through respiratory secretions, the hands of the health-care personnel or the contaminated environmental surfaces has been described [3, 5, 6]. Animal-to-human transmission is uncommon, although human Rotavirus strains that possess a high degree of genetic homology with animal strains have been identified [5, 7, 8]. There is some evidence that Rotavirus may be present in contaminated water and can also be concentrated by shellfish [7]. Treatment of Rotavirus gastroenteritis is symptomatic [9].
Elderly people living in long-term care facilities (LTCFs) are vulnerable to outbreaks from infectious gastroenteritis, and more likely to experience serious outcomes [10–13]. LTCF residents are particularly susceptible to gastroenteritis because of changes in immune response, gastrointestinal physiology, use of immunosuppressive or acid-suppressive medications, and presence of comorbidities associated with ageing [14–17]. Since institutionalized elderly individuals are clustered in confined living arrangements with common delivery of medical care, food, and water, daily activities arranged in groups and frequent contact with visitors, LTCFs represent a unique environment for the spread of infectious agents [18, 19]. Some residents have dementia and are unable to follow hygiene precautions. In addition, shortage of care staff and inadequate knowledge about infection control measures is a common problem in LTCFs. As a result, the diagnosis and introduction of control measures may be delayed [10]. In recent years, outbreaks of Rotavirus also occurred among elderly in LTCFs with more severe diarrhoea and longer duration of illness than in children [5].
According to the Law on communicable diseases, all cases of acute gastroenteritis and all outbreaks of communicable diseases in Slovenia have to be reported to the National Institute of Public Health (NIPH) of Slovenia. Rotavirus outbreaks in preschool and school environments are commonly reported in Slovenia. However, the first three outbreaks of Rotavirus gastroenteritis in LTCFs were reported only in 2008 (Table 1) [11, 20].
We describe the outbreak of acute gastroenteritis in LTCF in the capital city in April 2013. LTCF notified the NIPH on 16 April 2013 about 21 residents with acute gastroenteritis symptoms. An outbreak control team (OCT) was formed and convened on 18 April 2013.
We report the epidemiological investigation conducted to characterize the outbreak, identify factors associated with contracting gastroenteritis and recommend control measures.
Materials and methods
Descriptive epidemiology
A case patient was defined as any person residing or working in the LTCF with acute diarrhoea (≥ three times/24 h) and at least one of the following symptoms: fever (≥ 38 °C), vomiting, nausea, malaise, headache and abdominal pain, with or without laboratory-confirmed Rotavirus since 11 April 2013.
We collected information on a range of potential exposures, over a period of 7 days prior to the onset of symptoms in the index case, including questions on foods and beverages eaten and places recently visited such as physicians, farms, food venues, families with small children, diet, physical activity, using a walking aid, number of residents per room, number of residents per toilet and bathroom, obesity, urine or faecal incontinence, medical devices, comorbidities (i.e., diabetes mellitus, renal disease, liver disease, cardiovascular disease, pre-existing malignant disease), and possible gastrointestinal symptoms in their family members. The staff reported if they cared for the affected residents and if the residents followed their instructions about restriction to their own units.
Case-control study
Cases were defined as residents with acute gastroenteritis between 11 and 23 April 2013. Residents were chosen randomly from the resident registry as control subjects if they had no evidence of gastroenteritis symptoms or laboratory-confirmed Rotavirus infection during the study period. We excluded individuals with admission date to LTCF during the outbreak period. Controls were selected at a 1:2 ratio and compared with cases in terms of exposure. Chart reviews were conducted for case patients and control subjects by using a data collection form focusing on potential risk factors between 1 and 30 April 2013.
Data analysis
Univariate analyses were performed to identify the variables that were significantly associated with acute gastroenteritis. Subsequently, a backward stepwise multivariable logistic regression model was created by using all statistically significant variables that were identified in the univariate analyses, checking also for interactions. For each variable in the multivariable models, odds ratios (ORs) and 95 % confidence interval (CI) were calculated. P-values of < 0.05 were considered statistically significant. All analyses were performed using Stata 12.0 (Stata Corporation, USA).
Laboratory investigation
Two stool specimens were sent to the Department of Medical Microbiology at the NIPH, and were tested for common enteric pathogens (Escherichia coli, Salmonella, Shigella, Clostridium difficile, Campylobacter, Enteroviruses, Adenoviruses and Rotaviruses).
Environmental investigation
The environmental health investigation included inspection of the institution’s sanitary conditions. The audit of infection control practices included observing of environmental cleanliness, hand-washing facilities, safe handling and disposal of clinical waste, and disinfection standards [21]. We inspected the kitchen and staff while preparing the food. Information about menus served in April 2013 was obtained.
Results
Outbreak description
LTCF comprised 224 residents (age 31–100 years; median 85 years), 177 (79 %) were women. The residents were cared for by 106 employees, including 18 kitchen staff. During the day, residents had an access to one full-time general practitioner (GP) and two registered nurses. LTCF had a special care unit for 35-bed bound residents and residents with dementia. Mobile residents (including residents using wheel chairs) could move freely around the LTCF, and could also visit their relatives or friends. The single or double bedrooms were located between the ground floor and the fifth floor. Double bedrooms shared a toilet and a bathroom. The residents had their meals in a large dining room on the ground floor.
A total of 37 case patients were recorded; of these 33 (89 %) were residents and 4 (11 %) nursing staff. The overall attack rate was 14.7 % among residents and 3.8 % among staff. The outbreak affected 32 (86.5 %) women and 5 (13.5 %) men. Age among affected residents ranged from 71 to 95 years (median: 85 years) and, among the staff, from 30 to 45 years (median: 35 years). The majority of the affected residents were 80–89 years old (53.5 %). The median duration of gastroenteritis symptoms was 1.3 days (1–2 days) among staff and 3.6 days (1–13 days) among residents. The highest proportion of cases was among mobile residents (32 of 33 cases; 97 %). Fifteen (45.5 %) of the affected residents had a single bedroom, and 18 (54.5 %) shared the room, toilet and bathroom with one or more persons.
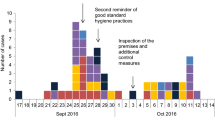
A 91-year-old mobile female resident who became ill on 11 April 2013 was identified as the index case in the outbreak. The next day, infection spread to her neighbour on the ground floor and to other residents from the first to fifth floor. Four affected staff became ill during the weekend between 19 and 22 April 2013. They had all provided care to symptomatic residents. During the outbreak none of the kitchen staff became ill. No cases were reported at the time among the family members of staff. The epidemic curve is shown in Fig. 1. Clinical manifestations of the case patients are presented in Table 2.
Case-control study
Cases had higher odds of having been older than 85 years (OR = 2.9; 95 % CI = 1.1–7.7), having had more than two chronic diseases (OR = 3.8; 95 % CI: 1.0–14.1) and having been mobile (OR = 12.9; 95 % CI: 1.8–554). Following the GP’s instructions (OR = 0.3; 95 % CI: 0.1–1.3), having dementia (OR = 0.3; 95 % CI: 0.1–0.8) and having visited physician the week prior to the onset of symptoms in the index case (OR = 0.4; 95 % CI: 0.1–1.1) were negatively associated with being a case (Table 3).
In the multivariable analysis, having more than two chronic diseases and being mobile were statistically significantly associated with acute gastroenteritis; adjusted ORs and 95 % CI were 4.7 (1.1–19.2) and 12.3 (1.14–133.1), respectively.
Microbiological results
Two stool samples were collected from 88 and 80-year-old female residents on 17 and 23 April 2013, respectively. On 25 April 2013, qualitative enzyme immunoassay confirmed antigens of group A Rotaviruses in one sample. No further genotyping of the samples was performed. Both individuals tested were negative for other common enteric pathogens.
Environmental results
The food preparation standards were good and in accordance with Hazard Analysis and Critical Points specifications. No residual food samples remained for microbiological testing. Because of highly likely person-to-person transmission, no swabbing of environmental surfaces was carried out in this outbreak.
Discussion
An outbreak of acute gastroenteritis affecting of 37 case patients occurred in LTCF in Ljubljana between 11 and 23 April 2013. Group A Rotavirus was detected in one stool sample. The epidemic curve was highly suggestive of person-to-person transmission [6]. Public health authorities were notified only when the number of affected residents was high, which delayed putting in place appropriate control measures.
Underreporting and late reporting of outbreaks is a common problem, although notification of Rotavirus infection in Slovenia is mandatory [10, 12]. In the future more efforts need to be focused on highlighting the importance of reporting outbreaks of acute gastroenteritis by the physicians as close as possible to onset so that outbreak investigation can be initiated in a timely manner and control measures are implemented as soon as possible, even before laboratory confirmation of the agent [11, 22].
Residents with more than two underlying diseases were more likely to acquire acute gastroenteritis in comparison with those with two or less diagnoses of chronic diseases. Comorbidities in elderly are often associated with immunosenescence, frailty and malnutrition, which are factors for higher susceptibility to infections [4, 12].
Mobile residents had elevated risk of infection. It is possible that mobility of the residents may result in higher chance of the transmission of diarrhoea infection within LTCF, as reported by Lin et al. [23].
Disregarding GP’s instructions in respect of restrictions to their units was associated with higher odds of acquiring infection. Here, we highlight the importance of an open dialogue between the health-care staff and LTCF residents regarding rapid response and appropriate interventions performance such as contact precautions, restricting or controlling visitors, contact restrictions of affected persons 2–3 days after their last symptoms because of prolonged viral shedding, and controlled staff interactions between outbreak ward and unaffected ward are recommended in times of outbreak [24].
Physician visit in the week prior to the onset of symptoms in the index case was negatively related to disease among cases. This might be associated with more thorough control and dialogue between residential GP and LTCF residents, also regarding infection protective measures.
Dementia led to lower risk of becoming sick; this is not in accordance with others findings, which report higher prevalence of Rotavirus infections in patients with dementia [5]. In our situation, we assume that the nursing staff paid higher attention to prevention of infection spread in the dementia wards, which usually have higher number of nursing staff and in which residents are restricted to their own units.
Among nursing staff acute gastroenteritis symptoms started during the weekend before a public holiday. Because of the reportedly reduced staffing level on weekends nursing workloads significantly increase [25]. This could have had implications on the provision of standard infection control precautions to residents and contributed to the spread of infection within LTCF environment.
Diagnosis of Rotavirus gastroenteritis was established only in one case patient and already towards the end of the outbreak. In the future, we need to communicate with physicians that rapid notification of the outbreak, together with identification of the agent, is crucial in the effort to control and contain the spread of Rotavirus infection within LTCFs.
Given the results of our investigation, we recommended some control measures. When the first residents presented with diarrhoea symptoms, strict hand washing and use of personal protective equipment by staff were implemented by the residential GP on 12 April, when the number of affected residents increased to eight [26]. At the same time, additional information on cleaning and disinfection of equipment, surfaces and rooms with an appropriate disinfectant for viruses, regular airing of rooms, sanitary inspection of proper disposal of incontinence pads, and restriction of residents to their own units was distributed to residents, their relatives and staff by the OCT. All affected employees were removed from work for a period of 1–3 days. Twelve days after the first report of symptoms of acute gastroenteritis no additional cases occurred, thus cohort isolation of symptomatic residents and LTCF closure to new admissions were not introduced [11, 20]. Moreover, we recommended LTCFs make sure that (a) their medical staff becomes aware of the instructions of the infection control teams that every LTCF has by law and (b) residents understand the importance of the recommended measures in case of outbreaks; these are prerequisites to eliminate the spread of Rotavirus and prevent possible future outbreaks.
Conclusion
Increased emphasis should be placed on timely management measures to stop the spread of Rotavirus in LTCFs, especially in mobile residents and those with comorbidities.
References
Cardemil CV, Cortese MM, Medina-Marino A, et al. Two rotavirus outbreaks caused by genotype G2PF[4] at large retirement communities: cohort studies. Ann Intern Med. 2012;157(9):621–31.
Barnes GL, Uren E, Stevens KB, Bishop RF. Etiology of acute gastroenteritis in hospitalized children in Melbourne, Australia, from April 1980 to March 1993. J Clin Microbiol. 1998;36(1):133–8.
Corwin AL, Subekti D, Sukri NC, et al. A large outbreak of probable rotavirus in Nusa Tenggara Timur, Indonesia. Am J Trop Med Hyg. 2005;72(4):488–94.
Anderson EJ, Weber SG. Rotavirus infection in adults. Lancet Infect Dis. 2004;4(2):91–9.
Parashar UD, Bresee JS, Gentsch JR, Glass RI. Rotavirus. Emerg Infect Dis. 1998;4(4):561–70.
Boone SA, Gerba CP. Significance of fomites in the spread of respiratory and enteric viral disease. Appl Environ Microbiol. 2007;73(6):1687–96.
Bajolet O, Chippaux-Hyppolite C. Rotavirus and other viruses of diarrhoea. Bul Soc Pathol Exot. 1998;91(5 Pt 1–2):432–7.
Nakagomi O, Nakagomi T. Genetic diversity and similarity among mammalian rotaviruses in relation to interspecies transmission of rotavirus. Arch Virol. 1991;120(1–2):43–55.
Wiedermann U, Kollaritsch H. Vaccines against traveller’s diarrhoea and rotavirus disease—a review. Wien Klin Wochenschr. 2006;118(19–20 Suppl. 3):2–8.
Mathei C, Niclaes L, Suetens C, Jans B, Buntinx F. Infections in residents of nursing homes. Infect Dis Clin North Am. 2007;21(3):761–72.
Trop Skaza A, Beskovnik L, Zohar Cretnik T. Outbreak of rotavirus gastroenteritis in a nursing home, Slovenia, December 2010. Euro Surveill. 2011;16(14):pii: 19837.
Trinh C, Prabhakar K. Diarrheal diseases in the elderly. Clin Geriatr Med. 2007;23(4):833–56.
Kirk MD, Veitch MG, Hall GV. Gastroenteritis and food-borne disease in elderly people living in long-term care. Clin Infect Dis. 2010;50(3):397–404. doi:10.1086/649878.
McGlauchlen KS, Vogel LA. Ineffective humoral immunity in the elderly. Microbes Infect. 2003;5(13):1279–84.
Nikolich-Zugich J. Ageing and life-long maintenance of T-cell subsets in the face of latent persistent infections. Nat Rev Immunol. 2008;8(7):512–22. doi:10.1038/nri2318.
Slotwiner-Nie PK. Infectious diarrhoea in the elderly. Gastroenterol Clin North Am. 2001;30(3):625–35.
Gavazzi G. Ageing and infection. Lancet Infect Dis. 2002;2(11):659–66.
Strausbaugh LJ, Sukumar SR, Joseph CL. Infectious disease outbreaks in nursing homes: an unappreciated hazard for frail elderly persons. Clin Infect Dis. 2003;36(7):870–6.
Garibaldi RA, Brodine S, Matsumiya S. Infections among patients in nursing homes: policies, prevalence, problems. N Engl J Med. 1981;305(13):731–5.
Epidemiological surveillance of reported communicable diseases in Slovenia in 2011. Institute of Public Health of the Republic of Slovenia. Ljubljana, November 2012. www.ivz.si/gradiva_nalezljive_bolezni?pi=5_5_Filename=attName.png_5_MediaId=7727_5_AutoResize=falsepl=105-5.3. Accessed: 15 April 2014.
Milward S, Barnett J, Thomlinson D. A clinical infection control audit program: evaluation of an audit tool used by infection control nurses to monitor standards and assess effective staff training. J Hosp Infect. 1993;24(3):219–32.
Schmid D, Lederer I, Pichler AM, Berghold C, Schreier E, Allerberger F. An outbreak of Norovirus infection affecting an Austrian nursing home and a hospital. Wien Klin Wochenschr. 2005;117(23–24):802–8.
Lin H, Ng S, Chan S, Chan WM, Lee KC, Ho SC, Tian L. Institutional risk factors for norovirus outbreaks in Hong Kong elderly homes: a retrospective cohort study. BMC Public Health. 2011;11:297–303. doi:10.1186/1471-2458-11-297.
Virginia Department of Health. Guidelines for the control of a suspected or confirmed outbreak of viral gastroenteritis in a nursing home. 2004. www.vhd.state.va.us/epi/noro_outbreak_guidelines.pdf. Accessed: 13 Feb 2004.
Lang TA, Hodge M, Olson V, Romano PS, Kravitz RL. Nurse-patient ratios: a systematic review on the effects of nurse staffing on patient, nurse employee, and hospital outcomes. J Nurs Adm. 2004;34(7–8):326–37.
Barker J, Vipond IB, Bloomfield SF. Effects of cleaning and disinfection in reducing the spread of Norovirus contamination via environmental surfaces. J Hosp Infect. 2004;58(1):42–9.
Conflict of interest
The authors declare that there are no actual or potential conflicts of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Šubelj, M., Učakar, V. An outbreak of acute gastroenteritis associated with group A Rotavirus in long-term care facility in Slovenia. Wien Klin Wochenschr 127, 415–420 (2015). https://doi.org/10.1007/s00508-014-0672-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-014-0672-8