Abstract
Improving quality of care delivery is an important focus for all practicing physicians. Frontline clinicians are in a great position to identify clinical problems and find innovative solutions. The current review describes the method used for quality improvement based on the Model for Improvement, a structural framework to guide improvement work. At its basis are three fundamental questions: What are we trying to accomplish? How will I know that a change will lead to improvement? And what changes could we make that will result in improvement? This preparation phase aims to identify and understand the problem, choose an intervention, and determine reliable measures to gauge improvement. The intervention is then tested using PLAN-DO-STUDY-ACT (PDSA) cycles, an iterative approach to systematically improve processes and outcomes. PLAN focuses on defining the goal of the cycle and describing in details what will be done. DO concentrates on the concrete application of the plan. STUDY focuses on data analyses as ACT identifies lessons learned from the cycle and orientate the goals of the following PDSA cycle. Learning from each cycle, developing an interdisciplinary team and repeated interventions are core principles involved in implementing a sustainable quality improvement program. The Model for Improvement will be illustrated by a common quality problem in pediatric nephrology.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In 1999, a report from the Institute of Medicine entitled ‘To Err Is Human: Building a Safer Health System’ demonstrated the high incidence of preventable medical errors within the healthcare system [1]. This report was a wake-up call for healthcare leaders but also for the public. Several publications revealed concerns regarding patient safety within the healthcare system [2,3,4,5,6]. National initiatives were undertaken to develop strategies with a focus on improving patient safety and delivering quality care [7,8,9]. Despite this new focus, concrete improvement in the quality of care delivered is smaller than expected [10, 11]. One reason for this lack of improvement is that frontline clinicians are not empowered or trained to address systems-level quality problems in healthcare delivery [11]. A gap therefore persists between what is technically possible in terms of innovations, technologies, and novel therapies, and the actual care delivered to patients. The goal of the quality improvement (QI) approach is to close this gap [12, 13]. The purpose of this educational review is to introduce a structured framework for QI, the Model for Improvement, and illustrate this approach with a pediatric nephrology case. Application of QI methodology in clinical care by frontline clinicians increases the potential of implementing an effective change that will improve clinical outcomes over time [12, 14, 15]. Improving vaccination rate in children with chronic kidney disease (CKD) is used to illustrate the application of QI methodology.
Clinical scenario—vaccination in CKD
A 7-year old girl with end-stage renal disease (ESRD) on dialysis presents to the emergency room with a 48-h history of cough and fever. Her condition quickly deteriorates, and she is transferred to the pediatric intensive care unit (PICU) for mechanical ventilation and management of severe pneumococcal pneumonia. It is brought to your attention that she did not receive the pneumococcal vaccination. You believe that her risk of pneumococcal infection would have been decreased if she had been properly vaccinated. You wonder why she was not immunized, given that children with ESRD are known to have an increased risk of infection [16,17,18,19]. Several questions are raised. Why did she not receive her pneumococcal vaccine as per current evidence-based recommendations [18]? How can you prevent a similar episode from recurring? How could you close the gap and improve the quality of care of children with CKD?
The Center for Disease Control (CDC) Advisory Committee has published specific guidelines regarding immunization for children with CKD and on dialysis [20]. Those guidelines recommend that children with CKD should receive standard childhood immunization and that live vaccines should be avoided by patients taking immunosuppressive therapy [16, 18,19,20]. Despite the available data and guidelines, a suboptimal rate of vaccination for seasonal influenza and Streptococcal pneumoniae has been described in the US pediatric population with ESRD [21]. The non-adherence to prevention recommendations points to both local and systemic hospital barriers. It also highlights the importance and magnitude of the problem to address vaccination in the CKD population.
The Model for Improvement
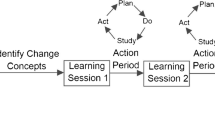
The Model for Improvement is a framework to guide quality improvement work. It was developed in the 1980s by the Associates in Process Improvement [22]. It is based on three fundamental questions: What are we trying to accomplish? How will I know that a change will lead to improvement? And what changes could we make that will result in improvement? (Fig. 1) [14, 15, 23]. By answering those questions, the service quality issue is defined and the improvement idea identified. The intervention is designed and the theory behind it is developed. This is the preparation phase of a QI effort [23, 24]. Then, the intervention is tested using PLAN-DO-STUDY-ACT (PDSA) cycles. Several PDSA cycles are undertaken towards the same goal (Fig. 2) [15]. QI methodology serves to guide an improvement effort towards a desired goal and predefined clinical outcomes.
Other improvement frameworks, born out of manufacturing industries, such as Six Sigma, and Lean methodology [23, 25] have also been adapted to be used in healthcare QI. However, the Model for Improvement has gained the most support and will be the focus of this review.
Selection of an improvement area for a QI project
A QI effort is often triggered by the patient experience such as the current example of severe pneumococcal pneumonia in a non-vaccinated patient. It can also be inspired by data demonstrating variations in patient care delivery or clinical outcomes [15, 23]. However, not all quality issues encountered in clinical practice are fixable. It is important to consider the feasibility of an improvement work. A good improvement work should address a quality issue that occurs frequently, affects regularly clinicians in their practice, and influence the patients’ care. This is a fundamental concept in healthcare QI [14, 15]. Clinicians are more likely to be engaged in a process when they personally face the problem on a regular basis [23]. When the improvement effort aligns with institutional priorities, it is easier to engage institutional leaders in the improvement effort.
What are we trying to accomplish?
Existence of a local problem
Before starting any QI initiative, it is necessary to confirm there is a problem and assess its importance [14, 23]. From the clinical case, it is known that pneumococcal pneumonia in a non-vaccinated patient with CKD can happen. Is this patient with ESRD an isolated case of non-vaccination? It is important to determine if this event is a one-time event or a real significant problem involving more than one patient. Before doing any extended analyses of baseline data and spending time, energy, and resources, an audit of the local problem should be done [14]. It provides data at one point in time. It is not giving any information about trend, variability, and stability of data over time but helps to answer the question of how frequent the problem of non-vaccination is, in the CKD population. You decide to assess the local problem of non-vaccination in your CKD clinic. You choose randomly the next CKD clinic. A total of 10 patients come to clinic and 3 of them are vaccinated (30%). Is this sample size enough? Many people, especially those attuned to power calculations to assess a relevant clinical difference, intuitively believe that more data are needed. However, a small and representative sample can be used to assess the scope of the local clinical issue [26, 27]. Furthermore, the goal of this initial step is to determine if there is a problem, which can generally be gleaned from a small sample size. Based on your audit, the rate of vaccination in CKD clinic is 30%. Is this rate of vaccination adequate? It is important to know the parameter of performance early in the process to assess if a local problem exists. This parameter serves to assess the quality gap in the local problem. The parameter of performance can be determined based on regional/national standards or even clinical trials [14]. Sometimes, it can be based on the clinical experience. For the vaccination rate in CKD population, it would be reasonable to have a rate of 80% or more. The parameter of performance is not the official performance target of the whole improvement process but a tool to assess if the problem exists locally. It can be helpful later when the goals of the improvement effort are developed. With your colleagues, you decide that a rate of vaccination of 80% or more is your parameter of performance. Your preliminary audit demonstrated a rate of vaccination of 30%. It is lower than your pre-established parameter of performance. The problem of non-vaccination in CKD population exists.
Narrow the scope of the improvement effort
When the area of improvement and the existence of a local problem are identified, it is important to narrow the scope of the problem. Not appropriately narrowed, the focus of an improvement work may not be effective in bringing a real improvement [14, 15, 22]. It is hard to address different aspects of a problem at the same time, and attempting to do so may result in loss of time, effort, and resources. This step is like developing a research question in the traditional research approach. The Feasible-Interesting-Novel-Ethical-Relevant (FINER) criteria are used to build good research questions, and also used to help narrow the focus of an improvement effort [14]. The goals of an improvement effort should respect those criteria [14]. This step is essential and will help to develop the aim statement of the improvement work.
As described above, vaccination of children with CKD is low in your CKD clinic, and it can be related to serious patient outcomes. Increasing the rate of vaccination of such patients is a goal within the control of the nephrologists involved in CKD clinics. With the low vaccination rate described in American studies on children with CKD [21], an improvement effort focusing on improving vaccination rate is not only interesting and relevant for the local organization but also other institutions. Other pediatricians may also be interested in the change implemented. Working on improving the outpatient vaccination rates provides opportunities to learn about the local outpatient system and how to optimize performance. This new knowledge of system processes is important to improve patient outcomes. Choosing to improve the outpatient vaccination service for CKD patient should never harm or disrespect the privacy of patients [28].
Developing the aim statement
Creating an aim statement is important as it provides the target goal. Thus, it needs to be clear, concise, and result-oriented [14, 15]. An effective aim statement is based on SMART criteria-specific (define clearly the goal and address who, what, when, where and why), measurable (quantify progression over time), attainable (achievable goal), reasonable (realistic and relevant goal with consideration of local resources), and doable within a defined time-frame [14, 23]. An example of an aim statement for the problem of non-vaccination in CKD patients is: ‘Increase the vaccination rate to more than 80% in CKD patients by improving access to outpatient vaccination services over the next 24 months.’
Building the improvement team and stakeholder engagement
Solving a quality care issue in a complex system, such as the healthcare system, is impossible with only one person. An interdisciplinary team is essential as a large spectrum of knowledge and skills is required [14, 23, 29]. Local ownership of a QI effort is a key concept. Stakeholders should be identified and engaged at the beginning of an improvement effort [23, 30]. They should be involved in defining the goals, developing the aim statement, and designing the intervention [23]. Their engagement will also be important in data collection and analyses [29].
It is important to identify the key stakeholders to lead, support, and champion the work [23, 29]. One way of categorizing potential stakeholders is by constructing an influence versus interest grid (Fig. 3) [23]. Stakeholders may vary from champions, helpers, and bystanders to resisters. It is important to bring together the different perspectives, and all types of stakeholders involved [29]. Identification and engagement of additional stakeholders anticipated to be resistant to certain changes is essential. It may facilitate implementation of the improvement intervention in the local organization and help to identify additional barriers [30]. Diversity of opinion also helps in determining how best to engage people and make the problem relevant for all front-line clinicians [23].
The influence versus interest grid to determine and classify stakeholders. Stakeholders can be classified based on two characteristics: interest and influence. Interest refers to the degree of concern a quality problem or/and an improvement change. Influence refers to the power of resisting or stimulating a change. Although the greatest champions of a QI project are those identified as having the most influence and interest, all four groups need to be engaged at some level
For example, to improve vaccination in children with CKD, the team should include nephrologists, pediatricians, and nurses involved in CKD, dialysis, and transplant clinics as they are the main healthcare professionals who meet children with CKD (Fig. 3). An infectious disease consultant needs to be involved as an expert in infectious diseases and vaccination (Fig. 3). The outpatient clinic and dialysis unit managers are also key people to be involved as they know available human and material resources. Additionally, engaging parents and families of children with CKD will also increase awareness and empower families in their clinical care.
Diagnostics of the problem
An improvement effort should be designed with consideration of the actual problem [14]. It is imperative to understand and map out why children with CKD are not vaccinated before planning any intervention. Understanding the problem is an essential step that should not be skipped. This will identify what specific process will be the focus of the improvement effort and also set realistic goals in addressing complex healthcare system issues. Several visual tools exist to help with this step [15].
- 1.
Fishbone diagram (Fig. 4): A useful tool to brainstorm root cause of a specific issue is the Fishbone or Ishikawa diagram [14, 15]. This tool is useful at the beginning of an improvement work. It organizes the causes into categories adapted to the specific quality issue. In this instance, it includes process, people/patient, machine, environment, material, and measurement [14]. For example, factors such as acute illness or immunosuppressive drugs are related to people/patient, whereas having no outpatient setting to provide vaccines or absence of a refrigerator to store vaccines in CKD clinic are related to environment and material respectively.
- 2.
Process mapping (Fig. 5): When a problem occurs as part of a complex system that includes several potential pathways or steps, a visual overview of the entire process is helpful [14, 15]. Process mapping is essentially a workflow diagram that helps to understand and illustrate a process or series of parallel processes. Figure 5 illustrates the process of vaccination in a child with CKD.
- 3.
Pareto chart (Fig. 6): The Pareto chart is a vertical bar graph where the different causes of a problem are plotted in decreasing order of relative frequency [14]. It helps to prioritize causes after a root cause analysis. The improvement effort should focus on causes with the greatest cumulative impact on the targeted problem [15]. A Pareto chart identifies factors that impact the outcomes by frequency of occurrence and can be explained as “80% of the problem is caused by 20% of the causes” [14, 15]. Figure 6 highlights causes of non-vaccination in CKD children and which one impact has the greatest impact. Figure 6 shows that the family physician/pediatrician (FP/P)’s concern about vaccination safety in CKD patient is a major factor contributing to the non-vaccination of children with CKD. Fixing this cause should be one of the first target of the QI effort.
A process map to determine the steps involved in the vaccination process in children with chronic kidney disease. The current process map shows the patient process from the moment that non-vaccination is identified to the moment the patient is vaccinated, or not vaccinated if he does not have any family physician/pediatrician (FP/P)
A Pareto chart helps to identify causes and their relative contribution to non-vaccination of chronic kidney disease children. The current Pareto chart (n = 50) shows that non-vaccination is explained by family physician/pediatrician (FP/P)’s concern regarding vaccination safety in chronic kidney disease (CKD) patient (dark blue bar). It means that this cause contributes to 54% of all causes of non-vaccination. Incapacity to book an appointment with FP/P to receive vaccine is noticed in nine cases, which contributes to an additional 18% (pale blue bar). Contribution of all other causes is smaller. To be efficient, an improvement effort should address first the FP/P’s concerns regarding vaccination safety in CKD children
How will we know that a change is an improvement?
Outcome, process, and balancing measures
Three categories of measures include outcome, process, and balancing measures [14, 15, 23, 31]. A good measure helps to understand a process and assess the impact of an intervention [15, 24]. The outcome measure is related to the final desired clinical outcome and to the performance of the whole improvement effort. It should ideally be related to a patient clinical outcome [15, 23, 31]. An example of outcome measure is the rate of vaccination of patients with CKD. Even with only few cycles, a change may be seen and influences the intervention. It is a proximal outcome, and it is helpful on the short term. Incidence of vaccine-preventable diseases in patients with CKD is also an outcome measure but will take several cycles before a change can be seen. It is a distal outcome that is helpful on the long term. Process measures are typically related to the intervention performance [14, 15, 23, 31]. If the intervention is to improve the vaccination outpatient service, the number of CKD patients referred to FP/P with the vaccination standardized letter and number of CKD patients able to meet their FP/P for vaccination are examples of process measures. Process measures should reflect key steps of intervention and be logically related to the outcome [23, 31]. They are useful short-term performance indicators of the intervention. Process measures should also be easily measurable. The difference between a process measure and an outcome measure can be reflected by the analogy between proteinuria (process measure) and development of chronic kidney disease (outcome measure). Balancing measures are related to the undesired effects of an intervention [31]. The unintended and undesired/negative consequences of a QI effort are often best considered and accounted for up front rather than allowing them to later derail the project. For example, if an improvement initiative will involve an extra visit to the FP/P’s office, it would be critical to take the cost to the parent in having to take more time off work, pay for parking costs, or arrange alternate child care. Outcome, process, and balancing measures are collected on multiple small and rapid PDSA cycles [15]. Data are assessed over time to identify any trends, variability, and stability with time.
What changes could we make that will result in improvement?
The two first questions of the Model for Improvement address understanding and defining the problem as well as choosing appropriate measures to quantify an improvement. The third question focuses on the change that will be implemented and the theory behind choosing a change. The healthcare system is inherently complex, and there are many factors at play that might determine the success or failure of an intervention [32]. Identifying and understanding these factors is important. To improve the vaccination rate of patients with CKD, there are several factors to consider, such as who will vaccinate those patients, what is the availability of vaccines in the CKD outpatient clinic, have patient access to vaccination clinics, will they need extra visits to the hospital, and does the patient’s medical condition contraindicate vaccination? There are theories that can be used to help analyze these factors, and thereby better plan, and subsequently evaluate any proposed intervention [32]. Two examples of such theories are impact and process theories. Impact theories pertain to hypotheses about how the targeted intervention will result (or not) in the desired change, while process theories are assumptions related to implementation activities of the targeted intervention (organizational plan) [32]. Both types of theories are essential when implementing a change in the healthcare system.
Patients with CKD can be vaccinated by their FP/P. If the primary physician has any concern about the vaccine safety for their patient, he will not proceed with vaccination. An intervention that targets this issue will help improve the vaccination rate. A letter from the nephrologist which assures the FP/P of the safety of the vaccination for patients with CKD seems like a good intervention to start with. This is an example of an impact theory. To implement such an intervention, a standardized letter can be written and given to every patient seen in the outpatient CKD clinic. If importance of vaccination is discussed in the first appointment in CKD clinic and the standardized letter is given to the patient/parents, the vaccination process with the primary physician will be facilitated, and this will help mitigate vaccination delay. This is an example of a process theory (see Grol et al., 2007 for a more comprehensive review on this topic).
Plan
Plan is the first stage of a PDSA cycle (Fig. 7). It defines the goal of the cycle and describes in details what will be done [15]. It is also the step where predictions are developed. The improvement team states their expectation about the impacts, the change that will result from the intervention [14]. It can be based on literature review, benchmarking with other organizations, and baseline data. Predictions will be used later in the study step [33].
Improving vaccination rate of chronic kidney disease (CKD) patients. This is an example of a PDSA cycle for the improvement effort targeting vaccination rate of children with CKD. Each step of the cycle is illustrated by a concrete example. FP/P: family physician/pediatrician. Adapted with permission from Provost and Murray, The Health Care Data Guide, 2011
Following an extended analysis to understand why CKD patients are not vaccinated, the FP/P’s concern regarding vaccination safety for this population has been identified as the most important factor. It is logical that this issue needs to be addressed in the first PDSA cycle. You predict that FP/P will be more comfortable to vaccinate CKD patients in their clinic, and vaccination rates will improve if you could allay their concern regarding vaccination safety. The intervention chosen is to refer patients to their FP/P for vaccination with a standardized letter outlining the importance and safety of vaccination in CKD population. The outcome measure chosen is the vaccination rate following the reference to FP/P. The number of CKD patients referred to FP/P with the vaccination standardized letter and number of CKD patients able to meet their FP/P for vaccination are process measures. Extra time and cost for the patient/families to visit the FP/P are balancing measures (Fig. 7).
Do
Do is the second step of the PDSA cycle. It focuses on the concrete application of the intervention planned in the previous step (Fig. 7) [15, 26, 34]. The intervention is implemented and initial predictions are tested. The various predefined measures (outcomes, process, and balancing) are now systematically collected.
In the first PDSA cycle, you addressed the FP/P’s concerns regarding vaccination safety in CKD patients. You execute the plan and begin tracking the number of patients referred to FP/P with the vaccination standardized letter and number of CKD patients able to meet their FP/P for vaccination. You will be monitoring the vaccination rate, the extra time, and cost for patients/families to visit the FP/P. After implementing the standardized referral and collecting data on the relevant measures, the next step is to analyze the results.
Study
The study step of the cycle concentrates on the data analyses. The goal of this step is to compare results from the intervention with initial predictions [14, 15]. Data are assessed over time. Time series data are more useful than one-time data. There is a unique set of tools to analyze quality data [31]. Initial analyses employ visual tools that consider data changes over time, such as the run chart [35].
Given that several short cycles of intervention are done on a small sample, it is important to analyze over time [14, 31]. Run charts graph data plotted over time to identify non-random trends or patterns in the process [35]. Figure 8 illustrates a run chart assessing the percent of vaccinated patients with CKD. Presence of a non-random data distribution implies that the intervention has an effect, which can be either a positive or negative [15]. An intervention with a positive effect should be reproduced as an intervention with a negative effect should be avoided. Sometimes, those non-random data distributions can be seen when an unplanned event happened and impact directly the intervention. An example of that could be arrival of new fellows who are not aware of the project and are not used to refer CKD patients to FP/P for vaccination. This new event may influence directly your measures. There are four specific patterns of non-random data distribution, which can be observed on a run chart: overall variability (too few or too many runs), shift (≥ 8 above or below the median), trend (≥ 7 points trending up or down), and astronomical points (outliers in the graph) [14, 15, 31, 35]. Figure 8 illustrates examples of different non-random data distributions.
Run chart detailing the percentage of vaccinated patients followed monthly in chronic kidney disease clinic. The median percentage of vaccinated patients is 49.3% (orange line). The central line on a run chart may be the median (if data are asymmetric) or the mean (if data are symmetric). The four non-random data distributions are illustrated. The overall variability is not enough in this run chart. A run is when the median line is crossed over (run). With a run chart of 39 data, at least 14 runs should be seen but no more than 26 (30). The current chart has only 13 runs. One shift is observed from March to October 2015 (green). This shift is related to a positive impact. The aim of this improvement initiative is to increase the percent of vaccinated patients. This shift reveals a higher percentage of vaccinated patients. This period should be reassessed to identify what made this event special and ensure it is reproduced. A trend is observed from February to August 2016 (red). This trend shows a negative effect, as the proportion of vaccinated patients is progressive decreasing. This could reflect a failure to sustain the initial positive effects of the change on vaccination rates. One point (orange) is an astronomical point, and it is related to a negative effect in the current example
Data analyses show that 12 patients out of 18 have been referred to a FP/P with the new standardized referral letter. However, no increase of the vaccination rate of CKD patients has been noticed (70 vs 68%) (Fig. 7). It may be that the FP/P never received or read the referral as they get too much mail. Upon further study, you realize that 8 out 12 patients referred to a FP/P were not able to book an appointment. From a subsequent survey of the children’s guardians, it emerges that the principal reason for not visiting the primary care physician was the fact that they visit the hospital so often for dialysis or CKD clinics that families did not want another visit. Furthermore, extra time and money ($10 for parking) were reported by one family who did manage to visit a pediatrician and have their child vaccinated.
Act
Act is the last step of the PDSA cycle where new lessons learned from the previous steps are used to fine tune the next cycle [34]. There are three potential outcomes. Are you stopping the intervention? Are you keeping the same intervention but need to refine it? Are you modifying the intervention to adapt it to the local environment? [15] The answer to these questions will guide the first step of the next PDSA cycle. Every cycle is dependent on the outcomes of the preceding one. A lesson from the first PDSA cycle is that the majority of patients referred to the primary care physicians never actually booked an appointment for vaccination. Referring CKD patients to their primary care physicians for vaccination is not optimal as patients are not able to book an appointment with their FP/P. Consequently, this intervention should be abandoned. Another intervention should be chosen, such as developing a vaccination service within CKD clinic and dialysis unit as patients visit often the hospital for dialysis or CKD clinic appointment. Hence, the next PDSA cycles will focus on the development and implementation of a vaccination service for children in the CKD clinic or on dialysis unit.
Resolution of the clinical scenario
After the completion of the first PDSA cycle, several other cycles are conducted (Fig. 9). A significant improvement of percent of vaccinated CKD patients is observed following the fifth cycle with evidence of an increasing trend starting in June 2017. The aim to increase to 80% (or more) the proportion of vaccinated CKD patients was achieved and surpassed. When a change is successfully implemented, the next step is to ensure that the change will be sustainable over time. In Fig. 9, the percent of vaccinated patients reaches a new plateau around 87% after December 2017. These results are sustainable over the following 12 months. Finally, the success of this improvement effort requires dissemination of the process improvement to the local hospital or clinical practice and also dissemination to the community. It is crucial to share at least locally results from this effort and to celebrate successes as well as learning from failures [14, 36]. It gives the opportunity to share results, engage all stakeholders, and also commend the team for their engagement.
Dissemination of a quality improvement project
Growing interest in quality improvement has contributed to an increasing number of publications over the last decades. Dissemination of a QI effort is an opportunity to share both successes and failures as learning from each step is an important principle [36]. Scholarly reporting of improvement project results also provides more value to this new improvement science. The prior inconsistency in disseminating results of improvement efforts stemmed from the absence of a standardized guidelines for reporting [37]. The Standards for Quality Improvement Reporting Excellence (SQUIRE) have been published and updated in 2015 [38] to decrease variability in reports as well as improve accuracy and comprehensiveness. Report of any QI effort should answer four fundamental questions: (1) Why did you start? (2) What did you do? (3) What did you find? (4) What did it mean? [39].
Conclusion
Pediatric nephrologists, as front-line clinicians, are well placed to identify problems and seek solutions to quality problems. An example is the poor vaccination rate in patients with CKD. In this educational review, we used the Model for Improvement to define the problem of vaccination in CKD children, develop an aim statement to address this issue, choose measures, and plan an intervention. A team including nephrologists, nurses, clinic managers, infectious disease physicians, patients, and families addressed the issue of poor vaccination in CKD patients. Several PDSA cycles were needed before a significant and sustainable improvement of vaccination rate was noticed. This example illustrates how to best use the QI approach. Patient safety and quality are fundamental to any healthcare system. By working as a team, in a stepwise manner, we can change the culture and make the healthcare system safer and better for children.
Key summary points
1. An improvement work should address a quality issue that occurs frequently, affects clinicians in daily practice, and influence the patients’ care. | |
2. The Model for Improvement is based on three questions: (i) What are we trying to accomplish? (ii) How will I know that a change will lead to improvement? (iii) What change could we make that will result in improvement? | |
3. Engagement of stakeholders to help champion the process change is vital to ensure ownership of the change and drive improvement. | |
4. An intervention should follow a Plan-Do-Study-Act cycle, with iterative PDSA cycles needed in quick succession to be refined or adapted. | |
5. Dissemination of the quality improvement effort is an opportunity to share successes and failures, and continuously learn to optimize healthcare delivery |
Multiple-choice questions
Answers are provided following the reference list.
- 1.
Which question is not a fundamental question of the Model of Improvement?
- a)
How will I know that a change will lead to improvement?
- b)
Does a problem exist?
- c)
What are we trying to accomplish?
- d)
What change could we make that will result in improvement?
- e)
None of those answers
- a)
- 2.
What means PDSA cycle?
- a)
Plan-Develop-Study-Act
- b)
Prepare-Do-Study-Analyze
- c)
Prepare-Develop-Study-Act
- d)
Plan-Do-Study-Act
- e)
Plan-Do-Study-Analyze
- a)
- 3.
What is not true about aim statement?
- a)
Should be specific
- b)
Should be measurable
- c)
Should be attainable
- d)
Should be timely
- e)
Should focus on the stakeholders
- a)
- 4.
Which of the following statement is false?
- a)
Engagement of stakeholders to help champion the process change is essential.
- b)
There are two characteristics to consider when trying to build an improvement team to address a specific problem, which are influence and interest.
- c)
Mapping out a quality problem to identify which processes will be the focus of your efforts and setting realistic goals is unimportant.
- d)
There are three family of measures: outcome measure (related to the final desired result and the patient clinical outcome), process measures (related to the intervention performance) and balancing measures (related to the undesired effects of an intervention).
- e)
Each intervention should follow a Plan-Do-Study-Act cycle, with iterative PDSA cycles needed in quick succession to be refined or adapted.
- a)
- 5.
Which of the following statement is true about run chart?
- a)
Run chart is a line graph of data plotted over time, where the x axis is the specific studied measure and y axis the time.
- b)
Presence of a non-random data distribution implies only that the intervention has a positive effect.
- c)
The central line on a run chart is always representative of the mean.
- d)
Four types of non-random data distribution can be seen on a run chart.
- e)
On a run chart, a trend is ≥8 points above or below the mean and a shift is ≥7 points trending up or down.
- a)
References
(2000) In: Kohn LT, Corrigan JM, Donaldson MS (eds) To err is human: building a safer health system, Washington (DC)
Baker GR, Norton PG, Flintoft V, Blais R, Brown A, Cox J, Etchells E, Ghali WA, Hebert P, Majumdar SR, O'Beirne M, Palacios-Derflingher L, Reid RJ, Sheps S, Tamblyn R (2004) The Canadian adverse events study: the incidence of adverse events among hospital patients in Canada. CMAJ 170:1678–1686
Brennan TA, Leape LL, Laird NM, Hebert L, Localio AR, Lawthers AG, Newhouse JP, Weiler PC, Hiatt HH (1991) Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard medical practice study I. N Engl J Med 324:370–376
Wilson RM, Runciman WB, Gibberd RW, Harrison BT, Newby L, Hamilton JD (1995) The quality in Australian health care study. Med J Aust 163:458–471
Vincent C, Neale G, Woloshynowych M (2001) Adverse events in British hospitals: preliminary retrospective record review. BMJ 322:517–519
Thomas EJ, Studdert DM, Burstin HR, Orav EJ, Zeena T, Williams EJ, Howard KM, Weiler PC, Brennan TA (2000) Incidence and types of adverse events and negligent care in Utah and Colorado. Med Care 38:261–271
Spencer E, Walshe K (2009) National quality improvement policies and strategies in European healthcare systems. Qual Saf Health Care 18(Suppl 1):i22–i27
Services USDoHaH (2011) National strategy for quality improvement in health care. In: Services USDoHaH (ed) p 27
Backman C, Vanderloo S, Forster AJ (2016) Measuring and improving quality in university hospitals in Canada: the collaborative for excellence in healthcare quality. Health Policy 120:982–986
Makary MA, Daniel M (2016) Medical error-the third leading cause of death in the US. BMJ 353:i2139
(2001) Crossing the Quality Chasm: A New Health System for the 21st Century, Washington (DC)
Berwick DM (1996) A primer on leading the improvement of systems. BMJ 312:619–622
Batalden PB, Davidoff F (2007) What is “quality improvement” and how can it transform healthcare? Qual Saf Health Care 16:2–3
Ogrinc GSHL, Moore SM, Barton AJ, Dolansky MA, Madigosky WS (2012) In: Improvement IfH (ed) Fundamentals of health care improvement: a guide to improving your patient’s care. Joint Commission, Oak Brook Terrace
Provost LPMS (2011) The health care data guide: learning from data for improvement. Jossey-Bass, San Francisco
Neu AM (2012) Immunizations in children with chronic kidney disease. Pediatr Nephrol 27:1257–1263
Mitsnefes MM, Laskin BL, Dahhou M, Zhang X, Foster BJ (2013) Mortality risk among children initially treated with dialysis for end-stage kidney disease, 1990-2010. JAMA 309:1921–1929
Esposito S, Mastrolia MV, Prada E, Pietrasanta C, Principi N (2014) Vaccine administration in children with chronic kidney disease. Vaccine 32:6601–6606
Miyairi I, Funaki T, Saitoh A (2016) Immunization practices in solid organ transplant recipients. Vaccine 34:1958–1964
Chi C PP, Pilishvili T, Moore M, Murphy T, Strikas R (2012) Guidelines for vaccinating dialysis patients and chronic kidney disease patients—recommendations of the Advisory Committee on Immunization Practices (ACIP) https://www.cdc.gov/vaccines/pubs/downloads/dialysis-guide-2012.pdf. Accessed 26 Oct 2017
Collins AJ, Foley RN, Chavers B, Gilbertson D, Herzog C, Johansen K, Kasiske B, Kutner N, Liu J, St Peter W, Guo H, Gustafson S, Heubner B, Lamb K, Li S, Li S, Peng Y, Qiu Y, Roberts T, Skeans M, Snyder J, Solid C, Thompson B, Wang C, Weinhandl E, Zaun D, Arko C, Chen SC, Daniels F, Ebben J, Frazier E, Hanzlik C, Johnson R, Sheets D, Wang X, Forrest B, Constantini E, Everson S, Eggers P, Agodoa L (2012) United States renal data system 2011 annual data report: atlas of chronic kidney disease & end-stage renal disease in the United States. Am J Kidney Dis 59(A7):e1–420
Langley GJ, Moen RD, Nolan KM, Nolan TW, Norman CL, Provost LP (2009) The improvement guide: a practical approach to enhancing organizational performance. Jossey-Bass Pub, San Francisco
Silver SA, Harel Z, McQuillan R, Weizman AV, Thomas A, Chertow GM, Nesrallah G, Bell CM, Chan CT (2016) How to begin a quality improvement project. Clin J Am Soc Nephrol 11:893–900
Friedman AN, Fadem SZ (2011) Making measures count. Clin J Am Soc Nephrol 6:1507–1511
Moraros J, Lemstra M, Nwankwo C (2016) Lean interventions in healthcare: do they actually work? A systematic literature review. Int J Qual Health Care 28:150–165
Reed JE, Card AJ (2016) The problem with plan-do-study-act cycles. BMJ Qual Saf 25:147–152
Etchells E, Ho M, Shojania KG (2016) Value of small sample sizes in rapid-cycle quality improvement projects. BMJ Qual Saf 25:202–206
Baily MA, Bottrell M, Lynn J, Jennings B, Hastings C (2006) The ethics of using QI methods to improve health care quality and safety. Hast Cent Rep 36:S1–S40
Weller J, Boyd M, Cumin D (2014) Teams, tribes and patient safety: overcoming barriers to effective teamwork in healthcare. Postgrad Med J 90:149–154
Schiller C, Winters M, Hanson HM, Ashe MC (2013) A framework for stakeholder identification in concept mapping and health research: a novel process and its application to older adult mobility and the built environment. BMC Public Health 13:428
McQuillan RF, Silver SA, Harel Z, Weizman A, Thomas A, Bell C, Chertow GM, Chan CT, Nesrallah G (2016) How to measure and interpret quality improvement data. Clin J Am Soc Nephrol 11:908–914
Grol RP, Bosch MC, Hulscher ME, Eccles MP, Wensing M (2007) Planning and studying improvement in patient care: the use of theoretical perspectives. Milbank Q 85:93–138
Varkey P, Reller MK, Resar RK (2007) Basics of quality improvement in health care. Mayo Clin Proc 82:735–739
Taylor MJ, McNicholas C, Nicolay C, Darzi A, Bell D, Reed JE (2014) Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Qual Saf 23:290–298
Perla RJ, Provost LP, Murray SK (2011) The run chart: a simple analytical tool for learning from variation in healthcare processes. BMJ Qual Saf 20:46–51
Birkinshaw J, Haas JB (2016) Increase your return on failure. Harv Bus Rev https://hbr.org/2016/05/increase-your-return-on-failure. Accessed 04 Jan 2018
Rubenstein LV, Hempel S, Farmer MM, Asch SM, Yano EM, Dougherty D, Shekelle PW (2008) Finding order in heterogeneity: types of quality-improvement intervention publications. Qual Saf Health Care 17:403–408
Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D (2016) SQUIRE 2.0-standards for quality improvement reporting excellence-revised publication guidelines from a detailed consensus process. J Am Coll Surg 222:317–323
Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D (2015) SQUIRE 2.0 (standards for quality improvement reporting excellence): revised publication guidelines from a detailed consensus process. Jt Comm J Qual Patient Saf 41:474–479
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Answers: 1b 2d 3e 4c 5d
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gaudreault-Tremblay, MM., McQuillan, R.F., Parekh, R.S. et al. Quality improvement in pediatric nephrology—a practical guide. Pediatr Nephrol 35, 199–211 (2020). https://doi.org/10.1007/s00467-018-4175-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-018-4175-0