Abstract
Background
This cross-sectional study aimed to determine the influence of genetic polymorphism in two renin-angiotensin system (RAS)-candidate genes on urinary trefoil family factor 3 (TFF3) levels in children with congenital anomalies of kidney and urinary tract (CAKUT).
Methods
The study included fifty children with CAKUT (PUV, VUR, and PUJO) and twenty age-matched controls. Urinary TFF3 levels were measured by enzyme-linked immunosorbent assay. Detection of genetic polymorphisms in two genes, i.e., I/D polymorphism (SNP at rs4340) in angiotensin-converting enzyme (ACE) and A/T polymorphism in the angiotensin II receptor type-2 (AT2R) due to point mutation at rs3736556 was performed by polymerase chain reaction. Progressive deterioration in kidney function was defined as fall in GFR to < 60 ml/min/1.73 m2 and/or progressive scarring.
Results
In our cohort, the genotypic distribution of patients and controls showed no difference. Progressive functional deterioration was significantly associated with the presence of D allele (p = 0.0004), A allele (p = 0.005), and both (p < 0.0001) in patients. Significantly raised TFF3 levels were detected in the urine of children having D allele (D/D > I/D > I/I; p < 0.0001) and A allele (A/A > A/T > TT; p < 0.0001). Also, children with both D/D and A/A allelic genotypes had significantly elevated urinary TFF3 compared to those having either of them.
Conclusions
The presence of D allele and/or A allele is significantly associated with progressive functional deterioration and elevated urinary TFF3 levels. These findings support the role of angiotensin II-AT2R-NF-κB interaction in progressive deterioration of kidney function and subsequent TFF3 expression in CAKUT.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary trefoil family factors (TFF) have shown great potential as biomarkers predicting the progressive deterioration in kidney function in children with congenital anomalies of the kidney and urinary tract (CAKUT) [1]. Of all trefoil peptides, TFF3 is considered to be the best predictor of functional damage to the kidney. It is hypothesized that raised levels of urinary TFF3 actually exhibit the pronounced activity of the renin-angiotensin (RAS) pathway in these children [1, 2]. However, the exact mechanism is still unknown.
On the other hand, there is strong evidence in the literature highlighting the association of genetic polymorphisms in RAS-candidate genes with congenital uropathies [3]. Of these, the stance of the angiotensin-converting enzyme (ACE) gene has been extensively studied. The presence of D allele in I/D polymorphism of the angiotensin-converting enzyme (ACE) gene has shown a significant association with progressive kidney injury in these children [4]. However, no significant difference in the ACE I/D genotype distribution among the patients and controls indicates a lack of association of this gene in the occurrence of CAKUT [3, 4]. Similarly, polymorphism in intron 1 of the angiotensin II receptor type-2 (AT2R) gene has shown a significant association with CAKUT in Italian children [3]. A significant association of the AT2R gene at rs3736556 and rs5194 was also noticed in Brazilian children with pelvi-ureteric junction obstruction (PUJO) [5]. The present study was designed to investigate the genotype distribution in two RAS-candidate genes, i.e., ACE and AT2R in fifty Indian children with CAKUT and twenty controls. We aim to determine the influence of these polymorphisms on the urinary TFF3 levels to confirm the possible role of the RAS pathway in regulating the TFF3 expression in these children.
Patients and methods
A cross-sectional study was conducted in the Department of Pediatric Surgery at our center. Prior to the start of the study, approval was obtained from the Institutional Ethics Committee. Parental consent and assent were also taken at the time of recruitment of the participants.
Patient population
Fifty children with common congenital uropathies (posterior urethral valves (PUV), vesicoureteral reflux (VUR), and PUJO) were included in this study. All were aged < 14 years at the time of diagnosis and had received treatment in accordance with departmental protocols. Twenty age-matched children with non-genitourinary diseases were also recruited within the control group. All participants (patients and controls) underwent blood sampling as a part of the study protocol. The same cohort had undergone urine sampling and biomarker (TFF3) measurement as a part of the previous study [1]. The archives of all the patients were screened for serial technetium-99m diethylenetriaminepentaacetic acid (DTPA) and technetium-99m dimercaptosuccinic acid (DMSA) scans. Progressive deterioration in kidney function was defined as a fall in GFR to < 60 ml/min/1.73 m2 on serial DTPA scans and/or new-onset cortical scar/scars or increase in the size of previous scar/scars on serial DMSA scans [1].
Blood sampling and genetic polymorphism
All children were subjected to a peripheral intravenous puncture and 5 ml of blood was collected in an ethylenediaminetetraacetic acid (EDTA) vial. DNA isolation was done using QIAGEN® isolation kit (QIAGEN Sciences Inc., Germantown, MD, USA). For AT2R gene polymorphism, the amplification-refractory mutation system (ARMS) PCR primers were used to detect point mutation (A to T transition) at rs3736556 site of the AT2R gene [5]. Normal (5′-TATGTTAATTTGTTAGGTCA-3′) and mutant (5′-TATGTTAATTTGTTAGGTCT-3′) ARMS reaction premixes were prepared according to previously published ARMS PCR guidelines and 40 μl aliquots of the premix were dispensed into reaction tubes suitable for use in a thermal cycler. Taq DNA polymerase was added and a conventional PCR device (Bio-Rad T100™ thermal cycler, Bio-Rad Laboratories, USA) was used. Thermocycling protocol consisted of pre-incubation (94 °C) for 2 min, then 35 cycles of denaturation (94 °C) for 15 s, annealing (59 °C) for 10 s, and extension (72 °C) for 30 s. For detecting ACE I/D polymorphism, previously published primer sequences, i.e., 5′-CTGAGA CCACTCCCATC-3′ and 5′-GATGTGGCCATCACATTCGTCAGAT-3′ were used to detect insertion/deletion of the Alu element in intron 16 (SNP at rs4340 site) of the ACE gene [4]. Amplification with these primers yields D and I alleles of 490 and 190 base pairs, respectively.
Case and control samples were randomly arranged in well plates with at least 20% of genotypes re-typed as quality control. The PCR products were subjected to gel electrophoresis using 2% agarose gel with ethidium bromide. Subsequently, visualization was performed under ultraviolet illumination.
Urine collection and biomarker measurement
Urinary sampling, sample storage, and biomarker measurement were performed as a part of the previous study [1]. The enzyme-linked immune absorbent assay kit (ImmunoTag™, Geno Technology Inc., USA) was used for TFF3 measurement in the supernatant. The ratio of urinary biomarker concentration to urinary creatinine was calculated to eliminate the variations due to urinary flow rate. Urinary creatinine was measured using Jaffe’s method.
Statistical analysis
Data extraction and analysis were performed using Microsoft Excel (Version 15.24) and Stata/SE 12.0, respectively. Data were expressed as numbers and proportion. Median and interquartile range (IQR) were used when the distribution was non-normal. Categorical variables were assessed using the chi-square test. Comparison of the median concentration of urinary TFF3 between two groups was performed using the Wilcoxon rank sum test. When the groups were more than two, Kruskal-Wallis test was used. A p value of < 0.05 was considered to be statistically significant.
Results
Baseline characteristics
The study included fifty patients and twenty controls (Table 1) with a median (IQR) age of 3 (1.5–5) and 2.3 (1.2–3.6) years, respectively. No significant difference (p = 0.29) was observed when comparing the age of patients and controls. The male:female distribution of the patients and controls were 42:8 and 16:4, respectively. The distribution of PUV, VUR, and PUJO in the cohort was 44% (22/50), 36% (18/50), and 20% (10/50), respectively. As per the archives, the median (range) GFR (in ml/min/1.73 m2) of the cohort decreased from 68.5 (17–120) to 55 (15–115). Overall, twenty-one (53%) children had progressive deterioration in kidney function. Seventeen of these showed a decline in GFR to < 60. However, four showed progressive scarring on serial DMSA scans.
The median (IQR) urinary concentrations of TFF3 in children with CAKUT and controls were 176.5 (116.2–230.7) mcg/gCr and 74.7 (31.6–103.6) mcg/gCr, respectively. The difference in the concentrations of TFF3 in cases versus controls was statistically significant (p < 0.001).
Polymorphisms in ACE and AT2R in cases and controls
The frequency of different genotypes in the study cohort is shown in Table 1. The I/I and A/T were the most common ACE and AT2R allelic genotypes, seen in 46% and 50% of the patients, respectively. None of the genotypes showed a significant association with CAKUT (Table 1) as compared to controls. The distribution of different genotypes in children with different uropathies is illustrated in Table 2. On a 3 × 2 table, no significant association of a specific allelic genotype was observed among children with different uropathies.
The presence of D allele (either D/D or I/D genotype) of ACE or A allele (either A/A or A/T genotype) of AT2R showed a significant association with progressive deterioration in kidney function (p = 0.0004 and 0.005, respectively). Similarly, a significant association (p < 0.0001) with progressive functional deterioration was seen when both the D and A alleles were present in patients as compared to when either of them was present. Supplementary Table 1 shows the distribution of different allelic genotypes according to progressive deterioration in kidney function.
Relationship of urinary TFF3 levels with polymorphisms in ACE and AT2R genes
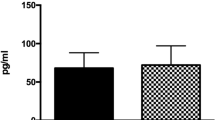
The median (IQR) concentrations of urinary TFF3 (Supplementary Table 2) in patients with D/D, I/D, and I/I allelic genotypes of the ACE gene were 364.3 (273.7–409.1), 203.7 (179.2–216.7), and 105.2 (82.8–154.7) mcg/gCr. This comparison showed a statistically significant difference (p < 0.0001). Figure 1 depicts the distribution of urinary TFF3 in different allelic genotypes. On the other hand, the comparison of urinary TFF3 levels in controls with D/D, I/D, and I/I allelic genotypes (Fig. 1) of the ACE gene showed no significant difference (p = 0.67).
Relationship of urinary TFF3 with ACE I/D gene polymorphism in children with congenital uropathies and controls. Upon comparing the TFF3 levels in different allelic genotypes among the patients, significantly elevated (p < 0.0001) levels of urinary TFF3 (Kruskal-Wallis test) were observed in the children with D/D genotype. Abbreviations ACE, angiotensin-converting enzyme; TFF3, trefoil family factor 3; mcg, microgram; mg, milligram; g, gram; Cr, creatinine
A similar trend was observed when the urinary TFF3 levels were compared (Fig. 2) among children with different allelic genotypes of the AT2R gene. The median (IQR) concentrations of urinary TFF3 (Supplementary Table 2) in patients with A/A, A/T, and T/T genotypes were 275.3 (261.2–398.3), 175.7 (137.9–191.0), and 86.8 (79.7–109.6) mcg/gCr. This comparison showed a statistically significant difference (p < 0.0001). In contrast, urinary TFF3 levels in controls with A/A, A/T, and T/T allelic genotypes showed no significant difference (p = 0.78).
Relationship of urinary TFF3 with AT2R gene polymorphism in children with congenital uropathies and controls. Upon comparing the TFF3 levels in different allelic genotypes among the patients, significantly elevated (p < 0.0001) levels of urinary TFF3 (Kruskal-Wallis test) were observed in children with the D/D genotype. Abbreviations AT2R, angiotensin II receptor type-2; TFF3, trefoil family factor 3; mcg, microgram; mg, milligram; g, gram; Cr, creatinine
Of the 50 children with CAKUT, nine had both D/D allelic genotype of ACE and A/A allelic genotype of AT2R. When the median urinary TFF3 concentration of these children was compared with five children, who had either D/D genotype of ACE or A/A genotype of AT2R, a statistically significant difference (p = 0.028) was observed. The distribution of urinary TFF3 in these children is illustrated in Fig. 3.
Comparison of urinary TFF3 levels among different allelic genotype combinations in the patient population. Children with both D/D allelic genotype of ACE and A/A allelic genotype of AT2R had significantly elevated urinary TFF3 as compared to those with only one of these polymorphisms (Wilcoxon rank sum test). Abbreviations ACE, angiotensin-converting enzyme; AT2R, angiotensin II receptor type-2; TFF3, trefoil family factor 3; mcg, microgram; mg, milligram; g, gram; Cr, creatinine
Discussion
The renin-angiotensin system (RAS) is one of the key regulators of kidney injury in congenital anomalies of the kidney and urinary tract [6, 7]. Apart from its potent effects on kidney hemodynamics, angiotensin II plays a major role in the transcription of various pro-inflammatory and pro-fibrogenic cytokines like transforming growth factor-β1 (TGF-β1), tumor necrosis factor-α (TNF-α), and others [7, 8]. Recently, it was hypothesized that the angiotensin II-NF-κB interaction might also be responsible for the pronounced expression of various emerging prognostic biomarkers like urinary trefoil family factor 3 [1]. However, concrete evidence was lacking.
The mechanisms of occurrence and progression of kidney damage in CAKUT are diverse and incompletely understood. Genetic polymorphisms in specific RAS-candidate genes are considered to be important factors responsible for this progression. The insertion/deletion (I/D) polymorphisms in the ACE gene are extensively studied in various animal and human studies. The presence of the D allele, noticed in more than half of the population, is associated with increased activity of the angiotensin-converting enzyme [4, 9]. Hohenfellner et al. had demonstrated the D/D allelic genotype of the ACE gene to be significantly associated with kidney failure in children with kidney malformations. This effect was shown to independently predict the adverse outcomes in these cases [10]. In another study including eighty-four Indian children with congenital uropathies, the presence of the D allele was depicted in more than 90% of the children with progressive scarring. It was also highlighted that the presence of the D allele is the only factor independently associated with scar progression and functional deterioration in these children [4]. Rigoli et al. have also demonstrated a striking association between the D/D genotype in children with CAKUT and parenchymal damage. On further sub-analysis, all children with newly developing parenchymal lesions had either the I/D or D/D allelic genotype [3]. In the present cohort, the presence of the D allele was significantly associated with progressive deterioration in kidney function. Moreover, raised levels of urinary TFF3 were found to be significantly associated with the D/D and I/D genotypes. The concentration of TFF3 was > 3.5 times in children with D/D genotype as compared to those with I/I genotype. Therefore, this significant association of the D allele with raised urinary TFF3 depicts a substantial role of angiotensin II in the expression of TFF3. It suggests that TFF3 expression is pronounced when the circulating serum levels of ACE and angiotensin II are greatly increased.
Similar to ACE I/D polymorphism, single-nucleotide polymorphisms (SNPs) in the AT2R gene have been thoroughly investigated. Miranda et al. have highlighted a significant association between the occurrence of PUJO with the AT2R gene at rs3736556 and rs5194 [5]. Apart from these sites, a SNP at the intron 1 region of this gene has also been studied by various authors, but the results are conflicting [3, 11]. The presence of the A allele (rs3736556) of AT2R, like the D allele of ACE, showed a significant association with progressive deterioration in kidney function in our cohort. Similarly, elevated levels of urinary TFF3 were found to be significantly associated with the presence of the A allele of AT2R (decreasing order of TFF3 as per genotype distribution: AA > AT > TT). In addition, the urinary TFF3 concentrations were significantly elevated in children having both the D/D and A/A allelic genotypes as compared to those having only one of them. These findings clearly demonstrate the role of another RAS product (AT2R) behind TFF3 expression and take us one step closer to confirm the possibility of angiotensin II-AT2R-NF-κB interaction behind the progressive deterioration of kidney function in CAKUT. While no studies in humans have shown similar findings, Esteban et al. have demonstrated NF-κB activation by angiotensin II via AT2R receptors to be responsible for disease progression in a ureteral obstruction mice model [12].
In corroboration with the findings of previous studies [3, 4, 10, 11], no significant differences in the ACE or AT2R genotype distribution were observed among the patients and controls. The reason for phenotypic differences and different TFF3 concentrations among the patients and controls (despite similar genotypic distribution) is because these genes are mainly responsible for disease progression rather than having a putative role in the genesis of CAKUT [4]. Therefore, as seen in the controls, it is possible that some children do not manifest the CAKUT phenotype (and have normal TFF3 levels) despite having the D allele and/or the A allele. This is due to the absence of disease-causing mutations in the specific nephrogenic genes, e.g., PAX2, BMP4, WT1, AT2R (for PUJO only), among others. [13]. In our study, the finding of no significant association of the presence of the D allele or A allele with elevated urinary TFF3 concentration in controls supports the above explanation.
Also, no significant association of a particular genotype of ACE or AT2R with a specific CAKUT phenotype was observed in the present cohort. This was contrary to the findings depicted by Miranda et al. [5], where a significant association of SNP in the AT2R gene was observed with the occurrence of PUJO. This variation could be because of limited sample size in the present cohort or a result of racial or ethnic differences.
To our knowledge, ours is the first study demonstrating the influence of genetic polymorphisms in the RAS-candidate genes on urinary TFF3 levels. These results substantiate the findings of the previous study [1]. It is believed that the measurement of urinary TFF3 levels and identification of the allelic genotypes associated with progressive functional deterioration (e.g., D/D and A/A allelic genotypes of ACE and AT2R) will help us to recognize at-risk children early in the course of the disease. Thus, reno-protective strategies can be implemented in a selective subset of children who are prone to kidney failure.
There are some limitations of this study. First, the present cohort was not representative of a typical CAKUT population due to limited sample size. PUV, the most severe CAKUT phenotype, was found to be most prevalent in our study. Although similar observations have been reported by Soliman et al. [14], the majority of studies demonstrate VUR to be most prevalent [1]. Therefore, a larger cohort including a more representative CAKUT population is needed before any definite conclusions can be drawn. In addition, the findings of no significant association between the occurrence of PUJO and SNP in the AT2R gene might be due to limited sample size. Further, children with relatively less prevalent CAKUT might not be included in our study due to small sample size. Second, the issues of incomplete (or variable) penetrance and pleiotropy need to be sorted in subsequent studies. Third, the present study illustrates the effect of genetic polymorphism in two genes only. The influence of other RAS-candidate genes (e.g., REN, ACE2, and AT1R) and more than one SNP per gene also need to be studied. Fourth, TFF3 is an emerging biomarker for predicting prognosis in children with CAKUT. Although previous studies have demonstrated TFF3 overexpression in certain ocular diseases and malignancies (gastric, colon, pancreatic, breast, etc.) in adults, very limited information is available on co-existent diseases of childhood that can act as potential confounders by exhibiting raised TFF3 levels. Thus, this factor needs to be studied further. Finally, the preliminary results of the influence of polymorphisms in RAS-candidate genes on urinary TFF3 are promising and highlight the possible roles of angiotensin II, NF-κB, and AT2R behind TFF3 expression. Further studies measuring the levels of RAS-products (angiotensin II, renin, etc.) and NF-κB in blood and urine need to be conducted to fill the final gap in the current knowledge.
Conclusion
In children with CAKUT, genetic polymorphisms in ACE and AT2R are associated with variable extents of kidney injury and variations in urinary TFF3 levels. The presence of the D allele of ACE and/or the A allele of AT2R is significantly associated with progressive deterioration in kidney function and elevated urinary TFF3 levels. However, despite no significant differences in genotype distribution among the patients and controls, normal urinary TFF3 levels are observed in the latter. The present study supports the role of angiotensin II-AT2R-NF-κB interaction in progressive functional deterioration and subsequent TFF3 expression in children with CAKUT. Further studies with a greater sample size exploring other RAS-candidate genes and more than one SNP per gene need to be conducted before any definite conclusions are drawn.
Code availability
Not applicable.
References
Anand S, Bajpai M, Khanna T, Kumar A (2021) Urinary biomarkers as point-of-care tests for predicting progressive deterioration of kidney function in congenital anomalies of kidney and urinary tract: trefoil family factors (TFFs) as the emerging biomarkers. Pediatr Nephrol 36:1465–1472
Baus-Loncar M, Al-azzeh ED, Romanska H, Lalani el N, Stamp GW, Blin N et al (2004) Transcriptional control of TFF3 (intestinal trefoil factor) via promoter binding sites for the nuclear factor kappaB and C/EBPbeta. Peptides 25:849-854
Rigoli L, Chimenz R, di Bella C, Cavallaro E, Caruso R, Briuglia S et al (2004) Angiotensin-converting enzyme and angiotensin type 2 receptor gene genotype distributions in Italian children with congenital uropathies. Pediatr Res 56:988–993
Bajpai M, Pratap A, Somitesh C, Tyagi J (2004) Angiotensin converting enzyme gene polymorphism in Asian Indian children with congenital uropathies. J Urol 171:838–840
Miranda DM, Dos Santos AC Jr, Sarubi HC, Bastos-Rodrigues L, Rosa DV, Freitas IS et al (2014) Association of angiotensin type 2 receptor gene polymorphisms with ureteropelvic junction obstruction in Brazilian patients. Nephrology 19:714–720
Bajpai M, Singh A (2013) Plasma renin activity: an early marker of progressive renal disease in posterior urethral valves. J Indian Assoc Pediatr Surg 18:143–146
Mandelia A, Bajpai M, Agarwala S, Gupta AK, Kumar R, Ali A (2013) The role of urinary TGF-β1, TNF-α, IL-6 and microalbuminuria for monitoring therapy in posterior urethral valves. Pediatr Nephrol 28:1991–2001
Toke A, Meyer TW (2001) Hemodynamic effects of angiotensin II in the kidney. Contrib Nephrol 135:34–46
Gard PR (2010) Implications of the angiotensin converting enzyme gene insertion/deletion polymorphism in health and disease: a snapshot review. Int J Mol Epidemiol Genet 1:145–147
Hohenfellner K, Wingen AM, Nauroth O, Wühl E, Mehls O, Schaefer F (2001) Impact of ACE I/D gene polymorphism on congenital renal malformations. Pediatr Nephrol 16:356–361
Hiraoka M, Taniguchi T, Nakai H, Kino M, Okada Y, Tanizawa A et al (2001) No evidence for AT2R gene derangement in human urinary tract anomalies. Kidney Int 59:1244–1249
Esteban V, Lorenzo O, Rupérez M, Suzuki Y, Mezzano S, Blanco J et al (2004) Angiotensin II, via AT1 and AT2 receptors and NF-kappaB pathway, regulates the inflammatory response in unilateral ureteral obstruction. J Am Soc Nephrol 15:1514–1529
Woolf AS (2000) A molecular and genetic view of human renal and urinary tract malformations. Kidney Int 58:500–512
Soliman NA, Ali RI, Ghobrial EE, Habib EI, Ziada AM (2015) Pattern of clinical presentation of congenital anomalies of the kidney and urinary tract among infants and children. Nephrology (Carlton) 20:413–418
Acknowledgements
The authors are grateful to Professor Balram Bhargava, Director General, Indian Council of Medical Research for providing support for this project.
Funding
The Indian Council for Medical Research (ICMR) provided funding for this study.
Author information
Authors and Affiliations
Contributions
Study design: Minu Bajpai. Data collection and analysis: Sachit Anand and Alok Kumar. Drafting of manuscript: Sachit Anand. Interpretation of results: Sachit Anand, Minu Bajpai, and Tripti Khanna. Revision of manuscript: Minu Bajpai and Tripti Khanna. All authors approve the final manuscript and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval
Prior to the start of the study, approval was provided by the Institutional Ethics Committee (Ref. No. IECPG-524/29.08.2019, RT-10/26.09.2019).
Consent to participate
Written informed consent obtained from parents for participation.
Consent for publication
Written informed consent obtained from parents for publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Anand, S., Bajpai, M., Khanna, T. et al. Influence of genetic polymorphism in renin-angiotensin system-candidate genes on urinary trefoil family factor 3 levels in children with congenital anomalies of kidney and urinary tract. Pediatr Nephrol 37, 139–145 (2022). https://doi.org/10.1007/s00467-021-05160-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-021-05160-2