Abstract
The calcineurin inhibitor tacrolimus, cornerstone of most immunosuppressive regimens, is a drug with a narrow therapeutic window: underexposure can lead to allograft rejection and overexposure can result in an increased incidence of infections, toxicity and malignancies. Tacrolimus is metabolised in the liver and intestine by the cytochrome P450 3A (CYP3A) isoforms CYP3A4 and CYP3A5. This review focusses on the clinical aspects of tacrolimus pharmacodynamics, such as efficacy and toxicity. Factors affecting tacrolimus pharmacokinetics, including pharmacogenetics and the rationale for routine CYP3A5*1/*3 genotyping in prospective paediatric renal transplant recipients, are also reviewed. Therapeutic drug monitoring, including pre-dose concentrations and pharmacokinetic profiles with the available “reference values”, are discussed. Factors contributing to high intra-patient variability in tacrolimus exposure and its impact on clinical outcome are also reviewed. Lastly, suggestions for future research and clinical perspectives are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The calcineurin inhibitor (CNI) tacrolimus (TAC), a macrolide lactone isolated from Streptomyces tsukubaensis, is the cornerstone of most immunosuppressive regimens in solid organ transplantation. In paediatric renal transplant recipients TAC has been shown to be more effective than cyclosporine (CsA)-based regimens in preventing acute rejection and improving long-term graft survival [1, 2].
A number of factors playing a role in the pharmacokinetic variability of TAC have been identified. These include patient characteristics, such as age or weight [3, 4], concomitant immunosuppression, such as corticosteroids or other co-medications (e.g. antibiotics) and polymorphism of the genes encoding the enzyme proteins involved in TAC metabolism [4, 5].
The unequivocal benefits of TAC must be counterbalanced against its side effects. Moreover, the multiple drug-to-drug interactions with inducers and inhibitors of the cytochrome P450 3A (CYP3A) isoforms CYP3A4/A5 increase the risk of TAC under- or overexposure. This review focusses on the clinical aspects of TAC pharmacodynamics, such as efficacy and toxicity, therapeutic drug monitoring (TDM), including pharmacokinetic and pharmacogenetic factors, and the impact of intra-patient variability in TAC pre-dose concentrations C0) on allograft outcomes.
Pharmacodynamics of TAC: mechanism of action and toxicity
Tacrolimus exerts its immunosuppressive effects primarily by affecting T-lymphocyte activation through inhibition of the enzyme calcineurin (CN). CN was originally isolated from neuronal tissue and exhibits calcium-binding properties, hence its name. In the cytoplasm calcium binding leads to CN activation and dephosphorylation of the nuclear factor of activated T cells (NFAT). Dephosphorylated NFAT translocates to the nucleus and forms complexes with transcriptional proteins, thereby inducing the transcription of genes required for the proliferation and activation of T-lymphocytes, including interleukin (IL)-2, IL-4 and interferon gamma. TAC forms intracellular complexes with specific immunophilin-binding proteins in the cytoplasm. These complexes bind CN, preventing dephosphorylation and nuclear translocation of NFAT, thereby inhibiting T- lymphocyte activation [6]. The mechanism of action of TAC is depicted in Fig. 1.
Mechanism of action of tacrolimus (TAC). Calcium binding leads to calcineurin (CN) activation and dephosphorylation (P) of the nuclear factor of activated T cells (NFAT). Dephosphorylated NFAT translocates to the nucleus and forms complexes with transcriptional proteins, inducing the transcription of genes required for the activation of T-lymphocytes (interleukin [IL]-2, IL-4 and interferon gamma [IF-γ]). TAC forms intracellular complexes with immunophilins, and these complexes bind CN, preventing the dephosphorylation and nuclear translocation of NFAT
In addition to T-lymphocytes, CN is expressed in other tissues, including the brain, spleen, thymus, platelets, heart, liver, testes, pancreas and kidney [7, 8]. Numerous actions have been attributed to CN, including a role in programmed death of neuronal cells, cardiac morphogenesis and induction of cardiac hypertrophy, regulation of the Na+, K+-ATPase in the kidney and neutrophil migration [7, 8]. These diverse actions explain why in addition to immunosuppression, TAC also displays an array of side effects, as listed in Table 1. An important consideration with regard to the use of TAC in adolescents is the fact that in contrast to CsA, TAC is rarely associated with hirsutism, gingivitis and gum hyperplasia, but it can cause alopecia and pruritus in some patients [10].
Acute and chronic nephrotoxicity
There is evidence to suggest that the use of TAC is associated with a lower risk of nephrotoxicity as compared with CsA. This can be explained by the weaker vasoconstrictive effects and fibrogenic potential of TAC relative to CsA [9] and has been demonstrated in clinical studies [22, 23].
Acute nephrotoxicity usually occurs within several days after the initiation of TAC treatment and may present as oligo- or anuria and a rapid rise in serum creatinine level. The acute nephrotoxic effects are typically reversible upon dose reduction or withdrawal of TAC. There is evidence to suggest that the predisposition to develop acute TAC-induced nephrotoxicity might be associated with the polymorphism of T-lymphocyte regulatory genes [24].
In contrast, chronic TAC-induced nephrotoxicity develops gradually and is clinically manifested as a slow decline in renal function, often with proteinuria and hypertension. While arterial hyalinosis was initially reported as a hallmark of CNI-associated nephropathy [25], more recent data suggest that damage mediated by donor-specific anti-HLA antibodies (chronic antibody-mediated rejection) might also underlie these pathologic changes [26]. Data from adult renal organ transplant recipients suggest an association between a low renal p-glycoprotein expression and the occurrence of histological damage in renal allografts [27, 28].
Pharmacokinetics of TAC
Tacrolimus is poorly absorbed in the gastrointestinal tract with a low and variable bioavailability in adults (mean 25%; range 4–93%) [29]. It is extensively bound to erythrocytes, with TAC whole blood concentrations exceeding about 15- to 35-fold those measured in plasma. Therefore, TAC whole blood concentrations are most widely used in clinical practice. In turn, > 90% of the TAC present in plasma is bound to proteins, mainly to α-1 acid glycoprotein and albumin. TAC is metabolised by the liver and intestinal CYP isoenzymes CYP3A4/A5 and is also a substrate to ATP-binding cassette protein B1 (ABCB1). The main route of excretion is the biliary tract and faeces. The elimination half-life of TAC is 12 (range 4–41) h. Liver failure might impact TAC elimination. In contrast, renal function impairment does not have an influence on TAC clearance [30,31,32].
The major TAC metabolite is the 13-O dimethyl metabolite which exhibits a low immunosuppressive activity, but can be quantified in blood [33]. In contrast, the 31-O-demethyl metabolite has been shown to be equipotent to TAC and to exhibit a considerable immunosuppressive activity. However, in a clinical setting the concentrations of 31-O-demethyl metabolite were too low to allow a pharmacokinetic analysis [33].
Factors affecting TAC pharmacokinetics
The inter-individual (or between patient) differences in TAC exposure are related to patient characteristics, such as weight and age, laboratory parameters such as haematocrit (Hct), concomitant medications and pharmacogenetic diversity of the CYP3A4/A5 genes which will be discussed later in this review.
Compared with adults, the impact of weight on TAC pharmacokinetics is much more prominent in studies including paediatric renal transplant recipients [4, 5]. It is known that young children have significantly higher relative TAC dose requirements than adults [3]. The explanation of this phenomenon is not entirely clear. It is assumed that the hepatic CYP3A4/A5 attains its full adult activity by the age of 1–2 years [34], but the maturation of the intestinal CYP3A4/A5 and phase II enzymes such as p-glycoprotein remain to be elucidated. Moreover, many factors can be involved in the variability in pharmacokinetics between adults and children, including intestinal uptake, hepatic blood flow and the proportion of liver to body weight, nutrition and underlying disease [10, 30]. In most healthy children weight and age can be used interchangeably, but this does not always hold true for paediatric patients with chronic kidney disease for whom failure to thrive is common. Naesens et al. reported that children older than 5 years at transplantation had lower weight-normalised TAC dose requirements with increasing age [35]. Knops et al. showed that children exhibit a biphasic course in TAC disposition characterised by a high and stable drug clearance until puberty followed by a significant decline in relative dose requirements thereafter [3]. In contrast, two paediatric pharmacokinetic studies have shown no improvement of an allometric population model after the addition of age as a covariate, leading the respective authors to conclude that adjustments in the TAC dose should be based on the child’s weight rather than age [4, 5].
TAC binds to erythrocytes, and the unbound fraction in blood is < 1%. Total TAC concentrations are measured in whole blood, while it is the unbound fraction that exerts pharmacological effects. The increase in total TAC concentration following a rise in Hct does not lead to an increase in the unbound fraction of the drug [36]. Therefore, the changes in TAC concentrations related to changes in Hct level should not lead to a prompt adjustment of dose [37]. Similar considerations apply to TAC dose amendment following rapid changes in plasma proteins.
Factors affecting TAC pharmacokinetics in paediatric renal transplant recipients identified by population modelling are listed in Table 2.
Drug–drug interactions
As corticosteroids exhibit CYP3A4-inducing properties, TAC dose requirements may be lower following corticosteroid dose reduction or withdrawal [41]. However, it is possible that this applies only to patients treated with higher doses of corticosteroids as no association has been found between the use of cortiocsteroids and TAC pharmacokinetics in paediatric pharmacokinetic studies [4, 5].
Importantly, in contrast to CsA, TAC has no effect on mycophenolic acid (MPA) exposure. CsA inhibits the multidrug resistance protein 2-mediated transport of 7-O-MPA glucuronide into the bile, leading to less MPA exposure. 7-O-MPA glucuronide is subject to enzymatic and non-enzymatic hydrolysis in bile and, more importantly, in the intestine, thereby liberating the unconjugated drug MPA, which is then reabsorbed into the systemic circulation. This enterohepatic circulation is responsible for a secondary MPA peak occurring 6–12 h after administration, which can account for up to 10–60% of the total dose-interval MPA-area under the time–concentration curve (AUC) [42]. The consequence of this interaction is that when MPA is used in combination with TAC, its dose should be lower than when it is used in combination with CsA [43]. In the TWIST study, the dose of concomitant mycophenolate mofetil (MMF) in combination with TAC in stable paediatric renal transplant recipients was 600 mg/m2 [44], while in combination with CsA the MMF dose is usually 1200 mg/m2.
Moreover, as TAC is metabolised by CYP3A4/A5, the inducers and inhibitors of these enzymes will have a clinically significant impact on TAC pharmacokinetics [45]. The clinically relevant drug–drug interactions are depicted in Fig. 2. The use of grapefruit juice or herbal medications by patients receiving TAC should be discouraged. While commencing or discontinuing co-medication(s) that might affect TAC blood levels, a period of meticulous TDM is recommended until the TAC pre-dose concentrations are stable [46]. When using potent CYP3A4/A5 inducers or inhibitors (see also Fig. 2), a preventive TAC dose adjustment of 30% followed by strict TDM may be applied. In case of an acute TAC intoxication, the use of a potent CYP3A4 inducer, such as phenytoin, to accelerate TAC clearance may be considered [47].
Relevant drug–drug interactions of TAC. HCV Hepatitis C virus, HIV human immunodeficiency virus. Adapted from the European Medicines Agency website (www.ema.europa.eu)
Pharmacogenetics of TAC
Tacrolimus is metabolised in the liver and intestine by the CYP3A isoforms CYP3A4 and CYP3A5. It is also a substrate for the multidrug efflux transporter glycoprotein that is expressed on various epithelial and endothelial cells and lymphocytes and encoded by the ABCB1 gene [48]. Polymorphisms of the CYP iso-enzymes 3A4 and 3A5 as well as of the ABCB1 gene have been extensively studied in adults with regard to TAC pharmacokinetics, and CYP3A5*1/*3 alleles have been shown to be the most significant in terms of TAC dose requirements. Although the CYP3A5 protein in the liver is detectable only in 10–40% of the Caucasian population [49], it may account for up to 50% of total hepatic CYP3A content in some individuals [50]. It has been shown that the incidence of the CYP3A5*1 allele (homo- or heterozygote) is around 15–25% in West-European populations [4, 51] and exceeds 50% in African Americans [52, 53].
The CYP3A5*1 allele constitutes the wildtype allele, with enzyme activity leading to higher TAC dose requirements, whereas the CYP3A5*3 allele results in an absence of protein activity. Carriers of CYP3A5*1 are also referred to as CYP3A5 expressers, whereas CYP3A5*3 homozygotes are referred to as CYP3A5 non-expressers. CYP3A5 expressers (genotype CYP3A5*1/*1 or CYP3A5*1/*3) require higher TAC doses to achieve a given TAC concentration. The recommendation for adult solid organ transplant recipients is to increase the standard TAC dose by 1.5- to 2-fold in CYP3A5 expressers, but not to exceed the daily dose of 0.3 mg/kg, followed by strict TDM [48].
Also in children it has been shown that the CYP3A5 polymorphism has a significant effect on the pharmacokinetic variability of TAC (see also Tables 2, 3). Children with the CYP3A5*1 allele have higher TAC dose requirements than CYP3A5 non-expressers [54,55,56]. For children and adolescents with at least one CYP3A5*1 allele, a 1.5- to 2-fold increase in dose followed by TDM is recommended, similar to the recommendations for adults [48]. It should be acknowledged that although CYP3A5 can explain up to 45% of inter-individual TAC pharmacokinetic variability [57], other factors described above can also affect TAC disposition.
Of note, the CYP3A4*22 and POR*28 (POR: P450 oxidoreductase) alleles, two recently identified gene polymorphisms, have been found to impact TAC dose requirements in adults [58, 59] and children [60]. Elens et al. studied the impact of the CYP3A4*22 allele (rs35599367, C > T) in a cohort of 185 adult renal transplant recipients, most of whom were Caucasian. Carriers of the T allele had 33% lower mean TAC dose requirements than carriers of the wildtype C allele. The frequency of the T allele was 3.5% [61]. De Jonge et al. found that the POR*28 T allele in CYP3A5 expressers can lead to TAC underexposure. This effect was alleviated in CYP3A5 non-expressers [62].
Rationale for the routine CYP3A5*1/*3 testing
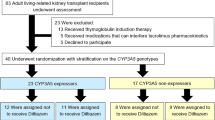
To date, there is no consensus on whether or not solid organ transplant candidates should routinely undergo CYP3A5 genotyping to guide the TAC dose. The recent guideline on the utility of CYP3A5 genotyping for TAC dosing in adults provides recommendations for solid organ transplant recipients with a known genotype, but does not advise for or against routine genotyping [48] because to date there is no evidence that routine CYP3A5 genotyping can positively impact patient outcomes. CYP3A5 expressers have higher TAC dose requirements and are potentially at risk for underexposure in the early post-transplantation period. A delay in achieving the target TAC concentrations in de novo transplant recipients may lead to acute rejection [63]. However, a Belgian study in adult renal transplant recipients showed that despite de novo renal transplant recipients who were CYP3A5 expressers needing more time to achieve the target pre-dose TAC concentrations, no association was found between the genetic polymorphism and patient outcomes, such as the incidence of acute rejection or graft dysfunction [58]. A recent Dutch randomised controlled trial investigated if adaptation of the starting TAC dose to the CYP3A5 genotype as compared with the standard body weight-based dosing would increase the proportion of de novo adult kidney transplant patients who achieved a target TAC C0 in steady state. The authors of this study found was no difference in the proportion of patients with the sub- or supra-therapeutic TAC C0. Moreover, there was no difference in the incidence of acute allograft rejection between the groups [64]. It has to be emphasised that data from adult patients may not be applicable to their paediatric counterparts, especially in children with a low weight. Although currently there is no evidence to support routine CYP3A5 genotyping in paediatric populations, the personal view of the authors is that this analysis should be performed in resourceful settings as it may be helpful in guiding TAC dose and anticipating potential interactions. Also, the CYP3A5 polymorphism may be relevant in other aspects of post-transplant care than immunosuppression. Vitamin D is catabolised by CYP3A4/A5, which implies that its genetic polymorphism may affect vitamin D concentrations [65].
TAC dose and TDM
Recommended starting dose
The recommendations for a patient-tailored TAC starting dose have been based on paediatric population pharmacokinetic models. In de novo renal transplant recipients a starting dose of 0.15 mg/kg twice daily was found to be too high for CYP3A5 non-expressers and for children weighing > 40 kg and too low for CYP3A5 expressers and for children with body weight of < 20 kg [5]. The target C0 was 5–15 ng/ml and the time since transplantation less than 2 months [5]. Recently, Andrews et al. showed a wide range in the starting TAC dose of between 0.27 and 1.33 mg/kg/day in children within 6 weeks after renal transplantation, with a target C0 of 5–15 ng/ml [40]. These dose recommendations are currently being evaluated in a prospective study.
In a paediatric study including patients beyond the first year from transplantation an additive effect of CYP3A5*1/*3 polymorphism and weight was reported in TAC dose simulations [4]. A TAC dose of 0.2 mg/kg/day would generate the following values: 5 ng/ml in a child weighing 20 kg and CYP3A5 expresser; 6 ng/ml in a child weighing 40 kg and CYP3A5 expresser; 8 ng/ml in a child weighing 20 kg and CYP3A5 non- expresser; and lastly 10 ng/ml in a child weighing 40 kg and CYP3A5 non-expresser [4]. These recommendations are similar to those published by Zhao et al. in de novo renal transplant recipients [5].
Methods of TDM
Therapeutic drug monitoring can be applied in two-ways: (1) a full or abbreviated pharmacokinetic profile where TAC concentrations are measured pre-dose and at given times following ingestion, or (2) pre- dose (trough) concentration C0). Obtaining a full 12-h pharmacokinetic profile is cumbersome and often requires a hospital admission. Therefore, abbreviated profiles for estimating TAC exposure have been performed and validated in adults [66] and children, where a profile including concentrations measured pre- and at 60 and 180 min after TAC ingestion showed a good correlation with the 12 h AUC [67]. The abbreviated AUC was predicted using Bayesian estimation. The following formula to calculate the full 12 h AUC was derived:
Although the most accurate way to measure TAC exposure is AUC as opposed to C0 [68, 69], there is no universal agreement on how often it should be applied. While in some centres AUC (full or abbreviated) is performed routinely at set times following transplantation, others use it on indication only, for example to elucidate the effect of concomitant medications on TAC exposure or in case of unexplained toxicity. In some paediatric renal transplant centers the TAC AUC is not performed routinely.
As performing even an abbreviated pharmacokinetic profile on a regular basis is not feasible, an adequate one-point sampling for estimation of TAC exposure remains essential. In most centres, TAC dose is guided by C0 obtained from a morning blood sample. To date, C0 remains an optimal time-point of TAC concentration sampling. TAC pharmacokinetics can be affected by concomitant food ingestion, especially fatty meals. While a standard continental breakfast in most patients does not lead to major changes in TAC exposure [70], it has been shown that the TAC AUC decreases significantly when TAC is taken with a fatty meal [71]. Obtaining a pre-dose TAC concentration from a morning sample in comparison with an evening sample is more “uniform” because most patients fast overnight and take breakfast only after TAC ingestion.
TDM: “reference values”
While defining a target TAC C0, the analytical method used to measure TAC concentration should be considered. A problem with immunoassays such as the enzyme-linked immunosorbent assay and microparticle enzyme immunoassay is the cross-reactivity of the antibody with TAC metabolites. Nowadays the liquid chromatography–tandem mass spectrometry technique is being increasingly applied, yielding 15–25% lower TAC concentrations in comparison with immunoassays as the cross-reactivity with TAC metabolites is eliminated [72, 73].
Achieving therapeutic concentrations of TAC can impact patient outcomes. As shown in the SYMPHONY trial, adult de novo renal transplant patients with a target TAC C0 of 3–7 ng/ml had a higher glomerular filtration rate and a lower incidence of acute rejection 1 year following transplantation than those treated with CsA or sirolimus [74]. However, in the above cited trial no comparison was made between various target TAC C0 head-to-head and patient outcomes. In adults, a target TAC C0 between 5 and 10 ng/ml in solid organ transplant recipients has been defined in a regimen including basiliximab, TAC, mycophenolate mofetil (MMF) and corticosteroids [75]. A recent study in adult renal transplant recipients on triple immunosuppression therapy including tacrolimus, MMF and corticosteroids showed that a mean TAC C0 of < 8 ng/ml was associated with the formation of donor specific antibodies (DSA) and a graded increase in risk with lower mean TAC C0 [76]. An increased risk of DSA formation might be an important consideration against CNI minimisation in renal transplant recipients.
There are no prospective trials analysing patient outcomes according to the target TAC C0 in the paediatric literature. In a prospective study on the feasibility of adding basiliximab to the standard immunosuppressive protocol of TAC, azathioprine and corticosteroids, the target TAC C0 were set at 10–20 ng/ml on days 0–21 and 5–15 ng/ml on days 22–183 [77]. The same target C0 were applied in the TWIST study that analysed the safety of early corticosteroid withdrawal in paediatric renal transplant recipients on combined therapy with TAC and MMF [44]. In some children TAC is used in combination with a mammalian target of rapamycin inhibitor, everolimus or sirolimus, with the aim to reduce nephrotoxicity; this strategy has proven to be beneficial in terms of cytomegalovirus replication and disease [78]. In this case the target TAC C0 is reduced.
In particular situations, such as very small kidney recipients or in CYP3A5 expressers, a three-times daily dosing regimen is sometimes contemplated. The rationale for this approach are the higher peak concentrations required to attain a given AUC with two-times daily regimens compared with three-times daily regimens. This approach is sometimes applied, but clinical data are very limited [79]. Evidence on the deleterious effect of high peak concentrations on the renal function is also weak. Of note, this approach of dosing three times daily might be challenging in terms of therapy adherence.
Designing a prospective trial with respect to the target TAC C0 would be challenging keeping in mind the heterogeneity in recipient-, donor- and centre-related characteristics regarding, for example, the underlying cause of end stage renal disease, repeat versus de novo transplantation, donor age and cardiovascular risk factors and concomitant immunosuppression. Moreover, in the era of personalised medicine the “one-dose-fits-all” approach is becoming obsolete. Ideally, the TAC dose and target C0 and AUC should be customised according to the state of over-and under-immunosuppression, clinically reflected as toxicity and allograft rejection, respectively. In this regard there is a growing interest in clinical application of biomarkers which allow an early and non-invasive detection of allograft injury [80]. An example of such a biomarker is the chemokine C-XC motif ligand 10 (CXCL10). It has been shown that increased urinary concentrations of CXCL10 are associated with acute rejection and BK virus infection in adult and paediatric renal transplant recipients [81].
Similarly to C0, the optimal target AUC values in paediatric renal transplant patients have not yet been established. Based on retrospective data and the locally applied protocol, Claeys et al. suggested an AUC of 150 h·ng/ml 1 year after transplantation in paediatric patients with a stable allograft function and around 90 h·ng/ml in the years thereafter [69]. During the first post-transplantation weeks A mean TAC AUC of 190–200 h·μg/l have been reported [82, 83]. In patients beyond the first year after transplantation the median AUC of 97 h·μg/l corresponded with a TAC C0 of 4–8 μg/l [4].
Intra-patient variability in TAC concentrations
In contrast to the inter-patient variability, the intra-patient variability (IPV) is defined as fluctuating pre-dose concentrations of a drug in a given period of time. This is also shown in Table 3. The TAC IPV can be quantified by calculating the coefficient of variation, the mean absolute variation or the variance [84].
The coefficient of variation is defined as a ratio of the standard deviation to the mean and can be calculated using the following formula:
where CV is the coefficient of variation, SD is the standard deviation, and X is the mean value of all analysed concentrations.
In most published studies to date TAC IPV was calculated in stable patients, 6 months from transplantation onwards [84]. There is a wide range of TAC IPV in adult and paediatric populations, from < 5 to > 50%, with average values of 15–30% [84]. Several factors influencing TAC IPV have been identified, including interactions with concomitant medications (see Fig. 2) and food [71], diarrhoea [85] and interchangeable administration of generic TAC formulations [86, 87]. Although conversion from the innovator product Prograf® to generic TAC has been found to be safe and did not lead to a significant TAC IPV in paediatric renal transplant recipients [88], the occurrence of acute allograft rejection shortly following conversion has been reported [88, 89]. Additional studies with extended follow-up are required to define the role of generic TAC in paediatric renal transplantation.
Poor adherence to immunosuppression has been postulated to play a key role in high TAC IPV, especially in adolescents [90]. This can be supported by the fact that adolescents have a poorer long-term graft survival than other age groups and a higher incidence of late acute rejection [91, 92].
High TAC IPV in renal transplant recipients is associated with poor patient outcomes, including inferior allograft survival, higher incidence of acute rejection and an increased risk of histologic lesions, such as moderate to severe fibrosis and tubular atrophy [90, 93,94,95]. Recently, high TAC IPV has been found to contribute to the development of donor specific HLA-antibodies [96]. The deleterious effect of a high TAC IPV has also been addressed in the paediatric literature. In a retrospective study including 69 paediatric renal transplant patients with a stable renal function, children and adolescents who experienced late acute rejection had a significantly higher variability coefficient than non-rejectors [97].
The potential strategies aimed at reducing of TAC IPV include improving non-adherence [98] and patient education regarding drug and food interactions with TAC. Conversion from the twice-daily to once-daily extended release TAC formulation may also contribute to a better adherence and a lower TAC IPV [99].
Future research and clinical perspectives
-
1)
There is a need for consensus on whether or not paediatric solid organ transplant candidates should routinely undergo CYP3A5 genotyping to guide the TAC dose. Selecting the starting dose based on a dosing algorithm that includes CYP3A5 genotype and a number of other variables may prove to be more valuable than genotype only.
-
2)
There is a lack of prospective randomised trials comparing different target values for TAC C0 and AUC on clinical outcomes in paediatric populations. Such studies would be helpful in providing evidence for the reference values for TAC C0 and AUC in paediatric renal transplant recipients.
-
3)
Clinical application of customised TAC dose and target C0/AUC for each patient; this will require the development and validation of biomarkers for a reliable assessment of the state of over- and under-immunosuppression in individual patients
-
4)
Attention should be given to the identification of factors associated with highly fluctuating TAC concentrations within an individual patient (e.g. poor therapy adherence, concomitant medications, interference with food, diarrhoeal illness, etc.). Interventions to reduce the intra-patient variability (e.g. patient education and switching to once-daily TAC formulation) may improve patient outcome.
-
5)
Paediatric studies with sufficiently long follow-up to assess the efficacy and safety of generic TAC formulations will support their implementation.
Summary
The important points of this review can be summarised as follows:
-
1.
TAC exerts its immunosuppressive effects through binding to calcineurin and inhibition of T-lymphocyte activation. As calcineurin is expressed in various tissues in the human body, TAC also displays a wide array of side effects.
-
2.
TAC has a narrow therapeutic window and therefore TDM is essential. The existing “reference values” for TAC pre-dose concentration and AUC are experience based rather than evidence based.
-
3.
CYP3A5*1/*3 polymorphism has a significant effect on TAC pharmacokinetics, but there is no consensus whether it should be routinely tested in children prior to renal transplantation. Prospective studies in adults have shown no beneficial effect of CYP3A5 genotyping on patient outcomes, but there are no paediatric studies.
-
4.
Intra-patient variability in TAC exposure is defined as fluctuating TAC pre-dose concentrations in a given period of time. It is associated with adverse outcomes following renal transplantation (allograft failure, late acute rejection, histologic changes such as fibrosis and tubular atrophy and formation of anti-HLA antibodies).
Multiple choice questions (answers are provided following the reference list)
-
1.
Which of the following is not a common side effect of tacrolimus
-
a)
Hypermagnesaemia
-
b)
Hypertension
-
c)
Tremor
-
d)
Hyperkalaemia
-
e)
De novo diabetes mellitus
-
a)
-
2.
Which of the following statements is true:
-
a)
TAC has a broad therapeutic window
-
b)
Food ingestion does not affect TAC pharmacokinetics
-
c)
While commencing treatment with fluconazole the dose of TAC should be increased to avoid underexposure and acute allograft rejection
-
d)
Children have higher relative TAC dose requirements than adults
-
e)
The difference in relative TAC dose requirements between adults and children can be explained by the maturation of the hepatic CYP3A4/A5
-
a)
-
3.
Which statement regarding TAC pharmacogenetics is true:
-
a)
The prevalence of the CYP3A5*1 allele is higher in Western European than in African populations
-
b)
CYP3A5 expressers have lower TAC dose requirements
-
c)
It has been shown that the routine pre-transplantation CYP3A5*1/*3 testing contributes to the lower incidence of acute allograft rejection in the early postoperative period
-
d)
It is recommended to increase the standard TAC dose by 1.5- to 2-fold in CYP3A5 expressers
-
a)
-
4.
Which statement is false:
-
a)
AUC is a more accurate method of evaluation of TAC exposure than a pre-dose concentration (trough level)
-
b)
TAC concentrations should be measured in plasma
-
c)
In most centers the target TAC pre-dose concentration 3 months after renal transplantation is set between 5 and 15 ng/ml
-
d)
There is a need to develop biomarkers which would allow an early and non-invasive detection of kidney injury
-
a)
-
5.
Intra-patient variability in TAC exposure:
-
a)
denotes the variability in exposure following administration of a given dose to children with the same weight
-
b)
is lowest in adolescents
-
c)
is associated with the risk of late acute allograft rejection
-
d)
statements a and c are true
-
e)
none of the above statement are true
-
a)
References
Filler G, Webb NJ, Milford DV, Watson AR, Gellermann J, Tyden G, Grenda R, Vondrak K, Hughes D, Offner G, Griebel M, Brekke IB, McGraw M, Balzar E, Friman S, Trompeter R (2005) Four-year data after pediatric renal transplantation: a randomized trial of tacrolimus vs. cyclosporin microemulsion. Pediatr Transplant 9:498–503
Neu AM, Ho PL, Fine RN, Furth SL, Fivush BA (2003) Tacrolimus vs. cyclosporine a as primary immunosuppression in pediatric renal transplantation: a NAPRTCS study. Pediatr Transplant 7:217–222
Knops N, Herman J, van Dyck M, Ramazani Y, Debbaut E, van Damme-Lombaerts R, Levtchenko E, van den Heuvel LP, Fieuws S, Kuypers D (2017) Tacrolimus dose requirements in paediatric renal allograft recipients are characterized by a biphasic course determined by age and bone maturation. Br J Clin Pharmacol 83:863–874
Prytula AA, Cransberg K, Bouts AH, van Schaik RH, de Jong H, de Wildt SN, Mathot RA (2016) The effect of weight and CYP3A5 genotype on the population pharmacokinetics of tacrolimus in stable Paediatric renal transplant recipients. Clin Pharmacokinet 55:1129–1143
Zhao W, Elie V, Roussey G, Brochard K, Niaudet P, Leroy V, Loirat C, Cochat P, Cloarec S, Andre JL, Garaix F, Bensman A, Fakhoury M, Jacqz-Aigrain E (2009) Population pharmacokinetics and pharmacogenetics of tacrolimus in de novo pediatric kidney transplant recipients. Clin Pharmacol Ther 86:609–618
Knops N, Levtchenko E, van den Heuvel B, Kuypers D (2013) From gut to kidney: transporting and metabolizing calcineurin-inhibitors in solid organ transplantation. Int J Pharm 452:14–35
Rusnak F, Mertz P (2000) Calcineurin: form and function. Physiol Rev 80:1483–1521
Klee CB, Ren H, Wang X (1998) Regulation of the calmodulin-stimulated protein phosphatase, calcineurin. J Biol Chem 273:13367–13370
Naesens M, Kuypers DR, Sarwal M (2009) Calcineurin inhibitor nephrotoxicity. Clin J Am Soc Nephrol 4:481–508
Staatz CE, Tett SE (2004) Clinical pharmacokinetics and pharmacodynamics of tacrolimus in solid organ transplantation. Clin Pharmacokinet 43:623–653
[No authors listed] (1994) Randomised trial comparing tacrolimus (FK506) and cyclosporin in prevention of liver allograft rejection. European FK506 Multicentre Liver Study Group. Lancet 344:423–428
Nakata Y, Yoshibayashi M, Yonemura T, Uemoto S, Inomata Y, Tanaka K, Furusho K (2000) Tacrolimus and myocardial hypertrophy. Transplantation 69:1960–1962
Prytula A, Vandekerckhove K, Raes A, De Wolf D, Dehoorne J, Vande Walle J, De Bruyne R (2016) Tacrolimus predose concentration is associated with hypertension in pediatric liver transplant recipients. J Pediatr Gastroenterol Nutr 63:616–623
Ikitimur B, Cosansu K, Karadag B, Cakmak HA, Avci BK, Erturk E, Seyahi N, Ongen Z (2015) Long-term impact of different immunosuppressive drugs on QT and PR intervals in renal transplant patients. Ann Noninvasive Electrocardiol 20:426–432
Ogunseinde BA, Wimmers E, Washington B, Iyob M, Cropper T, Callender CO (2003) A case of tacrolimus (FK506)-induced pancreatitis and fatality 2 years postcadaveric renal transplant. Transplantation 76:448
Hayes W, Boyle S, Carroll A, Bockenhauer D, Marks SD (2017) Hypomagnesemia and increased risk of new-onset diabetes mellitus after transplantation in pediatric renal transplant recipients. Pediatr Nephrol 32:879–884
Burroughs TE, Swindle JP, Salvalaggio PR, Lentine KL, Takemoto SK, Bunnapradist S, Brennan DC, Schnitzler MA (2009) Increasing incidence of new-onset diabetes after transplant among pediatric renal transplant patients. Transplantation 88:367–373
Bonthuis M, van Stralen KJ, Jager KJ, Baiko S, Jahnukainen T, Laube GF, Podracka L, Seeman T, Tyerman K, Ulinski T, Groothoff JW, Schaefer F, Verrina E (2014) Dyslipidaemia in children on renal replacement therapy. Nephrol Dial Transplant 29:594–603
Van Laecke S, Van Biesen W (2015) Hypomagnesaemia in kidney transplantation. Transplant Rev (Orlando) 29:154–160
Mohebbi N, Mihailova M, Wagner CA (2009) The calcineurin inhibitor FK506 (tacrolimus) is associated with transient metabolic acidosis and altered expression of renal acid-base transport proteins. Am J Physiol Ren Physiol 297:F499–F509
Georgiou GK, Dounousi E, Harissis HV (2016) Calcineurin inhibitors and male fertility after renal transplantation—a review. Andrologia 48:483–490
Ojo AO, Held PJ, Port FK, Wolfe RA, Leichtman AB, Young EW, Arndorfer J, Christensen L, Merion RM (2003) Chronic renal failure after transplantation of a nonrenal organ. N Engl J Med 349:931–940
Lucey MR, Abdelmalek MF, Gagliardi R, Granger D, Holt C, Kam I, Klintmalm G, Langnas A, Shetty K, Tzakis A, Woodle ES (2005) A comparison of tacrolimus and cyclosporine in liver transplantation: effects on renal function and cardiovascular risk status. Am J Transplant 5:1111–1119
Wu Z, Xu Q, Qiu X, Jiao Z, Zhang M, Zhong M (2017) FOXP3 rs3761548 polymorphism is associated with tacrolimus-induced acute nephrotoxicity in renal transplant patients. Eur J Clin Pharmacol 73:39–47
Nankivell BJ, Borrows RJ, Fung CL, O'Connell PJ, Allen RD, Chapman JR (2003) The natural history of chronic allograft nephropathy. N Engl J Med 349:2326–2333
Stegall MD, Park WD, Larson TS, Gloor JM, Cornell LD, Sethi S, Dean PG, Prieto M, Amer H, Textor S, Schwab T, Cosio FG (2011) The histology of solitary renal allografts at 1 and 5 years after transplantation. Am J Transplant 11:698–707
Naesens M, Lerut E, de Jonge H, Van Damme B, Vanrenterghem Y, Kuypers DR (2009) Donor age and renal P-glycoprotein expression associate with chronic histological damage in renal allografts. J Am Soc Nephrol 20:2468–2480
van Gelder T, van Schaik RH, Hesselink DA (2014) Pharmacogenetics and immunosuppressive drugs in solid organ transplantation. Nat Rev Nephrol 10:725–731
Scott LJ, McKeage K, Keam SJ, Plosker GL (2003) Tacrolimus: a further update of its use in the management of organ transplantation. Drugs 63:1247–1297
Zhao W, Fakhoury M, Jacqz-Aigrain E (2010) Developmental pharmacogenetics of immunosuppressants in pediatric organ transplantation. Ther Drug Monit 32:688–699
Venkataramanan R, Swaminathan A, Prasad T, Jain A, Zuckerman S, Warty V, McMichael J, Lever J, Burckart G, Starzl T (1995) Clinical pharmacokinetics of tacrolimus. Clin Pharmacokinet 29:404–430
Plosker GL, Foster RH (2000) Tacrolimus: a further update of its pharmacology and therapeutic use in the management of organ transplantation. Drugs 59:323–389
Mancinelli LM, Frassetto L, Floren LC, Dressler D, Carrier S, Bekersky I, Benet LZ, Christians U (2001) The pharmacokinetics and metabolic disposition of tacrolimus: a comparison across ethnic groups. Clin Pharmacol Ther 69:24–31
Bjorkman S (2006) Prediction of cytochrome p450-mediated hepatic drug clearance in neonates, infants and children : how accurate are available scaling methods? Clin Pharmacokinet 45:1–11
Naesens M, Salvatierra O, Li L, Kambham N, Concepcion W, Sarwal M (2008) Maturation of dose-corrected tacrolimus predose trough levels in pediatric kidney allograft recipients. Transplantation 85:1139–1145
Hebert MF, Zheng S, Hays K, Shen DD, Davis CL, Umans JG, Miodovnik M, Thummel KE, Easterling TR (2013) Interpreting tacrolimus concentrations during pregnancy and postpartum. Transplantation 95:908–915
Storset E, Holford N, Midtvedt K, Bremer S, Bergan S, Asberg A (2014) Importance of hematocrit for a tacrolimus target concentration strategy. Eur J Clin Pharmacol 70:65–77
Zhao W, Fakhoury M, Baudouin V, Storme T, Maisin A, Deschenes G, Jacqz-Aigrain E (2013) Population pharmacokinetics and pharmacogenetics of once daily prolonged-release formulation of tacrolimus in pediatric and adolescent kidney transplant recipients. Eur J Clin Pharmacol 69:189–195
Jacobo-Cabral CO, Garcia-Roca P, Romero-Tejeda EM, Reyes H, Medeiros M, Castaneda-Hernandez G, Troconiz IF (2015) Population pharmacokinetic analysis of tacrolimus in Mexican paediatric renal transplant patients: role of CYP3A5 genotype and formulation. Br J Clin Pharmacol 80:630–641
Andrews LM, Hesselink DA, van Gelder T, Koch BCP, Cornelissen EAM, Bruggemann RJM, van Schaik RHN, de Wildt SN, Cransberg K, de Winter BCM (2017) A population pharmacokinetic model to predict the individual starting dose of tacrolimus following pediatric renal transplantation. Clin Pharmacokinet. https://doi.org/10.1007/s40262-017-0567-8
van Duijnhoven EM, Boots JM, Christiaans MH, Stolk LM, Undre NA, van Hooff JP (2003) Increase in tacrolimus trough levels after steroid withdrawal. Transpl Int 16:721–725
Tonshoff B, David-Neto E, Ettenger R, Filler G, van Gelder T, Goebel J, Kuypers DR, Tsai E, Vinks AA, Weber LT, Zimmerhackl LB (2011) Pediatric aspects of therapeutic drug monitoring of mycophenolic acid in renal transplantation. Transplant Rev (Orlando) 25:78–89
Braun F, Schocklmann H, Ziegler E, Kunzendorf U, Armstrong VW, Renders L (2009) Increased mycophenolic acid exposure in stable kidney transplant recipients on tacrolimus as compared with those on sirolimus: implications for pharmacokinetics. Clin Pharmacol Ther 86:411–415
Grenda R, Watson A, Trompeter R, Tonshoff B, Jaray J, Fitzpatrick M, Murer L, Vondrak K, Maxwell H, van Damme-Lombaerts R, Loirat C, Mor E, Cochat P, Milford DV, Brown M, Webb NJ (2010) A randomized trial to assess the impact of early steroid withdrawal on growth in pediatric renal transplantation: the TWIST study. Am J Transplant 10:828–836
van Gelder T (2002) Drug interactions with tacrolimus. Drug Saf 25:707–712
Kidney Disease: Improving Global Outcomes Transplant Work G (2009) KDIGO clinical practice guideline for the care of kidney transplant recipients. Am J Transplant 9[Suppl 3]:S1–155
Bax K, Tijssen J, Rieder MJ, Filler G (2014) Rapid resolution of tacrolimus intoxication-induced AKI with a corticosteroid and phenytoin. Ann Pharmacother 48:1525–1528
Birdwell KA, Decker B, Barbarino JM, Peterson JF, Stein CM, Sadee W, Wang D, Vinks AA, He Y, Swen JJ, Leeder JS, van Schaik R, Thummel KE, Klein TE, Caudle KE, MacPhee IA (2015) Clinical pharmacogenetics implementation consortium (CPIC) guidelines for CYP3A5 genotype and tacrolimus dosing. Clin Pharmacol Ther 98:19–24
Hustert E, Haberl M, Burk O, Wolbold R, He YQ, Klein K, Nuessler AC, Neuhaus P, Klattig J, Eiselt R, Koch I, Zibat A, Brockmoller J, Halpert JR, Zanger UM, Wojnowski L (2001) The genetic determinants of the CYP3A5 polymorphism. Pharmacogenetics 11:773–779
Kuehl P, Zhang J, Lin Y, Lamba J, Assem M, Schuetz J, Watkins PB, Daly A, Wrighton SA, Hall SD, Maurel P, Relling M, Brimer C, Yasuda K, Venkataramanan R, Strom S, Thummel K, Boguski MS, Schuetz E (2001) Sequence diversity in CYP3A promoters and characterization of the genetic basis of polymorphic CYP3A5 expression. Nat Genet 27:383–391
Hesselink DA, van Schaik RH, van der Heiden IP, van der Werf M, Gregoor PJ, Lindemans J, Weimar W, van Gelder T (2003) Genetic polymorphisms of the CYP3A4, CYP3A5, and MDR-1 genes and pharmacokinetics of the calcineurin inhibitors cyclosporine and tacrolimus. Clin Pharmacol Ther 74:245–254
Oetting WS, Schladt DP, Guan W, Miller MB, Remmel RP, Dorr C, Sanghavi K, Mannon RB, Herrera B, Matas AJ, Salomon DR, Kwok PY, Keating BJ, Israni AK, Jacobson PA, De KAFI (2016) Genomewide association study of tacrolimus concentrations in African American kidney transplant recipients identifies multiple CYP3A5 alleles. Am J Transplant 16:574–582
Andrews LM, De Winter BC, Van Gelder T, Hesselink DA (2016) Consideration of the ethnic prevalence of genotypes in the clinical use of tacrolimus. Pharmacogenomics 17:1737–1740
Gijsen V, Mital S, van Schaik RH, Soldin OP, Soldin SJ, van der Heiden IP, Nulman I, Koren G, de Wildt SN (2011) Age and CYP3A5 genotype affect tacrolimus dosing requirements after transplant in pediatric heart recipients. J Heart Lung Transplant 30:1352–1359
de Wildt SN, van Schaik RH, Soldin OP, Soldin SJ, Brojeni PY, van der Heiden IP, Parshuram C, Nulman I, Koren G (2011) The interactions of age, genetics, and disease severity on tacrolimus dosing requirements after pediatric kidney and liver transplantation. Eur J Clin Pharmacol 67:1231–1241
Lalan S, Abdel-Rahman S, Gaedigk A, Leeder JS, Warady BA, Dai H, Blowey D (2014) Effect of CYP3A5 genotype, steroids, and azoles on tacrolimus in a pediatric renal transplant population. Pediatr Nephrol 29:2039–2049
Haufroid V, Mourad M, Van Kerckhove V, Wawrzyniak J, De Meyer M, Eddour DC, Malaise J, Lison D, Squifflet JP, Wallemacq P (2004) The effect of CYP3A5 and MDR1 (ABCB1) polymorphisms on cyclosporine and tacrolimus dose requirements and trough blood levels in stable renal transplant patients. Pharmacogenetics 14:147–154
Kuypers DR, de Loor H, Naesens M, Coopmans T, de Jonge H (2014) Combined effects of CYP3A5*1, POR*28, and CYP3A4*22 single nucleotide polymorphisms on early concentration-controlled tacrolimus exposure in de-novo renal recipients. Pharmacogenet Genomics 24:597–606
Elens L, van Gelder T, Hesselink DA, Haufroid V, van Schaik RH (2013) CYP3A4*22: promising newly identified CYP3A4 variant allele for personalizing pharmacotherapy. Pharmacogenomics 14:47–62
Gijsen VM, van Schaik RH, Soldin OP, Soldin SJ, Nulman I, Koren G, de Wildt SN (2014) P450 oxidoreductase *28 (POR*28) and tacrolimus disposition in pediatric kidney transplant recipients—a pilot study. Ther Drug Monit 36:152–158
Elens L, Bouamar R, Hesselink DA, Haufroid V, van der Heiden IP, van Gelder T, van Schaik RH (2011) A new functional CYP3A4 intron 6 polymorphism significantly affects tacrolimus pharmacokinetics in kidney transplant recipients. Clin Chem 57:1574–1583
de Jonge H, Metalidis C, Naesens M, Lambrechts D, Kuypers DR (2011) The P450 oxidoreductase *28 SNP is associated with low initial tacrolimus exposure and increased dose requirements in CYP3A5-expressing renal recipients. Pharmacogenomics 12:1281–1291
MacPhee IA, Fredericks S, Tai T, Syrris P, Carter ND, Johnston A, Goldberg L, Holt DW (2004) The influence of pharmacogenetics on the time to achieve target tacrolimus concentrations after kidney transplantation. Am J Transplant 4:914–919
Shuker N, Bouamar R, van Schaik RH, Clahsen-van Groningen MC, Damman J, Baan CC, van de Wetering J, Rowshani AT, Weimar W, van Gelder T, Hesselink DA (2015) A randomized controlled trial comparing the efficacy of CYP3A5 genotype-based with bodyweight-based tacrolimus dosing after living donor kidney transplantation. Am J Transplant 16:2085–2096
Prytula A, Cransberg K, Raes A (2017) CYP3A4 is a crosslink between vitamin D and calcineurin inhibitors in solid organ transplant recipients: implications for bone health. Pharmacogenomics J 17:481–487
Armendariz Y, Pou L, Cantarell C, Lopez R, Perello M, Capdevila L (2005) Evaluation of a limited sampling strategy to estimate area under the curve of tacrolimus in adult renal transplant patients. Ther Drug Monit 27:431–434
Zhao W, Fakhoury M, Baudouin V, Maisin A, Deschenes G, Jacqz-Aigrain E (2011) Limited sampling strategy for estimating individual exposure of tacrolimus in pediatric kidney transplant patients. Ther Drug Monit 33:681–687
Lee MN, Butani L (2007) Improved pharmacokinetic monitoring of tacrolimus exposure after pediatric renal transplantation. Pediatr Transplant 11:388–393
Claeys T, Van Dyck M, Van Damme-Lombaerts R (2010) Pharmacokinetics of tacrolimus in stable paediatric renal transplant recipients. Pediatr Nephrol 25:335–342
Stifft F, Undre N, van Hooff JP, Christiaans MH (2016) Effect of breakfast on the exposure of the once-daily tacrolimus formulation in stable kidney transplant recipients. Ther Drug Monit 38:456–462
Bekersky I, Dressler D, Mekki QA (2001) Effect of low- and high-fat meals on tacrolimus absorption following 5 mg single oral doses to healthy human subjects. J Clin Pharmacol 41:176–182
Staatz CE, Taylor PJ, Tett SE (2002) Comparison of an ELISA and an LC/MS/MS method for measuring tacrolimus concentrations and making dosage decisions in transplant recipients. Ther Drug Monit 24:607–615
Filler G, Smith N (2014) The need for tacrolimus assay standardization. Ther Drug Monit 36:693–695
Ekberg H, Tedesco-Silva H, Demirbas A, Vitko S, Nashan B, Gurkan A, Margreiter R, Hugo C, Grinyo JM, Frei U, Vanrenterghem Y, Daloze P, Halloran PF (2007) Reduced exposure to calcineurin inhibitors in renal transplantation. New Engl J Med 357:2562–2575
Wallemacq P, Armstrong VW, Brunet M, Haufroid V, Holt DW, Johnston A, Kuypers D, Le Meur Y, Marquet P, Oellerich M, Thervet E, Toenshoff B, Undre N, Weber LT, Westley IS, Mourad M (2009) Opportunities to optimize tacrolimus therapy in solid organ transplantation: report of the European consensus conference. Ther Drug Monit 31:139–152
Davis S, Gralla J, Klem P, Tong S, Wedermyer G, Freed B, Wiseman A, Cooper JE (2017) Lower tacrolimus exposure and time in therapeutic range increase the risk of de novo donor-specific antibodies in the first year of kidney transplantation. Am J Transplant. https://doi.org/10.1111/ajt.14504
Grenda R, Watson A, Vondrak K, Webb NJ, Beattie J, Fitzpatrick M, Saleem MA, Trompeter R, Milford DV, Moghal NE, Hughes D, Perner F, Friman S, Van Damme-Lombaerts R, Janssen F (2006) A prospective, randomized, multicenter trial of tacrolimus-based therapy with or without basiliximab in pediatric renal transplantation. Am J Transplant 6:1666–1672
Hocker B, Zencke S, Pape L, Krupka K, Koster L, Fichtner A, Dello Strologo L, Guzzo I, Topaloglu R, Kranz B, Konig J, Bald M, Webb NJ, Noyan A, Dursun H, Marks S, Ozcakar ZB, Thiel F, Billing H, Pohl M, Fehrenbach H, Schnitzler P, Bruckner T, Ahlenstiel-Grunow T, Tonshoff B (2016) Impact of everolimus and low-dose cyclosporin on cytomegalovirus replication and disease in pediatric renal transplantation. Am J Transplant 16:921–929
Martial LC, Verstegen RH, Cornelissen EA, Aarnoutse RE, Schreuder MF, Bruggemann RJ (2016) A preliminary study searching for the right dose of tacrolimus in very young (≤ 4 years) renal transplant patients. J Pharm Pharmacol 68:1366–1372
Brunet M, Shipkova M, van Gelder T, Wieland E, Sommerer C, Budde K, Haufroid V, Christians U, Lopez-Hoyos M, Barten MJ, Bergan S, Picard N, Millan Lopez O, Marquet P, Hesselink DA, Noceti O, Pawinski T, Wallemacq P, Oellerich M (2016) Barcelona consensus on biomarker-based immunosuppressive drugs management in solid organ transplantation. Ther Drug Monit 38[Suppl 1]:S1–20
Jackson JA, Kim EJ, Begley B, Cheeseman J, Harden T, Perez SD, Thomas S, Warshaw B, Kirk AD (2011) Urinary chemokines CXCL9 and CXCL10 are noninvasive markers of renal allograft rejection and BK viral infection. Am J Transplant 11:2228–2234
Kim JS, Aviles DH, Silverstein DM, Leblanc PL, Matti Vehaskari V (2005) Effect of age, ethnicity, and glucocorticoid use on tacrolimus pharmacokinetics in pediatric renal transplant patients. Pediatr Transplant 9:162–169
Montini G, Ujka F, Varagnolo C, Ghio L, Ginevri F, Murer L, Thafam BS, Carasi C, Zacchello G, Plebani M (2006) The pharmacokinetics and immunosuppressive response of tacrolimus in paediatric renal transplant recipients. Pediatr Nephrol 21:719–724
Shuker N, van Gelder T, Hesselink DA (2015) Intra-patient variability in tacrolimus exposure: causes, consequences for clinical management. Transplant Rev (Orlando) 29:78–84
Hochleitner BW, Bosmuller C, Nehoda H, Fruhwirt M, Simma B, Ellemunter H, Steurer W, Hochleitner EO, Konigsrainer A, Margreiter R (2001) Increased tacrolimus levels during diarrhea. Transpl Int 14:230–233
van Gelder T, Substitution EACoG (2011) European Society for Organ Transplantation Advisory Committee recommendations on generic substitution of immunosuppressive drugs. Transpl Int 24:1135–1141
Medeiros M, Lumini J, Stern N, Castaneda-Hernandez G, Filler G (2017) Generic immunosuppressants. Pediatr Nephrol. https://doi.org/10.1007/s00467-017-3735-z
Naicker D, Reed PW, Ronaldson J, Kara T, Wong W, Prestidge C (2017) Nationwide conversion to generic tacrolimus in pediatric kidney transplant recipients. Pediatr Nephrol 32:2125–2131
Abdulnour HA, Araya CE, Dharnidharka VR (2010) Comparison of generic tacrolimus and Prograf drug levels in a pediatric kidney transplant program: brief communication. Pediatr Transplant 14:1007–1011
Pollock-Barziv SM, Finkelstein Y, Manlhiot C, Dipchand AI, Hebert D, Ng VL, Solomon M, McCrindle BW, Grant D (2010) Variability in tacrolimus blood levels increases the risk of late rejection and graft loss after solid organ transplantation in older children. Pediatr Transplant 14:968–975
Smith JM, Ho PL, McDonald RA, North American Pediatric Renal Transplant Cooperative S (2002) Renal transplant outcomes in adolescents: a report of the north American pediatric renal transplant cooperative study. Pediatr Transplant 6:493–499
Van Arendonk KJ, James NT, Boyarsky BJ, Garonzik-Wang JM, Orandi BJ, Magee JC, Smith JM, Colombani PM, Segev DL (2013) Age at graft loss after pediatric kidney transplantation: exploring the high-risk age window. Clin J Am Soc Nephrol 8:1019–1026
Vanhove T, Vermeulen T, Annaert P, Lerut E, Kuypers DR (2016) High intrapatient variability of tacrolimus concentrations predicts accelerated progression of chronic histologic lesions in renal recipients. Am J Transplant 16:2954–2963
Borra LC, Roodnat JI, Kal JA, Mathot RA, Weimar W, van Gelder T (2010) High within-patient variability in the clearance of tacrolimus is a risk factor for poor long-term outcome after kidney transplantation. Nephrol Dial Transplant. 25(8):2757–2763.
Prytula AA, Bouts AH, Mathot RA, van Gelder T, Croes LK, Hop W, Cransberg K (2012) Intra-patient variability in tacrolimus trough concentrations and renal variability in the clearance of tacrolimus is a risk factor for poor long-term outcome after kidney transplantation. Nephrol Dial Transplant 25:2757–2763
O'Regan JA, Canney M, Connaughton DM, O'Kelly P, Williams Y, Collier G, deFreitas DG, O'Seaghdha CM, Conlon PJ (2015) Tacrolimus trough-level variability predicts long-term allograft survival following kidney transplantation. J Nephrol 29:269–276
Rodrigo E, Segundo DS, Fernandez-Fresnedo G, Lopez-Hoyos M, Benito A, Ruiz JC, de Cos MA, Arias M (2016) Within-patient variability in tacrolimus blood levels predicts kidney graft loss and donor-specific antibody development. Transplantation 100:2479-2485. Function decline in pediatric renal transplant recipients. Pediatr Transplant 16:613–618
Claes A, Decorte A, Levtchenko E, Knops N, Dobbels F (2014) Facilitators and barriers of medication adherence in pediatric liver and kidney transplant recipients: a mixed-methods study. Prog Transplant 24:311–321
Kuypers DR, Peeters PC, Sennesael JJ, Kianda MN, Vrijens B, Kristanto P, Dobbels F, Vanrenterghem Y, Kanaan N, Team AS (2013) Improved adherence to tacrolimus once-daily formulation in renal recipients: a randomized controlled trial using electronic monitoring. Transplantation 95:333–340
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Answers: 1. a; 2. d; 3. d; 4. b; 5. c
Rights and permissions
About this article
Cite this article
Prytuła, A., van Gelder, T. Clinical aspects of tacrolimus use in paediatric renal transplant recipients. Pediatr Nephrol 34, 31–43 (2019). https://doi.org/10.1007/s00467-018-3892-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-018-3892-8