Abstract
Background
We previously showed worse outcomes among lower socioeconomic status (SES) groups following metabolic/bariatric surgery (MBS). In light of healthcare changes in response to COVID-19, this study aims to evaluate post-pandemic MBS outcomes and determine if prior socioeconomic disparities persisted in the post-COVID era.
Methods
A retrospective chart review of patients undergoing primary Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG) between 2015 and 2022 was performed. Patients were stratified into pre- and post-COVID groups. Post-COVID cohort was further stratified into high (HT) and low (LT) tier status based on Distressed Communities Index, a geocoded composite measure of SES. Preoperative characteristics and postoperative outcomes were compared between pre- and post-COVID cohorts, as well as between post-COVID HT and LT groups.
Results
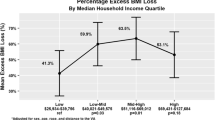
Of 709 patients, 82.9% were pre-COVID and 17.1% were post-COVID. Post-COVID cohort had greater rate of public insurance (46% vs. 37%, p < 0.001), longer wait time to surgery (mean 358 ± 609.8 days vs 241.9 ± 368.5 days, p = 0.045), and were more likely to undergo RYGB (69% vs. 56%, p = 0.010). Post-COVID patients also had lower risk of any complications on multivariable analysis (OR 0.599, 95% CI 0.372–0.963), had higher follow-up rates at post-discharge (95.8% vs 79.7%, p < 0.005), 6-month (93% vs. 82%, p < 0.001) and 12-month visits (75% vs. 63%, p = 0.005), and lost more weight at 12 months (67% excess weight loss (%EWL) vs. 58%EWL, p = 0.002). Among post-COVID HT and LT cohorts, previously seen disparities in complications were no longer seen. Finally, there were no differences in weight or follow-up rates between post-COVID HT and LT.
Conclusions
Post-COVID changes to MBS care have resulted in improved short-term outcomes and reduced disparities for patients of lower SES. Further studies are needed to identify these positive factors to perpetuate practice patterns that optimize care for patients of all socioeconomic status.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
The coronavirus disease of 2019 (COVID-19) led to drastic changes in healthcare access and delivery. The infectious disease burden necessitated the reallocation of resources including staff, equipment, and even physical spaces to accommodate the influx of patients [1]. As little was known about the transmission of the virus in the early stages of the pandemic, elective surgeries were often suspended or regulated according to medical necessity [1, 2]. This led to a notable decrease in operations, with a nadir of 27% fewer procedures performed from 2019 to 2020 [3]. Similarly, performance of metabolic/bariatric surgeries (MBS) dropped by 12.1% [4,5,6]. What is more, post-pandemic patient and procedure type shifted, favoring more sleeve gastrectomy and younger patients [4, 5].
One major factor affecting access to and outcomes following MBS is socioeconomic status (SES) [7,8,9,10]. SES can be difficult to calculate as it is multifactorial and requires information beyond the medical record. Distressed Communities Index (DCI) is a geocoded composite score that provides a more comprehensive measure of SES [11]. DCI measures community economic well-being by accounting for the following: community education rates, poverty rates, income, housing status, employment status, rate of change in employment, and business growth. Several studies have used DCI for surgical risk stratification and to predict surgical outcomes [12,13,14]. Our group previously used DCI to evaluate differences in outcomes between high and low resource communities following MBS, revealing worse 30-day complication rates and increased prevalence of weight recurrence among patients from distressed communities compared to their more prosperous counterparts [15, 16].
Few studies have specifically reported on the outcomes in patients undergoing MBS in the post-COVID era, and none have evaluated the effect of SES. Thus, given the change in the healthcare landscape and the known discrepancies seen among our patients, we aimed to evaluate post-pandemic MBS outcomes and determine if these disparities between high and low resourced communities persisted in the post-pandemic era.
Methods
A retrospective cohort analysis of all patients ≥ 18 years undergoing primary laparoscopic Roux-en-Y gastric bypass (RYGB) or sleeve gastrectomy (SG) between 2015 and 2022 was performed at a single academic institution following approval by the intuitional review board. Clinical data were extracted from the electronic medical record (EMR): demographics, preoperative characteristics, wait time to surgery from initial consultation, 30-day complication rates, weight, and postoperative follow-up rates. Telehealth visits utilized self-reported weights. Patients undergoing surgery before March 1, 2020 were placed into the pre-pandemic cohort, while those with surgery dates after March 1, 2020 were placed into the post-pandemic cohort.
Distressed communities index
DCI defines community borders by zip code and assigns each community a score from 0 (no distress) to 100 (severe distress). Communities are then ranked into 5 categories: distressed, at risk, mid-tier, comfortable, and prosperous [11]. Zip codes were obtained from the EMR to score and categorize each patient into their respective DCI category. Patients were then stratified into high tier DCI status (HT), which includes mid-tier, comfortable and prosperous communities, and low tier DCI status (LT) which includes at-risk and distressed communities.
Weight calculations
Preoperative weight was reported as the body mass index (BMI) on the date of surgery. Postoperative weight loss was reported in standardized measure of percent excess weight loss (%EWL) and percent total weight loss (%TWL) [17]. Excess weight was calculated as the difference between initial weight and ideal body weight, with ideal body weight calculated based on a BMI of 25 kg/m2. Weight loss was recorded at 6- and 12-month postoperative time points.
Follow-up visits
In addition to the standard 6-month and 12-month postoperative follow-up rates, we reported short-term (30-day) follow-up rates for all of our patients. All patients at our institution are scheduled for a post-discharge telephone visit 2–3 days following discharge and an in-person 2-week postoperative visit. Six- and 12-month visits were in person or via telemedicine based on patient availability and preference.
Statistics
Statistical analysis was done using R Studio Software, version 4.1.2 (R Studio Team, 2020, PBC, Boston, MA). Student’s t test was used to compare continuous variables and Chi-squared analyses were used to compare categorical variables between HT and LT groups. Multivariable linear regressions were performed for continuous dependent variables, while multivariable binary regressions were performed for nominal dependent variables. Both types of analyses controlled for age, sex, race, type of surgery, preoperative BMI, American Society of Anesthesiologists (ASA) status, and type of insurance.
Results
Of 709 patients undergoing primary MBS, 588 (82.9%) underwent surgery prior to March 1, 2020, and 121(17.1%) underwent surgery after the start of the COVID-19 pandemic. Demographic data are summarized in Table 1. Overall, mean age was 48.6 ± 12.2 years and 76.0% were women. There were no differences between pre- and post-COVID groups in age, sex, race, or ethnicity. Post-COVID patients were more likely to have public insurance (46.3% vs 36.6% pre-COVID patients, p < 0.001), with higher proportions of Medicaid and military health insurance. DCI breakdown and percentage of HT vs LT patients were similar between pre- and post-COVID groups.
Table 2 shows the demographic data of the post-COVID groups. Mean age was 48.2 ± 12.7 years and 74.4% of patients were female. When stratified by DCI tier, 72.7% (88) were HT and 24.8% (30) were LT. Three patients had unknown DCI status. HT and LT groups were similar in age, sex, race, and ethnicity. Post-COVID LT patients had a higher rate of public insurance than post-COVID HT (66.7% LT vs 36.4% HT, p < 0.001) counterparts.
Post-COVID patients had significantly longer wait time from initial consultation to surgery date than pre-COVID patients (358 ± 610 days post-COVID vs 242 ± 369 days pre-COVID, p = 0.045). This was true even when controlling for age, gender, race, ethnicity, insurance type, BMI, ASA, and type of surgery (pre- vs post-COVID coefficient 110.053, p = 0.012). Post-COVID patients also had slightly lower preop BMI at time of surgery (42.8 ± 6.2 kg/m2 post-COVID vs. 44.3 ± 7.4 kg/m2 pre-COVID, p < 0.023), which while statistically significant was not clinically significant. Both groups had similar preoperative weight loss and ASA status. Finally, the post-COVID group had higher rates of RYGB than pre-COVID cohort (69.4% RYGB post-COVID vs. 56.3% pre-COVID, p = 0.010) (Table 3).
Among post-COVID patients, HT and LT patients had similar preoperative characteristics including preoperative BMI, wait time to surgery from initial consultation, and ASA profiles (Table 4). LT patients trended toward greater rates of RYGB (83.3% LT vs. 64.8% HT), although this was not statistically significant with p = 0.094.
Post-COVID patients trended toward shorter hospital length of stay (LOS) (1.7 ± 1.0 days post-COVID vs 1.9 ± 1.4 days pre-COVID, p = 0.076) but had similar rates of patients discharged by postoperative day 1 (POD1) (48.8% post-COVID vs 42.7% pre-COVID, p = 0.260). While most 30-day complication rates were similar between groups, univariate analysis showed significantly lower wound complication rates in the post-COVID cohort (0.8% post-COVID vs 5.4% pre-COVID, p < 0.001) (Table 5). However, when controlling for preoperative characteristics, this difference was no longer seen. Instead, multivariable binary logistic regression showed that post-COVID patients were half as likely to experience any complication, with an odds ratio of 0.599 [95% CI 0.372–0.963] (Table 6).
Post-COVID patients also had statistically higher rates of follow-up, particularly at the post-discharge telephone (95.8% vs 79.7%, p < 0.001), 6-month postop (92.6% vs 81.6%, p < 0.001), and 12-month postop (75.2% vs 62.8%, p < 0.005) visits (Table 5). There was no difference in the 2-week follow-up visit rates, with both groups having over 99% attendance. Post-COVID patients also had greater weight loss at both 6-month (53.6 ± 17.0%EWL vs. 48.3 ± 17.0%EWL, p = 0.004) and 12-month (66.7 ± 22.5%EWL vs. 58.1 ± 23.0%EWL, p = 0.002) postop. On multivariable linear regression, again controlling for factors including preoperative BMI, and type of surgery, differences in %EWL and %TWL were only statistically significant at the 12-month time point (Table 7).
Table 8 compares postoperative outcomes among post-COVID patients stratified by HT and LT DCI groups. There were no differences in LOS (1.8 ± 0.95 days), and while there was a greater percentage of LT patients discharged on POD 1 (45.5% HT vs 63.3% LT), this was not statistically significant (p = 0.139). There were no differences in 30-day complication rates and follow-up rates were similar across all times points. Finally, there were no differences in weight loss between groups at 6 months (54.5 ± 17.9%EWL HT vs 50.6 ± 15.2%EWL LT, p = 0.313) and 12 months (65.6 ± 23.0%EWL HT vs 69.5 ± 21.4%EWL LT, p = 0.473) postoperatively.
Discussion
COVID-19 has left its mark on healthcare systems world-wide. In addition to changes in MBS access and delivery, postoperative care protocols and telehealth have transformed the field [2, 18]. The burden of obesity makes bariatric patients particularly vulnerable—SES exacerbates this vulnerability [10, 19, 20]. Thus, in the face of major healthcare changes, our study characterizes outcomes in the post-COVID era with attention to disparities between SES groups.
One of the most notable adverse impacts of the pandemic is the reduction in the number of MBS procedures performed. This has led to delays in the care for patients with obesity [6, 21, 22]. Our study population is no exception; post-COVID status was an independent predictor for increased wait time to surgery, with average wait time 4 months longer than pre-COVID counterparts. Again, this is likely a reflection of prioritization of urgent procedures and limits of hospital capacity. Even with this limitation, our study is unique as we saw no differences in age or ASA status between groups [4, 5]. This suggests that despite delays, obesity management of sicker and older patients was not compromised.
This study did identify two notable preoperative differences between pre- and post-COVID groups. First, there was an increase in the prevalence of public insurance, rising from 36.6% pre-COVID to 46.3% post-COVID. This may be attributable to the expansion of Medicaid and laxity of eligibility criteria in response to the COVID-19 [23, 24]. Second, we saw an increase in prevalence of RYGB performed, from 56 to 69%. This is consistent with trends seen in the MBSAQIP registry; while overall prevalence of SG increased from 2019 to 2020, subgroup analyses found a 11% increase in the rate of RYGB among adults ≥ 19 years [4, 5]. This suggests that the post-COVID environment allowed for greater patient catchment without compromising operative technique.
Consistent with prior studies, there was no difference in LOS and complication rates were mostly similar between pre- and post-COVID groups [4, 6, 25]. The one exception was rate of any complication; multivariable analyses showed that post-COVID patients were half as likely to have any complication compared to the pre-COVID cohort, suggesting a protective effect of hospital protocols and practice patterns since the pandemic began. This may be due in part to increased accessibility to the health care team through telehealth, though the effect new policies aimed at infection prevention and earlier discharge are unknown. Further studies are required to determine additional factors allowing for the improvement of complication metrics.
Perhaps one of the most positive and pervasive changes incurred by the pandemic is the standardization of telehealth. While pre-pandemic studies demonstrated the safety and efficacy of telehealth for postoperative care, the demands of the pandemic catalyzed its widespread adoption [26, 27]. The impact of this is most apparent in our follow-up rates. Prior to the pandemic, 2-week postop visit had over 99% attendance rate, primarily due to required in-person wound evaluation. Visits with telehealth options, however, had less than 80% attendance. For example, although a post-discharge telephone visit has been a part of our practice since 2014, attendance prior to the pandemic was only 80%. Post-COVID attendance improved to 96%. This is likely due to new protocols enforcing remote visits (to satisfy isolation requirements), improvements in telehealth platform usability, and new billing codes facilitating visit compensation. Similar improvements in follow-up were seen at 6 and 12 months, likely due to telehealth accessibility and insurance coverage. Gould et al. showed insurance coverage to be a major barrier of long-term follow-up [28]. As aforementioned, Medicaid coverage was expanded and was less likely to be revoked, thus increasing the pool of insured patients. Given the rates of public insurance in our post-COVID cohort, future studies are needed to see whether these high rates of follow-up persist as Medicaid returns to its baseline coverage patterns.
Interestingly, while other studies predominantly report similar pre- and post-COVID weight loss following MBS, we saw greater 12-month weight loss in the post-COVID group [29, 30]. This was true even after controlling for surgery type, important to our population as RYGB is associated with greater weight loss [31,32,33]. Prior studies have suggested improved weight loss with increased follow-up rates, but this finding is not definitive [28, 34, 35]. Weight loss is multifactorial, making it difficult to pinpoint an exact cause for this difference. Thus, further studies are needed to identify these factors so that practice patterns promoting increased weight loss can be maintained.
Like our previously reported pre-COVID cohort, post-COVID LT and HT patients were similar in preoperative characteristics [15]. Unsurprisingly, post-COVID LT patients had 30% greater rates of public insurance compared to post-COVID HT and 15% greater rates of public insurance compared to pre-COVID LT groups. This is, again, attributable to the insurance expansion discussed above which is more likely to impact lower SES patients. Although post-COVID patients as a whole had longer wait time to surgery, there was no difference in wait time between LT and HT subgroups.
Importantly, prior to the pandemic, LT patients were half as likely to be discharged home on POD 1, 50% more likely to have any complication, and over twice as likely to be readmitted after discharge [15]. In the post-COVID era, these differences were no longer seen. This suggests that post-COVID protocols have evened the playing field for patients of lower SES, even with the added burden of the global pandemic. Furthermore, these findings reiterate the fact that despite the disparities in resources, LT patients benefit just as much from MBS as patients from more prosperous communities.
Limitations
This study has several limitations, including its retrospective nature. What is more, implementation of telehealth follow-up visits necessitates self-reported weights. This is often measured on a home scale and cannot be independently verified. Nonetheless, studies have shown close fidelity of self-reported weights to clinic measured weights, making self-reported weight a viable proxy [36, 37]. This study is also limited in its single institution setting. While all protocols have a common framework, each hospital has its own policies and a single institutional study may mask the effect of differing practice patterns. Larger, multi-institutional studies should be conducted to confirm our results. Likewise, while patients are stratified to pre- and post-pandemic cohorts, the precautions and limitations imposed early in the pandemic have largely changed with time and abatement of the virus. Therefore, early post-COVID era may be different from late post-COVID era, with subsequent impact on patient care. Thus, as we transition away from the immediate post-pandemic era amidst continued healthcare evolution, future studies are needed to identify disparities and determine MBS protocols that optimize outcomes for patients of all SES.
Conclusion
To our knowledge, this is the first study evaluating both post-pandemic outcomes and the changes in socioeconomic disparities in patients undergoing bariatric surgery. Health care changes in the wake of the pandemic have resulted in fewer complications and improved weight loss and follow-up. Most importantly, disparities seen among low tier patients prior to the pandemic were no longer seen in the post-COVID era. Thus, post-pandemic changes have had a protective effect on our patient population, especially among socioeconomically disadvantaged patients. This highlights the power of positive MBS protocol changes and the ability to create an even playing field for patients of all SES groups.
References
Rubino F, Cohen RV, Mingrone G, le Roux CW, Mechanick JI, Arterburn DE, Vidal J, Alberti G, Amiel SA, Batterham RL, Bornstein S, Chamseddine G, Del Prato S, Dixon JB, Eckel RH, Hopkins D, McGowan BM, Pan A, Patel A, Pattou F, Schauer PR, Zimmet PZ, Cummings DE (2020) Bariatric and metabolic surgery during and after the COVID-19 pandemic: DSS recommendations for management of surgical candidates and postoperative patients and prioritisation of access to surgery. Lancet Diabetes Endocrinol 8:640–648
Murtha JA, Alagoz E, Breuer CR, Eierman L, Jawara D, Farrar-Edwards D, Voils CI, Funk LM (2023) Impact of COVID-19 on the postoperative bariatric surgery patient experience. Ann Surg 277:e745–e751
Moss WD, Pires GR, Samlowski E, Webb J, DeAngelo MM, Eddington D, Brintz BJ, Agarwal J, Kwok AC (2022) Characterizing the volume of surgery and post-operative complications during the COVID-19 pandemic. Langenbecks Arch Surg 407:3727–3733
Verhoeff K, Mocanu V, Dang J, Wilson H, Switzer NJ, Birch DW, Karmali S (2022) Effect of the COVID-19 pandemic on bariatric surgery in North America: a retrospective analysis of 834,647 patients. Surg Obes Relat Dis 18:803–811
Messiah SE, Xie L, Mathew MS, Marroquin Marroquin E, Almandoz JP, Qureshi FG, Schneider BE, de la Cruz-Munoz N (2022) Impact of the COVID-19 pandemic on metabolic and bariatric surgery utilization and safety in the United States. Obes Surg 32:2289–2298
McGlone ER, Carey IM, Currie A, Mahawar K, Welbourn R, Ahmed AR, Pring C, Small PK, Khan OA (2023) Bariatric surgery provision in response to the COVID-19 pandemic: retrospective cohort study of a national registry. Surg Obes Relat Dis 19:1281–1287
Carden A, Blum K, Arbaugh CJ, Trickey A, Eisenberg D (2019) Low socioeconomic status is associated with lower weight-loss outcomes 10-years after Roux-en-Y gastric bypass. Surg Endosc 33:454–459
Stenberg E, Naslund I, Persson C, Szabo E, Sundbom M, Ottosson J, Naslund E (2020) The association between socioeconomic factors and weight loss 5 years after gastric bypass surgery. Int J Obes (Lond) 44:2279–2290
Martin M, Beekley A, Kjorstad R, Sebesta J (2010) Socioeconomic disparities in eligibility and access to bariatric surgery: a national population-based analysis. Surg Obes Relat Dis 6:8–15
Hruby A, Hu FB (2015) The epidemiology of obesity: a big picture. Pharmacoeconomics 33:673–689
Economic Innovation Group (2023) Distressed communities. https://eig.org/distressed-communities/. Accessed 12 Mar 2023
Mehaffey JH, Hawkins RB, Charles EJ, Turrentine FE, Hallowell PT, Friel C, Jones RS, Tracci MC (2020) Socioeconomic “Distressed communities index” improves surgical risk-adjustment. Ann Surg 271:470–474
Charles EJ, Mehaffey JH, Hawkins RB, Fonner CE, Yarboro LT, Quader MA, Kiser AC, Rich JB, Speir AM, Kron IL, Tracci MC, Ailawadi G, Investigators for the Virginia Cardiac Services Quality I (2019) Socioeconomic distressed communities index predicts risk-adjusted mortality after cardiac surgery. Ann Thorac Surg 107:1706–1712
Hawkins RB, Charles EJ, Mehaffey JH, Williams CA, Robinson WP, Upchurch GR, Kern JA, Tracci MC, Virginias Vascular G (2019) Socioeconomic distressed communities index associated with worse limb-related outcomes after infrainguinal bypass. J Vasc Surg 70:786-794 e782
Johns AJ, Soufi K, DeJesus-Gaeta E, Smith W, Ali MR, Ahmed SM (2022) Distressed communities associated with worse long-term follow-up after bariatric surgery. J Am Coll Surg 235:S19
Johns AJ, Luce MS, Kaneski MJ, Lowery RA, Jachniewicz B, Salas A, McCreary R, Russell RM, Lyo V, Ali MR, Ahmed SM (2023) The long weight: association between distressed communities index and long-term weight outcomes following bariatric surgery. Surg Endosc 37:7218–7225
Brethauer SA, Kim J, el Chaar M, Papasavas P, Eisenberg D, Rogers A, Ballem N, Kligman M, Kothari S, Committee ACI (2015) Standardized outcomes reporting in metabolic and bariatric surgery. Surg Obes Relat Dis 11:489–506
Irarrazaval MJ, Inzunza M, Munoz R, Quezada N, Branes A, Gabrielli M, Soto P, Dib M, Urrejola G, Varas J, Valderrama S, Crovari F, Achurra P (2021) Telemedicine for postoperative follow-up, virtual surgical clinics during COVID-19 pandemic. Surg Endosc 35:6300–6306
Abdelaal M, le Roux CW, Docherty NG (2017) Morbidity and mortality associated with obesity. Ann Transl Med 5:161
Anekwe CV, Jarrell AR, Townsend MJ, Gaudier GI, Hiserodt JM, Stanford FC (2020) Socioeconomics of obesity. Curr Obes Rep 9:272–279
Gualtieri P, Marchetti M, Renzo LD, De Santis GL, Palma R, Colica C, Frank G, De Lorenzo A, Di Lorenzo N (2022) Impact of COVID-19 on the destiny of bariatric patients. Nutrients 15:163
Ahmed B, Altarawni M, Ellison J, Alkhaffaf BH (2021) Serious impacts of postponing bariatric surgery as a result of the COVID-19 pandemic: the patient perspective. J Patient Exp 8:23743735211008280
Benitez J (2022) Comparison of unemployment-related health insurance coverage changes in medicaid expansion vs nonexpansion states during the COVID-19 pandemic. JAMA Health Forum 3:e221632
Jacobs PD, Moriya AS (2023) Changes in health coverage during the COVID-19 pandemic. Health Aff (Millwood) 42:721–726
Singhal R, Tahrani AA, Ludwig C, Mahawar K, collaborators G (2021) Global 30-day outcomes after bariatric surgery during the COVID-19 pandemic (GENEVA): an international cohort study. Lancet Diabetes Endocrinol 9:7–9
Nikolian VC, Williams AM, Jacobs BN, Kemp MT, Wilson JK, Mulholland MW, Alam HB (2018) Pilot study to evaluate the safety, feasibility, and financial implications of a postoperative telemedicine program. Ann Surg 268:700–707
Smith WR, Atala AJ, Terlecki RP, Kelly EE, Matthews CA (2020) Implementation guide for rapid integration of an outpatient telemedicine program during the COVID-19 pandemic. J Am Coll Surg 231:216–222 e212
Gould JC, Beverstein G, Reinhardt S, Garren MJ (2007) Impact of routine and long-term follow-up on weight loss after laparoscopic gastric bypass. Surg Obes Relat Dis 3:627–630 (discussion 630)
Huang EY, Grunvald E, Blitzer RR, Lee AM, Broderick RC, Li JZ, Cheverie JN, Sandler BJ, Horgan S, Jacobsen GR (2023) Despite regression of healthy lifestyle habits, weight loss after bariatric surgery is not affected during the COVID-19 pandemic. Surg Endosc 37:607–612
Pereira X, Romero-Velez G, Skendelas JP, Rodriguez-Quintero JH, Grosser R, Lima DL, Moran-Atkin E, Choi J, Camacho D (2021) The COVID-19 pandemic did not affect target weight loss 1 year post bariatric surgery. Obes Surg 31:4926–4932
Gomes-Rocha SR, Costa-Pinho AM, Pais-Neto CC, de Araujo PA, Nogueiro JPM, Carneiro SPR, Santos-Sousa H, Lima-da-Costa EJ, Bouca-Machado R, Preto JR, Group C-O (2022) Roux-en-Y gastric bypass vs sleeve gastrectomy in super obesity: a systematic review and meta-analysis. Obes Surg 32:170–185
Shoar S, Saber AA (2017) Long-term and midterm outcomes of laparoscopic sleeve gastrectomy versus Roux-en-Y gastric bypass: a systematic review and meta-analysis of comparative studies. Surg Obes Relat Dis 13:170–180
Ju Z, Anderson W, Istfan N, Carmine B, Carter C, Pernar L, Marshall A, Hess DT (2022) Comparison of weight loss outcomes between Roux-en-Y gastric bypass and sleeve gastrectomy in a racially mixed urban patient population. Surg Obes Relat Dis 18:1218–1227
Reiber BMM, Leemeyer AR, Bremer MJM, de Brauw M, Bruin SC (2021) Weight loss results and compliance with follow-up after bariatric surgery. Obes Surg 31:3606–3614
Kim HJ, Madan A, Fenton-Lee D (2014) Does patient compliance with follow-up influence weight loss after gastric bypass surgery? a systematic review and meta-analysis. Obes Surg 24:647–651
Christian NJ, King WC, Yanovski SZ, Courcoulas AP, Belle SH (2013) Validity of self-reported weights following bariatric surgery. JAMA 310:2454–2456
Jenkins TM, Boyce TW, Ralph Buncher C, Zeller MH, Courcoulas AP, Evans M, Inge TH (2017) Accuracy of self-reported weight among adolescent and young adults following bariatric surgery. Obes Surg 27:1529–1532
Acknowledgements
There are no acknowledgments to make outside of the listed authors.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Alexandra Johns, Leah Timbang, Dr. Annie Wang, and Ms. Navneet Kaur Singh have no conflicts of interest or financial ties to disclose. Drs. Shushmita Ahmed and Victoria Lyo had travel expenses to educational conferences paid for by Intuitive Surgical. Dr. Shushmita Ahmed is the California STAR Representative for ASMBS for CA/NV Chapter of ASMBS. Dr. Victoria Lyo received funding for separate research from the National institute of Health, Building Interdisciplinary Research Careers in Women’s Health at UC Davis through Grant Number: 5K12HD051958 and is a member of the American Society for Metabolic & Bariatric Surgery (ASMBS) Research Committee and Board Member of the CA/NV Chapter of the ASMBS. Dr. Mohamed Ali received funding for other research from the ASMBS Foundation, has received consulting fees from Stryker and Olympus, received travel support from Stryker, is on the DSMB for a University of Michigan NIH study, and is co-chair of the ASMBS Emerging Technology Committee, ASMBS liaison to the Fellowship Council Curriculum Committee, and is a member of the American Board of Surgery Bariatric FPD Exam Writing Group.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ahmed, S.M., Johns, A., Timbang, L. et al. Effect of COVID-19 changes on outcomes and socioeconomic disparities following metabolic and bariatric surgery. Surg Endosc (2024). https://doi.org/10.1007/s00464-024-11212-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00464-024-11212-z