Abstract
Introduction
The growth of surgeon burnout is of significant concern. As we work to reimagine the practice of surgery, an accurate understanding of the extent of surgeon burnout is essential. Our goal was to define the current prevalence of burnout and quality of life (QOL) among SAGES surgeons.
Methodology
An electronic survey was administered to SAGES members to establish a current baseline for QOL, burnout, depression, and career satisfaction. To assess outcomes, we utilized the validated Maslach Burnout Inventory for Medical Personnel, the Medical Outcomes Study Short Form, and the Primary Care Evaluation of Mental Disorders. All scoring followed validated norm-based methods.
Results
Of 4194 active members, 604 responded (14.40%). 69% met burnout threshold, with high levels of emotional exhaustion and depersonalization, and low personal accomplishment. 81% reported “being at the end of their rope”, 74% felt emotionally drained, and 65% felt used up daily. Nearly all maintained caring about what happened to their patients (96%), easily understanding how their patients feel (84.3%) and being capable of dealing effectively with their patient’s problems (87.6%). However, respondents never, rarely, or occasionally felt energetic (77.5%) or experienced a sense of professional accomplishment (57.8%). The overall QOL score was 69/100, with lower Mental than Physical scores (62.69 (SD 10.20) vs.77.27 (SD 22.24)). More than half of respondents met depression criteria. While 77% supported they would become a physician again, less than half would choose surgery again or recommend surgery to their children. Furthermore, less than a third felt work allowed sufficient time for their personal lives.
Conclusions
Participating SAGES surgeons reported alarmingly high rates of burnout and depression. Despite experiencing emotional exhaustion and depersonalization, they maintained a strong commitment to patient care. These findings likely reflect the broader state of surgeons, underscoring the urgent need for action to address this critical issue.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Burnout is an occupational phenomenon resulting from chronic and mounting workplace stress and anxiety. The syndrome is characterized by three broad dimensions: feelings of energy depletion or exhaustion; increased mental distance from and individual’s work, often expressed as feelings of negativism or cynicism related to one’s job; and reduced professional efficacy. Healthcare workers are at particular risk for burnout, and the rate of burnout among surgeons specifically is much greater than the general population [1]. Burnout has profound effects on both the personal and professional lives of affected surgeons, as well as the quality of care provided to patients. Specifically, physicians with burnout demonstrate a greater likelihood of committing a major medical error, being involved in a malpractice suit, and having lower patient satisfaction ratings [2,3,4]. Surgeons experiencing burnout are more likely to ruminate on their mistakes, to assign a disproportionate amount of self-blame, and to be unable to reflect and recover professionally from bad outcomes [5]. As a result, burnout is often complicated by disruptive behaviors and poor clinical outcomes, and surgeons experiencing burnout are more likely than their peers to reduce their work hours, exit their profession, and turn to drugs, alcohol, or suicide as coping mechanisms. As such, burnout is a threat to the entire healthcare system and should become a public health priority.
A landmark 2009 study on burnout in surgeons revealed 40% of the nearly 8000 respondents had high emotional exhaustion, depersonalization, and generally met criteria for burnout [6]. In addition, 30% screened positively for symptoms of depression. Since this important benchmark, there has been increased awareness of burnout in surgery and surgical training. Financial and productivity pressures continue to mount, and surgeons are required to comply with increasing administrative burdens. These conditions collectively have fostered an environment that diminishes the joy in the practice of surgery, and expands the prevalence of burnout and its sequelae [7, 8]. Without changes, it is estimated that by 2025 there will be a nationwide physician shortage, with many driven away from the profession due to the effects of burnout [9]. However, these forecasts are based primarily on extrapolations from the incidence rates and relevant factors documented in the aforementioned 2009 study (6). An updated assessment of the current incidence and factors associated with burnout is warranted to develop the most effective action plan to address the problem.
Only by identifying the problem and its sources can we successfully seek to facilitate a transition from burnout to joy in our profession. The goal of this study was to estimate the incidence of burnout and assess the quality of life among gastrointestinal and endoscopic surgeons. The hypothesis is that despite increased awareness, burnout remains prevalent among surgeons.
Methods
Study design
An observational cross-sectional study design was used. The methodology was modeled after the 2009 Shanafelt et al. survey of American College of Surgeons members [6].
Study population
Active members of the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) (n = 4194) were electronically sent a survey link with a message stating the purpose of the survey was to better understand the factors that contribute to career satisfaction among surgeons. Participants were blinded to any other specific hypothesis of the study. The survey included 39 questions about demographic information, practice characteristics, quality of life, symptoms of depression, and career satisfaction. The survey was accessible for 4 weeks (September 2022), then opened again for 6 days during the SAGES Annual Conference (March 2022). Three e-mail messages were sent during the September period reminding surgeons to complete the survey.
All SAGES members that have completed training and were currently in practice were included. Active candidate and associate members including surgical residents, fellows, and other associates were included. Those that retired or were in non-clinical practice were excluded. All practice locations and practice types were included.
Several validated tools were used to gather information on burnout, mental and physical quality of life (QOL), and symptoms of depression The Maslach Burnout Inventory for Medical Personnel (MBI-HSS) was used to identify burnout. The MBI-HSS is a validated 22-item questionnaire with 3 subscales: emotional exhaustion (EE) (9 items), depersonalization (DP) (5 items), and professional accomplishment (PA) (8 items), each with a 7-point Likert-type, frequency response scale (0 = never, 1 = a few times a year or less, 2 = once a month or less, 3 = a few times a month, 4 = once a week, 5 = a few times a week, 6 = every day) [1, 2]. Each scale measures its own dimension of burnout. The same cut score was used to define burnout as in the Shanafelt et al. study, where surgeons with a high score on either the depersonalization and/or emotional exhaustion subscales were considered to professional burnout [6]. Higher scores on the EE and DP subscales indicate a higher burnout symptom burden; lower scores on the PA subscale indicate a higher burnout symptom burden. Symptoms of depression were screened using the 2-item Primary Care Evaluation of Mental Disorders (PRIME-MD), a standardized depression screening tool validated to perform as well as longer instruments. Mental and physical QOL were measured using the Medical Outcomes Study Short Form (SF-36) with norm-based scoring methods used to calculate overall, mental and physical component summary scores, and scores for the eight domains. Higher scores indicate better health status, and a mean score of 50 has been articulated as a normative value for all scales [10]. Additional questions developed and validated in the original survey to explore demographic factors, professional characteristics and career satisfaction were also included (Appendix).
The main outcomes were to: (1) measure burnout and QOL among SAGES member surgeons; (2) examine the relationship between specific personal and practice characteristics and burnout among SAGES surgeons; (3) compare outcomes to the 2009 Shanafelt landmark study.
Descriptive summary statistics were performed for the incidence of burnout, positive depression screen, and mental and physical QOL among surgeons. Our analytic approach was informed by the PROMIS scientific standards for instrument development and validation. The survey followed the EQUATOR network methodology for Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES).
Results
During the study period, a total of 615 surveys were initiated by SAGES members. 609 were completed across all scales; 5 were excluded as respondents were retired or in non-clinical practice, leaving 604 included in the analysis (response rate 14.40%). The majority of respondents were practicing surgeons (91.88%, n = 555), with less than 10% in residency or fellowship training (8.11%, n = 49). 85.93% (n = 519) practiced in the US, 5.13% (n = 31) practiced in Canada, and 8.94% (n = 54) practiced internationally: 13 each in South America and Europe, 14 in Asia, and 6 each in the United Kingdom and Middle East/Africa.
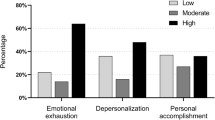
By scale, the MBI-HSS showed overall burnout in 69% of respondents, and high levels of burnout in each of the three inventory categories (Table 1). 65% reported feeling burned out from their work (EE5), 81% reported being at the end of their rope (EE9), 74% felt emotionally drained from their work (EE1), 65% reported feeling used up at the end of each work day (EE2), 62% felt fatigued when they get up in the morning and have to face another day on the job (EE3), 60% felt frustrated by their job, and 59% reported they are working too hard (EE8) often, usually, or every day. Respondents did not endorse interacting with people all day as really a strain (EE4, 17%) or that working with people directly puts too much stress on them (EE7, 10%) often, usually, or every day (Fig. 1a). Respondents did not report high symptoms of depersonalization, and had lower scores on the DP scale (Fig. 1b). For the PA scale, respondents reported low personal accomplishment, with low scores in 5 of the 8 items. More than half of respondents recording never, rarely, or occasionally do I feel very energetic (PA4); I feel exhilarated after working closely with my patients (PA6); and I have accomplished many worthwhile things in my job (PA7). Respondents maintained, “I can easily create a relaxed atmosphere with my patients (PA5)”, “I can easily understand how my patients feel about things (PA1)”, and “I deal very effectively with the problems of my patients (PA2)” (Fig. 1c).
From the SF-36, the overall QOL score was 69.13%. For the eight individual SF-36 domains, there was < 50% reported for Energy/Fatigue (47.96), and < 75% for every other domain except Physical Functioning (90.41%) and Pain (77.40%). By scale, the Mental results were substantially lower than the Physical results. Full details of the overall score, individual domains, and scales are in Table 1.
Based on the PRIME-MD, more than 50% of respondents met criteria for depression, citing little interest/pleasure in doing things (54.64%) and feeling down/hopeless/depressed (59.11%) for at least several days in the prior 2 weeks (Table 2).
The career satisfaction questions revealed that less than 1/3 (32.35%) of respondents reported that work left enough time for their personal lives. While nearly three-fourths (76.99%) responded that they would become a physician again, less than 50% would become a surgeon again (49.67%). Furthermore, less than 50% would recommend that their children pursue a career as a physician/surgeon (42.38%) (Fig. 2).
Discussion
Surgeon burnout is a serious issue in trainees and attending surgeons, because of its association with physician attrition, physician mental and physical health, and surgical outcomes. In this analysis of burnout among SAGES surgeons, burnout was highly prevalent at 69%, with high levels of emotional exhaustion and depersonalization, and a low sense of personal accomplishment. Respondents reported a low overall QOL, with the lowest scores in the Mental/ Emotional domains, and more than half met criteria for depression. Career satisfaction was low, with less than one-third reporting sufficient time for their personal lives and fewer than half reporting they would choose to become a surgeon again.
Surgeons are at increased risk for burnout as a result of long work hours, delayed gratification, challenges with work and home balance, and challenges associated with patient care [2, 11]. Female surgeons face additional challenges from gender-based discrimination (exclusion, questioning of expertise, role misidentification, salary disparities, and unequal resource allocation) and ancillary demands (related to appearance and self-advocacy) [12]. Even surgical trainees feel the impact. A 2018 representative survey found 38.5% of US surgical trainees reported weekly burnout symptoms and 4.5% reported suicidal thoughts during the prior year [13]. The landmark 2009 study on burnout in practicing surgeons from American College of Surgeons members found the reported rate of burnout was 40% [6]. In that study, from the MBI-HSS, 31.7% of respondents reported high rates of emotional exhaustion, 26% scored high in depersonalization, and 12.8% reported a low sense of personal accomplishment. 28% had a mental QOL score more than one-half a standard deviation below the population norm. Based on the PRIME-MD scale, 30% screened positive for depression. While over 70% of respondents in the Shanafelt study reported they would become a surgeon again, only 51% wanted their children to pursue a surgical career. Furthermore, 36% of surgeons in the Shanafelt study were concerned they did not have enough time for their home life. Using the same methodology, our rates for burnout, depression, career dissatisfaction, and QOL were much higher than documented in the Shanafelt lankmark study. Specifically, 69% of our respondents met criteria for burnout compared to their 40%, with corresponding rises in the levels of emotional exhaustion and depersonalization, and a drop in personal accomplishment. Our overall QOL score was 69/100, with substantially lower scores in the Mental than Physical scale (62.69 (SD 10.20) vs.77.27 (SD 22.24)). 54% had a Mental QOL score more than one-half a standard deviation below the population norm, compared to 28% in the Shanafelt work. From the PRIME-MD, more than half our respondents met screening criteria for depression, compared to 30% in the prior benchmark. Rates to become a physician again (77%), were comparable to the prior reports. However, substantially lower numbers of surgeons in the current study reported that their work allowed sufficient time for their personal lives, that they would become a surgeon again or recommend the career to their children than in the prior work. In the Shanafelt study, responders worked a median of 60 h/week, and were on call an average of 2 nights/week [6]. While not directly measured in the present study, surgeon time at work is likely greater than this, and now includes additional time for administrative tasks, electronic medical records, and effects of resident duty hours reductions, which directly correlate with burnout rates [14, 15].
One striking finding of the current work was that surgeons had poor perception of their individual state. Despite reporting they are working too hard and feeling frustrated, burnt out, and emotionally fatigued, surgeons reported they maintained the ability to empathize with patients, deal with their patients’ problems, and that they cared what happened to their patients. This may be from the resilience emphasized in surgical training or a lack of individual emotional awareness, or a combination of those factors. More granular analysis is needed to determine the sources of this discrepancy. This is in alignment with prior work, where a survey of 1150 US surgeons showed their subjective assessment of their well-being relative to colleagues was poor. The majority (89.2%) believed that their well-being was at or above average, despite the reality that 70.5% had scores in the bottom 30% relative to national norms [16]. What is clear and hopeful from the current work is that surgeons continue to value and care for their patients. The majority of surgeons report patient care is the most meaningful aspect of their work [17].
While the present study findings of the prevalence of burnout are higher than the prior benchmark study, they are aligned with broader contemporary reports on burnout within medicine as a field overall. The Medscape 2023 U.S. physician burnout and depression report showed 53% of physicians overall reported burnout and 23% reported depression, increases of 11% and 8%, respectively, compared to the 2018 report [18]. A recent cross-sectional survey of over 600 academic medical students, trainees, and surgeons found 1 in 7 respondents reported suicidal ideation in the past year, further affirming this epidemic among the surgical workforce in the US [19,20,21,22]. There is both greater awareness of the burnout epidemic in surgery, alongside further deterioration of surgeon wellness and career satisfaction. Importantly, these trends are reflected in the increasing rates of suicide and reports of suicidal ideation and loss of surgeons from practice [19, 20, 23]. Every year, attrition and reduced clinical activity from burnout costs the US healthcare system approximately $4.6 billion [24]. Awareness of the prevalence and impact of burnout is also documented in studies describing the struggles faced by trainees and practicing surgeons across all surgery service lines internationally [25,26,27,28,29,30].
Currently, it is well recognized that burnout is pervasive and the practice environment is the major issue [31]. Yet to date, there has been little effective change. The symptoms of burnout and professional distress remain dramatically more common in physicians than in workers in other fields, and ubiquitous in the surgical specialties [7, 18]. So what has been done to address the problem? In the last decade, health care organizations responded to the awareness of burnout by promoting a “culture of wellness” and messaging that encouraged physicians to focus on self-care and become more resilient. But they maintained an incongruence between their espoused values and actual behavior [32, 33]. This created further physician frustration that the burden of that change was focused mainly on the individual and failed to address the underlying practice environment, and widened the wedge between physicians and leaders in their practice environment [34]. A sweeping, top-down change, from a professional culture of perfectionism to a culture of excellence with self-compassion and growth mindset must be pursued for effective organizational change [34]. Roadmaps that consider individual, institutional, and cultural factors to facilitate these changes have been developed and published at society and organizational levels [35,36,37,38,39,40]. These frameworks can be used to construct surgery-specific strategies and multimodal models that create impact for all stakeholders. A commitment from surgical societies, professional organizations, physician leaders, and individual physicians to accelerating this shift from awareness to action will be critical for maintaining the workforce and attracting the next generation of surgeons [41].
The limitations of this work are recognized. The largest is the study design and relatively low response rate. With the response rate, a multivariate analysis could not be performed. We further acknowledge there could be a response bias affecting the reliability and validity of the results. We included SAGES members in the analysis, with the assumption that they were a representative population and only asked for general demographic data. But the survey was de-identified, so we cannot determine causative factors or connect responses across the demographics and individual scales for subgroup analysis. We attempted to mitigate these limitations using the CHERRIES checklist and targeting SAGES members across all relevant platforms for the widest distribution. There is also a lack of standard definition and clarity in the thresholds for defining burnout in surgery, which could affect our interpretation of the results. Burnout in this work and in the Shanafelt et al. work [6] were measured by assessing the frequency of symptoms in 2 domains, emotional exhaustion and depersonalization from the MBI. However, there are multiple scales, interpretations of the scales, and levels for defining burnout that can be used [42]. Even using the same tool, prevalence estimates of burnout can vary considerably, depending on the burnout definition selected [43, 44]. Further, surgeons may have a distinct threshold level compared to other physicians. The reality that we chose this rigorous lifestyle compared to other subspecialties, and have been conditioned to function within its constraints may impact specialty-specific considerations regarding appropriate thresholds for burnout, depression, and QOL. Despite these potential limitations, the themes delineated are operationally critical, as prior studies have shown that burnout symptoms are strongly associated with both thoughts of attrition and suicide, regardless of the threshold or definition selected [43].
Regardless of any limitations, this study is a valuable addition to the literature which may reset and specifically update the benchmark for burnout, depression, and quality of life in the practicing surgeon. There has been no meaningful improvement in self-reported symptoms of burnout, QOL, depression, and career satisfaction over time with increased awareness; to the contrary, all have deteriorated. These salient results provide impetus for research exploring and documenting effective strategies for mitigating burnout in the surgical disciplines.
In conclusion, participating SAGES surgeons revealed alarmingly high rates of burnout and depression. Despite experiencing emotional exhaustion and depersonalization, they maintained a strong commitment to patient care. These findings likely reflect the broad status of surgeons across our health system, underscoring the urgent need for action to address this critical issue. These results offer a reset and contemporary definition of the problem, and its prevalence. This updated baseline can help guide future work evaluating rates of burnout, depression, and career satisfaction across specific demographic and professional characteristics. The results can also be used to drive practice improvement at the institutional, national, and individual levels to help reimagine the practice of surgery.
References
Shanafelt TD, Sloan JA, Habermann TM (2003) The well-being of physicians. Am J Med 114:513–519
Shanafelt TD, Balch CM, Bechamps G et al (2010) Burnout and medical errors among American surgeons. Ann Surg 251:995–1000
Balch CM, Oreskovich MR, Dyrbye LN et al (2011) Personal consequences of malpractice lawsuits on American surgeons. J Am Coll Surg 213:657–667
Halbesleben JR, Rathert C (2008) Linking physician burnout and patient outcomes: exploring the dyadic relationship between physicians and patients. Health Care Manage Rev 33:29–39
Brenner MJ, Hickson GB, Boothman RC, Rushton CH, Bradford CR (2022) Honesty and transparency, indispensable to the clinical mission-part III: how leaders can prevent burnout, foster wellness and recovery, and instill resilience. Otolaryngol Clin N Am 55:83–103
Shanafelt TD, Balch CM, Bechamps GJ et al (2009) Burnout and career satisfaction among American surgeons. Ann Surg 250:463–471
Shanafelt TD, Hasan O, Dyrbye LN et al (2015) Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc 90:1600–1613
Sinsky C, Colligan L, Li L et al (2016) Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med 165:753–760
Poorman E (2019) Burnout among doctors is a public health crisis. WBUR. January 17, 2019. https://www.wbur.org/news/2019/01/17/harvard-study-doctor-burnout
Ware JE, Dewey JE (2002) How to score version 2 of the SF-36 Health Survey. Lincoln, RI: Quality Metric Incorporated
Gifford E, Galante J, Kaji AH et al (2014) Factors associated with general surgery residents’ desire to leave residency programs: a multi-institutional study. JAMA Surg 149:948–953
Finn CB, Syvyk S, Bakillah E et al (2023) Barriers and facilitators to clinical practice development in men and women surgeons. JAMA Surg 159:43
Hu YY, Ellis RJ, Hewitt DB et al (2019) Discrimination, abuse, harassment, and burnout in surgical residency training. N Engl J Med 381:1741–1752
Shanafelt TD, Dyrbye LN, Sinsky C et al (2016) Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc 91:836–848
Jamal MH, Rousseau MC, Hanna WC, Doi SA, Meterissian S, Snell L (2011) Effect of the ACGME duty hours restrictions on surgical residents and faculty: a systematic review. Acad Med 86:34–42
Shanafelt TD, Kaups KL, Nelson H et al (2014) An interactive individualized intervention to promote behavioral change to increase personal well-being in US surgeons. Ann Surg 259:82–88
Shanafelt TD, West CP, Sloan JA et al (2009) Career fit and burnout among academic faculty. Arch Intern Med 169:990–995
Kane L (2023) ‘I Cry but No One Cares’: physician burnout & depression report. Accessed Dec 2023. https://www.medscape.com/slideshow/2023-lifestyle-burnout-6016058?faf=1. Medscape
Chati R, Huet E, Grimberg L, Schwarz L, Tuech JJ, Bridoux V (2017) Factors associated With burnout among French digestive surgeons in training: results of a national survey on 328 residents and fellows. Am J Surg 213:754–762
Ebrahimpour A, Razi M, Mortazavi SJ et al (2023) Job satisfaction, career burnout, and work-related well-being prevalence among orthopedic surgeons: a nationwide study. Arch Bone Jt Surg 11:293–300
Olfson M, Cosgrove CM, Wall MM, Blanco C (2023) Suicide risks of health care workers in the US. JAMA 330:1161–1166
Drudi LM, Mitchell EL, Chandra V et al (2022) A gender-based analysis of predictors and sequelae of burnout among practicing American vascular surgeons. J Vasc Surg 75:1422–1430
Collins RA, Herman T, Snyder RA et al (2023) Unspoken truths: mental health among academic surgeons. Ann Surg 279:429–436
Han S, Shanafelt TD, Sinsky CA et al (2019) Estimating the attributable cost of physician burnout in the United States. Ann Intern Med 170:784–790
Yu JH, Roh HW, Song MR, Lee JH, Haam S, Kim M (2023) Factors in turnover intention of cardiothoracic surgery residents. Sci Rep 13:20243
Campbell DA, Sonnad SS, Eckhauser FE, Campbell KK, Greenfield LJ (2001) Burnout among American surgeons. Surgery 130:696–702
Golub JS, Weiss PS, Ramesh AK, Ossoff RH, Johns MM (2007) Burnout in residents of otolaryngology-head and neck surgery: a national inquiry into the health of residency training. Acad Med 82:596–601
Sharma A, Sharp DM, Walker LG, Monson JR (2008) Stress and burnout in colorectal and vascular surgical consultants working in the UK National Health Service. Psychooncology 17:570–576
Qureshi HA, Rawlani R, Mioton LM, Dumanian GA, Kim JYS, Rawlani V (2015) Burnout phenomenon in U.S. plastic surgeons: risk factors and impact on quality of life. Plast Reconstr Surg 135:619–626
O’Kelly F, Manecksha RP, Quinlan DM et al (2016) Rates of self-reported ‘burnout’ and causative factors amongst urologists in Ireland and the UK: a comparative cross-sectional study. BJU Int 117:363–372
Schonfeld IS, Bianchi R, Palazzi S (2018) What is the difference between depression and burnout? An ongoing debate. Riv Psichiatr 53:218–219
Shanafelt TD, Schein E, Minor LB, Trockel M, Schein P, Kirch D (2019) Healing the professional culture of medicine. Mayo Clin Proc 94:1556–1566
Egener B, McDonald W, Rosof B, Gullen D (2012) Perspective: organizational professionalism: relevant competencies and behaviors. Acad Med 87:668–674
Shanafelt TD (2021) Physician well-being 2.0: where are we and where are we going. Mayo Clin Proc 96:2682–2693
Golisch KB, Sanders JM, Rzhetsky A, Tatebe LC (2023) Addressing surgeon burnout through a multi-level approach: a national call to action. Curr Trauma Rep 9:28–39
West CP, Dyrbye LN, Erwin PJ, Shanafelt TD (2016) Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet 388:2272–2281
National Academies of Sciences, Engineering, and Medicine; National Academy of Medicine; Committee on Systems Approaches to Improve Patient Care by Supporting Clinician Well-Being (2019) Committee on systems approaches to improve patient care by supporting clinician well-being. In: Taking action against clinician burnout: a systems approach to professional well-being. National Academies Press, Washington, DC
Shanafelt T, Trockel M, Ripp J, Murphy ML, Sandborg C, Bohman B (2019) Building a program on well-being: key design considerations to meet the unique needs of each organization. Acad Med 94:156–161
DeChant PF, Acs A, Rhee KB et al (2019) Effect of organization-directed workplace interventions on physician burnout: a systematic review. Mayo Clin Proc Innov Qual Outcomes 3:384–408
American Medical Association (2022) AMA recovery plan for American’s physicians. American Medical Association. https://www.ama-assn.org/amaone/ama-recovery-plan-america-s-physicians. Accessed Dec 2023
Dres M, Copin MC, Cariou A et al (2023) Job strain, burnout, and suicidal ideation in tenured university hospital faculty staff in France in 2021. JAMA Netw Open 6:e233652
Sauder M, Zagales I, Zagales R et al (2022) Comprehensive assessment of burnout among surgical trainees and practicing surgeons: a systematic review. J Surg Educ 79:1188–1205
Hewitt DB, Ellis RJ, Hu YY et al (2020) Evaluating the association of multiple burnout definitions and thresholds with prevalence and outcomes. JAMA Surg 155:1043–1049
Hudson P, James K, Von Bargen E (2021) Professional burnout survey for practicing female pelvic medicine and reconstructive surgeons: a cross-sectional study. Female Pelvic Med Reconstr Surg 27:e326–e332
Acknowledgements
The authors acknowledge SAGES President Patricia Sylla, MD for critical review of the manuscript draft.
Funding
The authors received no funding or support for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The authors have no relevant conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Maslach Burnout Inventory Health Professionals
Select one choice below for each question (0–6).
Never- 0.
Rarely-1.
Occasionally-2.
About Half the Time-3.
Often- 4.
Usually- 5.
Everyday- 6.
Emotional exhaustion.
-
1.
I feel emotionally drained from my work.
-
2.
I feel used up at the end of each work day.
-
3.
I feel fatigued when I get up in the morning and have to face another day on the job.
-
6.
Interacting with people all day is really a strain for me.
-
8.
I feel burnt out from my work.
-
13.
I feel frustrated by my job.
-
16.
Working with people directly puts too much stress on me.
-
14.
I feel that I am working too hard on my job.
-
20.
I feel that I am at the end of my rope.
Depersonalisation.
-
5.
I feel that I treat some patients as if they were impersonal objects.
-
10.
I have become more callous/uncaring towards people since I took this job.
-
11.
I worry that my job is hardening me emotionally.
-
15.
I don't really care what happens to some patients.
-
22.
I feel that patients blame me for some of their problems.
Personal achievement.
-
4.
I can easily understand how my patients feel about things.
-
7.
I deal very effectively with the problems of my patients.
-
9.
I feel I'm positively influencing other people’s lives through my work.
-
12.
I feel very energetic.
-
17.
I can easily create a relaxed atmosphere with my patients.
-
18.
I feel exhilarated after working closely with my patients.
-
19.
I have accomplished many worthwhile things in my job.
-
21.
In my work I deal with emotional problems very calmly.

SF-36
1. In general, would you say your health is:
-
Excellent (1).
-
Very Good (2).
-
Good (3).
-
Fair (4).
-
Poor (5).
2. Compared to 1 year ago, would you say your health is:
-
Much better now than one year ago (1).
-
Somewhat better than one year ago (2).
-
About the same (3).
-
Somewhat worse than one year ago (4).
-
Much worse now than one year ago (5).
3. The following items are about activities you might do during a typical day. Does your health now limit you in these activities? If so, how much?
-
(Circle One Number on Each Line).
-
Yes, Limited a Lot (1).
-
Yes, Limited a Little (2).
-
No, Not limited at All (3).
-
a.
Vigorous activities, such as running, lifting heavy objects, participating in strenuous sports.
-
b.
Moderate activities, such as moving a table, pushing a vacuum cleaner, bowling, or playing golf.
-
c.
Lifting or carrying groceries.
-
d.
Climbing several flights of stairs.
-
e.
Climbing one flight of stairs.
-
f.
Bending, kneeling, or stooping.
-
g.
Walking more than a mile.
-
h.
Walking several blocks.
-
i.
Walking one block.
-
j.
Bathing or dressing yourself.
4. During the past 4 weeks, have you had any of the following problems with your work or other regular daily activities as a result of your physical health?
-
(Circle One Number on Each Line).
-
Yes (1).
-
No (2).
-
a.
Cut down the amount of time you spent on work or other activities.
-
b.
Accomplished less than you would like.
-
c.
Were limited in the kind of work or other activities.
-
d.
Had difficulty performing the work or other activities (for example, it took extra effort).
5. During the past 4 weeks, have you had any of the following problems with your work or other regular daily activities as a result of any emotional problems (such as feeling depressed or anxious)?
-
(Circle One Number on Each Line).
-
Yes (1).
-
No (2).
-
a.
Cut down the amount of time you spent on work or other activities.
-
b.
Accomplished less than you would like.
-
c.
Didn't do work or other activities as carefully as usual.
6. During the past 4 weeks, to what extent has your physical health or emotional problems interfered with your normal social activities with family, friends, neighbors, or groups?
-
Not at all (1).
-
Slightly (2).
-
Moderately (3).
-
Quite a bit (4).
-
Extremely (5).
7. How much bodily pain have you had during the past 4 weeks?
-
None (1).
-
Very mild (2).
-
Mild (3).
-
Somewhat severe (4).
-
Severe (5).
-
Very severe (6).
8. During the past 4 weeks, how much did pain interfere with your normal work (including both work outside the home and housework)?
-
Not at all (1).
-
A little bit (2).
-
Moderately (3).
-
Quite a bit (4).
-
Extremely (5).
These questions are about how you feel and how things have been with you during the past 4 weeks. For each question, please give the one answer that comes closest to the way you have been feeling.
(Circle One Number on Each Line).
9. How much of the time during the past 4 weeks...
-
a.
Did you feel full of pep? 1 2 3 4 5 6.
-
b.
Have you been a very nervous person? 1 2 3 4 5 6.
-
c.
Have you felt so down in the dumps that nothing could cheer you up? 1 2 3 4 5 6.
-
d.
Have you felt calm and peaceful? 1 2 3 4 5 6.
-
e.
Did you have a lot of energy? 1 2 3 4 5 6.
-
f.
Have you felt downhearted and blue? 1 2 3 4 5 6.
-
g.
Did you feel worn out? 1 2 3 4 5 6.
-
h.
Have you been a happy person? 1 2 3 4 5 6.
-
i.
Did you feel tired? 1 2 3 4 5 6.
10. During the past 4 weeks, how much of the time has your physical health or emotional problems interfered with your social activities (like visiting with friends, relatives, etc.)?
-
(Circle One Number).
-
All of the time (1).
-
Most of the time (2).
-
Some of the time (3).
-
A little of the time (4).
-
None of the time (5).
11. How TRUE or FALSE is each of the following statements for you.
-
(Circle One Number on Each Line).
-
Definitely True (1).
-
Mostly True (2).
-
Don't Know (3).
-
Mostly False (4).
-
Definitely False (5).
-
a.
I seem to get sick a little easier than other people 1 2 3 4 5.
-
b.
I am as healthy as anybody I know 1 2 3 4 5.
-
c.
I expect my health to get worse 1 2 3 4 5.
-
d.
My health is excellent 1 2 3 4 5.
Patient Health Questionnaire-2 (PHQ-2)
Over the last 2 weeks, how often have you been bothered by the following problems?
-
Not at all (0).
-
Several days (1).
-
More than half the days (2).
-
Nearly every day (3).
-
1.
Little interest or pleasure in doing things.
-
2.
Feeling down, depressed or hopeless.
PHQ-2 score obtained by adding score for each question (total points).
A PHQ-2 score ranges from 0 to 6. The authors identified a score of 3 as the optimal cutpoint when using the PHQ-2 to screen for depression. If the score is 3 or greater, major depressive disorder is likely.
Career satisfaction questions
Select one (Yes/ No).
Would become physician again (career choice) Yes/ No.
Would become a surgeon again (specialty choice) Yes/ No.
Would you recommend your children pursue a career as a physician/surgeon Yes/ No.
Work schedule leaves enough time for personal/family life Yes/ No.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Keller, D.S., Narula, N., Schwarz, E. et al. A cross sectional survey on burnout and career satisfaction in surgeons: a joint work from the SAGES quality, outcomes, and safety and reimaging the practice of surgery burnout task forces. Surg Endosc 38, 4776–4787 (2024). https://doi.org/10.1007/s00464-024-11123-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-024-11123-z