Abstract
An ecological study and a case-crossover analysis were conducted to evaluate the impact of heat waves on nonaccidental deaths, and to identify contributing factors of population vulnerability to heat-related deaths in Jinan, China. Daily death data and meteorological data were collected for summer months (June to August) of 2012–2013. Excess mortality was calculated and multivariate linear regression models were used to assess the increased risk of heat waves on deaths. Univariate and multivariate logistic regression models were performed to estimate the odd ratios (ORs) of risk factors and their 95 % confidence intervals (CIs). Overall, heat waves were related to 24.88 % excess deaths of total nonaccidental deaths and 31.33 % excess deaths of circulatory diseases, with an OR of 16.07 (95 % CI 8.80–23.33) for total nonaccidental deaths and 12.46 (95 % CI 7.39–17.53) for deaths of circulatory diseases. The case-crossover analysis indicated that older people were more likely to die during heat waves (OR = 1.233, 95 % CI 1.076–1.413) and more deaths occurred outside a hospital during heat waves (OR = 1.142, 95 % CI 1.006–1.296). In conclusion, heat waves have caused excess deaths and significantly increased the risk of circulatory deaths. The risk factors identified in our study have implications for public health interventions to reduce heat-related mortality during extreme heat events.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Extreme heat and heat waves (HW) have caused hundreds of thousands of deaths over the past decades (Macpherson 2014; Steffen et al. 2014; UNISDR 2015). HW can not only cause direct death from heat stroke but also lead to excess deaths of other diseases (e.g., circulatory diseases and respiratory diseases). It has been projected that the frequency, duration, and intensity of HW are likely to increase in the future, which may result in a greater impact on human health (Bittner et al. 2014; Christopher et al. 2014; Steffen et al. 2014). An average of 400 deaths are counted as directly related to heat in the USA each year, with the highest death rates occurring in persons aged 65 years or more (Basu 2009). The global estimate for annual increases in heat-related deaths approximately around 90,000 in 2030 and more than 255,000 in 2050 (Hales et al. 2014).
The effects of HW on human health depend on the characteristics of HW (including intensity, duration, and frequency), exposure access and time to HW and vulnerability of population (Christopher et al. 2014; Lin et al. 2011). Higher mortality risk from HWs was reported in the USA when HWs were more intense, with a longer duration, or occurring earlier in summer times (Anderson and Bell 2011). A study in 66 communities of China (Jinan not included) has suggested that a total of 5.0 % excess deaths might be associated with HW (Ma et al. 2015).
The impacts of HW on deaths vary due to socioeconomic, demographic, and environmental factors, which could influence resilience to HW. Identifying contributing factors of population vulnerability to HW is particularly crucial because it will affect the most disadvantaged populations. Previous studies indicate that some subgroups of different age, gender, and socioeconomic status may be more susceptible to HW than others (Stafoggia et al. 2006; Youngmin and Seunghun 2006; Bouchama et al. 2007; O’Neill et al. 2007; Yu et al. 2010). For example, some studies have found that females might be more vulnerable to HW-related deaths than males (Ishigami et al. 2008; Bell et al. 2008; Sun et al. 2014; Ma et al. 2015), while others have found no differences (Bell et al. 2008; Son et al. 2012). Older people and those who with preexisting circulatory or respiratory diseases may have higher risks of deaths associated with HW or high temperatures (Youngmin and Seunghun 2006; Bouchama et al. 2007; Yu et al. 2010). Given the heterogeneity among these research findings regarding the vulnerability of different age groups, more research is needed to examine the relation between high temperatures and mortality of older population (Hajat et al. 2007; Stafoggia et al. 2006; Ishigami et al. 2008; Basu 2009).
In recent years, the association between HW and deaths has become an issue of interest in China. Several studies have been performed in Guangdong Province (Zeng et al. 2014; Ma et al. 2015), Nanjing (Wu et al. 2013; Chen et al. 2015), and Ningbo (Bai et al. 2014). However, these study sites are all located in subtropical zones of south China. Jinan, being called one of the four “ovens” in northern China (Zhang et al. 2012a), is located in a warm temperature zone. Due to the mountains to the south of the city, Jinan temperature inversions are common and can lead to particularly hot summer days. From 1951 to 2007, the mean annual air temperature has increased significantly with a speed of 0.24 °C/decade, much higher than that of the average global speed of 0.16 °C/decade (Shi et al. 2007; Hu and Song 2012). However, there has been little evidence on the risk of deaths from heat wave and associated contributing factors to the population vulnerability in Jinan. Our study aimed to assess the impact of HW on deaths in Jinan, as well as to identify the associated risk factors, in order to provide evidences for policy and decision-making for the prevention of heat-health in a warming climate.
Materials and methods
Background of Jinan
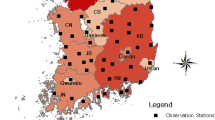
As the capital city of Shandong Province, Jinan is located in the northwestern part of Shandong province at 36° 40′ northern latitude and 116° 57′ east of Greenwich, about 400 km south of Beijing (Fig. 1). Its population was 6.95 million by the end of 2012 and people ≥65 years old accounted for 9.2 %.
Climate description
Jinan has a warm temperate climate with four distinct seasons, very dry spring, hot and humid summer, windy autumn, and cold winter. The average annual temperature is 14.70 °C (58.5 °F) and average total annual rainfall is 670 mm (China Meteorological Administration). Jinan city is surrounded by mountains on its three sides, which leads to poor airflow in the city. In addition, temperature inversions are common and can lead to particular hot and humid summer days. Jinan usually has particularly prolonged heat waves lasting for 105–120 days every year. As a developing urban region in China, Jinan has relatively poor public health facilitations with a higher density of population, lacking a strategic and action plan to respond to extreme heat events. This results in a particularly high population vulnerability to heat in the study area of China, quite different due to situations in developed countries (Basu et al. 2008; Bart et al. 2009).
Data collection
Death data
Daily death data from June to August for 2012 and 2013 were obtained from the Jinan Municipal Center for Disease Control and Prevention (Jinan CDC), which is the data custodian of local death data collection through the National Death Registry Network System. All death information was reported by local medical institutions, including hospitals, community health services, ambulance centers, and village clinics. The death registry data included gender, age, marital status, education level, place of death, date of death, cause of death, and the corresponding ICD-10 codes. Deaths of external causes, such as suicide, poisoning, and traffic accidents (ICD-10:V01-Y89), were excluded from this analysis as no evidence shows an association between HW and increased risk of these deaths. Only nonaccidental deaths (ICD-10:A00-R99) were included in our analysis.
Meteorological data
Daily meteorological data, including daily mean/minimum/maximum temperatures, relative humidity, wind speed, and barometric pressure were collected from the China Meteorological Data Sharing Service System (CMDSSS), compilation quality-controlled global surface observations. Quality control and inspection of the original meteorological data were performed by the CMDSSS, according to a standard protocol to identify and correct outliers and inconsistency in the datasets. This system was operated by the National Meteorological Information Center of Chinese Meteorological Administration, as well as the World Data Center of Meteorology (WDCM) in Beijing. There was only one weather station in Jinan in the dataset, which was used to retrieve the data for the local weather conditions.
Definition of HW
Consistent with the Chinese Meteorological Administration, we defined heat waves as ≥3 consecutive days with daily mean daily maximum temperature exceeding 35 °C. HW should consist of consecutive days with temperatures above a threshold temperature that can either be physiologically based (absolute threshold) or location based (relative threshold) (Robinson 2001). There is no single, universal definition of HW. Different studies have applied various temperature metrics (Chen et al. 2015; Montero et al. 2014).
Case-crossover analysis
The study period was restricted to the summer season (June–August), when HW generally occurred in Jinan. Case-crossover study design, as a special study design of a case–control study, has been applied for the study of transient effect of exposures on the subsequent occurrence of a rare acute-onset disease and commonly used in environmental epidemiology to examine excessive mortality or morbidity related to extreme heat events (Stafoggia et al. 2006; Bell et al. 2008; Zhang et al. 2013). For the case-crossover analysis to identify associated risk factors, deaths from the HW days were chosen as the case group and deaths from the non-HW days of the two summers were chosen as the control group. In order to select an appropriate control group, we have analyzed lagged effect of HW in our study. Using a cross correlation analysis, we detected significantly delayed effects of heat waves for nonaccidental deaths and circulatory diseases in our study, which lasted for 5 and 4 days, respectively. Various lag times have been reported for the strongest association of heat with mortality, ranging from the same day to 3 days following a heat wave (Ma et al. 2015; Son et al. 2012). Based on our analyses of lagged effect, we allowed a 5-day window period in selecting the control period to partially control for the harvesting effect of HW on mortality. The reason for the selection of longer control periods is to get enough cases outside the HW period in order to reach the minimum requirement for the statistical power in comparison. In addition, days of the week were not matched, as the death data did not show a particular pattern over the exposure period.
Excess mortality
The excess mortality was estimated by the difference in daily number of deaths between HW days and non-HW days, illustrated in the following equation (Wu et al. 2013). These models are based on rate difference calculation, which is simple and requires fewer assumptions. They have been widely used for a long period of time for different studies (William et al. 2006).
where EM refers to excess mortality; DHW represents the average number of daily deaths during HW days, while DNH represents the average number of daily deaths during non-HW days.
Data analysis
We firstly quantified the excess deaths due to heat wave and the odds ratios (ORs) of increased risk for total nonaccidental deaths and cause-specific deaths. Then, we conducted a case-crossover analysis to identify associated risk factors of the heat waves for excessive deaths.
To quantify the impact, descriptive analyses were firstly performed to characterize the heat waves, meteorological data, and cause-specific deaths. The excess mortality was then calculated and two-sample t test was used to compare the difference of the average number of total nonaccidental deaths and cause-specific deaths between the HW days and non-HW days. The statistical significance was defined at the 5 % level. Thirdly, multiple linear regression models were developed to analyze the risks of heat waves on the number of deaths. ORs and the 95 % confidence intervals (CIs) were presented as measures of the effects. To identify risk factors, the epidemiological characteristics of individual factors, including gender, age, education level, marital status, the place of death, and the cause of death, were firstly described. The initial selection of included risk factors was based on literature review of previous studies on heat-health associations. There have been other risk factors discussed in previous studies that were not included in our analysis. For example, race and occupation and these data were available in the datasets. However, in terms of race, Han accounted for 99.4 % of the total population. In terms of occupation, it was difficult to be categorized and compared. Univariate logistic regression model was performed to examine the ORs of these factors. Gender was naturally divided into male and females. Age was divided into three groups, 0–64, 65–74, and over 75 years, as in the original data records. There were different groups of education level in 2012 and 2013 datasets. After we merged the datasets, three education levels were generated, including ≤6, 7–12, and ≥13 years. However, the number of those above 13 years of education only accounted for 3.96 % (679/17,216) of the total. Taking into account the requirement for the statistical power in comparison, we merged the education level into two groups, <6 years (illiterate or elementary school level) and ≥6 years (higher education level). Marital status was divided into three groups, including married, unmarried, and widowed/divorced. The place of death was recorded as “in hospital” (death in hospitals, clinics, or emergency rooms of emergency center) and “outside hospital” (all other deaths). The cause of death was coded for circulatory diseases (ICD-10:I00-I99) and for respiratory diseases (ICD-10:J00-J99).Variables with significant differences between the case group and control group (p < 0.05) in the univariate logistic regression model were included in further multivariate conditional logistic regression models.
Multivariate logistic regression models were developed to analyze the risks of heat waves on the number of deaths, which were adopted by previous studies examining heat-health relationships (Ma et al. 2015; Zeng et al. 2014). The dependent variables were coded as zero for the control periods and one for the exposure periods. The independent variables included age, education level, marital status, place of death, and cause of death. OR was used as an estimate of the strength of the association in the logistic regression. Our model could be described as follows:
where βageXage refers to age group, βeduXedu refers to education level, βplaceXplace refers to place of death, and βCVDXCVD refers to death of CVD.
All the analyses were performed with SPSS20 (IBM CorpLtd., Armonk, NY).
Results
Four HWs with a total of 18 HW days were identified from the study period. The characteristics of the HWs are summarized in Table 1. Two HW events occurred in June and July 2012 and two HW events occurred in August 2013. The first HW began on 18 June 2012, lasting for 5 days. The second one sustained from 26 July to 29 July 2012 with the highest maximum temperature 36.9 °C. The third one began on 5 August 2013 and last for 3 days. The fourth one was from 11August to 16August 2013 with a maximum temperature of 38.2 °C. Besides the difference in maximum temperature and duration, the dewpoint temperature for HW#1 event (2012 June 18–2012 June 22) was lower than that of the other three HW events, while similar for HW#2 and HW#3, and the HW#4 had the highest.
The characteristics of cause-specific daily death counts and meteorological data for HW days and non-HW days are summarized in Table 2. A total number of 17,126 death cases were reported during June–August of 2012–2013, of which deaths of circulatory diseases accounted for 54.89 % (9400/17,126) and 6.91 % (1183/17,126) for respiratory diseases. The average daily number of total nonaccidental deaths and deaths due to circulatory diseases during the HW days were significantly higher than that from non-HW days (p < 0.001). There was no significant difference for deaths of respiratory diseases detected. The mean temperature, maximum temperature, minimum temperature, and wind speed during HW days was higher than that during non-HW days (p < 0.05). There was no significant difference for relative humidity and pressure.
The excess mortality varied across HW and for different causes of death (Table 3). The highest excess mortality of total nonaccidental deaths was 32.42 % from HW three and the lowest was 16.67 % from HW four with the total excess mortality was 24.88 %. The total excess mortality from circulatory diseases exceeded 30 % with the highest 44.59 % from HW#2 and the lowest 25.10 % from HW#4. The excess mortality for respiratory diseases in 2013 exceeded 30 %, while those in 2012 were less than zero, particularly −29.58 % for HW#4. The lower humidity in 2012 might contribute to the difference. The lower humidity in 2012 might contribute to the difference. Air quality might be an issue too as air pollution is usually severe in Jinan as a developing city. However, our study cannot address the answer to the decline of the respiratory diseases due to data unavailability. Further studies are required to examine the impact of heat during air pollution.
The multiple linear regression models indicated that HW may lead to more than 16 times increase in the risk for total nonaccidental deaths and almost 13-fold increase in risk of deaths of circulatory diseases (Table 4). There was no increased risk of HW for respiratory deaths.
The ORs from the univariate logistic regression analysis indicates that older people (≥75 and 65–74 years), those widowed/divorced, those with a lower education level (≤6 years), with circulatory diseases and outside hospitals were more likely to die during HW (Table 5).
The conditional logistic regression analysis, as demonstrated in Table 6, confirms that older people were more likely to die during HW (OR = 1.221, 95 % CI 1.064–1.399), and more deaths occurred outside a hospital during HWs (OR = 1.138, 95 % CI 1.003–1.290). No significant difference was detected for education levels marital status and the causes of death.
Discussion
Our study has detected an increased risk of HW on nonaccidental death, which is the first such kind of study conducted in a temperate city in northern China. Consistent with previous studies on heat wave and deaths in Europe, the USA, Australia, and Asia (Ishigami et al. 2008Basu 2009; Anderson and Bell 2011; Son et al. 2012; Steffen et al. 2014; Ma et al. 2015), we have found that heat wave may lead to extra deaths, particularly circulatory deaths, in Jinan city. In addition, our study has also suggested that the following subgroups were at higher risks of dying during heat waves, including75 years and older, a lower education level and preexisting circulatory diseases. Moreover, more people would die outside hospitals in Jinan during HW.
Age has been found to modify the association between HW and mortality. Similar to other studies, the elderly have been found to be at a greater risk of deaths following HW. However, in some studies, persons over age 65 years were found to be at highest risk (Basu et al. 2008; Bell et al. 2008; Ishigami et al. 2008; Hajat et al. 2007; Ma et al. 2015; Zeng et al. 2014), while other studies reported the highest-risk age groups to be even older (Baccini et al. 2008; Ballester et al. 1997). Our study confirms a higher vulnerability to heat waves among old people who are over 75 years of age (Dilaveris et al. 2006; Heat-related mortality-Chicago, July 1995).
There are several reasons to explain why older people are more vulnerable to HW (Youngmin and Seunghun 2006; Ishigami et al. 2008; Yu et al. 2010; Son et al. 2012; Zeng et al. 2014; Ma et al. 2015). The most important physiopathological mechanisms might be the weakening or decreasing of the thermal regulation with aging (Basu and Samet 2002; Basu 2009; Yu et al. 2010). The impairment of thermoregulatory ability can be attributed to the combination of several factors, including reduced sweat gland output, reduced skin blood flow, smaller increase in cardiac output, and less redistribution of blood flow from renal and splanchnic circulations (Bouchama and Knochel 2002; Dufour and Candas 2007; Basu 2009; Kenny et al. 2010; Hansen et al. 2011). Increased blood viscosity, elevated cholesterol levels associated with higher temperatures, and higher sweating thresholds may also trigger heat-related mortality (Basu 2009; Yu et al. 2010). The problem can be more serious for the individuals with cardiovascular, respiratory and renal diseases (StafoggiaM et al. 2008; Yu et al. 2010). In addition, socioeconomic factors, such as low income and lack of air conditioner, might also increase the risks (O’Neill et al. 2005; Youngmin and Seunghun 2006; Basu 2009). These studies imply that a greater number of aging population are vulnerable. The risk of HW will continue to rise in the following decades as the rapid aging trend proceeds in the world and China (Zhang et al. 2012a, b). Therefore, it is urgent and essential to make adaption plans to reduce heat-related burden of disease among the ageing population.
Our findings indicate that more deaths would happen outside hospitals during HW, which has implications for public health policies and practices. Some previous studies report similar findings (Medina-Ramón et al. 2006; Son et al. 2012; Ma et al. 2015). The findings of our study are similar to these studies. The study in 66 communities in China divided the place of death into “in hospital,” including a hospital, clinic or medical center, as well as outpatients admitted to the emergency room, and “outside hospital,” including all other deaths, such as deaths at home (Ma et al. 2015). They found the effects of HW were more pronounced for those dying outside hospitals than those dying in hospital. In the study of seven major cities in Korea, the estimated HW effect for out-of-hospital deaths was found higher than that for in-hospital deaths (Son et al. 2012). A multicity case-only analysis in Italy found those dying outside a hospital were more susceptible to extreme heat (OR = 1.066; 95 % CI 1.036–1.098) (StafoggiaM et al. 2008). Moreover, Stafoggia reported that patients in general medicine were at a higher risk than those in high and intensive care units (StafoggiaM et al. 2008). Dying in a hospital may reflect the difference in socioeconomic status such as health insurance status and access to health care (O’Neill et al. 2007; Son et al. 2012).
People with circulatory disease may be more likely to die during a HW, which is similar to previous studies (Rey et al. 2007; Basu 2009; Ma et al. 2015). Individuals with preexisting cardiac dysfunction have a reduced ability to sufficiently increase their cardiac output to maintain adequate skin blood flow when core temperature is elevated (Kenny et al. 2010). If there is a long-term exposure to an extreme heat event, stress on heart and the other organs can be exacerbated by dehydration (Keatinge et al. 1986; Bouchama and Knochel 2002). This is important from a public health point of view since circulatory diseases are the leading cause of death in Jinan, accounting for 53.43 and 53.76 % of the total deaths in 2012 and 2013, respectively.
The association between a lower education level and HW-related deaths has not been clarified by our analysis. Studies suggested education attainment could be seen as an indicator of socioeconomic position (Wnkleby et al. 1992; O’Neill et al. 2007). A lower education level could be related to poor baseline health status, limited access to health care, and lack of knowledge and adaptive behaviors (O’Neill et al. 2007; Son et al. 2012; Liu et al. 2013).
We have not detected significant difference in deaths between females and males. Some studies reported that females might be more vulnerable to HW-related deaths than males (Ishigami et al. 2008; Bell et al. 2008; Sun et al. 2014; Ma et al. 2015), which might be attributable to physiological differences between genders (D’Ippoliti et al. 2008; Son et al. 2012). However, other studies found that males might be specifically vulnerable for circulatory causes of deaths or no significant difference between genders was detected (Bell et al. 2008; Son et al. 2012). The inconsistency in findings highlights the need to conduct local studies to support evidence-based decision-making.
Several limitations of the study should be acknowledged. Firstly, the study was focused on one city, which may limit the generalization of the research findings. However, the unique summer weather conditions in Jinan provided us an opportunity to study HW-related deaths in temperate zones in north China. Secondly, the data were limited to 2 years, which may affect the adjustments for possible confounding factors in the multivariate models. Thirdly, this study did not account for the mortality displacement effect (harvesting) and interactions between air pollution and high temperature because of data unavailability. The effect of HW on nonaccidental deaths might be overestimated (Basu 2009; Analitis et al. 2014; Iny et al. 2014). Finally, different definitions of HW result in considerable differences in associations between HW and mortality. We did not distinguish different effects of individual heat waves either (Chen et al. 2015).
To the best of our knowledge, this is the first study in north China to comprehensively examine the excess death related to HW, as well as population vulnerability to HW-related deaths. In conclusion, our study shows that HW significantly increases the risks of total nonaccidental deaths and, particularly deaths of circulatory diseases. These findings have important implications for public interventions, particularly to assist the development of surveillance systems and emergency response mechanisms. In addition, more attentions should be paid to the vulnerable subpopulations based on the identified risk factors, such as older people and those with circulatory diseases, and to increase public awareness by health education and health promotion on health risks of HW.
References
Analitis A, Michelozzi P, D’Ippoliti D et al (2014) Effects of heat waves on mortality: effect modification and confounding by air pollutants. Epidemiology 25(1):15–22. doi:10.1097/EDE.0b013e31828ac01b
Anderson GB, Bell ML (2011) Heat waves in the United States: mortality risk during heat waves and effect modification by heat wave characteristics in 43 U.S. communities. Environ Health Perspect 119(2):210–218. doi:10.1289/ehp.1002313
Baccini M, Biggeri A, Accetta G et al (2008) Heat effects on mortality in 15 European cities. Epidemiology 19(5):711–719. doi:10.1097/EDE.0b013e318176bfcd
Bai L, Ding GQ, Gu SH et al (2014) The effects of summer temperature and heat waves on heat-related illness in a coastal city of China,2011-2013. Environ Res 132:212–219. doi:10.1016/j.envres.2014.04.002
Ballester F, Corella D, Perez-Hoyos S et al (1997) Mortality as a function of temperature: a study in Valencia, Spain, 1991–1993. Int J Epidemiol 26(3):551–61. doi:10.1093/ije/26.3.551
Bart D, Lindsey A, Rochelle S et al (2009) Estimating the mortality effect of the July 2006 California heat wave. Environ Res 109(5):614–9
Basu R, Samet JM (2002) Relation between elevated ambient temperature and mortality: a review of the epidemiologic evidence. Epidemiol Rev 24(2):190–202. doi:10.1093/epirev/mxf007
Basu R, Feng WY, Ostro B (2008) Characterizing temperature and mortality in nine California counties, 1999–2003. Epidemiol 19:138–145
Basu R (2009) High ambient temperature and mortality: a review of epidemiologic studies from 2001 to 2008. Environ Heal 8:40–52. doi:10.1186/1476-069X-8-40
Bell ML, O’Neill MS, Ranjit N et al (2008) Vulnerability to heat-related mortality in Latin America: a case-crossover study in Sao Paulo, Brazil, Santiago, Chile and Mexico City, Mexico. Int J Epidemiol 37:796–804. doi:10.1093/ije/dyn094
Bittner MI, Matthies EF, Dalbokova D et al (2014) Are European countries prepared for the next big heat-wave? Eur J Pub Health 24(4):615–619. doi:10.1093/eurpub/ckt121
Bouchama A, Knochel JP (2002) Heat stroke. N Engl J Med 346(25):1978–1988. doi:10.1056/NEJMra011089
Bouchama A, Dehbi M, GamalM MF, ShoukriM MB (2007) Prognostic factors in heat wave-related deaths. A meta analysis. Arch Intern Med 167(20):2170–2176. doi:10.1001/archinte.167.20.ira70009
Chen K, Bi J, Chen J et al (2015) Influence of heat wave definitions to the added effect of heat waves on daily mortality in Nanjing, China. Sci Total Environ 506–507:18–25. doi:10.1016/j.scitotenv.2014.10.092
Christopher BF, Vicente RB, David JD, Katharine JM, Michael DM (2014) Climate change 2014-impacts, adaptation, and vulnerability. Cambridge University Press, New York
Dilaveris P, Synetos A, Giannopoulos G et al (2006) Climate impacts on myocardial infarction deaths in the Athens territory: the climate study. Heart 92(12):1747–1751. doi:10.1136/hrt.2006.091884
D’Ippoliti D, Michelozzi P, Marino C et al (2008) The impact of heat waves on mortality in 9 European cities: results from the EuroHEAT project. Environ Health 19(6):s286–287. doi:10.1097/01.ede.0000340332.18427.d0
Dufour A, Candas V. (2007). Ageing and thermal responses during passive heat exposure: sweating and sensory aspects. Eur J Appl Physiol100(1): 19–26.doi:10.1007/s00421-007-0396-9.
Hajat S, Kovats RS, Lachowycz K (2007) Heat-related and cold-related deaths in England and wales: who is at risk? Occup Environ Med 64:93–100. doi:10.1136/oem.2006.029017
Hales S, Kovats S, Lioyd S et al (2014) Quantitative risk assessment of the effects of climate change on selected causes of death,2030s and 2050s. WHO Press.22, Geneva
Hansen A, Bi P, Nitschke M, et al. (2011). Older persons and heat-susceptibility: the role of health promotion ina changing climate. Health Promotion Journal of Australia22 Special: s17-21.doi:10.1071/HE11417
Heat-related mortality-Chicago, July 1995. MMWR Morb Mortal Wkly Rep 1995; 44: 577–9
Hu G, Song H (2012) Analysis of Air-Temperature Variation Trend and Abrupt Change in Jinan Based on Mann-Kendall Test. J Univ OF JINAN ( Sci and Tech ) 26(1):96–101, in Chinese
Iny J, Fann N, Zanobetti A, Hubbell B (2014) Effect modification of ozone-related mortality risks by temperature in 97 US cities. Environ Int 73:128–134. doi:10.1016/j.envint.2014.07.009
Ishigami A, Hajat S, Kovats RS et al (2008) An ecological time-series study of heat-related mortality in three European cities. Environ Health Perspect 7:5–11. doi:10.1186/1476-069X-7-5
Keatinge WR, Coleshaw SR, Easton JC, et al. (1986). Increased platelet and red cell counts, blood viscosity, and plasma cholesterol levels during heat stress, and mortality from coronary and cerebral thrombosis. Am J Med. 81(795–800).doi:10.1016/0002-9343(86)90348-7
Kenny GP, Yardley J, Brown C et al (2010) Heat stress in older individuals and patients with common chronic diseases. CMAJ 182(10):1053–1060. doi:10.1503/cmaj.081050
Lin Y, Ho T, Wang Y (2011) Mortality risk associated with temperature and prolonged temperature extremes in elderly populations in Taiwan. Environ Res 111:1156–1163
Liu T, Xu YJ, Zhang YH, et al.(2013). Associations between risk perception, spontaneous adaptation behavior to heat waves and heatstroke in Guangdong province, China.BMC Public Health 13(913).doi:10.1186/1471-2458-13-913
Ma WJ, Zen WL, Zhou MG et al (2015) The short term effect of heat waves on mortality and its modifiers in China: An analysis from 66 communities. Environ Int 75:103–109. doi:10.1016/j.envint.2014.11.004
Macpherson CC (2014) Climate change matters. J Med Ethics 40(4):288–90. doi:10.1136/medethics-2012-101084
Medina-Ramón M, Zanobetti A, Cavanagh DP, Schwartz J (2006) Extreme temperatures and mortality: assessing effect modification by personal characteristics and specific cause of death in a multi-city case-only analysis. Environ Health Perspect 114(9):1331–1336. doi:10.1289/ehp.9074
Montero JC, Miron IJ, Criado IJ et al (2014) Difficulties of defining the term, “heat wave”, in public health. Int J Environ Health Res 23(5):377–379. doi:10.1080/09603123.2012.733941
O’Neill MS, Zanobetti A, Schwartz J (2005) Disparities by race in heat-related mortality in four US cities: The role of air conditioning prevalence. J Urban Health 82(2):191–197. doi:10.1093/jurban/jti043
O’Neill MS, Zanobetti A, Schwartz J (2007) Modifiers of the Temperature and Mortality Association in Seven US Cities. Am J Epidemiol 157(12):1074–1082. doi:10.1093/aje/kwg096
Rey G, Jougla E, Fouillet A et al (2007) The impact of major heat waves on all-cause and cause-specific mortality in France from 1971 to 2003. Int Arch Occup Environ Health 80:615–626. doi:10.1007/s00420-007-0173-4
Robinson PJ (2001) On the definition of a heat wave. J ApplMeteorol 40(4):762–775. doi:10.1175/1520-0450(2001)040<0762:OTDOAH>2.0.CO;2
Shi ZB, Dong XG, Shi XW, Ren GZ (2007) Climate characteristic of high temperature weather in Jinan in recent 50a. Meteorol Environ Sci 30:95–97, in Chinese
Son JY, Lee JT, Anderson GB, Bell ML (2012) The impact of heat waves on mortality in seven major cities in Korea. Environ Health Perspect 120:566–71. doi:10.1289/ehp.1103759
Stafoggia M, Francesco F et al (2006) Vulnerability to heat-related mortality: a multicity, population-based, case-crossover analysis. Epidemiology 17(3):315–323. doi:10.1097/01.ede.0000208477.36665.34
StafoggiaM FF et al (2008) Factors affecting in-hospital heat-related mortality: a multi-city case-crossover analysis. J Epidemiol Community Health 62:209–215. doi:10.1136/jech.2007.060715
Steffen W, Hughes L, Perkins S.(2014). Heat waves: hotter, longer, more often. Sydney, Climate Council of Australia Ltd.21-29
Sun XM, Sun Q, Zhou XF et al (2014) Heat wave impact on mortality in Pudong New Area, China in 2013. Sci Total Environ 493:789–794. doi:10.1136/jech.2007.060715
UNISDR (United Nations Office for Disaster Risk Reduction). (2015). The human cost of weather related disasters. Available http://www.unisdr.org/archive/46793.
William W, Thompson L, Lorraine C (2006) Epidemiology of seasonal influenza: use of surveillance data and statistical models to estimate the burden of disease. JID 194(Suppl 2):82–91. doi:10.1086/507558
Wnkleby MA, Jatulis DE, Frank E, Fortmann SP (1992) Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health 82(6):816–820. doi:10.2105/AJPH.82.6.816
Wu F, Jing YS, Li XY et al (2013) Effect of heat wave on the death-toll of cardiovascular diseases in Nanjing area. J EnvironHygiene 3(4):288–292, in Chinese
Youngmin K, Seunghun J (2006) A vulnerability study of the low-income elderly in the context of high temperature and mortality in Seoul, Korea. Science of the Total Environment 371:82–88. doi:10.1016/j.scitotenv.2006.08.014
Yu WW, Vaneckova P, Mengersen K et al (2010) Is the association between temperature and mortality modified by age, gender and socio-economic status? Sci Total Environ 408:3513–3518. doi:10.1016/j.scitotenv.2010.04.058
Zeng WL, Lao XQ, Rutherford S et al (2014) The effect of heat waves on mortality and effect modifiers in four communities of Guangdong Province, China. Sci Total Environ 482(483):214–221. doi:10.1016/j.scitotenv.2014.02.049
Zhang Y, Bi P, Sun Y et al (2012a) Projected Years Lost due to Disabilities (YLDs) for bacillary dysentery related to increased temperature in temperate and subtropical cities of China. J Environ Monit 14(2):510–516
Zhang NJ, Guo M, Zheng XY (2012b) China: awakening giant developing solutions to population aging. The Gerontol 57(5):589–596. doi:10.1093/geront/gns105, in Chinese
Zhang Y, Nitshke M, Bi P (2013) Risk factors for direct heat-related hospitalization during the 2009 Adelaide heat wave: a case crossover study. Sci Total Environ 442:1–5. doi:10.1016/j.scitotenv.2012.10.042
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Zhang, J., Liu, S., Han, J. et al. Impact of heat waves on nonaccidental deaths in Jinan, China, and associated risk factors. Int J Biometeorol 60, 1367–1375 (2016). https://doi.org/10.1007/s00484-015-1130-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00484-015-1130-7