Abstract
Background
Hypogammaglobulinemia is a major adverse effect from rituximab. However, the association between rituximab-induced hypogammaglobulinemia and infection frequency is unknown.
Methods
Patients who received rituximab for complicated nephrotic syndrome between February 2006 and October 2020 were enrolled in this retrospective observational study. Infections requiring antibacterial or antiviral agents or hospitalization were identified, and the characteristics of infections were compared according to infection type.
Results
One hundred and forty patients were enrolled. Fifty infection events were detected in 36 patients, 45 infection events in 32 patients required hospitalization, and 1 severe infection event required intensive care unit admission. In eight patients who developed severe hypogammaglobulinemia (serum IgG level < 200 mg/dL) for more than 1 year after rituximab treatment, eight infections occurred in six patients; six of these infections did not occur during the period of severe hypogammaglobulinemia. Febrile neutropenia accounted for 54.2% (13/24) of all infections among the patients with hypogammaglobulinemia. The incidence of infections was 0.028 (95% confidence interval = 0.017–0.448), 0.071 (95% [CI] = 0.041–0.114), and 0.096 (95% [CI] = 0.019–0.282) patient-years in patients with normal serum IgG levels and those with mild and severe hypogammaglobulinemia, respectively. Immunoglobulin replacement therapy was not administered to any patients except for the treatment of infection.
Conclusions
Our results showed no statistically significant association between hypogammaglobulinemia severity and infection rate. In addition, the frequency of infection was relatively low even in patients with severe hypogammaglobulinemia, suggesting that immunoglobulin replacement therapy may not be necessary for rituximab-treated patients with severe hypogammaglobulinemia.
Graphical abstract
A higher resolution version of the Graphical abstract is available as Supplementary information.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rituximab is an anti-CD20 monoclonal antibody, which is an effective and relatively safe treatment for patients with complicated steroid-dependent or frequently relapsing nephrotic syndrome (SDNS/FRNS) [1, 2], and also could be an effective treatment for multidrug-resistant steroid-resistant nephrotic syndrome (SRNS) [3]. Rituximab binds to CD20 and leads to B-cell depletion and dysfunction, which can impact T cell immunity and reduce immunoglobulin levels [4]. In addition to B- and T-cell-mediated immunosuppression, rituximab may also induce neutropenia. These effects of rituximab on the immune system may increase the incidence of infection after rituximab treatment [4, 5].
The incidence of infections and hypogammaglobulinemia after rituximab treatment differs among patients with primary diseases [5,6,7,8]. Several studies reported that the incidence of hypogammaglobulinemia ranged between 11 and 58% after rituximab treatment in patients with childhood-onset SDNS [9,10,11,12,13]. Most patients develop transient and mild hypogammaglobulinemia, with their serum immunoglobulin G (IgG) levels returning to baseline within a year; however, some patients develop severe persistent hypogammaglobulinemia and require immunoglobulin replacement treatment [9, 14,15,16].
Whether rituximab-induced hypogammaglobulinemia is associated with increased infection risk is unclear. Moreover, it remains unclear whether persistent severe hypogammaglobulinemia after rituximab treatment, which might require immunoglobulin replacement therapy, results in severe and recurrent infection in patients with SDNS/FRNS or SRNS. The threshold for the initiation of immunoglobulin replacement therapy after rituximab treatment varies based on the underlying conditions in the absence of formal guidelines [16]. Therefore, it is crucial to determine the incidence of infection and the association between the degree of immunoglobulin deficiency and infection among patients with SDNS/FRNS or SRNS.
In the present study, we investigated the association between the severity of hypogammaglobulinemia and the risk of infection after rituximab treatment in patients with complicated SDNS/FRNS or SRNS.
Methods
Study design and patient population
In this retrospective observational study, we enrolled patients with childhood-onset complicated SDNS/FRNS or SRNS who were treated with rituximab between February 1, 2006, and October 31, 2020, in the National Center for Child Health and Development in Tokyo. Patients who were followed for less than 6 months after rituximab treatment and those without available data on serum IgG levels were excluded. The last follow-up was October 31, 2021.
SDNS was defined as two consecutive relapses during tapering or within 2 weeks of stopping steroid treatment. FRNS was defined as two or more relapses within the first 6 months of remission or four or more relapses within any 12-month period. SRNS was defined as persistent proteinuria after 4 weeks of treatment with 60 mg/m2/day oral prednisolone. Complicated nephrotic SDNS/FRNS was defined as the development of SDNS or FRNS under immunosuppressive agents. B-cell depletion was defined as a peripheral blood CD19+ or CD20+ B-cell count of < 1% of the total number of lymphocytes, and B-cell recovery was defined as a peripheral blood CD19+ or CD20+ B-cell count of ≥ 1% of the total number of lymphocytes. Hypogammaglobulinemia was categorized as mild (serum IgG level, 200–500 mg/dL) or severe (serum IgG level, < 200 mg/dL) [6, 14, 17, 18]. Persistent severe hypogammaglobulinemia was defined as a serum IgG level of < 200 mg/dL for more than 1 year after rituximab treatment initiation. In the present study, infections were defined as events requiring antiviral or antibacterial treatment or hospitalization during the follow-up period.
Treatment protocol
Rituximab was administered at a single dose of 375 mg/m2, two doses of 375 mg/m2 every 2 weeks, or 4 weekly doses of 375 mg/m2 as a single course. CD19+ or CD20+ B-cell counts were assessed once every 1–2 months by flow cytometry until B-cell recovery was observed. Oral immunosuppressive treatments were continued after rituximab treatment. Relapses were treated with 60 mg/m2 prednisolone daily, with a maximum daily dose of 60 mg. Prednisolone was tapered off within 2–3 months after remission. Starting in January 2012, trimethoprim-sulfamethoxazole, with a trimethoprim dose of 5 mg/kg, was administered once every 2 days during B-cell depletion for Pneumocystis jiroveci pneumonia prophylaxis. In patients with fever during B-cell depletion, extensive assessments including blood tests, chest X-ray, urinalysis, and blood culture were immediately performed.
Data collection and analysis
The following clinical data were extracted using chart review: sex, age at onset of nephrotic syndrome, age at initiation of rituximab treatment, immunosuppressive agents during and after rituximab treatment, number of rituximab treatments, history of SRNS, use of IgG replacement therapy, and characteristics of infections requiring antibacterial or antiviral agents or hospitalization during the follow-up period. The laboratory data included serum IgG and albumin levels once every 1–2 months after rituximab treatment, complete blood count, C-reactive protein level, and serum IgG level during infection. Serum IgG levels with serum albumin levels < 3.0 g/dL were excluded to minimize the effect of urinary leakage of IgG.
The enrolled patients were divided into two groups. Patients who exhibited severe hypogammaglobulinemia for more than 1 year after rituximab treatment were categorized into the persistent severe hypogammaglobulinemia group; whereas patients who never developed severe hypogammaglobulinemia during the period of at least 1 year after rituximab treatment were categorized into the other group. Patient characteristics were compared between the two groups. The characteristics of infection events were compared according to type of infection to assess the relationship between the infection type and the severity of hypogammaglobulinemia. The association between severe hypogammaglobulinemia and infection was estimated using patient-year analysis. In the present study, person-time was defined as the period between the first rituximab course and last follow-up date. Person-time with normal serum IgG levels, mild hypogammaglobulinemia (serum IgG level, 200–500 mg/dL), or severe hypogammaglobulinemia (serum IgG level, < 200 mg/dL) was measured for each patient. Infection events during the relapse of nephrotic syndrome were excluded in patient-year analysis.
Statistical analysis
Data were expressed as medians with the interquartile ranges (IQRs) for continuous variables and percentages for categorical variables. The Mann–Whitney U test was used to compare continuous variables, and Fisher’s exact test was used to compare categorical variables. A P value of < 0.05 was considered to indicate statistical significance. Statistical analyses were performed using JMP version 14.0 (SAS Institute Japan, Tokyo, Japan) and Stata/SE 17.0 (StataCorp LLC, College Station, TX).
Results
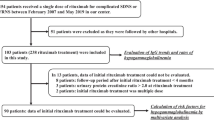
Patient characteristics
During the study period, 140 of the 207 patients who were administered rituximab for complicated SDNS/FRNS fulfilled the inclusion criteria (Fig. 1). Patient characteristics are shown in Table 1. In the entire study cohort, 41 patients received one course of rituximab whereas the remaining patients received more than one course. None of the patients received IgG replacement therapy. At the time of last follow-up, eight patients (5.7%) had developed persistent severe hypogammaglobulinemia. Age at onset of nephrotic syndrome was significantly lower in the persistent severe hypogammaglobulinemia group than in the other group (P = 0.03). Age at first rituximab treatment was also significantly lower in the persistent severe hypogammaglobulinemia group than in the other group (P = 0.004).
Figure 2 shows the clinical course of patients with persistent severe hypogammaglobulinemia. Briefly, the median age at onset and median duration of persistent severe hypogammaglobulinemia were 8.1 (IQR 5.2–12.8) and 2.6 (IQR 1.2–5.3) years, respectively. Two patients developed persistent severe hypogammaglobulinemia at age < 4 years and achieved normalized serum IgG levels within 2 years after developing persistent severe hypogammaglobulinemia. The remaining six patients developed persistent severe hypogammaglobulinemia at age ≥ 7 years and did not achieve normalized serum IgG levels at last follow-up.
Clinical course of patients who developed persistent severe hypogammaglobulinemia after rituximab treatment. Boxes indicate the period between the age at onset and the age at last follow-up, crosses indicate infections, triangles indicate rituximab treatment, and gray lines indicate the duration of severe hypogammaglobulinemia
Infections
Table 2 shows the characteristics of infection events. During the follow-up period, 50 infection events occurred in 36 patients and 45 infection events in 32 patients required hospitalization. Of these, 21, 15, 8, 7, 2, and 1 event included febrile neutropenia, varicella-zoster virus infection, bacterial infection, pneumonia, herpetic gingivostomatitis, and mumps meningitis, respectively (4 events were mixed infections). The median age at the time of infection was 8.4 (IQR 5.4–13.3) years. Infection requiring intensive care unit admission occurred in one patient who developed Pneumocystis jiroveci pneumonia, and no deaths occurred. A detailed description of this patient was previously reported [19]. The median duration of hospitalization was 8.5 (IQR 7.0–10.0) days.
The characteristics of the patients with infection were compared with those of the patients without infection during follow-up period. The number of patients with less than one oral immunosuppressive agent was not significantly higher in patients with infection (0%, P = 0.57) than patients without infection (2.9%).
Association between the degree of hypogammaglobulinemia and infection
Table 3 shows the characteristics of infections categorized according to the infection type. Of the four patients with mixed infections, one patient with viral pneumonia and febrile neutropenia was categorized in the pneumonia group, one patient with bacterial pneumonia and pneumococcal bacteremia was categorized in the bacterial infection group, and two patients with febrile neutropenia and herpetic gingivostomatitis were categorized in the febrile neutropenia group. Infections with hypogammaglobulinemia accounted for 57.1% (24/42) of all infections and febrile neutropenia accounted for 54.2% (13/24) of all infections with hypogammaglobulinemia. During the follow-up period including the relapse of nephrotic syndrome, seven infections with severe hypogammaglobulinemia were recorded: varicella-zoster virus infection (n = 2), febrile neutropenia (n = 1), bacterial pneumonia with pneumococcal bacteremia (n = 1), bacteremia with peritonitis (n = 1), bacteremia (n = 1), and Pneumocystis jiroveci pneumonia (n = 1). All except one patient who suffered from bacterial pneumonia with pneumococcal bacteremia were treated with intravenous immunoglobulin, and all except one patient who suffered from Pneumocystis jiroveci pneumonia improved immediately after treatment.
In the persistent severe hypogammaglobulinemia group, eight infections occurred in six patients (75.0%), six infections (75.0%) were in the absence of severe hypogammaglobulinemia, and recurrent infection occurred in one patient during a follow-up period of 13 years (Fig. 2). The patient with Pneumocystis jiroveci pneumonia developed persistent severe hypogammaglobulinemia for more than 1 year after the infection event, but did not develop recurrent infection. Table 4 shows the incidence density of infections stratified by the period of each severity of hypogammaglobulinemia. The overall incidence of infections was 0.055 patient-years. The incidence density of infections was similar in patients with normal serum IgG levels and those with mild and severe hypogammaglobulinemia: 0.028 (95% confidence interval [CI] = 0.017–0.448), 0.071 (95% [CI] = 0.041–0.114), and 0.096 (95% [CI] = 0.019–0.282), respectively.
Pneumocystis jiroveci pneumonia prophylaxis after rituximab treatment
Of the 140 patients who fulfilled the inclusion criteria, 120 patients (85.7%) received Pneumocystis jiroveci pneumonia prophylaxis after rituximab treatment more than once whereas three patients did not receive prophylaxis due to drug allergy. None of the patients developed Pneumocystis jiroveci pneumonia after the initiation of Pneumocystis jiroveci pneumonia prophylaxis (Table 2).
Discussion
The present single-center retrospective study investigated the association between the severity of hypogammaglobulinemia and the risk of infection in patients with childhood-onset complicated SDNS/FRNS or SRNS treated with rituximab. Our analyses revealed that the incidence of infections was similar between patients with severe hypogammaglobulinemia and those with normal serum IgG levels. Moreover, the incidence of infections in patients with severe hypogammaglobulinemia was low (0.096 patient-years) and all except one patient had a favorable clinical course. Febrile neutropenia, which is rarely attributable to serum IgG levels, was the most common infection in patients with hypogammaglobulinemia.
Clinical trials have reported conflicting results regarding the association of rituximab-induced hypogammaglobulinemia with infection. In adult patients with rheumatoid arthritis and autoimmune diseases, a serum IgG level below 600 mg/dL was an independent risk factor for the development of post-rituximab infection [20]. In adult patients with anti-neutrophil cytoplasmic antibody-associated vasculitis, severe hypogammaglobulinemia, which was defined as a serum IgG level below 375 mg/dL, was reported to be associated with increased odds of severe infection [21]. In contrast, other studies failed to observe an association between rituximab-induced hypogammaglobulinemia and infection [17, 22, 23]. These contradictory findings might be related to the differences in immunosuppressive regimens and the underlying conditions among the studies. In a study of patients with childhood-onset SDNS who were treated with rituximab, Cyrielle et al. reported that 13 infections occurred in 46 patients who developed hypogammaglobulinemia [10]. Fujinaga et al. also reported that seven infections occurred in seven patients with persistent hypogammaglobulinemia who received mycophenolate mofetil after rituximab treatment and that infection events did not occur in two patients with persistent hypogammaglobulinemia who received cyclosporin A after rituximab treatment [11]. However, the association between rituximab-induced hypogammaglobulinemia and infection in childhood-onset idiopathic nephrotic syndrome remains unclear.
To our knowledge, this is the first study demonstrating the relationship between the severity of rituximab-induced hypogammaglobulinemia and infection in childhood-onset idiopathic nephrotic syndrome. In the present study, the incidence density of infections in patients with severe hypogammaglobulinemia was still low (0.096 per person-years) although the incidence density of infections was slightly higher in patients with severe hypogammaglobulinemia than in those with normal serum IgG levels or mild hypogammaglobulinemia. Two previous studies on patients with childhood-onset autoimmune diseases who were treated with rituximab reported that the incidence densities were 0.078 and 0.087 for hospitalized infections after rituximab treatment [24, 25]. Interestingly, these incidence densities were higher than the overall incidence density (0.055 per person-years) observed in the present study, suggesting that the rate of infection might be low in patients with childhood-onset idiopathic nephrotic syndrome.
Whether rituximab treatment in patients with nephrotic syndrome increases the risk of infection remains unclear. A previous study on patients with nephrotic syndrome reported that 57% (4/7) of patients with rituximab treatment developed a bacterial infection, and 43% (25/58) of patients with other immunosuppressive agents developed bacterial infections [26]. Our study reported that 5.7% (8/140) of patients developed bacterial infection. Moreover, the incidence of pneumonia, which was one of the most common infections in patients with nephrotic syndrome [27], was 1.57–17.37 per 1000 person-years in previous studies on healthy children [28, 29] and 7.73 per 1000 person-years (7/905.8) in our study. This shows that the risk of pneumonia in our patients was almost similar to healthy children.
The type of infection is another important aspect regarding the relationship between hypogammaglobulinemia and infection. Bacterial and respiratory infections are the two most common infection types in patients with hypogammaglobulinemia [30, 31]. In the present study, febrile neutropenia accounted for 54.2% (13/24) of all infections with hypogammaglobulinemia, suggesting that some infections in the presence of hypogammaglobulinemia might be the result of a mechanism other than low serum IgG levels.
To date, no specific guidelines exist for managing drug-induced hypogammaglobulinemia and the threshold for the initiation of immunoglobulin replacement therapy after rituximab treatment depends on specific underlying conditions [16, 32]. The UK Department of Health clinical guidelines on all causes of secondary antibody deficiency recommend the initiation of immunoglobulin replacement therapy in the following patients: (i) those whose underlying cause of hypogammaglobulinemia cannot be reversed and (ii) those who develop hypogammaglobulinemia (serum IgG level < 500 mg/dL), with a history of severe or recurrent bacterial infection despite the use of prophylactic oral antibiotics for 3 months, and with functional antibody deficiency [33]. A study on autoimmune diseases suggested severe hypogammaglobulinemia, defined as a serum IgG level below 200 mg/dL, as a criterion for immunoglobulin replacement therapy initiation after rituximab treatment in patients with recurrent severe infections, especially respiratory system and bacterial infections, and functional antibody deficiency [31]. In the present study, only one of the eight patients who developed persistent severe hypogammaglobulinemia developed recurrent infections during the long follow-up period and only one patient had a severe infection requiring intensive care unit admission. Considering the abovementioned threshold, the current study patients may not meet the indications for immunoglobulin replacement therapy.
The drawbacks of immunoglobulin replacement therapy, including the need for frequent hospital visits to receive immunoglobulin replacement because of the short medication half-life, insufficiency to prevent major causes of infection such as febrile neutropenia, and high cost, should be considered [3, 34]. In the present study, we could not assess the efficacy of immunoglobulin replacement therapy as none of the study patients received the treatment. However, our study showed the following results, which raised the possibility that immunoglobulin replacement therapy might not be necessary in patients with childhood-onset complicated SDNS/FRNS or SRNS who develop persistent severe hypogammaglobulinemia after rituximab treatment: (i) infections in the persistent severe hypogammaglobulinemia group mainly occurred when the patients did not develop severe hypogammaglobulinemia; (ii) infection rates in patient-year analysis were low; and (iii) more than half of the infections were rarely attributable to serum IgG levels.
The present study has several limitations that should be acknowledged. First, serum IgG levels were not strictly monitored due to the retrospective study design and serum IgG levels during infection were missing in some cases. Second, although the data of serum IgG levels with serum albumin levels of < 3.0 g/dL was excluded to minimize the possibility of urinary loss, the serum IgG levels still could be affected by urinary loss. However, persistent severe hypogammaglobulinemia was not caused by the urinary loss of IgG, as proteinuria did not persist for long time periods in the enrolled patients. Third, potential confounders of susceptibility to infection should be considered. This study included patients with childhood-onset complicated SDNS/FRNS or SRNS treated with rituximab, who had one or two oral immunosuppressive therapies and might have several recurrent relapses during the follow-up period. During the relapse period, several factors other than rituximab-induced immunosuppression, such as steroid treatment, hypoalbuminemia and urinary loss of complement factor, and immunoglobulin, could cause infection. However, almost all patients in the present study had oral immunosuppressive treatments after rituximab treatment, and infection events during the relapse period were excluded in patient-year analysis, which helped to reduce the confounding factor to estimate the relationship between rituximab-induced hypogammaglobulinemia and infection rate.
In conclusion, our findings suggest a weak association between the severity of hypogammaglobulinemia and infection in patients with complicated SDNS/FRNS or SRNS. Our patients, including the persistent severe hypogammaglobulinemia group, may not have had recurrent or severe infections enough to meet the indications for immunoglobulin replacement therapy. Additional studies are warranted to further interrogate the association between hypogammaglobulinemia and infection and to determine the threshold for the initiation of immunoglobulin replacement therapy after rituximab treatment.
Data availability
The data from this study are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
References
Kamei K, Ishikura K, Sako M, Aya K, Tanaka R, Nozu K, Kaito H, Nakanishi K, Ohtomo Y, Miura K, Takahashi S, Morimoto T, Kubota W, Ito S, Nakamura H, Iijima K (2017) Long-term outcome of childhood-onset complicated nephrotic syndrome after a multicenter, double-blind, randomized, placebo-controlled trial of rituximab. Pediatr Nephrol 32:2071–2078. https://doi.org/10.1007/s00467-017-3718-0
Iijima K, Sako M, Nozu K, Mori R, Tuchida N, Kamei K, Miura K, Aya K, Nakanishi K, Ohtomo Y, Takahashi S, Tanaka R, Kaito H, Nakamura H, Ishikura K, Ito S, Ohashi Y (2014) Rituximab for childhood-onset, complicated, frequently relapsing nephrotic syndrome or steroid-dependent nephrotic syndrome: a multicentre, double-blind, randomised, placebo-controlled trial. Lancet 384:1273–1281. https://doi.org/10.1016/S0140-6736(14)60541-9
Trautmann A, Vivarelli M, Samuel S, Gipson D, Sinha A, Schaefer F, Hui NK, Boyer O, Saleem MA, Feltran L, Muller-Deile J, Becker JU, Cano F, Xu H, Lim YN, Smoyer W, Anochie I, Nakanishi K, Hodson E, Haffner D, International Pediatric Nephrology Association (2020) IPNA clinical practice recommendations for the diagnosis and management of children with steroid-resistant nephrotic syndrome. Pediatr Nephrol 35:1529–1561. https://doi.org/10.1007/s00467-020-04519-1
Kelesidis T, Daikos G, Boumpas D, Tsiodras S (2011) Does rituximab increase the incidence of infectious complications? A narrative review. Int J Infect Dis 15:e2–e16. https://doi.org/10.1016/j.ijid.2010.03.025
Christou EAA, Giardino G, Worth A, Ladomenou F (2017) Risk factors predisposing to the development of hypogammaglobulinemia and infections post-rituximab. Int Rev Immunol 36:352–359. https://doi.org/10.1080/08830185.2017.1346092
Barmettler S, Ong MS, Farmer JR, Choi H, Walter J (2018) Association of immunoglobulin levels, infectious risk, and mortality with rituximab and hypogammaglobulinemia. JAMA Netw Open 1:e184169. https://doi.org/10.1001/jamanetworkopen.2018.4169
Worch J, Makarova O, Burkhardt B (2015) Immunreconstitution and infectious complications after rituximab treatment in children and adolescents: what do we know and what can we learn from adults? Cancers (Basel) 7:305–328. https://doi.org/10.3390/cancers7010305
Kavcic M, Fisher BT, Seif AE, Li Y, Huang YS, Walker D, Aplenc R (2013) Leveraging administrative data to monitor rituximab use in 2875 patients at 42 freestanding children’s hospitals across the United States. J Pediatr 162:1252–1258. https://doi.org/10.1016/j.jpeds.2012.11.038
Inoki Y, Kamei K, Nishi K, Sato M, Ogura M, Ishiguro A (2022) Incidence and risk factors of rituximab-associated hypogammaglobulinemia in patients with complicated nephrotic syndrome. Pediatr Nephrol 37:1057–1066. https://doi.org/10.1007/s00467-021-05304-4
Parmentier C, Delbet JD, Decramer S, Boyer O, Hogan J, Ulinski T (2020) Immunoglobulin serum levels in rituximab-treated patients with steroid-dependent nephrotic syndrome. Pediatr Nephrol 35:455–462. https://doi.org/10.1007/s00467-019-04398-1
Fujinaga S, Tomii Y (2020) Profound effect of post-rituximab mycophenolate mofetil administration for persistent hypogammaglobulinemia in young children with steroid-dependent nephrotic syndrome. Clin Exp Nephrol 24:386–387. https://doi.org/10.1007/s10157-020-01858-z
Marzuillo P, Guarino S, Esposito T, Sessa AD, Orsini SI, Capalbo D, Giudice EMd, Manna AL (2019) Rituximab-induced IgG hypogammaglobulinemia in children with nephrotic syndrome and normal pre-treatment IgG values. World J Clin Cases 7:1021–1027. https://doi.org/10.12998/wjcc.v7.i9.1021
Fujinaga S, Ozawa K, Sakuraya K, Yamada A, Shimizu T (2016) Late-onset adverse events after a single dose of rituximab in children with complicated steroid-dependent nephrotic syndrome. Clin Nephrol 85:340–345. https://doi.org/10.5414/CN108835
Khojah AM, Miller ML, Klein-Gitelman MS, Curran ML, Hans V, Pachman LM, Fuleihan RL (2019) Rituximab-associated hypogammaglobulinemia in pediatric patients with autoimmune diseases. Pediatr Rheumatol Online J 17:61. https://doi.org/10.1186/s12969-019-0365-y
Irie E, Shirota Y, Suzuki C, Tajima Y, Ishizawa K, Kameoka J, Harigae H, Ishii T (2010) Severe hypogammaglobulinemia persisting for 6 years after treatment with rituximab combined chemotherapy due to arrest of B lymphocyte differentiation together with alteration of T lymphocyte homeostasis. Int J Hematol 91:501–508. https://doi.org/10.1007/s12185-010-0528-6
Wijetilleka S, Mukhtyar C, Jayne D, Ala A, Bright P, Chinoy H, Harper L, Kazmi M, Kiani-Alikhan S, Li C, Misbah S, Oni L, Price-Kuehne F, Salama A, Workman S, Wrench D, Karim MY (2019) Immunoglobulin replacement for secondary immunodeficiency after B-cell targeted therapies in autoimmune rheumatic disease: systematic literature review. Autoimmun Rev 18:535–541. https://doi.org/10.1016/j.autrev.2019.03.010
Casulo C, Maragulia J, Zelenetz AD (2013) Incidence of hypogammaglobulinemia in patients receiving rituximab and the use of intravenous immunoglobulin for recurrent infections. Clin Lymphoma Myeloma Leuk 13:106–111. https://doi.org/10.1016/j.clml.2012.11.011
Agarwal S, Cunningham-Rundles C (2007) Assessment and clinical interpretation of reduced IgG values. Ann Allergy Asthma Immunol 99:281–283. https://doi.org/10.1016/S1081-1206(10)60665-5
Sato M, Ito S, Ogura M, Kamei K, Miyairi I, Miyata I, Higuchi M, Matsuoka K (2013) Atypical Pneumocystis jiroveci pneumonia with multiple nodular granulomas after rituximab for refractory nephrotic syndrome. Pediatr Nephrol 28:145–149. https://doi.org/10.1007/s00467-012-2286-6
Mariette X, Gottenberg JE, Ravaud P, Combe B (2011) Registries in rheumatoid arthritis and autoimmune diseases: data from the French registries. Rheumatology (Oxford) 50:222–229. https://doi.org/10.1093/rheumatology/keq368
Shah S, Jaggi K, Greenberg K, Geetha D (2017) Immunoglobulin levels and infection risk with rituximab induction for anti-neutrophil cytoplasmic antibody-associated vasculitis. Clin Kidney J 10:470–474. https://doi.org/10.1093/ckj/sfx014
Marco H, Smith RM, Jones RB, Guerry MJ, Catapano F, Burns S, Chaudhry AN, Smith KG, Jayne DR (2014) The effect of rituximab therapy on immunoglobulin levels in patients with multisystem autoimmune disease. BMC Musculoskelet Disord 15:178. https://doi.org/10.1186/1471-2474-15-178
Keystone E, Fleischmann R, Emery P, Furst DE, van Vollenhoven R, Bathon J, Dougados M, Baldassare A, Ferraccioli G, Chubick A, Udell J, Cravets MW, Agarwal S, Cooper S, Magrini F (2007) Safety and efficacy of additional courses of rituximab in patients with active rheumatoid arthritis: an open-label extension analysis. Arthritis Rheum 56:3896–3908. https://doi.org/10.1002/art.23059
Kearsley-Fleet L, Sampath S, McCann LJ, Baildam E, Beresford MW, Davies R, De Cock D, Foster HE, Southwood TR, Thomson W, Hyrich KL (2019) Use and effectiveness of rituximab in children and young people with juvenile idiopathic arthritis in a cohort study in the United Kingdom. Rheumatology (Oxford) 58:331–335. https://doi.org/10.1093/rheumatology/key306
Tambralli A, Beukelman T, Cron RQ, Stoll ML (2015) Safety and efficacy of rituximab in childhood-onset systemic lupus erythematosus and other rheumatic diseases. J Rheumatol 42:541–546. https://doi.org/10.3899/jrheum.140863
Alfakeekh K, Azar M, Sowailmi BA, Alsulaiman S, Makdob SA, Omair A, Albanyan E, Bawazeer MS (2019) Immunosuppressive burden and risk factors of infection in primary childhood nephrotic syndrome. J Infect Public Health 12:90–94. https://doi.org/10.1016/j.jiph.2018.09.006
Wei CC, Yu IW, Lin HW, Tsai AC (2012) Occurrence of infection among children with nephrotic syndrome during hospitalizations. Nephrology (Carlton) 17:681–688. https://doi.org/10.1111/j.1440-1797.2012.01650.x
Jain S, Williams DJ, Arnold SR, Ampofo K, Bramley AM, Reed C, Stockmann C, Anderson EJ, Grijalva CG, Self WH, Zhu Y, Patel A, Hymas W, Chappell JD, Kaufman RA, Kan JH, Dansie D, Lenny N, Hillyard DR, Haynes LM, Levine M, Lindstrom S, Winchell JM, Katz JM, Erdman D, Schneider E, Hicks LA, Wunderink RG, Edwards KM, Pavia AT, McCullers JA, Finelli L, CDC EPIC Study Team (2015) Community-acquired pneumonia requiring hospitalization among U.S. children. N Engl J Med 372:835–845. https://doi.org/10.1056/NEJMoa1405870
Sun Y, Li H, Pei Z, Wang S, Feng J, Xu L, Gao P, Cao B, Zhan S (2020) Incidence of community-acquired pneumonia in urban China: a national population-based study. Vaccine 38:8362–8370. https://doi.org/10.1016/j.vaccine.2020.11.004
Furst DE (2009) Serum immunoglobulins and risk of infection: how low can you go? Semin Arthritis Rheum 39:18–29. https://doi.org/10.1016/j.semarthrit.2008.05.002
Looney RJ, Srinivasan R, Calabrese LH (2008) The effects of rituximab on immunocompetency in patients with autoimmune disease. Arthritis Rheum 58:5–14. https://doi.org/10.1002/art.23171
Roberts DM, Jones RB, Smith RM, Alberici F, Kumaratne DS, Burns S, Jayne DR (2015) Immunoglobulin G replacement for the treatment of infective complications of rituximab-associated hypogammaglobulinemia in autoimmune disease: a case series. J Autoimmun 57:24–29. https://doi.org/10.1016/j.jaut.2014.11.004
Department of Health and Social Care (2011) Clinical guidelines for immunoglobulin use: second edition update. https://www.gov.uk/government/publications/clinical-guidelines-for-immunoglobulin-use-second-edition-update. Accessed 30 October 2021
McAtee CL, Lubega J, Underbrink K, Curry K, Msaouel P, Barrow M, Muscal E, Lotze T, Srivaths P, Forbes LR, Allen C, Bernhardt MB (2021) Association of rituximab use with adverse events in children, adolescents, and young adults. JAMA Netw Open 4:e2036321. https://doi.org/10.1001/jamanetworkopen.2020.36321
Acknowledgements
The authors would like to thank Dr. Chie Nagata at the National Center for Child Health and Development for her advice on statistical analysis. The authors would also like to express their gratitude to Drs. Shuichi Ito and Kenji Ishikura for their contributions to our clinical practice.
Author information
Authors and Affiliations
Contributions
All authors are physicians who treated the patients in this study. Yuta Inoki conducted the study, collected the clinical and laboratory data, and wrote the manuscript; Kentaro Nishi, Mai Sato, and Masao Ogura reviewed and edited the manuscript; Koichi Kamei, the corresponding author, supervised the work and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Ethics Committee of the National Center for Child Health and Development (approval number: 2021–169).
Consent to participate
Informed consent regarding participation was exempted in accordance with the principles of the Declaration of Helsinki and the ethical guidelines issued by the Ministry of Health, Labor, and Welfare, Japan.
Consent for publication
Informed consent for publication was exempted in accordance with the guidelines.
Conflict of interest
Koichi Kamei has obtained research funding from Public Foundation of Vaccination Research Center, the Terumo Foundation for Life Sciences and Arts, and Taiju Life Social Welfare Foundation; donations from Chugai Pharmaceutical Co. Ltd., Astellas Pharma Inc., Ono Pharmaceutical Co., Teijin Pharma Ltd., Shionogi Co. Ltd., and Otsuka Pharmaceutical Co. Ltd.; and lecture fees from Tanabe Mitsubishi Pharma, Baxter Ltd., and Zenyaku Kogyo Co. Ltd. All other authors have no potential conflicts of interests to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Inoki, Y., Nishi, K., Sato, M. et al. The association between hypogammaglobulinemia severity and infection risk in rituximab-treated patients with childhood-onset idiopathic nephrotic syndrome. Pediatr Nephrol 38, 451–460 (2023). https://doi.org/10.1007/s00467-022-05652-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05652-9