Summary
Aim
To investigate associations between the postoperative immune response and the levels of extracellular circulating DNA (cDNA), C-reactive protein (CRP), neutrophil/lymphocyte (N/L) ratio, and regulatory T (Treg) cells in the peripheral blood and their role as potential predictors of postoperative septic complications.
Methods
This was a prospective observational study involving 115 adult patients who underwent elective surgery. Patients were divided into three groups: with benign disease, with malignant disease, and with malignant disease and administration of dexamethasone. Serum CRP levels, N/L ratio, monocyte human leukocyte antigen-DR (HLA-DR) expression, proportion of Treg cells, and cDNA levels were measured at different time points before and after surgery.
Results
All patients had increased CRP levels after surgery. Septic patients had higher serum CRP levels at baseline. Compared with the other groups, the dexamethasone group had significantly higher CRP levels before and after surgery, a significantly higher N/L ratio before surgery, a significantly lower rise in the N/L ratio after surgery, and a significantly lower HLA-DR expression at baseline, which remained stable after surgery. In the malignant-disease group, we observed a significant postoperative decrease in the HLA-DR expression.
Conclusions
Our results suggest that the immunosuppressive effect of surgery and the presence of a malignant disease may contribute to a higher risk of postoperative sepsis. Preoperative CRP levels may be a reliable predictor of sepsis in oncological patients.
Zusammenfassung
Ziel
der Studie war es, Zusammenhänge zwischen der postoperativen Immunantwort und den Konzentrationen der zirkulierenden extrazellulären DNA (cDNA), des CRPs, des Quotienten Neutrophile/Lymphozyten (N/L) und der regulatorischen T (Treg) Zellen im peripheren Blut sowie deren Rolle als mögliche Vorhersager von postoperativen septischen Komplikationen zu untersuchen.
Methoden
In diese prospektive Beobachtungsstudie haben wir 115 erwachsene Patienten, die einer elektiven Operation unterzogen wurden, eingeschlossen. Die Patienten wurden in 3 Gruppen eingeteilt: eine mit benigner Erkrankung, eine mit maligner Erkrankung und eine mit maligner Erkrankung und Gabe von Dexamethason. Die Serum-Konzentrationen des CRPs, der N/L Quotienten, der HLA-DR Expression der Monozyten, des Anteils der Treg Zellen und die Konzentrationen der cDNA wurden zu verschiedenen Zeitpunkten vor und nach der Operation gemessen.
Ergebnisse
Alle Patienten hatten nach der Operation erhöhte CRP Konzentrationen. Bei den Patienten mit postoperativer Sepsis waren die CRP Ausgangswerte höher. Im Vergleich mit den anderen Gruppen hatte die Gruppe der Patienten mit Dexamethason signifikant höhere CRP Werte vor und nach der Operation. Außerdem waren die N/L Quotienten präoperativ vergleichsweise signifikant erhöht, während postoperativ bei dieser Gruppe ein signifikant niedrigerer Anstieg der N/L Quotienten beobachtet wurde. Die Ausgangswerte der HLA-DR Expression waren bei diesen Patienten signifikant erniedrigt und blieben postoperativ stabil. Bei der Gruppe der Patienten mit maligner Erkrankung beobachteten wir postoperativ einen signifikanten Abfall der HLA-DR Expression.
Schlussfolgerungen
Unsere Ergebnisse lassen vermuten, dass der immunsuppressive Effekt einer Operation und das Vorliegen einer malignen Erkrankung zu einem erhöhten Risiko für das Auftreten einer postoperativen Sepsis beitragen können. Präoperative CRP Werte scheinen einen verlässlichen Vorhersagewert bezüglich Sepsis bei onkologischen Patienten zu haben.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical trauma is followed by an inflammatory response as part of an adaptive immune response. The response of a host to surgery and injury occurs in two consecutive phases: systemic inflammatory response syndrome (SIRS) develops first and then evolves into compensated anti-inflammatory response syndrome (CARS) within several days or weeks [1–11]. Both the type and site of the surgery affect the postoperative immune response. It is generally acknowledged that abdominal operations, due to their extent and high risk of microbial contamination, are often associated with SIRS and secondary immunosuppression. The surgical damage to anatomical barriers facilitates the penetration of pathogenic microbes into the body. This, together with decreased immunoreactivity, weakens the natural antimicrobial protection and makes the host susceptible to infection [2, 5–9, 12, 13].
Although a positive correlation between postoperative immunosuppression and the occurrence of infection-related postoperative complications has been reported, so far there has been no conclusive evidence to confirm this association [14, 15]. Immune reactivity in the postoperative period may be affected by such factors as age, sex, primary and associated diseases, as well as the drugs that have been taken before, during, or after the surgery [1–3, 9, 16].
It is known that patients who undergo surgery due to malignant disease have a greater tendency to develop infection-related complications in the postoperative period [9, 17, 18]. There is no consensus as to the effect of the perioperative administration of immunomodulatory drugs (such as corticosteroids, statins, and vasoactive catecholamines) on immune reactivity [4, 19–27]. Given the complexity of the host’s immune response to tissue injury and surgery, it is difficult to determine the effect of each of the contributing factors on the expression of the immune response and the occurrence of postoperative immunodepression.
There is growing evidence that the enhanced level of extracellular circulating nucleic acids may be used as a potential biomarker for tissue injury in systemic inflammation (even that caused by surgery) and sepsis, especially in patients with cancer.
The intensity of the immune reaction to surgical trauma can be evaluated on the basis of clinical and laboratory findings specifically associated with SIRS.
However, the expression of the immune response to surgical trauma or injury may be assessed more accurately by measuring immune activation markers, such as the serum levels of C-reactive protein (CRP), neutrophil/lymphocyte (N/L) ratio, monocyte human leukocyte antigen-DR (HLA-DR) antigen expression, and the activity of regulatory T (Treg) cells in the peripheral blood [28–30]. The extent of surgical tissue damage can be evaluated by measuring the serum levels of extracellular circulating DNA (cDNA).
The aim of our study was to investigate how and to what extent the type of surgery, nature of the primary disease, and perioperative administration of immunomodulatory drugs, such as dexamethasone, affect the expression of the immune response and to determine the role of immune activation markers (such as CRP, N/L ratio, HLA-DR, and Treg cells) as potential predictors of postoperative septic complications.
Patients and methods
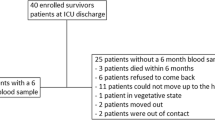
It was a prospective observational study that included a total of 115 patients aged from 18 to 80 years who were recruited between October 2010 and June 2011. All patients underwent elective surgery due to intestinal organs diseases, expansive process of central nervous system, or degenerative hip disease. They were classified as status I or II patients according to the American Society of Anesthesiologists (ASA) Physical Status Classification System. Based on the primary disease and postoperative administration of drugs, they were divided into three groups: patients with benign disease (benign-disease group), patients with malignant disease (malignant-disease group), and patients with malignant disease who received dexamethasone (dexamethasone group).
The exclusion criteria were as follows: clinical or microbiological evidence of infection, immunosuppressive therapy for a longer period of time, any chronic diseases that might cause immunosuppression. Patients in whom an ongoing infection was detected during surgery were also excluded from the study. The study was approved by the Ethics Committees of the University Hospital Centre Osijek and of the Medical Faculty Osijek.
Abdominal and neurosurgical procedures were performed under balanced general anesthesia, while hip implant surgery was performed under regional anesthesia in most patients. All patients underwent the usual antimicrobial prophylaxis. Neurosurgical patients who underwent craniotomy for a primary or a metastatic brain tumor were administered dexamethasone in the perioperative period, at a dose of 8–24 mg, for minimum 24 h, with the maximum therapy duration of 20 days. Drug administration began between the first and 13th day before the surgery and continued for 5–10 days after the surgery, depending on the clinical course.
After the operation, patients were monitored in the intensive care unit of the Anaesthesiology Department or in the Intermediary Care Units of the respective surgical departments (abdominal surgery, orthopaedic surgery). Patients’ clinical status was evaluated 24 h after the surgery using APACHE III score adapted for patients who underwent elective surgical procedure [31].
Assessment of the immune response to surgical trauma and infection was based on the expression of the clinical signs of SIRS as well as on the changes of the hematological and biochemical markers of immune activity. Sepsis was diagnosed when SIRS and clinically or microbiologically confirmed infection were determined [32]. Clinical status of patients with local infection, SIRS, or sepsis was evaluated with APACHE III and Elebute-Stoner scale [33–35].
We measured serum cDNA and CRP levels, monocyte HLA-DR expression, proportion of Treg cells, and N/L ratio in the peripheral blood. Blood for analysis was drawn from the peripheral vein. The measurements were conducted 1 day before the surgery (T0), 24 h after beginning the surgical procedure (T1), and 2 (T2), 3 (T3), and 5 days (T4) after the surgery. cDNA levels were measured at T0 and T1; CRP levels at T0, T1, T2, T3, and T4; HLA-DR expression and N/L ratio at T0, T1, and T2.
Measurement of extracellular circulating DNA in serum
We used 100 μL of serum to isolate DNA using the DNeasy Blood & Tissue Kit (QIAGEN GmbH, Germany), according to the manufacturer’s protocol. The amount of cDNA in the sera of patients was determined by real-time PCR using the QuantifilerTM Human DNA Quantification Kit (Applied Biosystems, USA) [36]. The measurement of serum CRP and procalcitonin levels and the differential blood count used to assess the N/L ratio are part of routine laboratory tests performed in our Clinical Hospital Center.
Immunophenotyping of peripheral blood monocytes
The HLA-DR expression on monocytes was determined by double staining with monoclonal antibodies specific for HLA-DR (FITC) and CD13 (PE) (BD Biosciences, USA). A flow cytometry analysis was performed by FACSCalibur, BD Flow Cytometer, by using the CellQuest software.
Statistical analysis
Data were described using descriptive statistical methods.
The Mann–Whitney and the Wilcoxon test were used to compare samples. The Friedman’s test was used to detect the differences between dependent samples. The receiver operating curve (ROC) analysis was used to determine the optimal threshold, area under the curve (AUC), specificity, and sensitivity of the tested parameters. The Spearman’s rho test was used to determine the association between non-normally distributed variables. The level of significance was set at P of 0.05. The statistical analysis was performed using SPSS 17.0 (SPSS Inc., Chicago, IL, USA), and the ROC analysis using MedCalc 11.5.0 (MedCalc Software, Ostend, Belgium).
Results
The study involved 115 patients. Their demographical and clinical characteristics are shown in Table 1. A benign disease was a cause of surgical procedure in 60 cases (53 %), and a malignant disease in 55 (47 %). In all, 23 patients (20 %) had metastatic or primary malignant brain tumor, and 10 patients (8.7 %) had stomach cancer. The rest of the malignant disease cases had either esophagus, pancreas, or colon cancer. Hip arthrosis was a cause of surgery in 41 patients (35.7 %). The rest of the patients had benign diseases of the digestive system (ulcer colitis, liver tumor, abdominal wall tumor) and central nerve system (meningioma, cerebral aneurism).
Statins (atorvastatin or simvastatin, 20 mg) were used by 13 % of the patients, mostly those with benign disease. Intrasurgical vasoactive support, including the dose of ephedrine (20–40 mg), was needed in 26.96 % of the patients, mostly those who underwent spinal anesthesia.
After surgery, patients were held in the intensive care unit for 24–48 h. Overall, 49 of the patients (42.6 %) had mechanical ventilation during 6 h [3, 5–8]. APACHE III score average value 24 h after surgery was 21 [14–27].
Postsurgical infection complications arose in 17 patients (14.78 %) (6 infection wounds, 1 mediastinitis, 1 peritonitis, 1 pleural empyema, 1 suphepatal apsces, 1 deep tissue infection after hip arthroplasty, 2 postsurgical meningitis, 4 pneumonia).
A total of 10 patients developed SIRS or sepsis during follow-up (six patients from the malignant disease-group, two from the benign-disease group, and two from the dexamethasone group). SIRS without infection was present in two patients. Sepsis was confirmed in two patients by positive hemoculture (Candida albicans, Enterococcus faecalis), while the diagnosis in the rest of the septic patients was based upon the presence of SIRS and clinical signs of infection, as well as microbiological test. Staphylococcus epidermidis was isolated from the infected wounds of two patients after the hip arthroplasty, and from the cerebrospinal fluid of two patients with postsurgical meningitis. Methicillin-resistant Staphylococcus aureus (MRSE) was isolated in patients with endoprothesical infection (deep infection after hip arthroplasty). Proteus mirabilis and Pseudomonas aeruginsa were isolated from the abdominal content in patients with diffused peritonitis. Acinetobacter baumani and E. faecalis were isolated in a skeptical patient with a negative hemoculture.
APACHE III score average value in patients with local infection was 27.5 (18.75–27.5), and 31 in ones with sepsis, while the Elebute-Stoner score in patients with local infection was 8 (6.5–12.5), and 14 in ones with sepsis (Table 2). The presence of sepsis did not contribute to the development of clinically relevant organic dysfunction like hemodynamic instability and kidney function disorder.
Massive pulmonary S embolism was a direct cause of death in a patient with liver hemangioma, pneumonia in a patient with (brain) glioblastoma and a patient with metastasic brain tumor and primary lungs tumor. Propagation of malignant disease that occurred 2.5 months after the surgery was the cause of death in a patient with esophagus cancer.
Serum CRP levels were measured on the day before the surgery and on the first, second, third, and fifth days after the surgery. Baseline CRP levels were above the upper limit of the reference range (> 5 mg/L) in 42 % of the patients. The highest median CRP level was observed on the second postoperative day in all three groups. Postoperative CRP levels were significantly higher in patients with malignant disease in all measurements (Kruskal–Wallis test, P < 0.001). There was also a significant difference in CRP levels within each group (Friedman’s test, P < 0.001, Table 3).
Immunophenotyping of the peripheral blood cells for monocyte HLA-DR expression was performed on the day before surgery and on the first and second days after the surgery. The HLA-DR expression decreased significantly after the surgery in the malignant-disease group (Friedman’s test, P < 0.001). The differences in the HLA-DR expression between the three groups are shown in Table 4.
No significant correlations were observed for cDNA levels. There was no significant increase in cDNA levels 1 day after the surgery in any of the groups (Table 5).
The N/L ratio was measured 1 day before the surgery and on the first and second days after the surgery. It was significantly higher in the malignant-disease group both before (P = 0.029) and after the surgery (P < 0.001). A significant difference in the N/L ratio was also observed within each group of patients, depending on the time point of the measurement (P < 0.001, Table 6).
Presurgical application of statin did not affect the change of serum CRP levels, the value of N/L ratio, and the concentration of cDNA in the postsurgical period. However, the patient group that received statins was found to have lower postsurgical decrease in HLA-DR compared with the patient group that did not receive those medications (P = 0.558; P < 0.001; Table 7).
The patient group that, during the surgery, needed vasoactive support was also found to have lower postsurgical decrease in HLA-DR compared with the group that did not receive vasopressors (P = 0.595; P < 0.001; Table 8). The patients who received vasopressors had lower N/L ratio the day before the surgery (P = 0.046) as well as on the first (P = 0.005) and on the second day after the surgery (P = 0.002) compared with those that needed vasopressors (Table 8).
The ROC analysis is presented in Fig. 1. The AUC for malignant diseases was 0.752 (P < 0.05; CI 95 %, 0.58–0.88; Fig. 1a). The best threshold (that is, such that maximizes sensitivity and specificity) to discriminate between septic and nonseptic patients in the oncological group was the value higher than 10.2 for CRP. At the threshold of > 10.2, the test had 71.4 % sensitivity and 80 % specificity (Fig. 1b). No threshold to efficiently discriminate between septic and nonseptic patients was found in the benign-disease group (Fig. 1b).
a Receiver operating curve parameters of all the parameters measured on the day before the surgery for predicting sepsis. The area under the curve (AUC) for malignant diseases was 0.752 (P < 0.05; CI 95 %, 0.58–0.88). The best threshold (that is, such that it maximizes sensitivity and specificity) to discriminate between septic and nonseptic patients in the malignant-disease group was the value > 10.2 mg/L for CRP. b At the threshold level of > 10.2 mg/L, the test had 71.4 % sensitivity and 80 % specificity. No threshold to efficiently discriminate between septic and nonseptic patients was found in the benign-disease group
Discussion
The aim of this study was to investigate how and to what extent the type of surgery, nature of the primary disease, and perioperative administration of immunomodulatory drugs, such as dexamethasone, affect the expression of the immune response and to determine whether it is possible to predict postoperative septic complications by measuring specific markers of immune activity. To assess the expression of postoperative immune suppression, we measured serum CRP levels, N/L ratio, and monocyte HLA-DR expression. We evaluated the immune status of patients by measuring the percentage of Treg cells in the preoperative period and assessed the extent of tissue damage by measuring serum cDNA levels.
Our patients were of medium or medium high surgery risk (ASA II/III). Relatively low value of APACHE III score 24 h after the surgery shows that surgical procedure did not result in a more significant disruption of their general condition. Vasoactive support was needed only in patients that were subjected to spinal anesthesia. Most of the patients were held under intensive care for 24 h. Around 50 % of the patients needed short-term mechanical ventilation (6 h).
Complications associated with the local infection (surgical site infection) were equally distributed among all three groups. Patients with malignant diseases who underwent abdominal procedure experienced more septic complications (SIRS or sepsis) postoperatively. It is widely known that extensive intra-abdominal procedures, including resection, are relatively often followed by SIRS, which can progress to sepsis, due to a high risk of microbial contamination during surgical manipulation [5–9, 12, 13]. It is also generally acknowledged that malignant diseases can lead to immunosuppression, and thus, a higher risk of developing serious infection complications [9, 17, 18]. Relatively low values of APACHE III and Elebute-Stoner score that were recorded in our patients during the occurrence of sepsis testify that it is a case of a lighter form of disease that did not lead to more severe organic dysfunction.
Tissue destruction (cytolysis) is the most important factor responsible for the release of cell DNA. An increase in serum DNA concentrations was reported after trauma injury, burns, surgery, and in cases of advanced malignant disease and sepsis [37–42]. According to Banki et al. [40, 41], the highest rise in cDNA levels (linked to surgical damage) is observed during and immediately after surgery. A subsequent rise in the DNA concentration may signal the development of postoperative complication or the spread of malignant disease [40, 41].
We observed no differences in baseline cDNA levels between our study groups, which suggests that localized malignant disease most probably does not affect DNA release. This finding is in line with that of other reports [42]. In our study, we did not observe a rise in postoperative DNA levels, probably because the number of measurements was too low. Therefore, the values obtained 24 h after surgery were not a reliable indicator of the extent of surgical damage.
According to a recent paper [42], cell DNA released during surgical manipulation (due to tissue damage) can act as a danger signal and induce immune response to damage.
Differences in the values of immune activation markers between our study groups suggest that patients may use different immune mechanisms. The highest increase in median postoperative CRP levels was observed in patients with malignant disease who underwent intra-abdominal procedures, which reflects the extent of surgical damage and the expression of systemic immune reaction to damage. A lower rise in CRP levels was observed in patients with benign disease (mainly patients with hip osteoarthritis), which indicates lower intensity of the immune response and less extensive surgical damage. A lower and delayed rise in serum CRP levels in patients with intracranial tumor who received dexamethasone in the perioperative period can be interpreted in two ways. First, those patients underwent craniotomy, which caused less extensive tissue damage compared with abdominal procedures, suggesting that a mild and mostly localized immune response occurs after an intracranial operation [43, 44]. The second possible interpretation is that a delayed and reduced immune response to damage caused by an intracranial surgery can be a result of the immunomodulatory effect of dexamethasone administered for the treatment of peritumoral edema. It is widely accepted that corticosteroids affect all aspects of the immune response and that their effectiveness in the inhibition of cytokine response is more pronounced if they are administered before a surgical insult [19]. In our study, preoperative CRP levels were higher in patients who developed SIRS after the surgery and septic complications occurred more often in patients with malignant disease. The ROC analysis suggested that baseline CRP levels might be used as a reliable predictor of postoperative SIRS and sepsis in these patients. In those patients not diagnosed with any infection before the surgery, the increased levels of CRP could point to spread of malignant disease, which makes them more susceptible to the development of septic complications.
We observed a higher N/L ratio at baseline in patients treated with dexamethasone, which most probably results from the pharmacological effect of this immunomodulatory drug. A significant postoperative rise in the median N/L ratio among patients with benign and malignant disease suggests the presence of inflammatory reaction and the associated activation of the endogenous anti-inflammatory system. Since oncological patients are exposed to extensive surgical damage and high risk of SIRS, the rise in the N/L ratio is expected to be higher than that in patients with benign disease. A lower N/L ratio among patients who were treated with dexamethasone during the perioperative period can be interpreted in two ways. First, craniotomies most probably induce a mild and mostly localized immune response and, accordingly, a lower anti-inflammatory response owing to less extensive tissue damage. The other possibility is that dexamethasone, when administered prior to craniotomy, may reduce the intracranial inflammatory response. In our study, we observed a significantly lower HLA-DR expression at baseline in patients who received dexamethasone, and this effect was most probably caused by drug intake [21, 45]. Moreover, we did not observe a reduction in postoperative HLA-DR expression, which is contrary to the findings reported by other authors [43]. This could also be attributed to the effect of dexamethasone. We assumed that the perioperative administration of corticosteroids inhibited intracranial inflammation and, as a result, the endogenous anti-inflammatory system was not activated.
A significant postoperative reduction in the HLA-DR expression in oncological patients who had normal HLA-DR levels at baseline suggests that immunosuppression was triggered by surgical damage. As stated above, SIRS accompanied by CARS and secondary immunosuppression often occur after extensive intra-abdominal procedures due to their extent and higher risk of microbial contamination [16, 46, 47]. In the group of patients with benign disease, less extensive tissue damage induced a milder inflammatory response and proportionally less expressed anti-inflammatory response with a noted decrease in the HLA-DR expression [48].
Within the patient group that received statins we noted lower postsurgical decrease in HLA-DR values. We could argue about possible immune-modulatory effect of these medications [24, 25], which can be neither confirmed nor ruled out based on this study. It should also be noted that 10 of 15 patients that received statins belonged to the benign group, and 3 of the patients to the malignant group with dexamethasone. It was also mentioned that these patients, due to the less extensive surgical wound, expect less intense inflammatory infection lower postsurgical decrease in HLA-DR values.
Within the patient group that received vasopressors we also noted lower postsurgical decrease in HLA-DR values. Those patients also show significantly lower values of N/L ratio compared with those that did not need vasoactive support. In this case we could assume possible immune-modulatory effect of the applied vasopressor (ephedrine) [49]. The collected results offer no solid ground for either proving or discarding this hypothesis. It should be pointed out that 46.7 % of patients (20 of 31) that were given vasopressors during surgery belonged to the benign group, and with regard to their less extensive surgical wound we could expect them to have less intense inflammatory reaction. The mentioned patients were subjected to spinal anesthesia that can also influence immune reactivity.
Based on these results, possible effect of statin and vasopressors on postsurgical immune reactivity remains ambiguous. The effect of these medications should be studied in a controlled environment on a homogenous group of surgical patients.
The results of this study support the hypothesis of the effect of the nature of disease, and the type and place of surgical procedure on the extent of the wound induced immune response. They also confirm immune-modulatory effect of the perisurgical application of corticosteroids. However, a transitory immune suppression as a part of an adapting response to the wound and the immune suppressive effect of corticosteroids are not the most important factors responsible for the occurrence of the postsurgical infection complications. The nature and the extent of the original disease, as well as extensiveness of the surgical procedure with possible risk of surgical complications, are decisive factors responsible for the occurrence of postsurgical sepsis.
The main limitation of this study was a short follow-up period, which made it impossible to gain a broader view into the kinetics of the examined immune activation markers or evaluate their clinical importance. A study with a longer follow-up and a higher number of patients could provide a deeper insight and contribute to a better understanding of this complex issue.
Conclusion
The main findings of our study may be summarized as follows. Our results support the hypothesis that the type and site of surgery, the nature of the primary disease, and perioperative drug administration can interfere with the expression of postoperative immune response. Differences in the levels of immune activation markers suggest that different groups of patients have different immune reaction patterns. In the absence of other risk factors, malignant disease has only a minor effect on immune reactivity. A pronounced postoperative rise in serum CRP levels, a higher N/L ratio, and a decrease in monocyte HLA-DR expression in oncological patients who underwent abdominal procedures indicate the presence of SIRS and secondary immunosuppression. A higher rate of septic complications among patients with malignant disease suggests that these patients are more susceptible to immunosuppression both because of the nature of the primary disease and the extent of the surgical procedure. A higher N/L ratio at baseline and a lower HLA-DR expression among patients who received dexamethasone prior to surgery suggest lower immunoreactivity caused by an immunomodulatory effect of the administered drug. Furthermore, a moderate rise in postoperative CRP levels and the N/L ratio together with a nonsignificant change in the HLA-DR expression support the hypothesis of an iatrogenically induced reduction of the immune response. Unlike CRP levels, the baseline levels of other immune activation markers (DNA, N/L ratio, HLA-DR expression) did not prove to be reliable predictors of postoperative SIRS or sepsis.
References
Salo M. Effects of anaesthesia and surgery on the immune response. Acta Anaesthesiol Scand. 1992;36:202–20.
Munford RS, Pugin J. Normal responses to injury prevent systemic inflammation and can be immunosuppressive. Am J Respir Crit Care Med. 2001;163:316–21.
Schulze S. Humoral and neural mediators of the systemic response to surgery. Dan Med Bull. 1996;40:365–77.
Guirao X, Lowry SF. Biologic control of injury and inflammation: much more than too little or too late. World J Surg. 1996;20:437–46.
Mannick JA, Rodrick ML, Lederer JA. The immunologic response to injury. J Am Coll Surg. 2001;193:237–44.
Murphy TJ, Paterson HM, Mannick JA, Lederer JA. Injury, sepsis, and regulation of Toll-like receptors responses. J Leukoc Biol. 2004;75:400–7.
Murphy TJ, Paterson HM, Kriynovich S, Zang Y, Kurt-Jones EA, Mannick JA, et al. Linking the “two-hit” response following injury to enhanced TLR4 reactivity. J Leukoc Biol. 2005;77:16–23.
Hensler T, Hecker H, Heeg K, Heidecke CD, Bartels H, Barthlen W, et al. Distinct mechanisms of immunosuppression as a consequence of major surgery. Infect Immun. 1997;65:2283–91.
Mokart D, Capo C, Blache JL, Delpero JR, Houvenaeghel G, Martin C, et al. Early postoperative compensatory anti-inflammatory response syndrome is associated with septic complications after major surgical trauma in patients with cancer. Br J Surg. 2002;89:1450–6.
Tschoeke SK, Ertel W. Immunoparalysis after multiple trauma. Injury. 2007;38:1346–57.
Castellheim A, Brekke OL, Espevik T, Harboe M, Mollnes E. Innate immune responses to danger signals in systemic inflammatory response syndrome and sepsis. Scand J Immunol. 2009;69:479–91.
Ziegenfuss T, Wanner GA, Grass C, Bauer I, Schüder G, Kleinschmidt S, et al. Mixed agonistic-antagonistic cytokine response in whole blood from patients undergoing abdominal aortic aneurysm repair. Intensive Care Med. 1999;25:279–87.
Angele MK, Faist E. Clinical review: immunodepression in the surgical patient and increased susceptibility to infection. Critical Care. 2002;6:298–305.
Flohé S, Lendemans S, Schade FU, Kreuzfelder E, Waydhas C. Influence of surgical intervention in the immune response of severely injured patients. Int Care Med. 2004;30:96–102.
Dehne M, Sablotzki A, Hoffmann A, Mühling J, Dietrich FE, Hempelmann G. Alterations of acute phase reaction and cytokine production in patients following severe burn injury. Burns. 2002;28:535–42.
Mokart D, Leone M, Sannini A, Brun JP, Tison A, Delpero JR, et al. Predictive perioperative factors for developing severe sepsis after major surgery. Br J Anaesth. 2005;95:776–81.
Hase S, Weinitschke K, Fischer K, Fornara P, Honda R, Unverzagt S, et al. Monitoring peri-operative immune suppression in renal cancer patients. Oncol Rep. 2011;25:1455–64.
Vuk-Pavlović S, Bulur PA, Lin Y, Qin R, Szumianski CL, Zhao X, et al. Immunosuppressive CD14 + HLA-DRlow/- monocytes in prostate cancer. Prostate. 2010;70:443–55.
Sapolsky RM, Romero LM, Munck AU. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocr Rev. 2000;21:55–89.
Schwiebert LM, Schleimer RP, Radka SF, Ono SJ. Modulation of MHC class II expression in human cells by dexamethasone. Cell Immunol. 1995;165:12–9.
Le Tulzo Y, Pangault C, Amiot L, Guilloux V, Tribut O, Arvieux C, et al. Monocyte human leukocyte antigen-DR transcriptional downregulation by cortisol during septic shock. Am J Crit Care Med. 2004;169:1144–51.
Sato N, Koeda K, Ikeda K, Kimura Y, Aoki K, Iwaya T, et al. Randomized study of the benefits of preoperative corticosteroid administration on the postoperative morbidity and cytokine response in patients undergoing surgery for esophageal cancer. Ann Surg. 2002;236:184–90.
Annane D, Bellissant E, Bollaert PE, Briegel J, Confalonieri M, de Gaudio R, et al. Corticosteroids in the treatment of severe sepsis and septic shock in adults. JAMA. 2009;301:2362–75.
Devaraj S, Rogers J, Jialal I. Statins and biomarkers of inflammation. Curr Atheroscler Rep. 2007;9:33–41.
Quist-Paulsen P. Statins and inflammation: an update. Curr Opin Cardiol. 2010;25:399–405.
Bergmann M, Sautner T. Immunomodulatory effects of vasoactive catecholamines. Wien Klin Wochenschr. 2002;114:752–61.
Oberbeck R. Catecholamines: physiological immunomodulators during health and illness. Curr Med Chem. 2006;13:1979–89.
de Jager CPC, van Wijk PT, Mathoera RB, de Jong-Leuvenink J, van der Poll T, Wever PC. Lymphocytopenia and neutrophil-lymphocyte count ratio predict bacteremia better than conventional infection markers in an emergency care unit. Crit Care. 2010;14:R192.
Gang F, Guorong L, An Z, Anne GP, Christian G, Jacques T. Prediction of clear cell renal cell carcinoma by integrity of cell-free DNA in serum. Urology. 2010;75:262–5.
MacConmara MP, Maung AA, Fujimi S, McKenna AM, Delisle A, Lapchak PH, et al. Increased CD4 + CD25 + T regulatory cell activity in trauma patients depresses protective Th1 immunity. Ann Surg. 2006;244:514–23.
Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG. The APACHE III prognostic system (Risk prediction of hospital mortality for critically ill hospitalized Adults). Chest. 1991;100:1619–36.
American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med. 1992;20:864–74.
Elebute EA, Stoner HB. The grading of sepsis. Br J Surg. 1983;70:29–31.
Pilz G, Kaab S, Kreuzer E, Werdan K. Evaluation of definition and parameters for sepsis assessment in patients after cardiac surgrey. Infection. 1994;22:8–17.
Kellner P, Prondzinsky R, Pallman L, Siegmann S, Unverzagt S, Lemm H. Predictive value of outcome scores in patients suffering from cardiogenic shock complicating AMI. Med Klin Intensivmed Notfmed. 2013;108:666–74.
Gornik I, Wagner J, Gasparović V, Lauc G, Gornik O. Free serum DNA is an early predictor of severity in acute pancreatitis. Clin Biochem. 2009;42:38–43.
Lam NY, Rainer TH, Chan LY, Joynt GM, Lo YM. Time course of early and late changes in plasma DNA in trauma patients. Clin Chem. 2003;49:1286–91.
Chiu TW, Young R, Chan LY, Burd A, Lo DY. Plasma cell-free DNA as an indicator of severity injury in burn patients. Clin Chem Lab Med. 2006;44:13–7.
Rhodes A, Wort SJ, Thomas H, Collinson P, Bennett ED. Plasma DNA concentration as a predictor of mortality and sepsis in critically ill patients. Crit Care. 2006;10:R60.
Banki F, Mason RJ, Oh D, Hagen JA, DeMeester SR, Lipham JC, et al. Plasma DNA as a molecular marker for completeness of resection and recurrent disease in patients with esophageal cancer. Arch Surg. 2007;142:533–8.
Banki F, Mason RJ, Hagen JA, Demeester SR, Lipham JC, Danenberg K, et al. Plasma DNA: a molecular marker of surgical insult and postoperative recovery in esophageal cancer. Eur Surg Res. 2008;40:273–8.
Holdenrieder S, Burges A, Reich O, Spelsberg FW, Stieber P. DNA integrity in plasma and serum of patients with malignant and benign diseases. Am N Y Acad Sci. 2008;1137:162–70.
Assadullah K, Woiciechowsky C, Döcke WD, Liebenthal C, Wauer H, Kox W, et al. Immunodepression following neurosurgical procedures. Crit Care Med. 1995;23:1976–83.
Woiciechowsky C, Assadullah K, Nestler D, Eberhardt B, Platzer C, Schöning B, et al. Sympathetic activation triggers systemic interleukin-10 release in immunodepression induced by brain injury. Nat Med. 1998;4:808–13.
Woiciechowsky C, Schöning B, Lanksch WR, Volk HD, Döcke WD. Mechanisms of brain-mediated systemic anti-inflammatory syndrome causing immunodepression. J Mol Med (Berl). 1999;77:769–80.
Haga Y, Beppu T, Doi K, Nozawa F, Mugita N, Ikei S, et al. Systemic inflammatory response syndrome and organ dysfunction following gastrointestinal surgery. Crit Care Med. 1997;25:1994–2000.
Mokart D, Textoris J, Chow-Chine L, Braun JP, Sannini A, Turrini O, et al. HLA-DR and B7-2 (CD86) monocyte expressions after major cancer surgery: profile in sepsis. Minerva Anestesiol. 2011;77:522–7.
Handy JM, Scott AJ, Cross AM, Sinha P, O’Dea KP, Takata M. HLA-DR expression and differential trafficking of monocyte subset following low to intermediate risk surgery. Anaesthesia. 2010;65:27–35.
Wu Z, Kong X, Zhang T, Ye J, Fang Z, Yang X. Pseudoephedrine/ephedrine shows potent anti-inflammatory activity against TNF-α-mrdiated acute liver failure induced by lipopolysaccharide/D-galactosamine. Eur J Pharmacol. 2014;724:112–21.
Acknowledgments
The authors would like to kindly thank Ministry of Science, Education and Sports of the Republic of Croatia for their generous support (Grant number: 219-0000000-3362).
Conflict of interest
The authors declare that there are no actual or potential conflicts of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Tamara Alkhamis and Dubravka Ivić contributed equally to this work.This research was supported by the Ministry of Science, Education and Sports of the Republic of Croatia, Grant number219-0000000-3362.
Rights and permissions
About this article
Cite this article
Alkhamis, T., Ivić, D., Wagner, J. et al. Postoperative immunosuppression markers and the occurrence of sepsis in patients with benign and malignant disease. Wien Klin Wochenschr 126, 774–784 (2014). https://doi.org/10.1007/s00508-014-0613-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-014-0613-6