Abstract
Background
The prognosis of Henoch-Schönlein purpura (HSP), IgA vasculitis, depends on kidney involvement. There is no consensus on the initiation of treatment for HSP nephritis (HSPN). Some centres start treatment before performing a kidney biopsy (KB) while in others, treatment is dictated by the importance of the clinical, biological and histological signs. The aim of this study was to evaluate which of these two approaches is associated with a better kidney outcome at 5-year follow-up.
Methods
This multicentre, retrospective, nonrandomised study included children treated for HSPN between 2006 and 2010 in a French paediatric nephrology unit. One group had an early KB at diagnosis (before starting treatment or in the 15 following days). In the second group, initial treatment was decided without performing a KB.
Results
Among the 107 children included, 63.5% had an early KB at diagnosis. Follow-up at 5 years was completed in 44 children (28 KB at diagnosis, 16 no KB at diagnosis). Median urine protein/creatinine at 5 years was 2.5 mg/mmol in the early biopsy diagnosis group and 12.5 mg/mmol in the non-biopsy group. An antiproteinuric treatment was given, at 5 years, to 35.7% of the early biopsy at diagnosis children and in 62.5% of the non-biopsied children.
Conclusions
Children with early KB at diagnosis seem to have a better renal outcome at 5 years compared to those without an early biopsy at diagnosis or biopsied later. However, this is a small patient cohort and data are missing. Further work is needed to build consensual guidelines on the management of HSPN in children.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
IgA vasculitis, formerly called Henoch-Schönlein purpura (HSP), is the most common vasculitis in children. Its long-term prognosis depends on the severity of the kidney involvement [1]. Henoch-Schönlein purpura nephropathy (HSPN) affects approximately one-third of patients and its initial manifestations range from benign transient haematuria and proteinuria to severe nephrotic-nephritic syndrome [2, 3]. Around 2% of patients referred to specialised centres progress to stage 5 chronic kidney disease (CKD 5) [1]. Patients can progress to CKD irrespective of their initial presentation, and even patients with minor initial clinical manifestations can evolve to CKD 5 [4,5,6,7]. Research shows that proteinuria during follow-up is the primary predictor of long-term kidney survival [2].
There is currently no consensus on the criteria for initiating treatment for HSPN. In France, certain centres carry out a kidney biopsy almost systematically before starting treatment, whereas in other centres, it is the importance of the biological signs of glomerular damage that dictates the therapeutic approach. We therefore included institutions using different approaches in a multicentre retrospective study and sought to evaluate which of these two strategies is associated with a better kidney outcome.
Methods
This was a multicentre, nonrandomised, retrospective cohort study. The target population comprised all children between 0 and 18 years of age diagnosed with HSPN between January 2007 and December 2011 in one of the 8 French participating paediatric nephrology units from tertiary care hospitals. The clinical spectrum of HSPN ranged from persistent non-nephrotic proteinuria with or without haematuria (defined as urine protein to creatinine ratio > 20 mg/mmol and < 200 mg/mmol associated with plasma albumin > 30 g/l; haematuria was defined as the presence of > 10,000 red blood cells/ml of urine) to nephrotic syndrome (urine protein to creatinine ratio > 200 mg/mmol with plasma albumin < 30 g/l), nephritic syndrome (haematuria, variable amount of proteinuria: urine protein to creatinine ratio > 20 mg/mmol and < 200 mg/mmol; nephrotic range proteinuria was not included), hypertension (using the 95th percentile for systolic and diastolic blood pressure as defined in 2004 by the Forth Report on the diagnosis, evaluation and treatment of high blood pressure in children), impaired kidney function (GFR < 90 ml/min/1.73 m2 using the Schwartz 2009 formula) and a mixed nephrotic-nephritic syndrome (patients who had nephritic syndrome and nephrotic range proteinuria). Patients who presented with isolated haematuria or transient proteinuria did not require treatment and were not included. Patients who received medications commonly used in the treatment of HSPN (corticosteroids for more than 7 days, ARBs, ACE inhibitors, immunosuppressants) for some other indication were not included. Some of the patients had an early kidney biopsy prior to the start of treatment or within 15 days of the start of treatment (group one: biopsy at diagnosis). The International Study of Kidney Disease in Children (ISKDC) classification was used to grade the histological lesions. The remaining patients had a later biopsy or no biopsy, depending on their response to the initial treatment (group two: no biopsy at diagnosis).
The main aim of this study was to evaluate the kidney outcome at 5-year follow-up of children who underwent early kidney biopsy at diagnosis and to compare it to their peers who did not have an early biopsy at diagnosis.
Data collection was based on patients’ medical records. The data were described using means and standard deviations for quantitative variables and headcount and percentage for qualitative variables. The impact of performing an early kidney biopsy at diagnosis on the evolution of patients at 5 years was studied by univariate analysis using Wilcoxon and Chi2 tests. The significance level used for all analyses was 0.05. All analyses were performed using SAS version 9.4 software.
Research ethics board approval was granted at each participating institution. Only anonymous retrospective data were gathered for this study. Patient consent was obtained from all the subjects included in the study.
Results
A total of 107 patients were included, 58 girls and 49 boys. Their median age at the time of HSP diagnosis was 8 years. The initial characteristics of the study population are presented in Table 1. Of the 107 children included in the study, 68 had an early kidney biopsy (group one: biopsy at diagnosis). Thirty-nine patients did not have an early biopsy (group two: no biopsy at diagnosis). Of these, 17 were later biopsied either because of a lack of response to initial treatment or secondary to deterioration of kidney function during follow-up. Twenty-two patients were never biopsied.
Median initial proteinuria was 3000 mg/l (350–17000) in group one: biopsy at diagnosis and 1825 mg/l (80–9300) in group two: no biopsy at diagnosis. Median initial albumin was 30 g/l (12–43) in group one: biopsy at diagnosis and 37 g/l (23–46) in group two: no biopsy at diagnosis. Median initial GFR was 102 ml/min/1.73 m2 (28–180) in group one: biopsy at diagnosis and 119 ml/min/1.73 m2 (85–215) in group two: no biopsy at diagnosis.
The clinical manifestations of nephropathy in children who underwent kidney biopsy at diagnosis were: non-nephrotic proteinuria with or without haematuria (34/68, 50%), nephrotic syndrome (28/68, 41.2%), nephritic syndrome (2/68, 2.9%) and nephrotic-nephritic syndrome (4/68, 5.9%).
The majority of children who had a biopsy at diagnosis had ISKDC grade III (43/68, 63.2%) and grade II (19/68, 28%) lesions. One patient had grade I lesions, 2 patients had grade IV lesions and 2 patients had grade V lesions. In one child, the biopsy was non-contributory due to technical problems.
Clinical-pathological correlations in group one: biopsy at diagnosis are shown in Table 2.
Of the 34 patients presenting with non-nephrotic proteinuria, 35.3% (12/34) had ISKDC grade II lesions and 61.8% (21/34) had grade III lesions. Of the 28 patients who had nephrotic syndrome, 17.9% (5/28) had ISKDC grade II lesions, 67.9% (19/28) grade III lesions, one patient had grade IV and 2 patients had grade V lesions. The 2 patients presenting with nephritic syndrome had grade III histological lesions. Of the 4 patients with severe initial nephrotic-nephritic syndrome, 2 had grade II, 1 had grade III and 1 had grade IV lesions.
The 39 children in group two: no biopsy at diagnosis presented with either non-nephrotic proteinuria (32/39, 82.1%) or nephrotic syndrome (7/39, 17.9%). No patients in this group had nephritic syndrome or mixed nephrotic-nephritic syndrome.
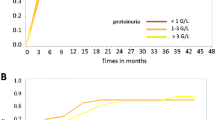
We analysed the median proteinuria of the patients at five time points during follow-up. Throughout follow-up, children who were biopsied at diagnosis had lower proteinuria than those who did not have early biopsies (data not shown).
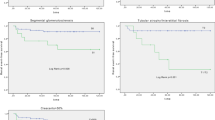
Follow-up at 5 years was completed in 44 children (41.1%), of whom 28 had undergone kidney biopsy at diagnosis and 16 had not been biopsied early (data shown in Table 3). Median proteinuria in group one: biopsy at diagnosis was 80 mg/l (0–500) and 2.5 mg/mmol of creatinine (0–45.5) versus 145 mg/l (0–690) and 12.5 mg/mmol of creatinine (0–57.5) in group two: no biopsy at diagnosis (p > 0.05). There was no systematic GFR data available at 5-year follow-up: patients had a favourable evolution without important proteinuria and therefore blood tests were not routinely performed. At 5-year follow-up, no patient had severe proteinuria (defined as urine protein to creatinine ratio > 200 mg/mmol).
In this cohort, initial treatment modalities included ACEi and ARBs alone; oral corticosteroids alone; oral corticosteroids and ACEi/ARBs; methylprednisolone pulse therapy followed by oral corticosteroids; other immunosuppressive therapies. At 5-year follow-up, 10 of the 16 patients in group two: no biopsy at diagnosis (62.5%) were still receiving antiproteinuric therapy (ACEi or ARBs). Ten of the 28 children who underwent kidney biopsy at diagnosis (35.7%) still needed treatment (ACEi or ARBs) (p > 0.05). No patients in either group were receiving corticosteroids or other immunosuppressants at 5-year follow-up (data shown in Table 3).
We analysed the initial treatment received by the 44 children for whom biological data were available at 5-year follow-up. Children in group two: no biopsy at diagnosis received aggressive treatment for mild manifestations — 8/13 (61.5%) of the patients presenting with non-nephrotic proteinuria received pulse IV methylprednisolone therapy followed by oral corticosteroids, while only 5/12 (41.7%) of the patients in group one: biopsy at diagnosis received this same treatment regimen for the same clinical presentation. Children in group two: no biopsy at diagnosis who presented with nephrotic syndrome did not receive immunosuppressive treatment other than corticosteroids, whereas 4/13 (30.8%) of the patients in group one: biopsy at diagnosis did.
Of the 107 patients included in this study, 44 were still followed at 5-year follow-up. Sixteen patients were lost to follow-up. For the 47 remaining patients, nephrology monitoring was deliberately stopped after recovery of kidney symptoms. Thus, follow-up was stopped after 1 year for 9 children, after 2 years for 18 children and after 3 years for 20 children.
Among the 35 children who presented with nephrotic syndrome, only 17 were still followed after 5 years (4 had been lost to follow-up and the monitoring had been stopped for 14 of them after a rapidly favourable evolution). The 2 children who initially presented with nephritic syndrome were still being followed at 5 years. Only one of the 4 patients who initially presented with mixed nephrotic/nephritic syndrome was still being followed at 5 years (1 patient was lost to follow-up and the other 2 stopped after a rapidly favourable evolution).
Discussion
Management of children with HSPN varies from one paediatric nephrology centre to another. Some teams perform a kidney biopsy before starting treatment, while others start treatment without histological diagnosis and perform a biopsy only if patients do not respond favourably to initial treatment. We wanted to assess the impact of these two different strategies on the long-term kidney prognosis of HSPN. To our knowledge, this is the first study attempting to assess this question.
In this retrospective study, we analysed the renal outcome in 107 children with HSPN. Sixty-eight patients had a kidney biopsy upon diagnosis. In general, there was a good correlation between the clinical presentation of patients and their histological lesions — patients with less severe kidney impairment (non-nephrotic proteinuria, with or without haematuria) had grade I to III histological lesions, while patients with more severe impairment (nephrotic syndrome, nephritic syndrome) had grade II to V histological lesions. However, there are patients for whom this correlation is weak; a patient with ISKDC III grade could have all types of clinical presentation and, conversely, a patient with very severe disease could have lesions varying from grade II to grade V. Several studies have found similar results [4, 5, 8, 9].
Previous research has shown that proteinuria during follow-up is the primary predictor of long-term kidney survival in HSPN [2, 10]. In our study, proteinuria (and the urine protein/creatinine ratio) was the main biological parameter of follow-up. This study shows that children who were biopsied at diagnosis had lower proteinuria during follow-up, but this difference is not statistically significant.
Another way of comparing the renal outcome of the two groups was to analyse the need for antiproteinuric therapy; at 5-year follow-up, 10/16 (62.5%) patients who did not have a biopsy at diagnosis required an antiproteinuric treatment, which was more often than their peers (10/28, 35.7%) who were biopsied at diagnosis.
Thus, there is a tendency to a better renal outcome at 5-year follow-up in group one: biopsy at diagnosis (less important proteinuria, fewer patients treated by an antiproteinuric agent) in comparison to group two: no biopsy at diagnosis, in spite of a milder disease at diagnosis in the second group.
The biopsy helps to adapt the treatment depending on the histological severity: 61.5% of the patients in group two: no biopsy at diagnosis received pulse IV methylprednisolone for non-nephrotic proteinuria, while only 41.7% of the patients in group one: biopsy at diagnosis received this therapy for the same biological presentation. Some patients with nephrotic syndrome in group one received immunosuppressant other than steroids while none of the patients in group two received this type of aggressive therapy. These results suggest that, in addition to clinical and biological symptoms, the biopsy at diagnosis is a useful tool to get a better overview of the kidney situation at presentation and to adapt the initial treatment. The biopsy also prevents misdiagnosis. Optimal evaluation of patients seems to be based on a combination of clinical, biological and histological arguments [11].
The total number of patients for whom biological data were available gradually decreased during follow-up (data available for 95 patients at 1 year, data available for only 44 patients at 5 years after initial management). Some children (16/107) were lost to follow-up. For a large number of children, follow-up was discontinued because patients had experienced complete regression of kidney symptoms quite rapidly after initial treatment. Surprisingly, only 20 of the 41 patients with important kidney impairment at the time of initial management (nephrotic proteinuria, nephritic syndrome, nephrotic-nephritic syndrome) were monitored at 5 years.
Data provided in this study were based on patient medical records and were collected from tertiary care hospitals. Patient follow-up was initially organised in the 8 paediatric nephrology centres that participated in the study. Once the patients recovered (completely/partially), some tertiary care hospitals addressed their patients for follow-up with their general paediatricians or their proximity hospitals. We contacted these professionals and we were surprised to find out that nephrologic follow-up was often discontinued because patients were considered ‘completely recovered’. This is a worrisome observation. It suggests that physicians who are not working in tertiary care hospitals are not aware of the importance of the long-term follow-up recommended for this disease. It also suggests that the dissemination of information concerning the duration and modalities of follow-up is not optimal. Currently, there are no guidelines regarding the optimal length of follow-up of children with HSPN, but literature data show that follow-up should be at least 5 years for all patients and even longer for children with severe initial kidney impairment [12]. In addition, even children with mild initial manifestations should benefit from long-term monitoring as it has been shown that deterioration in kidney function can occur even years later in the course of follow-up and even after apparent complete ‘recovery’ [4, 5, 7, 13]. Follow-up is simple to organise and should consist of blood pressure and proteinuria measurement at regular intervals in order to identify patients at risk of progression to CKD [12, 14, 15].
This study has limitations. It is a retrospective study with a risk of recall bias because all the events examined are past events. As with other observational studies, this retrospective cohort only allows the assumption that there is an association between exposure and outcome.
In conclusion, renal outcome seems to be better in children who underwent kidney biopsy at diagnosis, indicating that performing an early kidney biopsy in children with HSPN allows a more holistic assessment of kidney lesions. Treatment can be better adapted compared to a therapeutic decision guided by clinical and biological criteria alone. Further work, of greater power and with better organised patient follow-up, is necessary to build consensual guidelines on the management of Henoch-Schönlein nephritis in children.
References
Davin J-C, Coppo R (2014) Henoch-Schönlein purpura nephritis in children. Nat Rev Nephrol 10:563–573
Coppo R, Andrulli S, Amore A, Gianoglio B, Conti G, Peruzzi L, Locatelli F, Cagnoli L (2006) Predictors of outcome in Henoch-Schonlein nephritis in children and adults. Am J Kidney Dis 47:993–1003
Jauhola O, Ronkainen J, Koskimies O, Ala-Houhala M, Arikoski P, Holtta T, Jahnukainen T, Rajanti J, Ormälä T, Turtinen J, Nuutinen M (2010) Renal manifestations of Henoch-Schonlein purpura in a 6-month prospective study of 223 children. Arch Dis Child 95:877–882
Goldstein AR, White RH, Akuse R, Chantler C (1992) Long-term follow-up of childhood. Henoch-Schonlein nephritis. Lancet 339:280–282
Koskimies O, Mir S, Rapola J, Vilska J (1981) Henoch-Schonlein nephritis: long-term prognosis of unselected patients. Arch Dis Child 56:482–484
Ronkainen J, Nuutinen M, Koskimies O (2002) The adult kidney 24 years after childhood Henoch-Schonlein purpura: a retrospective cohort study. Lancet 360:666–670
Tudorache E, Azema C, Hogan J, Wannous H, Decramer S, Deschenes G, Ulinski T (2015) Even mild cases of paediatric Henoch-Schonlein purpura nephritis show significant long-term proteinuria. Acta Paediatr 10:843–848
Coppo R, Mazzucco G, Cagnoli L, Lupo A, Schena FP (1997) Long-term prognosis of Henoch–Schönlein nephritis in adults and children. Nephrol Dial Transplant 12:2277–2283
Delbet JD, Geslain G, Auger M, Hogan J, Salomon R, Peuchmaur M, Deschênes G, Buob D, Parmentier C, Ulinski T (2020) Histological prognostic factors in children with Henoch-Schönlein purpura nephritis. Pediatr Nephrol 35:313–320
Edström Halling S, Söderberg MP, Berg UB (2010) Predictors of outcome in Henoch-Schönlein nephritis. Pediatr Nephrol 25:1101–1108
Ninchoji T, Kaito H, Nozu K, Hashimura Y, Kanda K, Kamioka I, Shima Y, Hamahira K, Nakanishi K, Tanaka R, Yoshikawa N, Iijima K, Matsuo M (2011) Treatment strategies for Henoch-Schonlein purpura nephritis by histological and clinical severity. Pediatr Nephrol 26:563–569
Narchi H (2005) Risk of long term renal impairment and duration of follow up recommended for Henoch-Schonlein purpura with normal or minimal urinary findings: a systematic review. Arch Dis Child 90:916–920
Davin JC, Coppo R (2013) Pitfalls in recommending evidence-based guidelines for a protean disease like Henoch-Schonlein purpura nephritis. Pediatr Nephrol 28:1897–1903
Bogdanovic R (2009) Henoch-Schönlein purpura nephritis in children: risk factors, prevention and treatment. Acta Paediatr 98:1882–1889
White RHR, Yoshikawa N, Feehally J (1999) Chapter 41. In: Barratt TM, Avner ED, Harmon WE (eds) Pediatric Nephrology, 4th edn. Williams & Wilkins, Philadelphia, pp 691–706
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Avramescu, M., Lahoche, A., Hogan, J. et al. To biopsy or not to biopsy: Henoch-Schönlein nephritis in children, a 5-year follow-up study. Pediatr Nephrol 37, 147–152 (2022). https://doi.org/10.1007/s00467-021-05086-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-021-05086-9