Abstract
Background
From 2006 to 2020, 24% of children starting haemodialysis in France weighed < 20 kg. Most new-generation long-term haemodialysis machines do not propose paediatric lines anymore but Fresenius has validated two devices for use in children above 10 kg. Our aim was to compare the daily use of these two devices in children < 20 kg.
Methods
Retrospective single-center evaluation of daily practice with Fresenius 6008® machines, and low-volume paediatric sets (83 mL), as compared to 5008® machines with paediatric lines (108 mL). Each child was treated randomly with both generators.
Results
A total of 102 online haemodiafiltration sessions were performed over 4 weeks in five children (median body weight 12.0 [range 11.5–17.0] kg). Arterial aspiration and venous pressures were maintained respectively over − 200 mmHg and under 200 mmHg. For all children, blood flow and volume treated per session were lower with 6008® vs. 5008® (p < 0.001), median difference between the two devices being 21%. In the four children treated in post-dilution mode, substituted volume was lower with 6008® (p < 0.001, median difference: 21%). Effective dialysis time was not different between the two generators; however, the difference between total duration of session and dialysis effective time was slightly higher (p < 0.05) with 6008® for three patients, due to treatment interruptions.
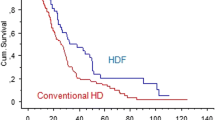
Conclusion
These results suggest that children between 11 and 17 kg should be treated with paediatric lines on 5008® if possible. They advocate for modification of the 6008 paediatric set to decrease resistance to blood flow. The possibility to use 6008® with paediatric lines in children below 10 kg deserves further studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Among the 748 children treated with maintenance haemodialysis (HD) in France from 2006 to 2020, 5% weighed less than 10 kg, 19% between 10 and 20 kg and 34% between 20 and 40 kg at HD initiation (unpublished data from the French Réseau Epidemiologique et Information en Néphrologie, REIN, registry). Low intra and extravascular volumes and small vascular access are two major issues in children on HD. Guidelines recommend that the extracorporeal volume must be less than 10% of the blood volume and therefore less than 8 mL/kg [1]. Fresenius Medical Care® offers paediatric and adult lines with volumes of 108 mL and 136 mL for the 5008® device and 83 mL and 122 mL for the 6008® device, respectively. Thus in theory, according to guidelines and knowing that the smallest available dialyzers have a priming volume of 17 mL (Gambro Polyflux2H) and 18 mL (Fresenius FxPaed), the paediatric set of the 6008® allows dialysis of children from 12.5 kg (extracorporeal volume of 100 mL) and the 5008® from 15.6 kg (extracorporeal volume of 125 mL). The manufacturer’s operating manual indicates an ultrafiltration (UF) accuracy of ± 1% UF plus ± 0.1% dialysate flow rate for these two devices. As such, 5008® and 6008® devices are the only chronic HD devices used in Europe and certified to be used in children above 10 kg. Blood flow is the main factor of dialysis efficacy and is limited by the quality of the vascular access and lines. It is recommended to maintain arterial aspiration pressure (AP) above − 200 mmHg and venous pressure (VP) lower than 200 mmHg to limit haemolysis, as well as a recirculation rate lower than 10% [1]. We report here our local experience of paediatric sets and devices proposed by Fresenius® in real life in our five smallest patients at the time of the evaluation.
Methods
We performed a retrospective single-center evaluation of daily practice with novel Fresenius 6008® dialysis machines, using low-volume paediatric sets, as compared to 5008® machines with paediatric lines. Each child underwent haemodiafiltration (HDF) with both devices in random order. All dialysis sessions were performed on a central venous catheter 8Fr–18 cm Medcomp Hemo-cathLT®. The duration of HDF session was constant during the study period. Blood flow was adjusted regularly by nurses during the dialysis sessions in order to optimize dialysis efficiency, keeping AP and VP within the recommended range. The average blood flow was calculated, using the volume treated per session and effective duration of session. The substitution rate was set by default to auto-sub. In predilution mode, after 15 to 30 min of treatment, if substitution flow was less than 75% of the blood flow, nurses manually adjusted the substitution flow. Effective dialysis time is the time during which there have been exchanges between blood and dialysate, whereas total session time is the time between connection and disconnection. The latter includes interruptions due to pressure alarms. Results were presented as median (minimum–maximum). Mann–Whitney tests were used to compare the distribution of data for each child. The median of the medians of differences observed in each child was calculated as a descriptive variable. This retrospective chart review was approved by the local IRB (Comité d’Ethique des Hospices Civils de Lyon, session 05/12/2022, number 22_5058).
Results
From 19/04/2022 to 13/05/2022, 102 sessions were performed in five children weighing 12.0 (11.5–17.0) kg and aged 2.9 (2.5–3.7) years. For all children, blood flow and volume treated were 25% and 21% lower with 6008® vs. 5008®, respectively (p < 0.001 for each child). In the four children treated in post-dilution mode, substituted volume was 21% lower with 6008® vs. 5008® (p < 0.001 for each child). Effective dialysis time was not different between the two generators; however, the difference between total session duration and effective dialysis time was slightly higher for three out of five patients with 6008® vs. 5008® (p < 0.001), due to treatment interruptions. For the last two patients, a similar trend was observed, however without reaching statistical significance. Lactate dehydrogenase (LDH) and haptoglobin serum levels measured at the end of sessions were not different between the two generators. Table 1 summarizes these data, patient per patient.
Discussion
Ultrafiltration accuracy is of major importance in the youngest children to maintain haemodynamic stability during sessions and thus prevent ischemic damages [2,3,4,5]. This accuracy was found to be poor in an in vitro study of two available continuous kidney replacement therapy machines [6], and ranges from 20 to 50 mL per hour according to the user manuals of the maintenance HD machines; it depends on the type of long-term HD machine and the dialysis modality. In addition, the maximum recommended extracorporeal blood volume is 10% of the patient’s total blood volume [1]. These elements explain that there are no maintenance HD machines still available and cleared in Europe for use in children below 10 kg and only one machine for children between 10 and 20 kg, namely the Fresenius 6008® device.
Paediatricians are grateful to the last two manufacturers still offering small volume lines in Europe, i.e. Baxter with AK98® device (36, 85, and 100 mL) and Fresenius with 4008® (56 mL) and 6008® (85 mL) devices. Of these, only Fresenius devices can be used for HDF. The former Fresenius 5008® device with paediatric line of 108 mL is still used in numerous paediatric units but is not produced anymore. For the Fresenius 6008® lines, the extracorporeal volume of the paediatric set has been reduced compared to the adult 6008® set by using thinner lines on the outside of the pump. The Fresenius 6008® paediatric lines are longer than those of the 5008® paediatric set and have a smaller diameter both for the venous and the arterial lines; for example, for the venous line we measured a length of 230 cm (versus 185), an external diameter of 4.3 mm (versus 5.5) and an internal diameter of 2.7 mm (versus 3.8) in the 6008® paediatric lines, as compared to the 5008® paediatric lines (respective values for 6008® adult lines of 196 cm, 7 mm and 4.8 mm, respectively). Smaller extracorporeal circuits should nevertheless allow sufficient blood flow rate, as this is a major parameter for achieving substitution targets [7, 8], as well as dialysis adequacy in a limited time [1]. Through this report, we want to highlight the fact that devices with lower volume lines can do worse than devices with relatively higher volume. Indeed, when comparing the two devices 5008® and 6008® with paediatric lines in our five smallest patients at the time of the retrospective evaluation, blood flow, blood treated and substituted volumes obtained with 6008® were lower than with 5008® to maintain AP and VP within the recommended ranges. In the current absence of an effective solution from manufacturers, we have chosen to keep the 5008® generator for patients weighing 10 to 17 kg and we use the 6008® device with paediatric set in children below 10 kg as an off-label use. This practice in these latter children deserves further studies.
Our results advocate for modification of 6008® device paediatric set with shorter and larger diameter tubing in order to decrease resistance to blood flow and thus enable higher blood flow rate and dialysis efficiency.
The Fresenius 6008® is a new generation device that offers patients weighing more than 40 kg many useful options such as online monitoring of urea clearance, blood volume controlled ultrafiltration, temperature control, assessment of vascular access recirculation, monitoring and control of sodium transfer during HD sessions [9] as well as the possibility to switch during the session from double-needle to single-needle mode without changing the blood lines. We regret that these options are not offered to patients weighing less than 40 kg and plea for a more intensive partnership with industrial partners so as to allow the smallest children to have access to the same quality and efficiency of equipment as the one offered to adult patients [10].
References
Fischbach M, Edefonti A, Schröder C, Watson A, European Pediatric Dialysis Working Group (2005) Hemodialysis in children: general practical guidelines. Pediatr Nephrol 20:1054–1066. https://doi.org/10.1007/s00467-005-1876-y2
Moore J, Klowak J, Isaza G, Arora S, Belostotsky V, Stein N, Chanchlani R (2020) Anterior ischemic optic neuropathy in a child receiving chronic hemodialysis. Case Rep Nephrol 2020:7012586. https://doi.org/10.1155/2020/7012586
Harshman LA, Hooper SR (2020) The brain in pediatric chronic kidney disease-the intersection of cognition, neuroimaging, and clinical biomarkers. Pediatr Nephrol 35:2221–2229. https://doi.org/10.1007/s00467-019-04417-1
Idrovo A, Pignatelli R, Loar R, Nieuwsma A, Geer J, Solomon C, Swartz S, Ghanayem N, Akcan-Arikan A, Srivaths P (2021) Preserved cerebral oxygenation with worsening global myocardial strain during pediatric chronic hemodialysis. J Am Soc Nephrol 32:2912–2919. https://doi.org/10.1681/ASN.2021020193
Hothi DK, Rees L, Marek J, Burton J, McIntyre CW (2009) Pediatric myocardial stunning underscores the cardiac toxicity of conventional hemodialysis treatments. Clin J Am Soc Nephrol 4:790–797. https://doi.org/10.2215/CJN.05921108
Crosier J, Whitaker M, Lambert HJ, Wellman P, Nyman A, Coulthard MG (2022) In vitro measurements of ultrafiltration precision in hemofiltration and hemodialysis devices used in infants. Pediatr Nephrol 37:3189–3194. https://doi.org/10.1007/s00467-022-05439-y
Peters SA, Bots ML, Canaud B, Davenport A, Grooteman MPC, Kircelli F, Locatelli F, Maduell F, Morena M, Nubé MJ, Ok E, Torres F, Woodward M, Blankestijn PJ, HDF Pooling Project Investigators (2016) Haemodiafiltration and mortality in end-stage kidney disease patients: a pooled individual participant data analysis from four randomized controlled trials. Nephrol Dial Transplant 31:978–984. https://doi.org/10.1093/ndt/gfv349
Kikuchi K, Hamano T, Wada A, Nakai S, Masakane I (2019) Predilution online hemodiafiltration is associated with improved survival compared with hemodialysis. Kidney Int 95:929–938. https://doi.org/10.1016/j.kint.2018.10.036
Sagova M, Wojke R, Maierhofer A, Gross M, Canaud B, Gauly A (2019) Automated individualization of dialysate sodium concentration reduces intradialytic plasma sodium changes in hemodialysis. Artif Organs 43:1002–1013. https://doi.org/10.1111/aor.13463
Ranchin B, Schmitt CP, Warady B, Craig JC, Licht C, Hataya H, Vidal E, Vande Walle J, Shroff R (2023) Devices for long-term hemodialysis in small children – a plea for action. Kidney Int. https://doi.org/10.1016/j.kint.2023.03.018
Acknowledgements
The authors thank Pr Rukshana Shroff and Mrs Lynsey Stronach, Great Ormond Street Hospital, London (UK), for sharing their experience on the use of 6008 devices and to Dr Mathilde Lassalle from the Réseau Epidemiologique et Information en Néphrologie (REIN) registry for data extraction.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mosca, M., Kouajip-Mabou, A., De Mul, A. et al. Daily practice evaluation of the paediatric set of a next-generation long-term haemodialysis machine. Pediatr Nephrol 38, 3863–3866 (2023). https://doi.org/10.1007/s00467-023-05943-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-023-05943-9