Abstract
Background
Enuresis (NE) is a clinical condition of multifactorial etiology that leads to difficulties in child/adolescent social interaction.
Methods
This was a prospective study on the impact of multidisciplinary assessment of 6- to 17-year-old patients with monosymptomatic nocturnal enuresis (MNE), including a structured history, clinical/neurological examination, bladder and bowel diaries, sleep diary and questionnaires, psychological evaluation [Child Behavior Checklist (CBCL) and PedsQL 4.0 questionnaires], urinary sonography, blood and urine laboratory tests, polysonography (PSG), and balance evaluation.
Results
A total of 140 enuretic participants were evaluated, of whom 27 were diagnosed with NE complicated by urinary disorder, four with hypercalciuria, three with nephropathy and one with attention-deficit hyperactivity disorder. Among the 87 participants who underwent PSG, six were diagnosed with severe apnea. Of the 82 MNE patients who underwent full assessment, 62 were male (75.6 %), and the mean age was 9.5 (±2.6) years. A family history of NE was diagnosed in 91.1 % of first- and second-degree relatives, constipation in 89.3 % and mild/moderate apnea in 40.7 %. Balance control alteration was identified by physical therapy evaluation of MNE patients. Participants’ quality of life evaluation scores were significantly lower than those of their parents.
Conclusion
Enuresis is a multifactorial disorder that requires a structured diagnostic approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Monosymptomatic nocturnal enuresis (MNE) can be defined as the presence of urine incontinence during sleep, in the absence of daytime symptoms, in toilet-trained children of at least 5 years of age. Primary MNE is manifested by episodes of bedwetting since the acquisition of bladder control, while secondary MNE is characterized by urine incontinence during sleep after full bladder control has been acquired for at least six months [1, 2]. The concept of MNE infers the absence of functional or chronic conditions as causes of nocturnal urine loss. Enuresis (NE) affects approximately 10 % of 7-year-old children and 1–2 % of adolescents and young adults, with familial occurrence in most affected patients [3, 4].
MNE has been considered to result from a pathogenic triad that includes a lack of vasopressin secretion during sleep, instability and/or reduction of nocturnal bladder capacity and inability to awaken by the sensation of a full bladder [5]. It is recognized that a series of comorbid medical conditions [6] and behavioral changes, including such disorders as attention-deficit hyperactivity disorder (ADHD) [7] and opposition defiant disorder [8], can present as nocturnal enuresis, while MNE can be adversely affected by the coexistence of other conditions, such as the presence of constipation [9] and sleep apnea [10], among others. Immaturity of the nervous system in terms of bladder function regulation has been suggested as an etiological factor of MNE [11]. However, regarding MNE, the developmental delay does not seem to be specific to bladder control, since children with MNE and nocturnal enuresis with daytime symptoms present immature motor performance skills, with losses in fine and global motor function, slower motor performance particularly for repetitive hand and finger movements [12], reduced ability of visual–motor and spatial perception, dysarthria and incoordination [13], suggesting a maturation deficit in the motor cortex circuits and related cortical areas and a possible postural control deficit.
MNE is a multifactorial entity in which the genetic factor seems to be of great importance while the environmental, somatic and psychosocial factors play a modulatory role [3, 7]. Despite the advances in acknowledging the multiple factors that may play a role in the physiopathology of MNE, the need for patient evaluation by a multidisciplinary team has been rarely addressed in the literature [14]. In the study presented here, we used a multidisciplinary evaluation of children and adolescents with NE to differentiate, at presentation, MNE, non-monosymptomatic enuresis (NMNE) and enuresis associated with underlying chronic diseases, as well as to recognize comorbidities. The aim of applying this approach was to establish a multidisciplinary evaluated cohort of patients with MNE for future follow-up with specific therapeutic interventions.
Methods
This was a prospective study conducted from August 2011 to December 2012 by a multidisciplinary team involving the Pediatric Nephrology and Sleep Physiology Units of Instituto da Criança of Hospital das Clinicas of the University of São Paulo Medical School, the University of São Paulo Physical Therapy Division and the Behavioral Therapy Unit of the Department of Psychology of the University of São Paulo. A structured protocol was applied to identify patients with MNE. The inclusion criteria were: age between 6–17 years and MNE diagnosis according to the “International Children’s Continence Society” (ICCS) criteria [1, 2], which determine that incontinence should be exclusively nocturnal. In addition, the present cohort included only patients without previous urinary incontinence during the day.
Patients were recruited using digital media, AM/FM radio interviews and articles in newspapers and magazines. After registration, interested patients and their families received a questionnaire by mail which focused on socioeconomic aspects [15] and an inventory for behavior assessment of 6- to 18-year-old participants [Child Behavior Checklist (CBCL)] [16, 17].
The socioeconomic profile of the study participants was evaluated by the “Critério Brasil” questionnaire [15], which evaluates the degree of education of the head of the household and a number of household characteristics, such as presence and quantity of specific comfort items. The questionnaire awards points depending on household characteristics and results in an economic classification defined as social classes A1, A2, B1, B2, C1, C2, D and E.
The CBCL has been validated in Brazil and it is composed of 130 questions related to the social competence and behavior patterns of 6- to 18-year-old individuals in the last six months, as observed by parents. The questionnaire was designed to be answered in a maximum of 15 minutes and uses scores to enable clinical comparison: the child/adolescent profile is assessed in relation to their overall operation, internalizing profiles (including isolation issues, somatic complaints, anxiety/depression) and externalizing profiles (including violation of rules and aggressive behavior). For the present study a cut-off score of 60 was used; participants who scored above that cut-off were classified as borderline or clinical cases, and considered as a group, as recommended by Achenbach and Rescorla for research using the CBCL [17].
All participants who returned a completed CBCL were invited to an initial clinic visit in which, after signing an informed consent form, they were evaluated sequentially by a pediatric nephrologist, a pediatric neurologist, a physical therapist and a psychologist. Anamnesis was structured according to ICCS recommendations [1, 2] and followed by a complete clinical examination, completion of sleep disorders questionnaires (Berlin Questionnaire, Children’s Sleep Disorders Scale and Epworth Scale) [18–20], evaluation of balance and completion by patients and their caregivers of a quality of life questionnaire [Pediatric Quality of Life Inventory version 4.0 (PedsQL 4.0)] [21].
The neurological examination included perinatal history, evaluation of potential risk factors for neurological conditions, cognitive assessment (adequacy of responses and simple calculations, abstraction), static and dynamic balance, axial and appendicular coordination, muscle strength, bone-tendon reflexes and cranial nerve evaluation.
The physical therapy evaluation consisted of an assessment of balance. Balance is the ability to maintain body stability. Data were acquired using a system comprised of a force plate (EMG System do Brasil Ltda®, São José dos Campos, SP, Brazil) and an analogue digital convertor (OR6 12-bits) connected to a computer at a frequency of 100 Hz. A computerized program transformed the primary center of pressure (COP) signal into numeric data throughout the acquisition duration. COP is the point that results from the action of vertical forces projected onto the force plate. COP displacement reflects the body’s movements in the attempt to keep the center of mass within the boundaries of the weight-supporting base (both feet) and maintain the body’s balance. The children were asked to stand barefoot with their arms at their side on a force plate embedded in the laboratory floor and to remain motionless. Because integration of visual, somatosensory and vestibular information is essential for balance, data from 60 seconds (60-s) trials were collected under four different sensory conditions: (1) eyes open, standing on a stable surface, (2) eyes closed, standing on a stable surface, (3) eyes open, standing on an unstable surface and (4) eyes closed, standing on an unstable surface. A 60-s rest interval was allowed between each sensory condition trial [22].
At the end of the first visit, the participants were scheduled for complementary urine and blood tests, kidney and urinary tract ultrasound and polysonography (PSG). They were also given instructions to keep a diaries on fluid intake and urinary and bowel habits for seven days and on bedwetting frequency [1] and sleeping pattern [23] for 30 days.
A diaper was used in all patients during the PSG in order to characterize the nocturnal urine volume. Blood tests to evaluate complete blood count, urea, creatinine and venous blood gas were requested. Urine was initially evaluated by urinalysis and by the single-sample calcium/creatinine ratio. Urine culture was obtained if urinalysis suggested urinary infection. If the urinary calcium/creatinine ratio was ≥0.21, a 24-h urine calcium collection was performed (positive when ≥4 mg/kg in 24 h).
A full-night PSG was performed using an EMBLA N7000® recording system (Natus Medical Inc., Pleasanton, CA) with the capability for electroencephalogram (EEG), chin electromyogram (EMG), ocular electrodes (EOG), respiratory variables recording (nasal pressure cannula, thermistor, thoracic and abdominal belts for effort detection), left and right tibialis EMG, pulse and position sensors, peripheral oxygen saturation and snoring microphones. The sleep stage and respiratory, motor and cardiac events were scored following the 2012 American Academy of Sleep Medicine (AASM) specifications [23].
The morphology of the urinary system, bladder capacity, post-voiding residual urine (normal ≤20 ml) and bladder thickness (normal ≤3 mm) were evaluated by renal and urinary tract sonography [24]. A bladder volume of ≤65 % of expected bladder capacity for age identified a small capacity bladder, while a bladder volume of >150 % of expected bladder capacity for age identified an increased capacity bladder. Sonographic evaluation of the rectum transverse diameter was performed in sequence (normal <30 mm) as a tool for the diagnosis of constipation [2, 25].
ICCS criteria were used to characterize “nocturnal polyuria” [1], “frequent episodes” of NE were defined as ≥4 episodes of bedwetting per week [2]. Constipation was defined by anamnesis, as the elimination of hard stools with effort, pain or difficulty, soiling and bleeding around the stool, with or without increasing the interval between bowel movements [9]. Diagnosis of constipation was confirmed by the Rome III questionnaire [26], the Bristol stool scale [27], bowel diary and the rectum transverse diameter measurement by pelvic sonography [25].
At the end of the initial clinic visit, each participant and his/her caregiver, after receiving instructions from a designated psychologist, were asked to separately complete the PedsQL 4.0 [21] questionnaire (use of the PedsQL.4.0 was authorized by the institution which owns its copyright. As a general rule, this instrument takes 5 min to complete and has three models for application in three age groups, namely, 5–7 years, 8–12 years and 13–18 years, respectively. This instrument investigates problems that occurred in the last month in the areas of physical capacity (8 questions), emotional aspects (5 questions), social aspects (5 questions) and school activities (5 questions). Parents and participants are instructed to score “zero” when the presented issue “is never a problem”, and to rate as “four” issues than “almost always constitute a problem”. The resulting score is converted to a scale of 0 to 100, with higher values indicating a better quality of life.
After completion of the investigation, participants diagnosed with NMNE, MNE preceded by NMNE or enuresis associated with genetic syndromes or underlying chronic diseases, such as hypercalciuria, diabetes mellitus, diabetes insipidus, sickle cell anemia, urinary malformations, chronic kidney disease, severe sleep apnea, neurodevelopmental delay, convulsive syndromes or ADHD, were referred for a specialized evaluation.
Statistical analysis
Descriptive analysis was performed with the R computing program version 3.2.2, on a Mac OS X Yosemite (10.10.5) computer. Descriptive analysis of demographics, the history and clinical examination and laboratory tests, the structure of sleep, the results of the CBCL and PedsQL questionnaires and balance assessment was performed by calculating the frequency for categorical variables and determining the median, mean and standard deviation for continuous variables. A significance level of 5 % (p <0.05) was adopted. Comparison of PedsQL 4.0 Scale scores between patients/parents was performed utilizing the paired Student’s t test to compare means of scores. A level of significance of p < 0.05 was adopted.
Results
Interest in enrolling in the study protocol was manifested by 256 children and adolescents with NE, of whom 140 reached the clinical and laboratory evaluation phase. The structured protocol evaluation of these 140 participants resulted in the following diagnoses: NE complicated by urinary disorder and/or urinary infection (27 participants), hypercalciuria (4 participants), nephropathy (3 participants) and ADHD (1 participant). Of the remaining 105 participants who reached the clinical and laboratory evaluation phase, 17 failed to complete the study protocol, and 88 were scheduled for PSG. Of these latter 88 participants, one went into remission before the procedure; among the remaining 87 participants who did undergo PSG, six were diagnosed with severe apnea and sent for specialized follow-up.
The initial clinical findings of 82 MNE participants were evaluated, including the participant who went into remission. Among these 82 children adolescents, 62 were male (75.6 %), the mean age was 9.5 ± 2.6 years and 72 (85.2 %) presented with primary enuresis. Thirty-four had attempted some type of previous treatment for NE, and five patients had undergone more than one type of therapy. Thirteen patients (15.9 %) had attempted alternative therapies (psychotherapy, color therapy, homeopathy, acupuncture, etc.).
The socioeconomic survey of the families of patients with MNE showed that 59/81 (72.8 %) patients belonged to higher economic status categories (A, B).
Clinical evaluation
Anamnesis
Among the 82 patients evaluated, 65 (79.2 %) reported frequent NE episodes, with an average of 5.9 (±1.93) nights/week, 57 (69.5 %) reported one to two bedwetting episodes per night and 80 (97.6 %) had a history of nocturnal polyuria. The use of diapers at night was reported by 81 (98.8 %) patients. Only 47 (57.3 %) parents were able to provide information on the number of times their child urinated during the day. Information regarding the period of the first NE episode was not available for 17 of the 82 patients (20 %); 38 (46.4 %) patients reported the first NE episode after the second hour of sleep onset. Fifty-four parents (of 74) admitted making routine attempts to awaken their child during the night with the aim to take him/her to the toilet to urinate, and 50/56 parents reported that their children slept so very deeply that they could not be awakened at night under any circumstances.
Toilet training was initiated by family decision in 50 of the 82 (61 %) patients and by school demand in 18 (22 %) patients. History of prematurity and of admission to neonatal intensive care with orotracheal intubation was reported for 14 (18.7 %) patients. Other reported medical conditions were: respiratory diseases (34 patients, 41.5 %), headache (5 patients, 5.1 %), previous history of urinary tract infection (>12 months before study entry) (11 patients, 13.4 %).
History of bedwetting was reported for at least one family member during childhood in 71/78 (91 %) patients. In 15 % of respondents, a family history of NE was reported by both parents.
Of the 82 patients, constipation and functional fecal incontinence were reported in 37 (45.1 %) and six (7.3 %), respectively. The age of bowel toilet training occurred between 24 to 36 months in 48/82 (58.5 %) patients, 56/82 (68.3 %) patients described Bristol ≤3 and 61/64 (95.3 %) were positive for Rome III criteria.
Clinical examination
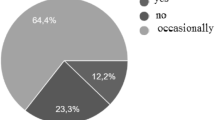
All 82 participants presented normal findings in the clinical and neurologic examination. The body mass index Z score was within normal range in 44 (53.7 %) patients, 25 (30.5 %) patients presented with overweight, obesity was diagnosed in ten (12.2 %) patients and malnutrition was diagnosed in three (3.7 %) patients.
Table 1 summarizes the main findings of the medical history and clinical examination of the participants diagnosed with MNE.
Bladder and bowel diary
All participants completed a diary on urinary and bowel habits diary for 7 days and a diary on bedwetting frequency for 30 days. The information given by the parents in the initial interview regarding their children’s micturition habits during the day was confirmed in most of the diaries. To the contrary, the number of “wet” nights initially reported by the parents greatly exceeded the number of events registered in the diary (p <0.00).
Sonography
Sonographic evaluation of the kidney and urinary tract demonstrated normal kidneys in all 82 patients. The mean bladder thickness was found to be 0.23 (±0.03) mm; bladder thickness was normal in 76 (92.7 %) patients and exceeded 3 mm in six (7.3 %) patients. The bladder capacity was normal in 55 (67.1 %) patients, and a small bladder capacity was determined in 27 (32.9 %) patients. Comparison of measured values by sonography with micturition volumes reported in the bladder diary revealed significantly higher volumes in the voiding diary (p <0.02).
The evaluation of the transverse diameter of the rectum by pelvic sonography showed an average value of 28.6 ± 0.77 mm; in 27 of the 82 (32.9 %) patients, the diameter of the rectum exceeded 30 mm.
Constipation and functional fecal incontinence
In 67 of the 82 (89.3 %) patients at least one of the adopted diagnostic criteria for constipation was positive. Constipation was treated with dietary orientation in all patients, but pharmacological treatment was necessary in 68 (82.9 %) patients, and 39/68 (57.4 %) patients were successfully managed with lactulose monotherapy.
Sleep diary and PSG
Snoring was diagnosed by the Sleep Disturbance Scale in Childhood in 31 of the 82 (37.8 %) patients; nine (11 %) patients had previously been submitted to adenotonsillectomy. Sleepwalking was reported in four (4.9 %) patients, nightmares in eight (9.9 %) patients and bruxism in 25 (30.9 %) patients. The scores on the Epworth Sleepiness Scale and the Questionnaire Berlin were normal for all the patients.
As previously described, PSG was performed in 87 of 88 patients with MNE. The apnea hypopnea index was considered to be normal in 48 (54.0 %) patients, mild (between 1 and 5 events per hour) in 30 (34.4 %) patients and moderate (5–10 events/h) in three (3.4 %) patients. Severe sleep apnea was confirmed in six of the 87 (6.9 %) participants who presented innocent findings during clinical evaluation. During PSG, nocturnal polyuria was confirmed by diaper weight in 21.3 % (17/82) of patients.
Physical therapy evaluation
As chronological age influences postural control, participants were divided into two age groups, Group A (between 6 and 11 years) and Group B (aged 12–16 years). Table 2 shows the descriptive analysis of the primary COP area in the four sensory conditions studied.
Psychological assessment
Of the 82 participants, 77 (93.9 %) completed the CBCL response analysis. The participants’ average scores remained below 60. The overall problem index averaged 58.2, with a median of 61, showing that, in general, participants were at the borderline range for behavioral problems. The index of externalizing problems, considered the most important causal factor for the treatment of enuresis, was on average 53.7 (±12.9), indicating a low frequency of this problem. The index of internalizing disorders was on average 58.2 (±11.6), with a median of 61, which is below the clinical range.
One participant presented characteristic behavioral changes compatible with ADHD during the initial clinic visit. This diagnosis was confirmed after further specialized evaluation.
The results of the PedsQL 4.0 questionnaire were analyzed in 65 of the 82 (79.3 %) patients. The responses of the children and parents/guardians are shown in Table 3.
Discussion
This study evaluated, in a cohort of patients with MNE, factors traditionally described in the literature as associated with NE [27–33], but not routinely assessed by a structured multidisciplinary protocol. Our results confirm that patients with NE may present multiple chronic clinical conditions and comorbidities. The prevalence rate of NE reported in epidemiological studies which have compared MNE and NMNE patients as groups, ranges from 6 to 28.6 % [32]. Most of these studies were developed before ICCS nomenclature standardization in 2006 [1].
In our study, MNE was characterized on the basis of structured anamnesis, complete physical examination, bladder and bowel diary evaluation and complementary work-up. Using this protocol, we were able to detect a significant proportion of participants who presented a chronic clinical condition that required specific care and who would therefore not benefit from inclusion in an MNE treatment protocol. The reported prevalence of constipation in the Brazilian pediatric population ranges from 14.7 to 38.5 % [34]. We were able to demonstrate constipation to be highly prevalent in our cohort, as already described in the literature [9, 28, 34]. As the diagnosis of constipation is still in need of a gold standard, we have included as instruments of evaluation, the Rome III criteria, a bowel diary, Bristol scale and measurement of the rectum diameter by sonography. Pharmacological treatment was necessary in 68 of the 82 (82.9 %) patients. A close relationship of constipation with MNE and NMNE is well described in the literature [2, 9, 28], which underscores the need for its identification and resolution prior to the initiation of MNE therapy.
We found that in our cohort of children and adolescents with MNE, the condition predominates in males and is frequently an inherited trait. These findings are in accordance with previously reported results from epidemiological studies. MNE has been reported to present predominantly without nocturnal polyuria and urinary incontinence to have a tendency to occur multiple times per night and in more than four nights a week [28–31]. Our results do differ from previously reported ones with respect to the reported predominance of children and adolescents of higher sociocultural level with MNE [29–31, 33]. It is possible that the media routes we selected to publicize the study did not reach the less economically privileged segments of the community. On the other hand, it may not be possible to extrapolate the results of the evaluation instrument that was used in our study, which was developed to evaluate the purchasing power of the Brazilian family unit, to those of international studies.
Based on universal parental experience, sleep in children with NE is deeper than that in non-enuretic ones [35]. The analysis of sleep in enuretic patients by neurophysiological variables, using EEG and PSG studies, has produced conflicting results. Some studies have found EEG signs of deeper sleep, based on an increased delta component during the night (N3 sleep percentage), while others have shown the sleep of enuretic patients to be more superficial [36] when compared with normal controls; in addition, there are studies in which no difference was demonstrated between the sleep of enuretic children sleep and either normative data [10, 37] or the sleep of a control group [38]. Our study participants presented with a normal sleep pattern, confirming the latter studies’ results.
In a recent literature review, the prevalence of childhood obstructive sleep apnea syndrome ranged from 0 to 5.7 % [39]. Our study’s participants presented a high prevalence of mild to severe sleep apnea (39/87; 46 %). The correlation between sleep enuresis (SE) and sleep disordered breathing (SDB) in both adults and children [40, 41] is supported by the improvement or full resolution of SE after treatment of SDB by adenotonsillectomy or intranasal corticosteroids [41, 42] and by community studies showing that children with habitual snoring had primary NE more often than those without snoring [43]. Therapy-resistant enuretic children were recently found to have subclinical signs of disordered breathing reflected by a high frequency of hypopneas, while the standard polysomnographic variables were normal [44]. Accordingly, another study showed that SE was significantly associated with presence of moderate-to-severe obstructive sleep apnea after adjustment for tonsillar hypertrophy, obesity, gender and age [45].
Recent studies have shown sleep fragmentation due to increased periodic leg movements during sleep in children with NE [46]. These studies however, included refractory NE from a tertiary care center and did not exclude children with ADHD or restless leg syndrome [46, 47]. In our study, we excluded any participant with a neurological and psychiatric condition that could be linked to increased movement during sleep. The participants in our study did not manifest periodic leg movements, but this alteration should be systematically evaluated in future studies.
The CBCL scores of our participants confirm the results of other published studies showing borderline range values for behavioral problems in all evaluated areas [6, 16, 48]. Our findings also demonstrate that patients with MNE present lower quality of life global ratings, especially in the physical and psychosocial spheres, as also shown in recent studies of NE [49, 50]. It is noteworthy that, in the present study, quality of life evaluation scores, as expressed by the participants, were significantly lower than the scores of their respective parents for the same questions, pointing out that parents may underestimate the quality of life compromise of their children. Moreover, the discrepancy between the intensity of the enuretic phenomena as per parents’ evaluation, during the structured anamnesis, and the NE frequency reported in the bladder diary may reflect the heavy burden NE poses to the family routine. The perception of a disrupted family routine due to NE may add to the reasons for the worse quality of life scores as per patients’ opinion. Treatment success most probably depends on direct emotional support of the child/adolescent by the clinical team.
There are no established normative values of balance for children and adolescents reported in the literature; neurological development promotes natural changes in these aspects, with the amplitude of body oscillations decreasing with age and muscular responses becoming more organized in the face of sudden disruptions with posture alignment and stability [12]. Our assessment of balance allowed us to identify delayed motor performance for age, with associated losses in motor skills suggesting motor cortex maturation deficit. The motor cortex includes areas of voluntary urination control, as well as areas for the planning and execution of fine movements. Any deficit in the maturation of these cortical areas can interfere directly with postural control, as the latter emerges from the dynamic interaction between the skeletal muscle, neural and sensory systems and involves control of the body’s position in space to maintain stability and guidance.
In conclusion, considering the multiple clinical conditions associated with NE, including the need to differentiate MNE and NMNE [51], the results of our study show that a full assessment of the NE patient is not only important but that it needs to be based on a structured protocol, with multidisciplinary assessment. Our data suggest that anamnesis, physical examination and elimination diaries need to be complemented minimally with a urine sample for conducting urinalysis and determining a urinary calcium/creatinine ratio and with a urinary sonography evaluation. This set of tools are useful to differentiate NMNE from MNE and serve as a guide for better therapeutic planning [1, 2, 50]. Our assessment of balance confirmed previous findings indicating that the MNE is associated with delayed motor performance for age, suggesting a motor cortex maturation deficit. This finding points out to research opportunities in elucidating NE pathogenesis, it may also possibly affect MNE treatment prognosis. Our data confirm that MNE may lead to poorer quality of life scores which may not be fully perceived by the patient’s caregivers, suggesting the need for a more individualized clinical follow-up of patients and their families.
The cohort of patients with MNE identified in our study will be part of a randomized trial of MNE. We suggest that the therapeutic response of the present cohort to different MNE treatment modalities may be optimized as, unlike cohorts from most of the available studies, it is constituted exclusively of monosymptomatic patients with therapeutically managed comorbidities.
References
Nevéus T, von Gontard A, Hoebeke P, Hjälmås K, Bauer S, Bower W, Jørgensen TM, Rittig S, Walle JV, Yeung CK, Djurhuus JC (2006) The standardization of terminology of lower urinary tract function in children and adolescents: report from the Standardisation Committee of the International Children’s Continence Society. J Urol 176:314–324
Austin PF, Bauer SB, Bower W, Chase J, Franco I, Hoebeke P, Rittig S, Walle JV, von Gontard A, Wright A, Yang SS, Nevéus T (2014) The standardization of terminology of lower urinary tract function in children and adolescents: update report from the Standardization Committee of the International Children’s Continence Society. J Urol 191:1863–1865
Yeung CK, Sihoe JD, Sit FK, Bower W, Sreedhar B, Lau J (2004) Characteristics of primary nocturnal enuresis in adults: an epidemiological study. Br J Urol Int 93:341–345
Von Gontard A, Schaumburg H, Hollmann E, Eiberg H, Rittig S (2001) The genetics of enuresis—a review. J Urol 166:2438
Butler RJ, Holland P (2000) The three systems: A conceptual way of understanding nocturnal enuresis. Scand J Urol Nephrol 34:270–277
von Gontard A, Niemczyk J, Weber M, Equit M (2014) Specific behavioral comorbidity in a large sample of children with functional incontinence: Report of 1,001 cases. Neurourol Urodyn 34:763–768
von Gontard A, Equit M (2015) Comorbidity of ADHD and incontinence in children. Eur Child Adolesc Psychiatry 24:127–140
Niemczyk J, Equit M, Braun-Bither K, Klein AM, Gontard V (2014) Prevalence of incontinence, attention deficit/hyperactivity disorder and oppositional defiant disorder in preschool children. Eur Child Adolesc Psychiatry 24:837–843
Borch L, Hagstroem S, Bower WF, Rittig CS, Rittig S (2013) Bladder and bowel dysfunction (BBD) and the resolution of urinary incontinence with succesfull management of bowel symptoms in children. Acta Paediatr 102:e215–e220
Nevéus T, Stenberg A, Läckgren G, Tuvemo T, Hetta J (1999) Sleep of children with enuresis: a polysomnographic study. Pediatrics 103:1193–1197
Baeyens D, Roeyers H, Naert S, Hoebeke P, Vande Walle J (2007) The impact of maturation of brainstem inhibition on enuresis: a startle eye blink modification study with 2-year followup. J Urol 178:2621–2625
von Gontard A, Freitag CM, Seifen S, Pukrop R, Rohling D (2006) Neuromotor development in nocturnal enuresis. Dev Med Child Neurol 48:744–750
Esposito M, Gallai B, Parisi L, Roccella M, Marotta R, Lavano SM, Mazzotta G, Patriciello G, Precenzano F, Carotenuto M (2013) Visuomotor competencies and primary monosymptomatic nocturnal enuresis in prepubertal aged children. Neuropsychiatr Dis Treat 9:921–926
Street E, Broughton L (1990) The treatment of childhood nocturnal enuresis in the community. Child Care Health Dev 16:365–372
Critério de Classificação Econômica Brasil 2009. Diretrizes de ordem geral, a serem consideradas pelas entidades prestadoras de serviços e seus clientes, a respeito da adoção do novo critério de classificação econômica brasil. Available at: http://www.abep.org/criterioBrasil.aspx. Accessed 26 April 2015
Santos EOL, Silvares EFM (2006) Enuretical children and referred children for university mental health services: a comparative study of their parents’ perception. Psicol Reflex Crit 19:277–282
Achenbach TM, Rescorla LA (2001) Manual for the ASEBA school—age forms and profiles. University of Vermont, Research Center for Children, Youths, and Families, Burlington
Ferreira VR, Carvalho LBC, Ruotolo F, Morais JF, Prado LBF, Prado GF (2009) Sleep disturbance scale for children: translation, cultural adaptation, and validation. Sleep Med 10:457–463
Vaz AP, Drummond M, Mota PC, Severo M, Almeida J, Winck JC (2011) Translation of Berlin questionnaire to Portuguese language and its application in OSA identification in a sleep disordered breathing clinic. Rev Port Pneumol 17:59–65
Bertolazi AN, Fagondes SC, Hoff LS, Pedro VD, Barreto SSM, Johns MW (2009) Portuguese-language version of the Epworth sleepiness scale: validation for use in Brazil. J Bras Pneumol 35:877–883
Klatchoian DA, Len CA, Terreri MT, Silva M, Itamoto C, Ciconelli RM, Varni JW, Hilário MO (2008) Quality of life of children and adolescents from São Paulo: reliability and validity of the Brazilian version of the Pediatric Quality of Life Inventory version 4.0 Generic Core Scales. J Pediatr 84:308–315
Winter DA (1995) Human balance and posture control during standing and walking. Gait Posture 3:193–214
Berry RB, Brooks R, Gamaldo CE, Harding SM, Marcus CL, Vauhn BV; for the American Academy of Sleep Medicine (2012) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications, version 2.0. www.aasmnet.org. American Academy of Sleep Medicine, Darien
Jequier S, Rousseau O (1987) Sonographic measurements of the normal bladder wall in children. AJR Am J Roentgenol 149:563–566
Joensson IM, Siggaard C, Rittig S, Hagstroem S, Djurhuus JC (2008) Transabdominal ultrasound of rectum as a diagnostic tool in childhood constipation. J Urol 179:1997–2002
Rasquin A, Di Lorenzo LC, Forbes D, Guiraldes E, Hyams JS, Staiano A, Walker LS (2006) Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology 130:1527–1537
Lewis SJ, Heaton KW (1997) Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol 32:920–924
Naseri M, Hiradfar M (2012) Monosymptomatic and non-monosymptomatic nocturnal enuresis: a clinical evaluation. Arch Iran Med 15:702–706
Fockema MW, Candy GP, Kruger D, Haffejee M (2012) Enuresis in South African children: prevalence, associated factors and parental perception of treatment. BJU Int 110(11 Pt C):E1114–E1120
Ozkan KU, Garipardic M, Toktamis A, Karabiber H, Sahinkanat T (2004) Enuresis prevalence and accompanying factors in schoolchildren: a questionnaire study from southeast Anatolia. Urol Int 73:149–155
Yeung CK, Sreedhar B, Sihoe JD, Sit FK, Lau J (2006) Differences in characteristics of nocturnal enuresis between children and adolescents: a critical appraisal from a large epidemiological study. BJU Int 97:1069–1073
Aljefri HM, Basurreh OA, Yunus F, Bawazir AA (2013) Nocturnal enuresis among primary school children. Saudi J Kidney Dis Transpl 24:1233–1241
Butler RJ, Golding J, Northstone K (2005) Nocturnal enuresis at 7.5 years old: Prevalence and analysis of clinical signs. BJU Int 96:404–410
Morais MB, Maffei HV (2006) Constipation. J Pediatr 76[Suppl 2]:S147–S156
Wolfish N, Pivik R, Busby K (1997) Elevated sleep arousal thresholds in enuretic boys: clinical implications. Acta Paediatr 86:381–384
Hunsballe JM (2000) Increased delta component in computerized sleep electroencephalographic analysis suggests abnormally deep sleep in primary monosymptomatic nocturnal enuresis. Scand J Urol Nephrol 34:294–302
Reimão R, Pachelli LC, Carneiro R, Faiwichow G (1993) Primary sleep enuresis in childhood: polysomnography evidences of sleep stage and time modulation. Arq Neuropsiquiatr 51:41–45
Inoue M, Shimojima H, Chiba H, Tsukahara N (1987) Rhythmic slow wave observed on nocturnal sleep encephalogram in children with idiopathic nocturnal enuresis. Sleep 10:570–579
Marcus CL, Brooks LJ, Draper KA, Gozal D, Halbower AC, Jones J, Schechter MS, Ward SD, Sheldon SH, Shiffman RN, Lehmann C, Spruyt K, American Academy of Pediatrics (2012) Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics 130(3):e714–e755
Brooks LJ, Topol HI (2003) Enuresis in children with sleep apnea. J Pediatr 142:515–518
Weider DJ, Sateia MJ, West RP (1991) Nocturnal enuresis in children with upper airway obstruction. Otolaryngol Head Neck Surg 105:427–432
Alexopoulos EI, Kaditis AG, Kostadima E, Gourgoulianis K (2005) Resolution of nocturnal enuresis in snoring children after treatment with nasal budesonide. Urology 66:194
Alexopoulos EI, Kostadima E, Pagonari I, Zintzaras E, Gourgoulianis K, Kaditis AG (2006) Association between primary nocturnal enuresis and habitual snoring in children. Urology 68:406–409
Nevéus T, Leissner L, Rudblad S, Bazargani F (2014) Respiration during sleep in children with therapy-resistant enuresis. Acta Paediatr 103:300–304
Alexopoulos EI, Malakasioti G, Varlami V, Miligkos M, Gourgoulianis K, Kaditis AG (2014) Nocturnal enuresis is associated with moderate-to-severe obstructive sleep apnea in children with snoring. Pediatr Res 76:555–559
Dhondt K, Baert E, Van Herzeele C, Raes A, Groen LA, Hoebeke P, Vande Walle J (2014) Sleep fragmentation and increased periodic limb movements are more common in children with nocturnal enuresis. Acta Paediatr 103:e268–e272
Dhondt K, Van Herzeele C, Roels SP, Raes A, Groen LA, Hoebeke P, Walle JV (2015) Sleep fragmentation and periodic limb movements in children with monosymptomatic nocturnal enuresis and polyuria. Pediatr Nephrol 30:1157–1162
Rocha MM, Costa NJ, Silvares EFM (2008) Changes in parents’ and self-reports of behavioral problems in Brazilian adolescents after behavioral treatment with urine alarm for nocturnal enuresis. Int Braz J Urol 34:749–757
Equit M, Hill J, Hübner A, von Gontard A (2014) Health-related quality of life and treatment effects on children with functional incontinence, and their parents. J Pediatr Urol 10:922–928
Naitoh Y, Kawauchi A, Soh J, Kamoi K, Miki T (2012) Health related quality of life for monosymptomatic enuretic children and their mothers. J Urol 188:1910–1914
Neveus T, Eggert P, Evans J, Macedo A, Rittig S, Tekgül S, Vande Walle J, Yeung CK, Robson L, International Children’s Continence Society (2010) Evaluation of and treatment for monosymptomatic enuresis: a standardization document from the International children’s continence society. J Urol 183:441–447
Acknowledgments
We thank Dr. J.W. Varni for permission to use the Peds QL 4.0 questionnaires and the MAPI Institute for their support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
This work was supported by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) Grant # 2011/17589-1.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
The study was approved by the Ethics Committee of Instituto da Criança of Hospital das Clínicas of the University of São Paulo Medical School in Research, number 0649/10, and informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Nascimento Fagundes, S., Azevedo Soster, L., Lebl, A.S. et al. Impact of a multidisciplinary evaluation in pediatric patients with nocturnal monosymptomatic enuresis. Pediatr Nephrol 31, 1295–1303 (2016). https://doi.org/10.1007/s00467-016-3316-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-016-3316-6