Abstract
Background
Non-calcium-containing phosphate binders, such as sevelamer preparations, are being increasingly used in patients on dialysis due to their lower association with hypercalcemia and cardiovascular morbidity and mortality. While minor gastrointestinal side effects are quite common with the use of sevelamer, more serious gastrointestinal toxicities have only rarely been reported.
Case—diagnosis/treatment
We report a pediatric patient on maintenance dialysis receiving sevelamer hydrochloride who developed severe abdominal pain and a high-grade stricture of the sigmoid colon. The patient underwent exploratory laparotomy, resulting in a partial colectomy and colostomy. Histopathologic examination showed colonic mucosal injury and characteristic “fish-scale”-like sevelamer hydrochloride crystals within the mucosa.
Conclusions
Whether the sevelamer crystals were causal, contributory or purely incidental remains to be clearly elucidated. However, our case raises sufficient concern to warrant additional investigation into whether there is a causal relationship between sevelamer use and intestinal mucosal injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sevelamer hydrochloride (Renagel®; Genzyme Corp., Cambridge, MA) is a non-calcium-based nonabsorbable polymer that is widely used as a phosphate binder in patients with end-stage renal disease (ESRD) to control serum phosphate levels [1]. Despite its high cost and reports of an association between its use and gastrointestinal (GI) adverse effects, such as constipation and abdominal pain [2], there has been an increase in sevelamer use due to its lower risk of hypercalcemia when compared to calcium-containing binders and to its propensity for decreasing low-density lipoprotein levels [2], both of which can increase cardioprotection [3]. To date, there have been very few reports of sevelamer products causing major life-threatening complications. Madan et al. reported the first case of stercoral ulceration as a complication from constipation caused by sevelamer hydrochloride in a 62-year-old woman; this condition developed within 1 month of the first administration of Renagel® [4]. In 2013, Swanson et al. were the first to describe a series of patients with chronic kidney disease (CKD) who presented with a variety of abdominal symptoms and were found to have sevelamer crystals in the sampled mucosa from several different GI tract sites (small bowel, large bowel, and esophagus) [5].
Here, we report our experience in caring for a teenager with ESRD who was on dialysis following a failed renal transplant and who presented with severe abdominal pain due to a stricture in the sigmoid colon. Histopathologic examination of the resection specimen showed mucosal injury and the presence of sevelamer crystals. To our knowledge, this is the first report of such an adverse effect in a pediatric patient, nor is it a listed complication of sevelamer use. Consequently, it is a case which warrants further investigation.
Case report
A 17-year-old Caucasian dialysis-dependent teenager presented to the emergency department with acute onset severe right lower quadrant abdominal pain. She had a long-standing history of CKD from multiple congenital anomalies, including a complex obstructive uropathy with ectopic ureters and a nonfunctioning right kidney. Her prior surgeries included anoplasty and creation of a sigmoid conduit in infancy and a revision of the conduit using the appendix as a catheterizable stoma 8 years previous in preparation for a renal transplant. Seven years previous, she had received a living donor renal transplant and undergone bilateral nephrectomies. Two months prior to her current admission, she lost her graft from recurrent rejection and urinary tract infections attributed to nonadherence with medications and catheterizations and was subsequently started on hemodialysis and sevelamer hydrochloride at a dose of 800 mg three times a day with meals. At baseline, she had intermittent loose stools, which were attributed to her medications and prior GI tract surgeries.
On admission, she was in severe pain and also endorsed nausea and a single episode of emesis. She noted having a bowel movement prior to the onset of pain that was not different from her baseline state. Imaging studies included an abdominal radiograph that showed moderate fecal burden but no dilated loops of bowel. A non-contrast computed tomography of the abdomen confirmed the moderate fecal burden as well as a left hemorrhagic ovarian cyst. No vascular calcifications were noted. Due to the concern for a possible GI obstruction based on the extent of the fecal burden and the observation that the fecal masses stopped short abruptly at the region of the sigmoid colon, a barium enema examination was performed. This demonstrated an 11-cm stricture and a high-grade obstruction at the junction of the descending and sigmoid colon. An emergent exploratory laparotomy was performed, which identified an intra-operatively, dilated descending colon with transition to colon of normal caliber. Fibrinous tissue was noted on the small bowel throughout its extent, and purulent fluid was found in the left pelvis. Sigmoidoscopy showed no signs of perforation. The dilated descending colon was resected with the transition point, and an end colostomy with a Hartmann’s pouch was created. The patient’s post-operative recovery was complicated by intermittent fevers; her intra-abdominal fluid collections grew Serratia marcescens and Abiotrophia/Granulicatella spp., for which she was treated with intravenous antibiotics and subsequently discharged.
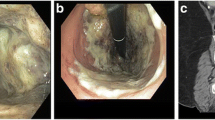
The dilated, impacted colon resection specimen demonstrated fibrotic changes within the bowel wall. A calcified fecalith had compressed and focally eroded the colonic mucosa, resulting in a foreign-body giant cell reaction within the subepithelial tissue. Proximal to the fecalith, numerous sevelamer crystals had accumulated in the bowel lumen, some in association with colonic mucosa that demonstrated acute ischemic-type injury and reactive epithelial changes (Fig. 1).
The administration of sevelamer was discontinued at discharge. At last follow-up, 2 months post-operatively, she was recovering well from her surgery.
Discussion
Hyperphosphatemia is a common occurrence in patients with ESRD on dialysis, necessitating dietary phosphorus restriction and the use of phosphate binders. Elevated serum phosphate levels have been shown to be a risk factor for increased cardiovascular and all-cause mortality, making it critical for healthcare providers to maintain phosphorus levels within the normal range [6]. In addition to its role as a phosphate binder with a lower risk of inducing hypercalcemia, sevelamer hydrochloride may have many other beneficial pleiotropic effects. Studies have shown that patients on sevelamer preparations have a slower progression of vascular calcification, increased trabecular bone density, decreased serum fibroblast growth factor-23 levels, lower levels of inflammatory markers (high-sensitivity C-reactive protein, interleukin-6, soluble CD14, tumor necrosis factor-alpha, and endotoxin), and fewer reactive oxygen species than those on calcium acetate [7]. Many of these features of sevelamer make it a desirable choice as a phosphate binder.
However, in addition to its adverse effects on the GI tract (e.g., nausea, vomiting, upper abdominal pain, and constipation), sevelamer hydrochloride has been associated with an increased risk of metabolic acidosis. This issue has supposedly been rectified with the development of sevelamer carbonate (Renvela®; Genzyme), although more research regarding its efficacy and side-effect profile is necessary [8].
Both sevelamer hydrochloride and sevelamer carbonate have been associated with constipation and abdominal pain in approximately 5–10 % of patients, with diarrhea, flatulence, and dyspepsia being slightly less often reported [2, 8]. Ethnic differences have been noted, with a higher reported incidence of constipation and vomiting in Japanese patients on hemodialysis, possibly attributable to differences in diet [9]. More serious GI side effects, as mentioned earlier, are rare.
In the study by Swanson et al., 14 endoscopic and one resection specimens collected from seven patients on sevelamer were found to have novel broad, irregularly spaced “fish-scale”-like crystals within the GI tract mucosa [5]. To confirm that the crystals were indeed derived from sevelamer, these investigators crushed sevelamer carbonate tablets (Renvela®; Genzyme) and submitted them for routine histological processing; the results suggested that the crystals were identical to those identified in the seven patients. The investigators also observed variation in the color of the crystals based on the characteristics of the adjacent tissue. Sevelamer crystals in ulcerated, ischemic, or necrotic tissue were deeply eosinophilic or rusty brown in color. In contrast, the sevelamer crystals in our patient were largely free-floating in the bowel lumen, with some having acquired a more deeply eosinophilic hue than the standard pale pink–yellow coloring normally seen on hematoxylin and eosin staining. Causality between the presence of sevelamer crystals and the GI symptomatology in the patients of the Swanson et al. study [5] and our patient is difficult to prove given the comorbidities that could have contributed to the development of GI symptoms.
However, Swanson et al. did observe a dose-dependent relationship between the sevelamer dose and severity of histologic mucosal injury [5]. Moreover, the acute mucosal injury seen adjacent to the sevelamer crystals raises the possibility that these crystals could have contributed to the injury. Certainly in our patient, it is quite likely that her stricture was at least partially a consequence of her prior sigmoid colon surgery. However, this surgery occurred 8 years prior to the development of her current GI symptoms, while the administration of sevelamer was begun only 2 months prior to the development of these GI symptoms. This time course, along with the presence of the characteristic “fish-scale”-like crystals in the pathologic bowel segment raises the possibility that sevelamer could have been a contributing, if not causal, factor in her symptomatology and may have led to worsening constipation and mucosal injury and inflammation. There was no radiologic or histopathologic evidence of vascular calcifications, and she had never developed elevated serum calcium levels over the last several years. Moreover, while she was receiving vitamin D supplementation, no calcium-containing phosphate binders had been prescribed to her. Taken together, it is highly unlikely that the acute ischemic changes in her descending colon were attributable to vascular calcium deposition.
In conclusion, patients with ESRD often have extensive medical comorbidities and sequelae associated with their CKD, thereby necessitating polypharmacy. Given the possibility, even if remote, that sevelamer crystals may be causally associated with mucosal injury and resultant GI complications, the benefits of sevelamer use in controlling phosphate levels need to be weighed against the risks of developing GI-associated sequelae. The purpose of our report is to highlight this rare observation in patients receiving sevelamer preparations and to caution healthcare providers taking care of pediatric patients with CKD to be aware of this potential risk. Particularly in patients who have undergone prior GI surgery or who have pre-existing abnormalities of the GI tract, sevelamer must be used with caution.
References
Navaneethan SD, Sakhuja A, Arrigain S, Sharp J, Schold JD, Nally JV Jr (2014) Practice patterns of phosphate binder use and their associations with mortality in chronic kidney disease. Clin Nephrol 82:16–25
Chen N, Wu X, Ding X, Mei C, Fu P, Jiang G, Li X, Chen J, Liu B, La Y, Hou F, Ni Z, Fu J, Xing C, Yu X, Huang C, Zuo L, Wang L, Hunter J, Dillon M, Plone M, Neylan J (2014) Sevelamer carbonate lowers serum phosphorus effectively in haemodialysis patients: a randomized, double-blind, placebo-controlled, dose-titration study. Nephrol Dial Transplant 29:152–160
Wang C, Liu X, Zhou Y, Li S, Chen Y, Wang Y, Lou T (2015) New conclusions regarding comparison of sevelamer and calcium-based phosphate binders in coronary-artery calcification for dialysis patients: a meta-analysis of randomized controlled trials. PLoS One 10:e0133938
Madan P, Bhayana S, Chandra P, Hughes JI (2008) Lower gastrointestinal bleeding: association with sevelamer use. World J Gastroenterol 14:2615–2616
Swanson BJ, Limketkai BN, Liu TC, Montgomery E, Nazari K, Park JY, Santangelo WC, Torbenson MS, Voltaggio L, Yearsley MM, Arnold CA (2013) Sevelamer crystals in the gastrointestinal tract (GIT): a new entity associated with mucosal injury. Am J Surg Pathol 37:1686–1693
Chang JF, Feng YF, Peng YS, Hsu SP, Pai MF, Chen HY, Wu HY, Yang JY (2014) Combined alkaline phosphatase and phosphorus levels as a predictor of mortality in maintenance hemodialysis patients. Medicine (Baltimore) 93:e106
Rastogi A (2013) Sevelamer revisited: pleiotropic effects on endothelial and cardiovascular risk factors in chronic kidney disease and end-stage renal disease. Ther Adv Cardiovasc Dis 7:322–342
Perry CM, Plosker GL (2014) Sevelamer carbonate: a review in hyperphosphataemia in adults with chronic kidney disease. Drugs 74:771–792
Iwasaki Y, Takami H, Tani M, Yamaguchi Y, Goto H, Goto Y, Goto Y, Shigematsu T (2005) Efficacy of combined sevelamer and calcium carbonate therapy for hyperphosphatemia in Japanese hemodialysis patients. Ther Apher Dial 9:347–351
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Kim, J., Olson, K. & Butani, L. Sevelamer crystals in the mucosa of the gastrointestinal tract in a teenager with end-stage renal disease. Pediatr Nephrol 31, 339–341 (2016). https://doi.org/10.1007/s00467-015-3269-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-015-3269-1