Abstract
Understanding how weather impacts health is critical, especially under a changing climate; however, relatively few studies have investigated subtropical regions. We examined how mortality in São Paulo, Brazil, is affected by cold, heat, and heat waves over 14.5 years (1996–2010). We used over-dispersed generalized linear modeling to estimate heat- and cold-related mortality, and Bayesian hierarchical modeling to estimate overall effects and modification by heat wave characteristics (intensity, duration, and timing in season). Stratified analyses were performed by cause of death and individual characteristics (sex, age, education, marital status, and place of death). Cold effects on mortality appeared higher than heat effects in this subtropical city with moderate climatic conditions. Heat was associated with respiratory mortality and cold with cardiovascular mortality. Risk of total mortality was 6.1 % (95 % confidence interval 4.7, 7.6 %) higher at the 99th percentile of temperature than the 90th percentile (heat effect) and 8.6 % (6.2, 11.1 %) higher at the 1st compared to the 10th percentile (cold effect). Risks were higher for females and those with no education for heat effect, and males for cold effect. Older persons, widows, and non-hospital deaths had higher mortality risks for heat and cold. Mortality during heat waves was higher than on non-heat wave days for total, cardiovascular, and respiratory mortality. Our findings indicate that mortality in São Paulo is associated with both cold and heat and that some subpopulations are more vulnerable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
São Paulo, the largest city in Latin America, is experiencing a variety of consequences from a changing climate such as heavy rainfall, high temperatures, and local differences in weather patterns. Efforts have been made to mitigate the increased health impacts of climate change in several Brazilian cities including São Paulo. Some governmental interventions include monitoring and reduction of greenhouse gas emissions, and establishing adaptation plans and mitigation actions (Barbi and Ferreira 2013). However, more locally based scientific evidence is needed to develop specific intervention strategies for particularly vulnerable populations and to effectively target at-risk groups. More extreme temperature is one of the most direct pathways through which climate change is likely to impact public health in São Paulo. In particular, more research is needed on how weather affects health in subtropical climates, such as São Paulo.
Health risks from high and low temperatures are expected to increase as climate change brings more frequent and extreme conditions (Peng et al. 2011; Hajat et al. 2014; Bassil et al. 2011). Numerous studies have reported impacts of temperature on health, particularly mortality (Lin et al. 2011; Curriero et al. 2002; Son et al. 2011, 2014; Monteiro et al. 2013; Basu 2009; Anderson and Bell 2009; Xu et al. 2014; Yi and Chan 2014), although most research was conducted for North America or Europe. Far less is known regarding impacts of temperature on mortality in some other regions of the world, especially in urban populations of countries with emerging economies. Effects of temperature on mortality can differ substantially by location and population, such as higher heat effects on mortality in cooler climates of the USA (Curriero et al. 2002; Anderson and Bell 2009) and higher associations for heat-related mortality in areas with a larger fraction of older buildings and manual workers (Xu et al. 2013). A study of 12 urban cities in countries with emerging economies, including São Paulo, Brazil, showed a wide variety of non-linear temperature-mortality relationships, with a range of temperature thresholds for heat- or cold-related deaths (McMichael et al. 2008). Moreover, some studies suggest that vulnerability to weather differs substantially by location and population. More work on temperature-health relationships is needed for rapidly developing urban centers, as the world’s population is estimated to be 70 % urban by 2050, largely through unmanaged development (WHO 2013).
In Latin America and the Caribbean, 79 % of the population live in urban settings (World Bank 2014), with over 20 million in the area of São Paulo, the largest city in Latin America and one of the 10 most populated cities in the world (Demographia 2014). To date, relatively few studies have been performed for São Paulo to assess impacts of temperature on health, although some work has been conducted (McMichael et al. 2008; Hajat et al. 2005; Bell et al. 2008; Sharovsky et al. 2004). Higher effects were observed for cardiovascular mortality for cold stress than heat stress (1996–2000) (Gonçalves et al. 2007). Another study (1991–1994) found little evidence for modification of heat or cold effects by area-level socioeconomic status (Gouveia et al. 2003).
Previous studies for São Paulo considered single days of high temperature, although prolonged periods of extreme heat (heat waves) can have higher risk than the summed risks of single days of high temperatures (Anderson and Bell 2009; Hajat et al. 2006). The impact of heat waves on health is likely to increase under climate change as heat waves are expected to be longer in duration, occur earlier in the warm season, and be more intense (i.e., hotter) (Meehl and Tebaldi 2004). Further, earlier studies have shown that heat waves differ in their association with health, based on heat wave characteristics (Anderson and Bell 2011; Son et al. 2012). Several mechanisms such as dyspnea, dehydration from lack of nightly cooling, and longer duration of heat may contribute to risk differences between heat waves and single days of heat (Schifano et al. 2009).
We investigated mortality effects of heat, cold, and heat waves in São Paulo for a 14.5-year period (1996–2010) and improved on earlier studies by considering (1) impacts of heat waves in addition to single days of heat, (2) differences in effects by heat wave characteristics (intensity, duration, and timing in season), (3) susceptibility based on individual characteristics (sex, age, education, marital status, and place of death), and (4) a much longer study time frame (over 14 years, May 1996 to December 2010) compared with previous work using 3–5 years of data. To our knowledge, this is the first study to estimate the health impacts of heat waves or effect modification by heat wave characteristics in São Paulo and is the most comprehensive study of weather and health in São Paulo to date.
Material and methods
Data
Daily mortality counts for São Paulo municipality (May 1, 1996 to December 31, 2010) were obtained from the city’s mortality information system (PRO-AIM). Data included date and cause of death, sex, age, education, marital status (single, married/living together, widow, or divorced), and place of death (in or out of hospital). We considered total mortality as all causes of death except external causes (International Classification of Diseases, ICD-10; World Health Organization 2007, A00-R99), cardiovascular mortality (ICD-10, I00-I99), and respiratory mortality (ICD-10, J00-J99). Educational level and marital status were assessed for those ≥21 years. Due to the use of existing health data, formal consent is not required.
Weather data (ambient temperature and relative humidity) were acquired from the State of São Paulo’s environmental regulatory agency, the Companhia Ambiental do Estado de São Paulo (CETESB). We calculated 24-h averages by first averaging hourly values across all monitors within São Paulo municipality for each day and then calculating 24-h values. The number of monitors in a given year ranged from 2 to 5 (average 3.0) for temperature and from 1 to 5 (average 3.1) for relative humidity. Although a variety of temperature metrics have been used in studies of weather and health, we used daily mean temperature as this variable has been used previously (Gouveia et al. 2003), which aids comparability to earlier work, and temperature metrics are highly correlated (e.g., correlation of daily 1-h max and daily 24-h average for a given monitor: average 0.90, range 0.88–0.93).
Air pollution was considered as a potential confounder. Hourly concentrations for particulate matter with aerodynamic diameter ≤10 μm (PM10) and ozone were obtained from CETESB. Fine particles (PM2.5) were not measured. We calculated 24-h averages for PM10, by first averaging hourly values across all monitors throughout the municipality for each day and then calculating 24-h values. For ozone, we calculated the maximum daily 8-h moving average. The number of monitors varied by year, averaging 12.7 for PM10 (range 11–14 for a given year) and 7.7 for ozone (range 6–10).
Statistical analysis
We estimated non-linear associations between temperature and mortality using over-dispersed Poisson generalized linear modeling:
where E(Y t) = expected number of deaths on day t; β0 = model intercept, DOW t = categorical variable for day of the week; ns(time t) = natural cubic spline of a variable representing time to adjust for long-term trends, with 6 degrees of freedom (df) per year; ns(T t-lag) = natural cubic spline of temperature for a specific lag from day t (df = 3, with equally spaced knots); and ns(humidity) = natural cubic spline of humidity on day t (df = 4).
Using these results, we created estimates of the non-linear relationship between temperature and risk of mortality. We also estimated heat- and cold-related temperature effects for specific portions of the temperature-mortality response curve. For heat effects, we calculated change in mortality risk at mean daily temperatures of 24.1 to 20.4 °C (90th to 50th percentiles) and 26.2 to 24.1 °C (99th to 90th percentiles). For the cold effect, we compared mortality risk at 16.5 to 20.5 °C (10th to 50th percentiles) and 14.3 to 16.5 °C (1st to 10th percentiles).
Previous work demonstrated that cold effects occur up to several weeks after exposure whereas heat effects have more immediate responses (Gouveia et al. 2003). We estimated heat-related mortality based on the same and previous days of temperature (lag 0–1) and cold-related mortality based on longer time periods (lag 0–20). For sensitivity analysis, we considered multiple lag structures of the same day (lag 0) and the average of the same and up to 30 previous days based on earlier work (Basu 2009; Xu et al. 2014). We assessed potential confounding by pollution (PM10 and ozone) by including a variable for each air pollutant, individually and simultaneously, in the model at lag 0 based on previous work (Bell et al. 2008).
Analysis of heat waves was restricted to the warm season (September–March). There exists no standard definition for a heat wave, although definitions generally combine requirements for duration and intensity (Anderson and Bell 2009; Anderson et al. 2013). We defined a heat wave as ≥2 consecutive days with daily mean temperatures ≥96th percentile warm season temperature. Heat wave effects were estimated as the change in mortality risk comparing heat wave and non-heat-wave days. We estimated the added heat wave effect for each heat wave using generalized linear modeling and then used Bayesian hierarchical modeling to generate an overall effect. We controlled for daily mean temperature, day of the week, relative humidity, and temporal trends. This estimates the association between heat waves and mortality, beyond the effects of individual days of heat.
To estimate how estimates were affected by heat wave characteristics (intensity, duration, and timing in season), we applied Bayesian hierarchical modeling, with a separate model for each characteristic (Anderson and Bell 2011; Son et al. 2012). Sensitivity analyses were conducted using different definitions of heat waves for intensity. We examined timing in season by comparing mortality risk for the first heat wave of the season to later heat waves.
We applied stratified models by cause of death (total, cardiovascular, and respiratory mortality), sex, age, educational level, marital status, and place of death. All analyses were conducted using R 2.10.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Supplemental Table S1 shows summary statistics for mortality, weather, and air pollution. The mean number of deaths per day was 174.3, 63.5, and 22.0 for total, cardiovascular, and respiratory causes, respectively. Daily temperature averaged 20.1 °C (range 7.5–28.7 °C). The distribution of study population characteristics is provided in Supplemental Table S2. A total of 933,954 deaths for all non-accidental causes were included in the analysis. More deaths occurred in those 15–64 and ≥75 years, those with a primary education, and persons married or living together than in other groups. Most deaths occurred in hospitals (84.7 %).
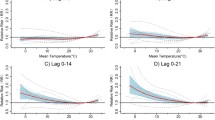
We evaluated multiple lag structures by calculating the heat (99th vs. 90th percentile) and cold effects (1st vs. 10th percentile) for lag0-1 to lag0-30 (Supplemental Fig. S1). Heat effects were most pronounced for short-term exposures, whereas cold effects persisted for longer lag times. For subsequent analysis, we chose lag 0–1 for heat effect and lag 0–20 for cold effect.
Temperature-mortality response curves (Fig. 1 and Supplemental Fig. S2) show higher heat effects for respiratory mortality and higher cold effects for cardiovascular mortality. The heat effect for total mortality was a 5.4 % (95 % confidence interval 4.8, 6.1 %) increase in mortality comparing the 90th and 50th percentiles of temperatures and 6.1 % (4.7, 7.6 %) comparing the 99th and 90th percentiles. Heat effects for respiratory mortality were higher than for cardiovascular mortality (Table 1). The increase in total mortality for the cold effect was 12.2 % (10.9, 13.5 %) comparing the 10th and 50th percentiles of temperature and 8.6 % (6.2, 11.1 %) comparing the 1st and 10th percentiles. The cold effect for cardiovascular mortality was higher than for respiratory or total mortality (Table 1). Both heat and cold effects remained after inclusion of pollution variables (PM10 and ozone) (Tables 1 and 2).
Relationship between temperature and risk of total mortality, comparing various temperature levels with a reference temperature of 20.5 °C. Note: Lag 0–1 days for heat effect; lag 0–20 days for cold effect. The shaded portions of the curves represent 95 % confidence intervals. The bars represent the ranges of the curves measured as heat effects (dark yellow: 99th–90th percentile; light yellow: 90th–50th percentile) and cold effects (dark gray: 1st–10th percentile; light gray: 10th–50th percentile) (Color figure online)
We investigated effect modification of the temperature-mortality relationship by sex, age, educational level, marital status, and place of death (Fig. 2 and Supplemental Tables S3 and S4). Heat effects (comparing 90th and 50th percentiles of temperature) were 1.7 % (95 % confidence interval (CI) 0.5, 3.0 %) higher for females than for males. For the heat effect (comparing 99th and 90th percentiles), those ≥75 years had 7.1 % (1.4, 13.1 %) higher risk than those 0–14 years. For cold effect (comparing 1st and 10th percentiles), the oldest age group had 13.2 % (3.5, 23.8 %) higher risk than the youngest group. For heat-related mortality, highest effect estimates were observed for those with no education. Trends by education were not observed for cold effects. Central estimates for both heat and cold effects were highest for widows and lowest for divorced persons. Heat and cold effects were higher for out-of-hospital than in-hospital deaths (Fig. 2). For cold effects (comparing 10th and 50th percentiles), risks were 7.3 % (4.1, 10.6 %) higher for out-of-hospital than in-hospital deaths.
Percentage change in total mortality risk for a heat (comparison of 99th vs. 90th percentile of mean temperature) and b cold (comparison of 1st vs. 10th percentile of mean temperature) by sex, age, education, marital status, and place of death in São Paulo. Note: The points represent the central estimates, and the vertical lines represent 95 % confidence intervals. Lag0-1 for heat effect; lag0-20 for cold effect
For our heat wave definition based on temperatures ≥96th percentile (25.6 °C) for ≥2 days, 27 heat waves occurred in the study period (average 1.8 heat waves/year) (Fig. 3 and Supplemental Table S5). The intensity ranged from 25.7 to 27.1 °C and the duration ranged from 2 to 5 days. Total mortality was 5.8 % higher (95 % CI 2.3, 9.3 %) on heat wave days compared to that on non-heat-wave days (Supplemental Table S6). The heat wave effect was highest for respiratory mortality (10.8 %, 95 % CI 2.8, 19.3 %). We did not observe statistically significant evidence of effect modification of heat wave effects by individual characteristics, although estimates generally increased with age, with the highest effect for those ≥75 years (Supplemental Table S7). Trends in heat wave effects by educational level were not observed, with the highest effect for those with university education. Associations remained using alternative heat wave definitions with different intensities (Supplemental Table S8), with higher risk from heat waves with higher intensity.
Percentage change in total mortality risk for heat wave effect by sex, age, education, marital status, and place of death in São Paulo. Note: The points represent the central estimates, and the vertical lines represent 95 % confidence intervals. Heat wave effects were estimated based on the heat wave definition of temperatures ≥96th percentile for ≥2 days. In refers to in-hospital deaths. Out refers to out-of-hospital deaths
For total, cardiovascular, and respiratory mortality, findings suggest higher mortality risk from heat waves with higher intensity and longer duration, although results were not statistically different (Supplemental Table S9). The first heat wave of the warm season had a higher total mortality estimate (6.2 %, 95 % CI −0.5, 13.3 %) than did later heat waves (5.4 %, 95 % CI 1.0, 10.1 %), although results were not statistically different. We found similar results for cardiovascular and respiratory mortality (Supplemental Table S10).
Discussion
Although many studies have documented a non-linear relationship between temperature and mortality, results vary across studies, including for the effects based on cause of mortality (Barnett 2007; Goodman et al. 2004). A study of California reported elevated risks for cardiovascular diseases compared to respiratory diseases from ambient temperature (Basu and Ostro 2008). Stronger heat effects were observed for respiratory mortality than all-cause mortality in three European cities (Ishigami et al. 2008). Medina-Ramón et al. (2006) found higher mortality risk from extreme cold for cardiovascular deaths, especially cardiac arrest, compared to other causes. Other studies also showed greater risks for several cause-specific outcomes such as myocardial infarction, cerebrovascular disease, chronic obstructive pulmonary disease, and diabetes (Medina-Ramón et al. 2006; Braga et al. 2002; Stafoggia et al. 2006). We found higher heat effects for respiratory mortality and higher cold effects for cardiovascular mortality. Possible mechanisms for higher heat effect for respiratory mortality include vascular changes leading to cardiovascular effects, or airway and systemic inflammation that may trigger a respiratory distress syndrome (Michelozzi et al. 2009). Some studies reported that cold specifically affects the cardiovascular system, causing fluctuations of blood pressure, vasoconstriction, hematological changes like increased platelet, red cell counts, blood viscosity, and plasma cholesterol, and fibrinogen (Keatinge and Donaldson 1995; Huynen et al. 2001).
We found that cold effects on mortality appeared higher than heat effects in São Paulo, a subtropical city with moderate climatic conditions. Although comparison of results across studies is challenging due to different choices for presentation of results for “heat” or “cold effects,” our finding is broadly consistent with previous results from the USA and elsewhere (Curriero et al. 2002; Anderson and Bell 2009; Gouveia et al. 2003; Zanobetti and Schwartz 2008). Mortality was not associated with high temperatures in Kerman, Iran, which could be explained by acclimatization to high temperatures in the desert climate (Khanjani and Bahrampour 2013). Cold was associated with higher risk of cardiovascular mortality than heat in Taiwanese subtropical areas (Lin et al. 2013). In the USA, heat effects appeared to be larger in the colder northern cities than in warmer southern cities (Anderson and Bell 2009; Zanobetti and Schwartz 2008). Findings support the hypothesis that populations in warmer climates are more adapted to high temperature and more vulnerable to cold. Adaptation may relate to physiological changes, behavior patterns, air conditioning, building characteristics, etc.
An increase in average temperature in winter due to climate change could result in a reduction of cold-related mortality during winter. Whereas the impacts of heat occur relatively quickly, on the same day or subsequent days, the adverse effects of cold weather include direct effects (e.g., hypothermia) and indirect effects (e.g., influenza and respiratory illnesses). Cold-related mortality occurs in regions of mild climate, as well as colder regions. A study in the USA estimated that due to climate change, winter mortality will decrease slightly but this lowered mortality will not offset the greater increase in summer mortality (Kalkstein and Greene 1997).
In this study, the heat effect was highest on the current and previous days (lag 0–1), whereas cold effects persisted for longer periods (lag 0–20). This finding is similar with previous studies reporting risk from acute exposure, such as same day and a few days earlier, for heat-related mortality, and that the association between cold and mortality persisted for up to a few weeks (Braga et al. 2002; Lin et al. 2013).
With adjustment for PM10 and/or ozone, both heat and cold effects were similar, in some cases slightly reduced, and remained positive and significant. Previous findings on confounding and/or effect modification by air pollutants on the temperature-mortality association vary by study. Some studies reported that PM10 or ozone significantly modified the effect of temperature on mortality (O'Neill et al. 2005a); however, others reported no confounding effect (Zanobetti and Schwartz 2008; Basu et al. 2008).
We found suggestive evidence of susceptible populations such as females for heat effect and males for cold effect. Previous findings for modification by sex remain mixed. Many studies reported that women in various locations had higher risk for temperature-related mortality than men (Son et al. 2011; Stafoggia et al. 2006); others found men to be at higher risk (McMichael et al. 2008), and some studies reported no differences by sex (Basu and Ostro 2008).
For both heat- and cold-related effects, older persons had higher risk, with trends in increasing risk with older age and the highest risk for those ≥75 years. Most previous studies consistently reported a greater risk for the elderly (Son et al. 2011).
Previous studies reported higher heat-related mortality risk for those with lower or no education (Son et al. 2011), persons living in lower-income areas (Stafoggia et al. 2006), and those that lack air conditioning (O'Neill et al. 2005b). However, some studies reported no differences by educational level (Basu and Ostro 2008). A study of São Paulo over a shorter time frame (4 years compared to 14.5 years for this study) found little evidence for modification of mortality effects of heat or cold by area-level socioeconomic position (Gouveia et al. 2003). Our findings suggest that the heat effect is highest for those with no education. Some studies reported the highest heat-related mortality for the most educated in Mexico City (Bell et al. 2008) and South Korea (Son et al. 2011), which corresponds to some findings for the cold effect in our study. Although we used individual-level data, socioeconomic status is more complex than the single indicators often used (e.g., education), and vulnerability by socioeconomic status may differ by location, type of health outcomes, and factors such as population characteristics and exposure patterns. Thus, more studies covering various locations and measures of socioeconomic position are needed.
Our results that heat- and cold-related mortality is higher for widowed persons and deaths occurring outside a hospital are consistent with previous studies. We also found a higher effect from heat wave for out-of-hospital than in-hospital deaths although results were not statistically different. As most death occurred in hospital (about 85 %) and there was a relatively small number of heat waves (27 heat waves occurred in the study period, average 1.8 heat waves/year) compared with other studies, we have a limited ability to investigate the difference between groups. A study in four Italian cities reported higher heat-related mortality for widows and widowers (Stafoggia et al. 2006). Many studies identified place of death as the strongest effect modifier to extreme temperature risks (Son et al. 2011; Basu and Ostro 2008; Medina-Ramón et al. 2006). Those who are widowed may be at higher risk due to related patterns of older age and socioeconomic status. Those who are not hospitalized may be more likely to experience extreme ambient temperature conditions.
Only a limited number of studies have investigated temperature-related mortality in São Paulo, and no previous study estimated the effects of heat waves or effect modification by heat wave characteristics in this region. Our findings indicated mortality effects for heat waves, beyond the effects of single days of heat. Estimated impacts were higher with heat waves of higher intensity and longer duration. Previous studies in other locations reported that the intensity, duration, and timing in season of heat waves may affect mortality risks (Anderson and Bell 2009, 2011; Son et al. 2012). Consistent with studies elsewhere (Anderson and Bell 2011; Son et al. 2012), our findings suggest higher effects for the first heat wave of the warm season compared to later heat waves, although results were not statistically different. This finding could result from adaptation through physiological and/or behavioral changes and could relate to changes in the underlying population where those at the greatest risk succumb during the first heat wave event of a season.
Higher temperatures, and therefore heat effect, may be more severe in urban than in rural areas due to the heat island effect from lowered evaporative cooling and greater heat retention caused by increased impervious cover and lowered vegetation cover (Patz et al. 2005). Most cities including São Paulo show a greater heat island effect such as increased rate of infectious disease and much higher mortality during heat waves enhanced by the urban heat island (Araujo et al. 2015; Tan et al. 2010). Urbanization is increasing rapidly worldwide (Allender et al. 2011), which could exacerbate the health impacts of heat in the future. Further, higher overall temperatures and more temperature extremes are anticipated due to climate change (Hajat et al. 2014; Peng et al. 2011). Studies of projected heat waves and health under climate change could potentially result in substantial health effects in the future (Peng et al. 2011; Patz et al. 2005).
Our results may benefit decision makers who design and implement interventions to attenuate the health impacts of extreme weather. Our findings on subpopulation may contribute to the planning of prevention efforts for individuals who are vulnerable (e.g., elderly, people who lack social networks, and people with low socioeconomic status). Our findings are particularly important for São Paulo, as environmental health policies for weather-related health are most effective when region-specific. Efforts such as heat wave warning systems, media announcement, and surveillance systems of morbidity and chronic patients can be developed to protect public health from extreme weather, and such policies need scientific evidence; thus, more research is needed in other locations. Our findings can also inform future studies of how climate change could impact human health.
Conclusions
Our findings provide evidence that both high and low ambient temperatures are associated with mortality risk in São Paulo. Although this study region is subtropical with moderate climate conditions, mortality was associated with cold, and in fact the cold effect is higher than the heat effect. Our findings add information on how temperature-mortality associations and vulnerability differ by location and population. Results also can aid decision makers from subtropical regions regarding measures to protect public health and target subpopulations from extreme heat and cold in the present day and under climate change.
References
Allender S, Wickramasinghe K, Goldacre M, Matthews D, Katulanda P (2011) Quantifying urbanization as a risk factor for noncommunicable disease. J Urban Health 88(5):906–918
Anderson BG, Bell ML (2009) Weather-related mortality. how heat, cold and heat waves affect mortality in the United States. Epidemiology 20:205–213
Anderson GB, Bell ML (2011) Heat waves in the United States: mortality risk during heat waves and effect modification by heat wave characteristics in 43 U.S. communities. Environ Health Perspect 119:210–218
Anderson GB, Bell ML, Peng RD (2013) Methods to calculate the heat index as an exposure metric in environmental health research. Environ Health Perspect 121:1111–1119
Araujo RV, Albertini MR, Costa-da-Silva AL, Suesdek L, Franceschi NC, Bastos NM, Katz G, Cardoso VA, Castro BC, Capurro ML, Allegro VL (2015) São Paulo urban heat islands have a higher incidence of dengue than other urban areas. Braz J Infect Dis 19(2):146–155
Barbi F, da Costa FL (2013) Climate change in Brazilian Cities: policy strategies and responses to global warming. Int J Environ Sci Dev 4(1):49–51
Barnett AG (2007) Temperature and cardiovascular deaths in the US elderly: changes over time. Epidemiology 18:369–372
Bassil KL, Cole DC, Moineddin R, Lou W, Craig AM, Schwartz B, Rea E (2011) The relationship between temperature and ambulance response calls for heat-related illness in Toronto, Ontario, 2005. J Epidemiol Community Health 65(9):829–831
Basu R (2009) High ambient temperature and mortality: a review of epidemiologic studies from 2001 to 2008. Environ Heal 8:40–52
Basu R, Ostro BD (2008) A multicounty analysis identifying the populations vulnerable to mortality associated with high ambient temperature in California. Am J Epidemiol 168:632–637
Basu R, Feng WY, Ostro BD (2008) Characterizing temperature and mortality in nine California counties. Epidemiology 19:138–145
Bell ML, O'Neill MS, Ranjit N, Borja-Aburto VH, Cifuentes LA, Gouveia NC (2008) Vulnerability to heat-related mortality in Latin America: a case-crossover study in São Paulo, Brazil, Santiago, Chile and Mexico City, Mexico. Int J Epidemiol 37:796–804
Braga AL, Zanobetti A, Schwartz J (2002) The effect of weather on respiratory and cardiovascular deaths in 12 U.S. cities. Environ Health Perspect 110:859–863
Curriero FC, Heiner KS, Samet JM, Zeger SL, Strug L, Patz JA (2002) Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol 155:80–87
Demographia (2014) Demographia world urban areas. Demographia, Belleville
Gonçalves FL, Braun S, Dias PL, Sharovsky R (2007) Influences of the weather and air pollutants on cardiovascular disease in the metropolitan area of São Paulo. Environ Res 104:275–281
Goodman PG, Dockery DW, Clancy L (2004) Cause-specific mortality and the extended effects of particulate pollution and temperature exposure. Environ Health Perspect 112:179–185
Gouveia N, Hajat S, Armstrong B (2003) Socioeconomic differentials in the temperature-mortality relationship in São Paulo, Brazil. Int J Epidemiol 32:390–397
Hajat S, Armstrong BG, Gouveia N, Wilkinson P (2005) Mortality displacement of heat-related deaths: a comparison of Delhi, São Paulo, and London. Epidemiology 16:613–620
Hajat S, Armstrong B, Baccini M et al (2006) Impact of high temperatures on mortality: is there an added heat wave effect? Epidemiology 17(6):632–638
Hajat S, Vardoulakis S, Heaviside C, Eggen B (2014) Climate change effects on human health: projections of temperature-related mortality for the UK during the 2020s, 2050s, and 2080s. J Epidemiol Community Health 68(7):641–648
Huynen MM, Martents P, Schram D, Weijenberg MP, Kunst AE (2001) The impact of heat waves and cold spells on mortality rates in the Dutch Population. Environ Health Perspect 109:463–470
Ishigami A, Hajat S, Kovats RS et al (2008) An ecological time-series study of heat-related mortality in three European cities. Environ Heal 7:5–11
Kalkstein LS, Greene JS (1997) An evaluation of climate/mortality relationships in large U.S. cities and the possible impacts of a climate change. Environ Health Prespect 105:84–93
Keatinge WR, Donaldson GC (1995) Cardiovascular mortality in winter. Artic Med Res 54(Suppl 2):16–18
Khanjani N, Bahrampour A (2013) Temperature and cardiovascular and respiratory mortality in desert climate. a case study of Kerman, Iran. Iran J Environ Health Sci Eng 10:11–16
Lin YK, Ho TJ, Wang YC (2011) Mortality risk associated with temperature and prolonged temperature extremes in elderly populations in Taiwan. Environ Res 111:1156–1163
Lin Y.K., Chang C.K., Wang Y.C., Ho T.J. (2013) Acute and prolonged adverse effects of temperature on mortality from cardiovascular diseases. e82678
McMichael AJ, Wilkinson P, Kovats RS et al (2008) International study of temperature, heat and urban mortality: the 'ISOTHURM' project. Int J Epidemiol 37:1121–1131
Medina-Ramón M, Zanobetti A, Cavanagh DP, Schwartz J (2006) Extreme temperatures and mortality: assessing effect modification by personal characteristics and specific cause of death in a multi-city case-only analysis. Environ Health Perspect 114:1331–1336
Meehl GA, Tebaldi C (2004) More intense, more frequent, and longer lasting heat waves in the 21st century. Science 305(5686):994–997
Michelozzi P, Accetta G, De Sario M et al (2009) High temperature and hospitalizations for cardiovascular and respiratory causes in 12 European cities. Am J Respir Crit Care Med 179:383–389
Monteiro A, Carvalho V, Oliveira T, Sousa C (2013) Excess mortality and morbidity during the July 2006 heat wave in Porto, Portugal. Int J Biometeorol 57:155–167
O'Neill MS, Hajat S, Zanobetti A, Ramirez-Aguilar M, Schwartz J (2005a) Impact of control for air pollution and respiratory epidemics on the estimated associations of temperature and daily mortality. Int J Biometeorol 50:121–129
O'Neill MS, Zanobetti A, Schwartz J (2005b) Disparities by race in heat related mortality in four US cities: the role of air conditioning prevalence. J Urban Health 82:191–197
Patz JA, Campbell-Lendrum D, Holloway T, Foley JA (2005) Impact of regional climate change on human health. Nature 438(7066):310–317
Peng RD, Bobb JF, Tebaldi C, McDaniel L, Bell ML, Dominici F (2011) Toward a quantitative estimate of future heat wave mortality under global climate change. Environ Health Perspect 119:701–706
Schifano P, Cappai G, De Sario M et al (2009) Susceptibility to heat wave-related mortality: a follow-up study of a cohort of elderly in Rome. Environ Heal 8:50–63
Sharovsky R, César LA, Ramires JA (2004) Temperature, air pollution, and mortality from myocardial infarction in São Paulo, Brazil. Braz J Med Biol Res 37:1651–1657
Son JY, Lee JT, Anderson GB, Bell ML (2011) Vulnerability to temperature-related mortality in Seoul, Korea. Environ Res Lett 6:034027
Son JY, Lee JT, Anderson GB, Bell ML (2012) The impact of heat waves on mortality in seven major cities in Korea. Environ Health Perspect 120:566–571
Son J.Y., Bell M.L., Lee, J.T. (2014) The impact of heat, cold, and heat waves in hospital admissions in eight cities in Korea. Int J Biometeorol. Epub ahead of print
Stafoggia M, Forastiere F, Agostini D et al (2006) Vulnerability to heat-related mortality: a multicity, population-based, case-crossover analysis. Epidemiology 17:315–323
Tan J, Zheng Y, Tang X, Guo C, Li L, Song G, Zhen X, Yuan D, Kalkstein AJ, Li F (2010) The urban heat island and its impact on heat waves and human health in Shanghai. Int J Biometeorol 54(1):75–84
WHO Centre for Health Development (2013) WHO Center for Health Development Annual Report 2013. Chuo-ku, Kobe: WHO
World Bank. (2014). http://www.data.worldbank.org. Accessed May 21, 2014
Xu Y, Dadvand P, Barrera-Gomez J, Sartini C, Mari-Dell-Olmo M, Borrell C, Medina-Ramon M, Sunyer J, Basagana X (2013) Differences on the effect of heat waves on mortality by sociodemographic and urban landscape characteristics. J Epidemiol Community Health 67(6):519–525
Xu Z, Hu W, Su H, Turner LR, Ye X, Wang J, Tong S (2014) Extreme temperatures and paediatric emergency department admissions. J Epidemiol Community Health 68(4):304–311
Yi W., Chan A.P. (2014) Effects of temperature on mortality in Hong Kong: A time series study. Int J Biometeorol. Epub ahead of print
Zanobetti A, Schwartz J (2008) Temperature and mortality in nine US Cities. Epidemiology 19:563–570
Acknowledgments
This work was supported by the US National Institutes of Health (NIEHS R21ES020152).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 196 kb)
Rights and permissions
About this article
Cite this article
Son, JY., Gouveia, N., Bravo, M.A. et al. The impact of temperature on mortality in a subtropical city: effects of cold, heat, and heat waves in São Paulo, Brazil. Int J Biometeorol 60, 113–121 (2016). https://doi.org/10.1007/s00484-015-1009-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00484-015-1009-7