Abstract
Neurogenic bladder (NGB) is an encompassing term that includes multiple causes of bladder dysfunction linked to a congenital or acquired neurological condition that adversely impacts the innervation of the lower urinary tract. Multiple static or progressive conditions can be associated with NGB in pediatric and adolescent patients. Currently, spinal dysraphism (i.e., spina bifida) is one of the most common etiologies, which occurs in 3–4 per 10,000 live births in developed nations. Abnormal bladder dynamics can lead to kidney damage secondary to high pressures or recurrent infections, as well as urinary incontinence. The current management paradigm centers on a proactive approach to preserving kidney function and achieving continence through behavioral, pharmacological, and surgical means. This educational review highlights the key components of urological management to maximize collaboration with pediatric nephrologists.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neurogenic or neuropathic bladder (NGB) is a type of lower urinary tract dysfunction caused by injury or disease of the central or peripheral nervous system, which leads to problems with the adequate storage and elimination of urine. It may result from several underlying causes, such as spinal dysraphism. The most common etiology, spina bifida (SB), is reported in ~ 1 in 3000 births in the USA [1]. Other underlying conditions include sacral agenesis/caudal regression syndrome, anorectal and cloacal malformations, spinal cord injury, and transverse myelitis. NGB may also be caused by nervous system disorders, such as multiple sclerosis or spinal cord tethering, whereby dysfunction progresses with time, or secondary to treatment or therapies, such as with surgical management of neoplasms [2]. In addition, Hinman syndrome (HS) or “non-neurogenic” NGB, is thought to have a neuropsychological origin that leads to functional bladder dysfunction with no actual neurological cause and remains poorly understood [3]. Etiologies of NGB can be reviewed in Table 1.
Close monitoring of NGB patients is mandatory during childhood and adolescence due to the possibility of disease progression, especially during rapid growth phases (first 2 years of life and puberty). Importantly, the first 2 years of life are a critical period for neuroplasticity [4]. Therefore, procedures such as early ventriculoperitoneal shunting and cord detethering have a potential impact in preventing or reducing developmental and motor impairment in these patients. Furthermore, effective care should aim to minimize long-term sequelae, including urologic outcomes, kidney function, cardiovascular health, and issues linked to the quality of life, such as anxiety, body image, self-esteem, mobility, education, and employment [5, 6], which is best achieved by multidisciplinary collaboration. However, even with careful medical monitoring, without optimal management of the bladder (and bowel), NGB may result in irreversible deterioration of kidney function, recurrent urinary tract infections (UTIs) and urinary and fecal incontinence.
Optimizing lower urinary tract management is a crucial component and one of the most significant modifiable factors associated with the long-term preservation of kidney function [7,8,9]. Since the introduction of clean intermittent catheterization (CIC) by Lapides in the early 1970s [10], the life expectancy and quality of life of patients with NGB have improved but remain far from ideal [11]. The current trend in evaluation and management centers on a proactive approach, aiming at prevention through close monitoring and early introduction of medical and surgical interventions [5, 8]. This includes prenatal detection, which offers the opportunity to discuss fetal interventions and provide counselling and planning for comprehensive management in the neonatal period [12].
This educational review aims to describe the priorities in urological management from prenatal detection throughout childhood and adolescence, focusing on bladder and bowel dynamics to maximize the preservation of kidney function, prevention of UTIs, and achievement of continence in the social setting.
Prenatal care
With advances in prenatal screening, neural tube defects can be suspected early and confirmed on subsequent anatomy ultrasounds at 18–20 weeks' gestation [13]. Early identification offers the opportunity for timely multidisciplinary discussion with high-risk obstetrics, pediatric neurosurgery, urology, and nephrology about the continuation of the pregnancy, the role of fetal intervention and short- and long-term outcomes. Fetal closure is feasible until 25 weeks gestation [12] and can have benefits in terms of reduced need for ventriculoperitoneal shunt placement and improved lower extremity motor function based on data from the MOMS trial (Management of Myelomeningocele Study) [14]. The effect of prenatal closure on kidney and bladder function is less clear, although a growing body of literature suggests the potential for modest benefits [15]. To date, data from the MOMS trial reveals significantly fewer school-aged children on CIC in the prenatal closure group [16]. Similarly, Horst et al. reported that children who underwent prenatal closure presented better outcomes: less neurogenic bladder dysfunction (50% and 100% of children on CIC and anticholinergics in the prenatal vs. postnatal closure groups, respectively), less bladder wall thickening (37.5% and 87.5%, respectively), and fewer febrile UTIs (37.5% in the prenatal vs. 62.5% in the postnatal group) at 2 years of age [17].
Proactive versus reactive management
Two contrasting approaches to NGB management are described in the literature: proactive and reactive (or expectant). Most patients with SB are born with normal kidney function, so any subsequent deterioration should be considered preventable [18]. A proactive approach is defined as carrying out interventions before adverse lower urinary tract dynamics occur. Such interventions include early initiation of CIC, close monitoring with imaging studies and urodynamics (UDS), liberal use of systemic or local medications, selective surgical interventions before the development of recurrent infections, ineffective emptying, and elevated bladder pressures. The reactive approach triggers interventions after developing such adverse changes resulting in kidney and/or bladder deterioration [7].
Urological therapies in NGB focus on avoiding high storage and voiding pressures, ensuring safe filling pressures with coordinated emptying at an adequate capacity for age to preserve kidney function [17]. Prakash et al. report an incidence of kidney function deterioration of 50% in children with delayed NGB presentation before 13 years of age. This contrasts with the 17% reported for the proactive management approach [19]. When a proactive approach is employed, UDS are performed within a few months of life, at toilet training age, and puberty, as well as when prompted by clinical or imaging findings such as recurrent UTIs, new onset of urinary incontinence, retention, or hydronephrosis. CIC is started in infancy and guided by changes in urine volumes, leakage, UDS parameters, and imaging studies (mainly serial ultrasounds). Serial ultrasounds should be ordered every 3–6 months in the first 3 years of life, and then every 6–12 months until adolescence. Pharmacological interventions, most notably anticholinergics such as oxybutynin, are initiated early on and adjusted in response to leakage between catheterizations, worsening pressures on UDS or hydronephrosis on ultrasound. Serum creatinine and cystatin C—if available—are obtained every 6 to 12 months to monitor kidney function [7, 20, 21]. A proactive NGB clinical pathway is proposed in Fig. 1.
Multidisciplinary care
Spina bifida affects neurological, musculoskeletal, genitourinary, and gastrointestinal systems requiring specialized care. In addition, consideration should be given to the psychosocial impact on the developing child with a chronic illness. The Spina Bifida Association recommends multidisciplinary clinics as the gold standard, which includes transition preparation from pediatric to adult care [19, 21, 22].
Imaging and urodynamic studies
Risk factors for kidney deterioration include delayed presentation, palpable bladder, recurrent UTIs, increased bladder wall thickness, secondary vesicoureteral reflux (VUR), increased post-void residuals (PVR), and high detrusor leak point pressures (DLPP) (> 40 cm H20) on urodynamics [23]. Since clinical findings alone are a poor guide, the following imaging and urodynamic studies are the cornerstone of monitoring and serve as the basis for most interventions. In addition to investigations, a diary of the frequency of voids or catheters, volumes, fluid intake, and urinary incontinence can provide additional information about the current state and effectiveness of treatments [21].
Renal and bladder ultrasound (RBUS)
RBUS imaging is radiation-free, non-invasive, and readily available, making it the most frequently obtained study to detect abnormalities and follow trends over time. Routine RBUS is recommended every 3–6 months in the first 3 years of life, then every 6–12 months after that [5, 17, 20]. Parameters to consider are the degree of hydronephrosis, parenchymal changes (echogenicity, loss of corticomedullary differentiation, development of cysts), bladder abnormalities (distention, wall thickening, diverticula, stones) and, if possible, post-void residual. Hydronephrosis is customarily reported using the society of fetal urology (SFU) grading system, and measurement of the anterior–posterior diameter of the renal pelvis (APD) [24]. A newer urinary tract dilation (UTD) classification system was proposed in 2014 and included additional findings: APD, calyceal dilation, renal parenchymal thickness and echogenicity, ureteral dilation, and bladder abnormalities [25]. These additional considerations are relevant to the ultrasound assessment in the setting of neurogenic bladder. However, despite being more comprehensive than the SFU and APD grading systems, the UTD classification can be perceived as cumbersome for routine use and has not yet been largely incorporated to practice in most centers. Of note, minimal or absent hydronephrosis should not provide complete reassurance. For example, Sager et al. reported “high-risk” UDS parameters in almost 50% of children < 1 year; however, only one-third had pelviectasis on ultrasound [26].
Voiding cystourethrogram (VCUG)
VCUG provides information on vesicoureteral reflux and the appearance of the bladder and urethra. In addition, it allows for assessing bladder capacity and post-void residual [27]. VCUG can be obtained as a stand-alone test in cases of recurrent UTIs or worsening hydronephrosis or in conjunction with a UDS (so-called “video” UDS).
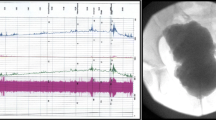
Urodynamics
UDS is the most comprehensive test to evaluate bladder dynamics during filling (storage phase) and emptying (voiding phase), compliance, capacity, detrusor contractility, lower urinary tract pressures, sphincter function, and detrusor-sphincter coordination. A baseline study is obtained soon after diagnosis (i.e., in the first year of life in congenital cases and once an acquired insult has stabilized). UDS is an invasive test that involves the insertion of urethral and rectal catheters to measure the bladder and abdominal pressures as the bladder is slowly filled with saline or contrast (for video UDS) at rates that mimic the urinary production (maximum 10% of the child’s estimated bladder capacity per minute). Contraction detrusor pressures > 15–20 cmH20 in the presence of detrusor-sphincter dyssynergia or an end-filling pressure or DLPP > 40 cmH20 indicates a high-pressure (“hostile”) bladder with increased risk for kidney damage. It is important to note that interpreting UDS in infants is challenging because patients are required to lie still in supine position for accurate intra-abdominal and vesical pressure readings [5, 23]. However, in centers with expertise, the study can yield valuable information identifying early a subset of infants at risk for kidney function deterioration, given that only 24% of UDS results in infants are considered low risk [28].
Dimercaptosuccinic acid scan (DMSA)
DMSA is sometimes recommended as a baseline study by 6 months of age [5] or within the first year following diagnosis [21] to document differential function and kidney scarring or dysplasia. Photopenic defects on DMSA scans can help estimate the degree of compromise in renal reserve and correlates with hypertension in adulthood [29]. Therefore, if done around the time of presentation, it compares the impact of future insults, such as recurrent febrile UTIs [21]. Nevertheless, this must be taken in the context of radiation exposure and how the study findings will change clinical management. Reassuringly, it has been reported that more than 95% of kidneys showed no defects on baseline DMSA scans [30], in contrast to a retrospective study of 60 infants less than a year of age that detected abnormalities in 30% [26]. Doyle et al. suggest a selective approach to a baseline DMSA based on their findings that over 80% of DMSA scans could be avoided without missing any cortical scarring; if testing is limited to patients with febrile UTIs [31], then the scan should be done at least 4 to 6 months after an episode of pyelonephritis [32].
Bladder management
Clean intermittent catheterization
CIC initiation is recommended shortly after birth, or at the time of diagnosis and frequency can be adjusted based on UDS, PVRs and ultrasound findings [5, 6, 11, 20, 33]. CIC remains the preferred method of management compared to indwelling or suprapubic catheters. Of all the options, permanent drainage with indwelling catheters carries the highest risk of complications and infections and should be avoided as a long-term strategy [7]. This does not include overnight drainage with indwelling catheters limited to the time the child is asleep. Traumatic catheterization may result in false passage and urethral stricture, which is more common in males given their longer urethra. Urethral self-catheterization can be more challenging for non-ambulatory female patients from a positioning standpoint or in the presence of upper extremity motor impairment. A continent catheterizable channel, such as appendicovesicostomy, can facilitate CIC for those patients. Hydrophilic catheters may offer some benefits, such as decreased hematuria and stricture rates and improved quality of life [34, 35]. However, reusing catheters remains controversial and has significant economic and environmental implications. The literature is heterogenous, with some studies demonstrating no change in the rate of UTIs [36, 37], while others suggest that single-use catheters decrease the incidence of infections [38, 39].
Diagnosis and treatment of UTIs
Clinical suspicion and well-established criteria are critical to diagnosing “true” UTIs vs. asymptomatic bacteriuria, particularly in patients that perform CIC. Asymptomatic bacteriuria is defined by bacterial colonization without an inflammatory response (pyuria), occurs in > 75% of NGB on CIC and does not benefit from systemic antibiotic therapy. A “true” UTI is defined as fever and urinalysis positive for leukocytes + / − nitrites, a urine culture consisting of > 50,000 colony forming units/milliliter (CFU/ml) from a catheter or suprapubic aspiration, or > 100,000 CFU/ml in a midstream urine sample [6]. Only confirmed febrile UTIs should be used to mitigate the development of antibiotic resistance [21, 40]. However, favoring treatment is reasonable in selected cases of unwell-appearing, febrile children without another focus of infection.
Pharmacotherapy
Continuous antibiotic prophylaxis (CAP)
It is unclear if CAP provides benefits for all patients with NGB. Infants at higher risk include those with SFU grades 3–4 hydronephrosis, VUR, and poor emptying [41], albeit based on weak evidence [42]. Therefore, in the case of breakthrough infections or UTIs after CAP cessation, a closer look at bladder dynamics and other modifiable risk factors should be considered.
Intravesical instillation of antimicrobials
In children that undergo CIC, an alternative to systemic CAP is the intravesical instillation of antimicrobials. This has been of particular interest since the emergence of extended-spectrum beta-lactamase (ESBL) organisms which limit oral antibiotic options. Two recent small pediatric studies demonstrated the safety and effectiveness of gentamicin instillations. In both studies, there was a decrease in UTIs, systemic absorption was not detected, and there were no adverse outcomes, including nephrotoxicity or ototoxicity [41,42,43]. Our institutional tobramycin/gentamicin intravesical instillation protocol can be reviewed in Table 2.
Optimization of bladder storage and emptying
Medications that decrease detrusor overactivity and pressures, enhance bladder capacity, and improve compliance include anticholinergics, beta-3 agonists, and botulinum toxin. The most studied anticholinergic medication to date is oxybutynin, which has a long track record of safety but has a significant side effect profile that can lead to discontinuation or poor adherence [35]. Doses can be adjusted by weight (0.2 mg/kg/dose up to 5 years of age, then 5 mg/dose two to three times daily) and started in infancy [35]. In selected cases, oxybutynin can also be administered intravesically [35, 44]. Although the systemic presence of metabolites is the most likely mechanism of action, there is a more favorable side effect profile when the intestinal first-pass metabolism is circumvented or decreased. Side effect minimization can also be achieved with extended-release preparations and transdermal administration. Side effects are mediated by anticholinergic activity in other organs, metabolites (mainly desethyoxybutyinin), and entry into the central nervous system [35]. The side effects of oxybutynin include dry mouth, constipation, blurred vision, headache, somnolence, impaired school performance, facial flushing, gastrointestinal discomfort, and dry, itchy skin. Ultimately, this drug effectively manages detrusor overactivity and high bladder filling pressures, but at the expense of side effects and the unknown impact of long-term exposure [21, 35]. Tolterodine and propiverine are other common non-selective anticholinergic medications used for the treatment of NGB with similar side effect profiles [20, 32].
Solifenacin, a newer anticholinergic medication and more selective to the bladder, provides a more favorable systemic side effect profile, requires only daily dosing and is an effective, safe [45] FDA-approved anticholinergic medication for pediatric use [46].
Mirabegron is in a new class of bladder medications (FDA-approved in pediatric patients > 3 years of age for neurogenic detrusor overactivity), acting as a beta 3 agonist with a therapeutic effect like anticholinergic medications [47, 48]. Given the uncommon but important side effect of hypertension in pediatric patients, blood pressure should be measured prior to and shortly after initiation. Mirabegron has also been shown to be effective as an adjuvant therapy alongside anticholinergic medication in children with refractory neurogenic bladder, reducing intravesical pressure, increasing bladder capacity, and helping to achieve continence in 70% of the study population [47].
Alpha blockers
Alpha (1) blockers (i.e., tamsulosin/silodosin/doxazosin) reduce sphincter tension and ease bladder emptying. However, use in pediatrics is off-label, and side effects of hypotension, dizziness, and drowsiness must be considered [49]. To date, no substantive data has been published confirming the effectiveness of alpha-blocker use in NGB [48], but it could be considered to improve PVRs in the setting of high sphincter tone.
Table 3 outlines medications used in the urological care of NGB.
Surgical interventions
With adequate medical management, most patients can achieve safe bladder pressures during storage and efficacious bladder emptying (via CIC or voiding). Nevertheless, a subgroup requires adjuvant surgical procedures to improve bladder dynamics, facilitate drainage, address low bladder outlet resistance leading to incontinence or facilitate CIC [50, 51].
Intravesical injections of botulinum toxin-A
Botulinum toxin-A injections improve bladder capacity and decrease detrusor pressure working through a completely different mechanism of action by blocking presynaptic acetylcholine compared to anticholinergic and beta-3 agonist medications. By the direct delivery into the detrusor muscle, the incidence of systemic side effects is negligible. Multiple reports have demonstrated improved bladder compliance with botulinum toxin-A injections in patients refractory to anticholinergic medication, in some cases delaying or avoiding the need for more invasive surgical interventions (i.e., augmentation cystoplasty) [49, 51, 52]. Additionally, botulinum toxin-A can be injected into the urethral sphincter to decrease urethral resistance in patients with NGB, and detrusor sphincter dyssynergia, who are unable to volitionally empty the bladder with CIC due to a tight sphincter, carrying a high risk of kidney deterioration [51, 53]. However, pediatric studies are lacking. Botulinum toxin-A must be repeated every 6–9 months as its effectiveness gradually decreases with time [50]. The need for anesthesia in younger children is one of the most important concerns with this intervention. With careful patient selection, and in adolescents, the procedure can be safely performed in the clinic with local anesthesia and sedation [54].
Bladder augmentation
Bladder augmentation (or augmentation cystoplasty) involves creating a larger, low-pressure reservoir for urine by anastomosing a detubularized segment of tissue (most commonly from the ileum or colon). It is considered a last resort, indicated for recalcitrant hostile bladders unresponsive to medical therapy [55]. Despite its impressive bladder outcomes (increasing compliance in 69–100%, restoring continence in 75–100% and improving quality of life), it comes with significant short- and long-term risks [34]. These include malignancy, bladder calculi, UTIs, mucus production, bladder perforation, metabolic, and electrolyte disturbances. The absorption of urinary electrolytes such as hydrogen ions, ammonium, and chloride by the bowel segment leads to hyperchloremic metabolic acidosis, which can ultimately impact growth and bone health [56]. Additionally, children with enterocystoplasty are at risk for vitamin B12 deficiency. CBC, serum B12, folate levels, and iron studies are recommended annually and should be supplemented accordingly. Long-term surveillance and CIC compliance are critical to preventing and managing these risks [51]. Bladder saline flushes are recommended 2 to 4 times daily to prevent mucous accumulation, UTIs and stone formation. New tissue engineering technology is being explored to address the risks of traditional bladder augmentation [57] (See Fig. 2D).
Continent catheterizable channels
Mitrofanoff first used the appendix to create an alternative catheterizable channel in 1980, but alternatives to the appendix have been described [58]. Continent catheterizable channels (CCC) have been associated with improved quality of life compared to CIC per urethra. A recent paper that reviewed pediatric and adult patients found CCCs associated with good health-related quality of life and easy and painless catheterization. Additionally, overall satisfaction and cosmetic perception were found in 91% of participants [59]. Creating a CCC does not replace the need to manage bladder pressures; it simply offers an alternative way to empty the bladder, in many cases allowing easier catheterization by patients, which maximizes their independence, or by their caregivers (See Figs. 2A and 3).
Temporary incontinent diversions
Temporary incontinent diversions may be considered in the younger child (before toilet training). Vesicostomy involves bringing the bladder to the skin and forming a stoma in the suprapubic region for continuous bladder drainage. This is an option when there is a concern for kidney function deterioration and CIC is not an option for anatomical or social reasons. Cutaneous ureterostomy involves creating a stoma with the distal ureter and is a surgical alternative in the setting of high-grade VUR and recurrent febrile UTIs or poor bladder dynamics that preclude consideration of vesicostomy [51]. Incontinent diversions tend to be reserved for infants prior to typical toilet training age and less common in older children.
Bladder neck closure procedures
Bladder neck closure, bladder neck reconstruction and the use of slings can be considered for patients with bladder neck incompetence and persistent urinary leakage. Bladder neck closure procedures are often paired with CCC creation to ensure safe bladder emptying. This consideration implies careful patient selection and understanding the risks of each, such as upper renal deterioration and bladder rupture in cases of poor adherence with regular bladder emptying [50] (See Fig. 2B).
Management of the neurogenic bowel
Optimal bowel emptying allows the bladder to fill and empty more effectively. The management goal is to have predictable bowel emptying with no encopresis between these times. A healthy diet, use of oral laxatives, and rectal therapies including digital stimulation, suppositories, enemas, and transanal irrigation (i.e., Peristeen®) should be considered in the management of neurogenic bowel [60].
Malone antegrade continence enema (MACE)
MACE is a surgical alternative that allows for antegrade enemas [51]. It is a continent catheterizable channel connecting the appendix to the colon and accessed through a stoma on the skin. Patients instill 10 to 30 ml/kg of water or saline into the stoma (often with a small amount of glycerin), which results in a predictable bowel movement daily. Most patients can empty the colon in about 60 min (See Figs. 2C and 3).
Cecostomy tube
The placement of a cecostomy tube is an alternative for patients without a suitable appendix, or when the appendix is not long enough to create both Mitrofanoff and MACE simultaneously [35, 61]. In addition, achieving fecal continence improves satisfaction and quality of life in children and care providers and should be a priority in pediatric care of patients with SB [61]. However, the drawback of cecostomy tubes is that a button-like device is left in place, which requires regular replacement under anesthesia and radiation exposure.
Comorbidity management
Kidney function
Kidney function in patients with SB requires more than monitoring serum creatinine (Cr). A recent retrospective review (5445 patients across 23 clinics) of kidney disease surveillance in the Spina Bifida Patient Registry (USA) yielded a disappointing 62% (range 6–100%) compliance with kidney disease l surveillance defined as ultrasound and serum Cr within 2 years of follow-up between 2013 and 2018. Current guidelines do not expressly or consistently guide kidney disease surveillance. Furthermore, the classic method of monitoring kidney function using serum Cr and estimated glomerular filtration rate (eGFR) equations may not be accurate in patients with SB with varied low muscle mass. Cystatin C is not impacted by sex, muscle mass, height, or body mass index (BMI). Therefore, eGFR formulas using Cystatin C may be more accurate in children and adults with spina bifida [62]. Considering the absence of an eGFR formula in patients with SB, serum Cr, and Cystatin C are often used as part of kidney surveillance [62]. Nuclear medicine GFR may also be helpful in kidney disease surveillance for patients with SB [5]. Future research to develop an eGFR formula specific to SB would be ideal. Until then, a recent paper compared Cr and Cystatin C-based Chronic Kidney disease in Children (CKiD) equations to the gold standard 99mTcDTPA clearance method and determined that the Cystatin C-based CKiD equation was the most accurate [63].
Blood pressure
Hypertension is an important modifiable cardiovascular risk factor and is seen at higher rates within the SB population. In a cross-sectional retrospective study of 225 adults with SB, less than half had normal blood pressure [64]. In another retrospective review, 41.5% of pediatric patients with SB had hypertension compared to a national prevalence of 3% [65]. In addition, children with SB have a higher risk of obesity due to less lean body mass and lower metabolic rates. Therefore, annual blood pressure checks and a focus on healthy eating, exercise options (especially for the non-ambulatory patient) and screening for diabetes (especially in the setting of hypertension or other risk factors) are essential aspects of NGB care [5]. Urinary tract dysfunction also increases the lifetime risk of developing hypertension. Moreover, patients with high spinal cord injury (at or above the level of the sixth thoracic vertebrae) can develop episodic hypertension associated with autonomic dysreflexia (AD). Visceral stimuli during bowel care and urinary retention are potent triggers for the sympathetic discharge that occurs in AD.
Kidney stones
Urolithiasis is more common in spinal dysraphism, primarily related to the neurogenic bladder, for several reasons: immobility, urine stasis, bacteriuria, catheterization, and lower urinary tract reconstruction. In a large cohort study of almost 12,000 pediatric patients with upper tract urolithiasis, the prevalence of stones in patients with normal spines was 0.24%. In contrast, the prevalence of stones in patients with spinal dysraphism was 4.03% [66]. The incidence of urolithiasis is 50% over 10 years in NGB [50]. Bladder augmentation is arguably the most significant risk factor for urolithiasis in patients with SB. In another retrospective review focusing on the risk of nephrolithiasis after bladder augmentation in 427 patients, the incidence is at least ten times that of the general population [67]. Close surveillance of children at highest risk, comprehensive metabolic workup, and prevention of stones, including fluid intake, diet and the need for medications, are areas that nephrology specializes in and further supports this type of care in these patients.
Monitoring kidney function using the most accurate data points and calculations to optimize medical care, addressing modifiable risk factors, such as hypertension and metabolic risk factors for urolithiasis are critical for patients with NGB. Predicting and preventing upper tract deterioration is the cornerstone to nephro-urological neurogenic bladder care. A center focused on a proactive approach identified the risk factors which correlated strongly with upper tract damage (defined as kidney scar development) in their patients as: older age, abnormal appearing bladder on ultrasound or VCUG and high leak point pressure on urodynamics. They advocate for a coordinated effort between urology and nephrology care providers as well as family engagement to affect the high prevalence of CKD for children and adults with neurogenic bladder deemed to be mostly preventable [68]. We know that kidney scar development and elevated creatinine are usually irreversible and late markers of upper tract damage. Promising work over the past two decades to identify non-invasive biomarkers and monitoring of bladder function to better manage and predict those at most risk for upper tract damage is exciting. Alternative inflammatory biomarkers to define UTI, identification of healthy flora protective against UTIs, bladder wall thickness and ultrasound shear wave elastography to assess bladder dynamics and at home monitoring of bladder pressures are promising areas of study that could further contribute to the proactive management of NGB [69].
Conclusion
The past few decades’ progress in managing pediatric neurogenic bladder resulted in a paradigm shift from reactive to proactive management. Early evaluation and management of NGB with the start of CIC at birth, early UDS and quick introduction of pharmacological agents and/or surgery for those with abnormal UDS is widely accepted and should be implemented along with multidisciplinary care throughout the lifespan. Nephrology and urology must collaborate closely, from prenatal consults to postnatal management, to prevent upper tract deterioration over time. In addition, the utmost focus of NGB treatment is to preserve kidney and bladder function throughout the lifespan. As in many other conditions where kidney function is at risk, the collaboration between nephrology and urology is critical.
Key summary points
-
1.
Optimal urologic care is one of the cornerstones to preserve kidney function in pediatric and adolescent patients with NGB.
-
2.
A paradigm shift from reactive to proactive management includes prenatal evaluation, the start of CIC at birth, early UDS and quick introduction of pharmacological agents and/or surgery for those with abnormal UDS aiming to prevent upper tract deterioration and improve quality of life (i.e., address incontinence as early as possible or desirable).
-
3.
Although most patients with NGB can achieve safe bladder pressures during storage and efficacious bladder emptying (via CIC or voiding), a subgroup requires adjuvant surgical procedures to improve bladder dynamics, treat incontinence or facilitate CIC.
Multiple choice questions
Answers appear following the references.
-
1.
Which of the following is untrue regarding proactive management of neurogenic bladder?
-
a)
CIC initiated at birth
-
b)
Urodynamics delayed until potty training age
-
c)
Anticholinergic medication initiated with findings of poor bladder compliance without hydronephrosis
-
d)
Kidney function studies (i.e. Creatinine, Cystatin- C) are regularly performed
-
2.
The management of recurrent UTIs in children who perform CIC includes all of the following, except:
-
a)
Intravesical antibiotic administration
-
b)
Prophylactic oral antibiotics
-
c)
Optimization of bladder dynamics
-
d)
Retrograde colonic irrigation
-
3.
Several medications can be used to treat poor compliant, high-pressure bladders, except:
-
a)
Oxybutynin
-
b)
Mirabegron
-
c)
Solifenacin
-
d)
Tamsulosin
-
4.
Intravesical injections of Botulinum toxin-A are effective to manage:
-
a)
High post void residual
-
b)
UTIs
-
c)
High pressure bladder
-
d)
Detrusor sphincter dyssynergia
-
5.
The following are true regarding urological surgeries for neurogenic bladder except:
-
a)
Mitrofanoff is a continent catheterizable channel that facilitates CIC
-
b)
Urinary diversions should be done for all infants with high grade VUR
-
c)
Bladder augmentation comes with significant short- and long-term risks including stones, cancer, metabolic changes, UTIs, and mucus production
-
d)
VUR due to neurogenic bladder is usually secondary and management should be focused on improving bladder dynamics
Change history
06 September 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00467-023-06141-3
References
Mai CT, Isenburg JL, Canfield MA et al (2019) National population-based estimates for major birth defects, 2010–2014. Birth Defects Res 111:1420–1435. https://doi.org/10.1002/bdr2.1589
Bauer SB (2008) Neurogenic bladder: etiology and assessment. Pediatr Nephrol 23:541–551. https://doi.org/10.1007/s00467-008-0764-7
Bauer SB (2017) The Hinman Syndrome. J Urol 197(2S):S132–S133. https://doi.org/10.1016/j.juro.2016.11.026
Reid LB, Rose SE, Boyd RN (2015) Rehabilitation and neuroplasticity in children with unilateral cerebral palsy. Nat Rev Neurol 11:390–400. https://doi.org/10.1038/nrneurol.2015.97
Woodhouse CRJ (2008) Myelomeningocele: neglected aspects. Pediatr Nephrol 23:1223–1231. https://doi.org/10.1007/s00467-007-0663-3
Spina Bifida Association (2018) Guidelines for the care of people with spina bifida. https://www.spinabifidaassociation.org/guidelines/
Fairchild RJ, Aksenov LI, Hobbs KT et al (2022) Medical management of neurogenic bladder in patients with spina bifida: a scoping review. J Pediatr Urol 19:55–63. https://doi.org/10.1016/j.jpurol.2022.10.016
Elzeneini W, Waly R, Marshall D, Bailie A (2019) Early start of clean intermittent catheterization versus expectant management in children with spina bifida. J Pediatr Surg 54:322–325. https://doi.org/10.1016/j.jpedsurg.2018.10.096
Dik P, Klijn AJ, van Gool JD et al (2006) Early start to therapy preserves kidney function in spina bifida patients. Eur Urol 49:908–913. https://doi.org/10.1016/j.eururo.2005.12.056
Lapides J, Diokno AC, Silber SJ, Lowe BS (1972) Clean, intermittent self-catheterization in the treatment of urinary tract disease. J Urol 107:458–461. https://doi.org/10.1016/S0022-5347(17)61055-3
Glinianaia SV, Morris JK, Best KE et al (2020) Long-term survival of children born with congenital anomalies: a systematic review and meta-analysis of population-based studies. PLoS Med 17:e1003356. https://doi.org/10.1371/journal.pmed.1003356
Church PT, Castillo H, Castillo J et al (2020) Prenatal counseling: guidelines for the care of people with spina bifida. J Pediatr Rehabil Med 13:461–466. https://doi.org/10.3233/PRM-200735
Douglas Wilson R, Van Mieghem T, Langlois S, Church P (2021) Guideline no. 410: prevention, screening, diagnosis, and pregnancy management for fetal neural tube defects. J Obstet Gynaecol Can 43:124-139.e8. https://doi.org/10.1016/j.jogc.2020.11.003
Adzick NS, Thom EA, Spong CY et al (2011) A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med 364:993–1004. https://doi.org/10.1056/NEJMoa1014379
Mazzone L, Hölscher AC, Moehrlen U et al (2020) Urological outcome after fetal spina bifida repair: data from the Zurich cohort. Fetal Diagn Ther 47:882–888. https://doi.org/10.1159/000509392
Brock JW, Thomas JC, Baskin LS et al (2019) Effect of prenatal repair of myelomeningocele on urological outcomes at school age. J Urol 202:812–818. https://doi.org/10.1097/JU.0000000000000334
Horst M, Mazzone L, Schraner T et al (2017) Prenatal myelomeningocele repair: do bladders better? Neurourol Urodyn 36:1651–1658. https://doi.org/10.1002/nau.23174
Joseph DB, Baum MA, Tanaka ST et al (2020) Urologic guidelines for the care and management of people with spina bifida. J Pediatr Rehabil Med 13:479–489. https://doi.org/10.3233/PRM-200712
Thibadeau J, Walker WO, Castillo J et al (2020) Philosophy of care delivery for spina bifida. Disabil Health J 13:100883. https://doi.org/10.1016/j.dhjo.2019.100883
Sager C, Burek C, Gomez YR et al (2022) Nephro-urological outcomes of a proactive management of children with spina bifida in their first 5 Years of life. J Pediatr Urol 18:181.e1-181.e7. https://doi.org/10.1016/j.jpurol.2021.12.002
Stein R, Bogaert G, Dogan HS et al (2020) EAU/ESPU guidelines on the management of neurogenic bladder in children and adolescent part I diagnostics and conservative treatment. Neurourol Urodyn 39:45–57. https://doi.org/10.1002/nau.24211
Shlobin NA, Yerkes EB, Swaroop VT et al (2022) Multidisciplinary spina bifida clinic: the Chicago experience. Childs Nerv Syst 38:1675–1681. https://doi.org/10.1007/s00381-022-05594-5
Prakash R, Puri A, Anand R et al (2017) Predictors of upper tract damage in pediatric neurogenic bladder. J Pediatr Urol 13:503.e1-503.e7. https://doi.org/10.1016/j.jpurol.2017.02.026
Fernbach SK, Maizels M, Conway JJ (1993) Ultrasound grading of hydronephrosis: introduction to the system used by the society for fetal urology. Pediatr Radiol 23:478–480. https://doi.org/10.1007/BF02012459
Nguyen HT, Phelps A, Coley B et al (2022) 2021 update on the urinary tract dilation (UTD) classification system: clarifications, review of the literature, and practical suggestions. Pediatr Radiol 52:740–751. https://doi.org/10.1007/s00247-021-05263-w
Sager C, Burek C, Corbetta JP et al (2017) Initial urological evaluation and management of children with neurogenic bladder due to myelomeningocele. J Pediatr Urol 13:271.e1-271.e5. https://doi.org/10.1016/j.jpurol.2016.12.024
Janssen KM, Kirsch AJ, Crisostomo-Wynne TC et al (2021) Standardized protocol for voiding cystourethrogram: are recommendations being followed? J Pediatr Urol 17:66.e1-66.e6. https://doi.org/10.1016/j.jpurol.2020.10.009
Tanaka ST, Yerkes EB, Routh JC et al (2021) Urodynamic characteristics of neurogenic bladder in newborns with myelomeningocele and refinement of the definition of bladder hostility: findings from the UMPIRE multi-center study. J Pediatr Urol 17:726–732. https://doi.org/10.1016/j.jpurol.2021.04.019
Veenboer PW, Hobbelink MGG, Ruud Bosch JLH et al (2015) Diagnostic accuracy of Tc-99m DMSA scintigraphy and renal ultrasonography for detecting renal scarring and relative function in patients with spinal dysraphism: DMSA-Scintigraphy Versus Ultrasound in Adults With SD. Neurourol Urodyn 34:513–518. https://doi.org/10.1002/nau.22608
Tanaka ST, Paramsothy P, Thibadeau J et al (2019) Baseline urinary tract imaging in infants enrolled in the UMPIRE protocol for children with spina bifida. J Urol 201:1193–1198. https://doi.org/10.1097/JU.0000000000000141
Cascio S, Doyle M, Mc Mahon O, Kelly G (2021) Urinary tract imaging in infants with spina bifida: a selective approach to a baseline DMSA. J Pediatr Urol 17:396.e1-396.e6. https://doi.org/10.1016/j.jpurol.2021.02.004
Sarikaya I, Sarikaya A (2019) Current status of radionuclide renal cortical imaging in pyelonephritis. J Nucl Med Technol 47:309–312. https://doi.org/10.2967/jnmt.119.227942
Yadav P, Alsabban A, de Los RT et al (2022) A systematic review of paediatric neurogenic lower urinary tract dysfunction guidelines using the Appraisal of Guidelines and Research Evaluation (AGREE) II instrument. BJU Int 131:520–529. https://doi.org/10.1111/bju.15902
Kavanagh A, Baverstock R, Campeau L et al (2019) Canadian urological association guideline: diagnosis, management, and surveillance of neurogenic lower urinary tract dysfunction. Can Urol Assoc J 13:E157–E176. https://doi.org/10.5489/cuaj.5912
Rawashdeh YF, Austin P, Siggaard C et al (2012) International children’s continence society’s recommendations for therapeutic intervention in congenital neuropathic bladder and bowel dysfunction in children: ICCS: therapeutic Intervention in Pediatric NBD. Neurourol Urodyn 31:615–620. https://doi.org/10.1002/nau.22248
Elliott CS, Dallas K, Shem K, Crew J (2022) Adoption of single-use clean intermittent catheterization policies does not appear to affect genitourinary outcomes in a large spinal cord injury cohort. J Urol 208:1055–1074. https://doi.org/10.1097/JU.0000000000002836
Madero-Morales PA, Robles-Torres JI, Vizcarra-Mata G et al (2019) Randomized clinical trial using sterile single use and reused polyvinylchloride catheters for intermittent catheterization with a clean technique in spina bifida cases: short-term urinary tract infection outcomes. J Urol 202:153–158. https://doi.org/10.1097/JU.0000000000000244
Ye D, Chen Y, Jian Z et al (2021) Catheters for intermittent catheterization: a systematic review and network meta-analysis. Spinal Cord 59:587–595. https://doi.org/10.1038/s41393-021-00620-w
Christison K, Walter M, Wyndaele J-JJM et al (2018) Intermittent catheterization: the devil is in the details. J Neurotrauma 35:985–989. https://doi.org/10.1089/neu.2017.5413
Ben-David R, Carroll F, Kornitzer E et al (2022) Asymptomatic bacteriuria and antibiotic resistance profile in children with neurogenic bladder who require clean intermittent catheterization. Spinal Cord 60:256–260. https://doi.org/10.1038/s41393-021-00679-5
Szymanski KM (2021) Is antibiotic prophylaxis really necessary for infants with neuropathic bladder? J Urol 206:13–14. https://doi.org/10.1097/JU.0000000000001818
Zegers SHJ, Dieleman J, van der Bruggen T et al (2017) The influence of antibiotic prophylaxis on bacterial resistance in urinary tract infections in children with spina bifida. BMC Infect Dis 17:63. https://doi.org/10.1186/s12879-016-2166-y
Andretta E, Longo R, Balladelli M et al (2022) Intravesical gentamicin: an option for therapy and prophylaxis against recurrent UTIs and resistant bacteria in neurogenic bladder patients on intermittent catheterization. Antibiotics 11:1335. https://doi.org/10.3390/antibiotics11101335
Lazarus J (2009) Intravesical oxybutynin in the pediatric neurogenic bladder. Nat Rev Urol 6:671–674. https://doi.org/10.1038/nrurol.2009.214
Franco I, Hoebeke P, Baka-Ostrowska M et al (2020) Long-term efficacy and safety of solifenacin in pediatric patients aged 6 months to 18 years with neurogenic detrusor overactivity: results from two phase 3 prospective open-label studies. J Pediatr Urol 16:180.e1-180.e8. https://doi.org/10.1016/j.jpurol.2019.12.012
US Food and Drug Administration (2020) FDA approves first treatment for a form of bladder dysfunction in pediatric patients as young as 2 years of age. https://www.fda.gov/news-events/press-announcements/fda-approves-first-treatment-form-bladder-dysfunction-pediatric-patients-young-2-years-age
Sager C, Sanmartino M, Burek C et al (2020) Efficacy and safety of Mirabegron as adjuvant treatment in children with refractory neurogenic bladder dysfunction. J Pediatr Urol 16:655.e1-655.e6. https://doi.org/10.1016/j.jpurol.2020.07.020
US Food and Drug Administration (2021) FDA approves new indication for drug to treat neurogenic detrusor overactivity in pediatric patients. https://www.fda.gov/news-events/press-announcements/fda-approves-new-indication-drug-treat-neurogenic-detrusor-overactivity-pediatric-patients#:~:text=Today%2C%20the%20U.S.%20Food%20and,neurological%20impairment%2C%20in%20children%20ages
Lucas E (2019) Medical management of neurogenic bladder for children and adults: a review. Top Spinal Cord Inj Rehabil 25:195–204. https://doi.org/10.1310/sci2503-195
Moussa M, Papatsoris AG, Abou Chakra M et al (2021) Perspectives on urological care in spina bifida patients. Intractable Rare Dis Res 10:1–10. https://doi.org/10.5582/irdr.2020.03077
Stein R, Bogaert G, Dogan HS et al (2020) EAU/ESPU guidelines on the management of neurogenic bladder in children and adolescent part II operative management. Neurourol Urodyn 39:498–506. https://doi.org/10.1002/nau.24248
Bowen DK, Meyer T, Rosoklija I et al (2022) Botulinum toxin in patients at-risk for bladder augmentation: durable impact or kicking the can? Neurourol Urodyn 41:1406–1413. https://doi.org/10.1002/nau.24962
Kao Y-L, Huang K-H, Kuo H-C, Ou Y-C (2019) The therapeutic effects and pathophysiology of botulinum toxin A on voiding dysfunction due to urethral sphincter dysfunction. Toxins 11:728. https://doi.org/10.3390/toxins11120728
Overland MR, Leva NV, DiSandro M, Copp HL (2022) Feasibility of awake intravesical botulinum toxin injection in pediatric neurogenic bladder. J Urol 208:702–710. https://doi.org/10.1097/JU.0000000000002709
Roth JD, Cain MP (2018) Neuropathic bladder and augmentation cystoplasty. Urol Clin North Am 45:571–585. https://doi.org/10.1016/j.ucl.2018.06.005
Eldred-Evans D, Khan F, Abbaraju J, Sriprasad S (2015) An unrecognised case of metabolic acidosis following neobladder augmentation cystoplasty. Int J Surg Case Rep 11:129–131. https://doi.org/10.1016/j.ijscr.2015.03.039
Wang X, Zhang F, Liao L (2021) Current applications and future directions of bioengineering approaches for bladder augmentation and reconstruction. Front Surg 8:664404. https://doi.org/10.3389/fsurg.2021.664404
Farrugia M-K, Malone PS (2010) Educational article: the Mitrofanoff procedure. J Pediatr Urol 6:330–337. https://doi.org/10.1016/j.jpurol.2010.01.015
Chavarriaga J, Fernández N, Campo MAO et al (2020) Self-perception, quality of life and ease of catheterization in patients with continent urinary diversion with the mitrofanoff principle. Int Braz J Urol 46:743–751. https://doi.org/10.1590/s1677-5538.ibju.2019.0388
Beierwaltes P, Church P, Gordon T, Ambartsumyan L (2020) Bowel function and care: guidelines for the care of people with spina bifida. J Pediatr Rehabil Med 13:491–498. https://doi.org/10.3233/PRM-200724
Ambartsumyan L, Rodriguez L (2018) Bowel management in children with spina bifida. J Pediatr Rehabil Med 11:293–301. https://doi.org/10.3233/PRM-170533
Szymanski KM, Szymanski AJ, Salama AK et al (2020) Estimating and tracking renal function in children and adults with spina bifida. J Pediatr Urol 16:169–177. https://doi.org/10.1016/j.jpurol.2019.12.009
Zhou G, Jiang M, Liu X et al (2022) Measurement and estimation of glomerular filtration rate in children with neurogenic bladder: a prospective study. Urology 170:174–178. https://doi.org/10.1016/j.urology.2022.08.004
Stepanczuk BC, Dicianno BE, Webb TS (2014) Young adults with spina bifida may have higher occurrence of prehypertension and hypertension. Am J Phys Med Rehabil 93:200–206. https://doi.org/10.1097/PHM.0b013e3182a92b03
Mazur L, Lacy B, Wilsford L (2011) The prevalence of hypertension in children with spina bifida: spina bifida and hypertension. Acta Paediatr 100:e80–e83. https://doi.org/10.1111/j.1651-2227.2011.02225.x
Ramachandra P, Palazzi KL, Holmes NM, Chiang G (2014) Children with spinal abnormalities have an increased health burden from upper tract urolithiasis. Urology 83:1378–1382. https://doi.org/10.1016/j.urology.2013.12.050
Salama AK, Misseri R, Hollowell N et al (2021) Incidence of nephrolithiasis after bladder augmentation in people with spina bifida. J Pediatr Urol 17:521.e1-521.e7. https://doi.org/10.1016/j.jpurol.2021.03.012
Ekberlİ G, Taner S (2023) Risk determination for upper urinary tract damage in children with neuropathic bladder. J Paediatr Child Health. https://doi.org/10.1111/jpc.16402
Bagińska J, Korzeniecka-Kozerska A (2021) Non-invasive markers in the management of pediatric neurogenic bladder over the last two decades – a review. Adv Med Sci 66:162–169. https://doi.org/10.1016/j.advms.2021.02.001
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Answers: B, D, D, C, B.
The original online version of this article was revised: In the Multiple Choice Questions section, the questions and answers were corrected in their assignment.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Brownrigg, N., Lorenzo, A.J., Rickard, M. et al. The urological evaluation and management of neurogenic bladder in children and adolescents—what every pediatric nephrologist needs to know. Pediatr Nephrol 39, 409–421 (2024). https://doi.org/10.1007/s00467-023-06064-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-023-06064-z