Abstract
Introduction
Subjective surgeon interpretation of near-infrared perfusion video is limited by low inter-observer agreement and poor correlation to clinical outcomes. In contrast, quantification of indocyanine green fluorescence video (Q-ICG) correlates with histologic level of perfusion as well as clinical outcomes. Measuring dye volume over time, however, has limitations, such as it is not on-demand, has poor spatial resolution, and is not easily repeatable. Laser speckle contrast imaging quantification (Q-LSCI) is a real-time, dye-free alternative, but further validation is needed. We hypothesize that Q-LSCI will distinguish ischemic tissue and correlate over a range of perfusion levels equivalent to Q-ICG.
Methods
Nine sections of intestine in three swine were devascularized. Pairs of indocyanine green fluorescence imaging and laser speckle contrast imaging video were quantified within perfused, watershed, and ischemic regions. Q-ICG used normalized peak inflow slope. Q-LSCI methods were laser speckle perfusion units (LSPU), the base unit of laser speckle imaging, relative perfusion units (RPU), a previously described methodology which utilizes an internal control, and zero-lag normalized cross-correlation (X-Corr), to investigate if the signal deviations convey accurate perfusion information. We determine the ability to distinguish ischemic regions and correlation to Q-ICG over a perfusion gradient.
Results
All modalities distinguished ischemic from perfused regions of interest; Q-ICG values of 0.028 and 0.155 (p < 0.001); RPU values of 0.15 and 0.68 (p < 0.001); and X-corr values of 0.73 and 0.24 (p < 0.001). Over a range of perfusion levels, RPU had the best correlation with Q-ICG (r = 0.79, p < 0.001) compared with LSPU (r = 0.74, p < 0.001) and X-Corr (r = 0.46, p < 0.001).
Conclusion
These results demonstrate that Q-LSCI discriminates ischemic from perfused tissue and represents similar perfusion information over a broad range of perfusion levels comparable to clinically validated Q-ICG. This suggests that Q-LSCI might offer clinically predictive real-time dye-free quantification of tissue perfusion. Further work should include validation in histologic studies and human clinical trials.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Many surgical complications, such as anastomotic leak, are in large part due to tissue ischemia [1,2,3]. Near-infrared imaging technologies like indocyanine green fluorescence imaging (ICG-FI) were developed in attempt to provide surgeons better information about the level of tissue perfusion intraoperatively [4, 5]. Throughout the history of ICG-FI, surgeons have been required to subjectively assess the fluorescence signal in order to infer the level of tissue perfusion. This reliance on subjective interpretation has been shown to have several issues. Previous studies have found that surgeons of various experience levels with fluorescence imaging have poor inter-observer agreement on the same ICG-FI videos [6,7,8,9,10]. Importantly, surgeons may not be able to predict those patients at increased risk of anastomotic leak when subjectively interpreting ICG-FI [7]. This difficulty with subjective interpretation may explain why some studies fail to show reduction in anastomotic leak [11], while others that enforce strict guidelines for interpretation, hinting at a more objective interpretation, show reduction in leak rate with the use of ICG-FI [12, 13].
Quantification of indocyanine green fluorescence imaging (Q-ICG) gives objectivity in signal interpretation [14, 15]. When the contrast dye is injected, the fluorescence intensity is captured for a given region over time, generating a fluorescence intensity curve. This allows the fluorescence intensity to be quantified in several ways using both static and dynamic parameters, such as max intensity, relative intensity, time to max intensity, and inflow slope [15, 16]. Studies also suggest that by normalization to the peak intensity, variability of intensity signal can be mitigated by neutralizing non-perfusion-related factors, such as distance and angle from the tissue and the specific device and imaging device in use [14,15,16].
Q-ICG has shown promise for allowing objective perfusion assessment. Pre-clinical studies showed excellent correlation between Q-ICG using dynamic parameters with histologic measures of perfusion [14]. Clinical studies have shown objective Q-ICG increases surgeon agreement on level of perfusion during intraoperative use [17], increases the safety of anastomosis creation, especially among junior surgeons [18], and can offer predictive value for anastomotic leak, even when subjective interpretation of ICG signal did not [7]. However, Q-ICG has several limitations that restrict its clinical utility in minimally invasive surgeries. Logistics of dye-based dynamic quantification parameters lead to inability for on-demand real-time assessment, difficulties with spatial resolution [19], and inability to conduct repeated assessments due to the metabolism rate of the contrast dye [16, 20]. The potential benefits offered by objective perfusion imaging assessment and the current limitations of Q-ICG indicate the need for an alternative near-infrared imaging system that allows for comparable quantification allowing for objective perfusion assessment that is real time, dye free, and repeatable.
Laser speckle contrast imaging (LSCI) measures coherent laser light scatter caused by the movement of red blood cells at the tissue surface [21]. This allows for on-demand dye-free, real-time perfusion imaging. LSCI platforms have recently been developed as an adjunct to ICG-FI in visceral and minimally invasive surgery [22, 23]. In clinical studies, LSCI has shown to present equivalent subjective perfusion assessment compared to ICG-FI [24]. Additionally, quantified laser speckle imaging (Q-LSCI) has been described in pre-clinical [25, 26] and clinical studies [24] but requires additional investigation before further clinical adoption.
In this study, we describe LSCI quantification parameters and investigate the ability of both Q-LSCI and Q-ICG to distinguish between perfused and ischemic regions in a porcine small bowel. Next, we investigate Q-LSCI correlation to Q-ICG throughout a gradient of tissue perfusion from perfused, watershed, to ischemic. We hypothesize that Q-LSCI will be able to distinguish ischemic tissue from perfused tissue comparable to Q-ICG and will correlate with Q-ICG over a broad range of tissue perfusion levels.
Materials and methods
Animals and surgical procedure
Three female Yorkshire swine were used in this experiment and were managed according to ethical guidelines per IACUC-approved Protocol (# B2021-32), institutional swine anesthesia standard operating protocol, and the ARRIVE 2.0 guidelines [27]. The average weight of the swine was 43.5 kg (SD 2.7 kg).
The animals were fasted on the morning of the surgical procedures. Anesthesia was induced using telazol (6 mg/kg), ketamine (3 mg/kg), and xylazine (3 mg/kg) and maintained using 1–2% isoflurane. All pigs were euthanized at the end of surgery. No specific exclusion criteria were used to exclude animals, and all the animals underwent same surgical procedure detailed below.
Laparotomy was performed and a bowel loop in the mid-small intestine was externalized. The bowel was divided with a stapler. Then, on each side of the division line, the bowel was devascularized for a length of 8 cm. Both ends were positioned for synchronous data collection from two experimental setups at once. In two swine, this procedure was performed twice with a loop of bowel distant from the first loop and greater than 60 min between indocyanine green dosing.
Near-infrared imaging platform experimental setup
Near-infrared imaging video was collected by mounting the imaging device at a fixed distance (12 cm) and angle (top-down orientation with 10 mm, 30-degree Stryker AIM™ endoscope) from the tissue. The near-infrared imaging platform used for this study was ActivSight™ (Activ Surgical Inc., Boston, MA, USA) which is capable of both ICG-FI and LSCI.
Paired ICG-FI and LSCI video collection was attempted on ten sections of small intestine (n = 3 animals), with one-paired collection lost due to failure of the imaging system during ICG-FI video collection. The average heart rate and mean arterial blood pressure were 100 bpm (SD 9 bpm) and 57 mmHg (SD 3 mmHg) during video collection. During two data collections (n = 3/9 quantified bowel sections), two swine required routine administration of norepinephrine to maintain a normal mean arterial pressure under anesthesia.
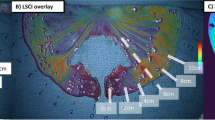
Eighteen ½ cm wide regions of interest were selected every 1 cm along the length of the bowel to the stapled end starting from 1 cm proximal to the devascularization line. Regions of interest were defined as perfused, watershed, or ischemic based on their distance from the last blood vessel leading to the bowel tissue. Four regions at or proximal to the last vessel were defined as perfused, the last two regions at the stapled end were defined as ischemic. The remaining twelve regions of interest in between were classified as watershed to create a gradient of perfusion levels from perfused through ischemic tissue (Fig. 1).
Experimental setup and regions of interest selection. A Bowel was externalized and devascularized for a length of 8 cm. Perfused, watershed, and ischemic regions are defined by the distance from devascularization line. B Eighteen ½ cm wide regions of interest are placed every 1 cm along the tissue with (green = perfused, orange = watershed, red = ischemic). Near-infrared videos are obtained using indocyanine green fluorescence imaging (C) and laser speckle contrast imaging (D) (Color figure online)
ICG-FI video collection and quantification
Following recommended dosing, 0.2 mg/kg of indocyanine green dye (2.5-mg/ml solution rounded up to the nearest milliliter) was injected into the central circulation [14] followed by an immediate flush of 10-ml normal saline. ICG-FI video was collected at 30 frames per second and collection was initiated prior to injection and for 5 min following injection.
Quantification of ICG-FI was done using custom computer software. Pixels within the pre-defined regions of interest were averaged, batched every 100 frames, and measured over the duration of the collection to create region of interest fluorescence intensity curves. To avoid aberrant peak slope selection secondary to signal noise, a smoothing function with an unweighted window size of 5 was applied prior to selection of the peak slope. This means that each intensity value at a given timepoint was averaged with the four nearest neighboring values. The Q-ICG parameter of normalized peak inflow slope was selected due to the large body of supporting evidence showing it correlates with histologic measures of perfusion and clinical outcomes [7, 14, 20]. Each video data were manually inspected, and the video was cropped to isolate the entire inflow section of all curves and the peak inflow slope of the curve was measured (Fig. 2). This was then normalized to the maximum intensity of the given fluorescence intensity curve to return the normalized peak inflow slope.
LSCI video collection and quantification
LSCI is real-time dye-free near-infrared imaging that measures tissue perfusion by detecting the movement of red blood cells at the surface of the tissue. This allows for near-instant quantification without the need to measure the volume of contrast dye over time. LSCI video was collected for a duration of 2 minutes immediately prior to ICG-FI video collection and a 2-s clip was used for quantification. LSCI was quantified using three quantification methods in order to assess different ways that LSCI signal might represent tissue perfusion level (Fig. 3).
-
1.
Laser speckle perfusion units
-
2.
Relative perfusion units
-
3.
Zero-lag normalized cross-correlation.
Visual representation of laser speckle contrast imaging quantification methods. Laser speckle perfusion units (LSPU) are displayed as a function of time for reference (dashed) and a region of interest (ROI, solid). LSPU quantification uses mean LSPU for a region of interest over a 2-s window (horizontal dashed line). Relative perfusion units utilize the ratio of the mean LSPU over a 2-s window within the ROI to the mean LSPU within the reference (dashed lines). Zero-lag normalized cross-correlation (X-corr) quantifies deviations from the means at a given time (arrows) throughout the 2-s time window
Laser speckle perfusion units (LSPU) are returned by the imaging platform as the fundamental arbitrary unit of LSCI and are defined by Eq. 1 [28]. These represent the level of blurring of the coherent laser light scatter caused by the movement of red blood cells. LSPU are limited in that they are sensitive to changes in camera distance, angle, and tissue and technological optical properties, such as laser power [21].
Relative perfusion units (RPU) attempt to mitigate these confounding factors using relative quantification to an internal control reference area. RPU measures LSPU values within a region of interest relative to known perfused region and are defined by Eq. 2. In this study, a surface-level capillary within the perfused region was used as the reference. LSPU and RPU quantification parameters have been described in pre-clinical and clinical studies [24,25,26, 29, 30].
A new parameter, zero-lag normalized cross-correlation (X-corr) was used to test if variability of LSCI signal conveyed important perfusion information and is defined in Eq. 3. This quantification methodology measures the variability in the LSPU signal similar to how pulse pressure measures the variability in systemic vascular perfusion. The reference region used to calculate RPU and X-corr were the same.
Ischemic vs perfused regions of interest
Average values of each quantification modality were calculated for all perfused and ischemic regions. Within each quantification modality, we tested for statistical difference and % change from ischemic to perfused regions to determine if that modality could reliably distinguish between the perfused and ischemic regions.
Correlation of Q-LSCI to Q-ICG in perfusion gradient
To investigate Q-LSCI ability to measure tissue ischemia over a gradient of perfusion levels, correlation between Q-ICG and Q-LSCI was measured over all perfused, ischemia, and watershed regions.
Statistical analyses
Student’s T and Mann–Whitney U tests were used to test for statistical differences between average perfused and ischemic regions within each quantification modality. Shapiro test for normality was used to test the populations for normality, Student’s T was applied when both averages demonstrated normality, and Mann–Whitney U when one or both did not. Correlation between Q-LSCI and Q-ICG parameters was done using Pearson Correlation Coefficient. Statistical analysis was performed using the Python (version 3.8.10) programming language and the SciPy Python library.
Results
ICG-FI video data
Nine ICG-FI videos were collected and data were analyzed within the regions of interest classified by perfusion status. Representative ICG-FI video data are shown in Fig. 4. The inflow period is completely captured within 67 and 267 s of this ICG-FI video. ICG-FI curves show distinction between perfused and ischemic regions of interest, while the watershed regions of interest represent a gradient of perfusion with overlapping ends. The peak fluorescence intensity of the perfused region of interest intensity curves occurs between 200 and 250 s into the recording (Fig. 4).
LSCI video data
Similarly, nine corresponding LSCI videos were collected and LSPU within each region of interest were analyzed. The corresponding LSCI video to Fig. 4 is shown in Fig. 5 over the 2-s window. As with ICG-FI, the LSCI curves show distinction between the perfused and ischemic regions, while the watershed regions of interest represent a gradient of perfusion with overlapping ends. The LSPU data of a surface-level capillary is shown and is used as the internal control reference in RPU and X-corr quantification. The LSPU curves show three distinct peaks in this 2-s window, consistent with variation in LSPU secondary to pulsatile flow with cardiac activity.
Ischemic vs perfused regions of interest
Q-ICG (normalized peak inflow slope) showed statistical differences between perfused and ischemic regions of interest; perfused = 0.155 (S.D. 0.034) and ischemic = 0.028 (S.D. 0.015) (p < 0.001). The perfused regions showed greater than 4.5-fold increase in normalized peak inflow slope from ischemic regions (% change = 454%). Quantification of LSCI using RPU statistically distinguished between perfused and ischemic regions as well; perfused = 0.68 (S.D. 0.13) and ischemic = 0.15 (S.D. 0.04) (p < 0.001). The perfused regions showed greater than 3.5-fold increase in RPU from ischemic regions (% change = 353%). LSPU and X-corr also distinguished between perfused and ischemic regions of interest; X-corr showed average correlation values of 0.79 (S.D. 0.19) for perfused regions and 0.24 (S.D. 0.20) for ischemic regions (p < 0.001) with a % change of 204%; LSPU showed average values of 64.93 (S.D. 21.08) for perfused regions and 14.56 (S.D. 6.96) for ischemic regions (p < 0.001) with a % change of 346% (Table 1).
Correlation of Q-LSCI to Q-ICG over perfusion gradient
Q-LSCI using LSPU showed a strong correlation with Q-ICG (normalized peak inflow slope) throughout a gradient of tissue perfusion levels (perfused, ischemic, and watershed) and Pearson correlation coefficient of r = 0.74 (p < 0.001) (Fig. 6). Quantification using RPU showed the strongest correlation to quantified indocyanine green; r = 0.79 (p < 0.001), suggesting that both LSPU and RPU estimate tissue perfusion level similar to Q-ICG. In contrast, quantifying perfusion using the variations in LSPU signal (X-corr) showed the weakest correlation; r = 0.46 (p < 0.001) (Fig. 6).
Correlation between quantified indocyanine green fluorescence imaging (normalized peak inflow slope) to quantified laser speckle contrast imaging parameters throughout different levels of tissue perfusion. Dashed line represents linear regression. Laser speckle quantification parameters are (A) laser speckle perfusion units (LSPU, r = 0.74, p < 0.001), (B) relative perfusion units (RPU, r = 0.79, p < 0.001), and (C) zero-lag normalized cross-correlation (X-corr, r = 0.46, p < 0.001)
Discussion
In this study, we investigated the utility of objective near-infrared perfusion video assessment using Q-LSCI to the histologically and clinically validated Q-ICG parameter of normalized peak inflow slope. We report that LSCI quantification methods of LSPU, RPU, and X-corr reliably distinguish between perfused and ischemic regions of interest in this porcine model. Peak normalized inflow slope (Q-ICG) showed greater than 4.5-fold increase from ischemic to perfused regions, supporting previous studies that it is a clinically useful parameter that reliably identifies ischemic tissue [14, 16, 20]. The Q-LSCI parameters LSPU, RPU, and X-corr also showed ability to reliably distinguish between ischemic and perfused regions. Among these parameters, LSPU and RPU showed the greatest change from ischemic to perfused regions with an approximately 3.5-fold increase, while X-corr showed an approximate twofold increase. This large magnitude of difference between ischemic and perfused regions suggests that LSPU and RPU may allow for immediate real-time identification of ischemia in a binary fashion that is often employed clinically [9].
To further dissect the similarities between Q-LSCI and Q-ICG throughout a gradient of tissue perfusion levels, we assessed correlation between the two modalities throughout all regions of interest from perfused, watershed, and ischemic. We found that Q-LSCI using RPU had the highest correlation to Q-ICG imaging normalized slope parameter (r = 0.79). This indicates that Q-LSCI quantifies the level of bowel perfusion comparable to the validated normalized peak inflow slope metric of Q-ICG. However, LSPU also had high correlation (r = 0.74) despite the dependency on camera distance, angle, and tissue optical properties that could limit the use in real-world clinical applications. This high correlation in this study can be explained by the fixed camera distance and angle to the target tissue, mitigating these limitations of LSPU. Finally, X-corr had the lowest correlation (r = 0.46). This correlation was much lower than RPU, indicating that in this porcine model, the variation in the laser speckle curve due to cardiac activity is less predictive of level of tissue perfusion throughout a broad range of perfusion levels compared to the average LSPU value.
Q-ICG methodology
ICG-FI measures the signal intensity emitted from the volume of contrast dye in the tissue. ICG-FI can be quantified using static or dynamic parameters. Static quantification indicates that the fluorescence intensity is measured at a single point in time while dynamic means that the change in fluorescence intensity is measured over time. Static analysis suffers from variability introduced by differences in contrast dye concentration and timing, distance and angle to the target tissue, diffusion of contrast dye into ischemic tissue [31], and technological choices made by the imaging platform manufacture [32, 33]. Previous literature supports the superiority of dynamic quantification parameters, such as time to max intensity, time to half-max intensity, and inflow slope as these avoid confounding variables encountered with static analysis [14, 16]. One study showed differences in the shape of the intensity curves in patients with and without anastomotic leak after esophageal reconstruction, although the study was not powered to show statistical differences [6]. However, another study on colorectal reconstruction showed a statistical difference in the normalized inflow slope parameter in patients that went on to develop anastomotic leak versus those that did not [7].
Similar to using dynamic over static analysis, normalization to the peak fluorescence intensity provides additional advantage as it further reduces variable effects of camera distance, dye dosage, and technological differences between imaging platforms that could reduce comparability of quantified parameters between patients and imaging systems [16, 20]. Normalized peak inflow slope was selected as the ICG-FI quantification parameter in this study due to the high correlation with histologic and clinical endpoints and being a prime candidate for clinically usable and relevant ICG-FI quantification [14,15,16, 20].
Q-LSCI methodology
LSPU are the arbitrary unit-less values derived from the laser speckle imaging system and are defined in Eq. 1. [28] LSPU have been shown to correlate modestly with tissue lactate levels [23] and previously showed poor correlation with Q-ICG [26]. However, LSPU are known to vary in magnitude due to distance from and angle to the target tissue, intrinsic tissue properties, laser power, and technological specifications within the imaging platform like laser power [21]. Although LSPU quantification is the easiest to implement clinically, it is generally unreliable to compare LSPU from one patient to the next, especially in a clinical setting within a diverse clinical contexts and patient factors. This would mean that values that represent high perfusion in one case may not represent the same level of perfusion in the next.
One way to mitigate LSPU limitations is to use a quantification methodology that utilizes an internal control and relative values specific to that patient and tissue. RPU are derived from measuring LSPU relative to a surface-level capillary on the target tissue, which tend to have the highest LSPU values, and are defined by Eq. 2. RPU quantification converts LSPU into a relative scale represented as a percentage ranging from 0 (no flow) to 100% (LSPU of the reference tissue) [30]. This quantification parameter has previously been described in pre-clinical studies by Nerup et al. and Liu et al. [26, 29, 30] and Skinner et al. in human colorectal resections [24]. The strength of RPU is that confounding variables that effects on LSPU like camera distance, angle to the tissue, and the optical properties of the tissue and imaging platform are minimized since the quantification is internally controlled using the reference region.
LSPU are also known to oscillate in response to pulsatile blood flow caused by cardiac activity [34]. To investigate if the variability of the laser speckle perfusion units better represent tissue perfusion status, we quantified laser speckle using X-corr as defined by Eq. 3. In Fig. 3, LSPU from two regions over time are visualized. X-corr quantifies the correlation between the LSPU deviations from the respective mean values of a reference region and a region of interest at each time point over the given time window. This means that regions that deviate from the mean LSPU value in the same direction and with similar magnitude as the reference region will have higher X-corr values, regions that deviate in opposite directions and with dissimilar magnitude will have lower X-corr values. The values range from -1, indicating the deviations are in exactly opposite directions with identical magnitude, to + 1, indicating the deviations move in the same directions with identical magnitude and 0 indicating no correlation between the LSPU deviations from the means. X-corr had the lowest percent change from ischemic to perfused regions of interest and poorest correlation over a broad range of tissue perfusion suggesting that the deviations of the LSCI signal caused by cardiac activity are less indicative of perfusion than the average LSPU value itself. This is analogous to how mean arterial blood pressure is used to measure global systemic perfusion as opposed to pulse pressure.
As with any quantification method that uses relative values to a reference region, implementation must be carefully designed. To function properly in a clinical setting, the user either must select the reference region or it must be accurately chosen algorithmically. Then, camera or tissue movement must be mitigated by either fixing them in space or using computer vision tracking software.
In this study, we present three Q-LSCI parameters: LSPU, RPU, and X-corr. Based on the ability to robustly distinguish between perfused and ischemic tissue regions, high correlation with validated Q-ICG parameter of normalized peak inflow slope, and potential mitigation of variables such as camera distance, angle, and tissue and patient factors, RPU is proposed to be the most clinically relevant parameter in this study.
Previous Q-LSCI studies
A recent study by Rønn et al. compared Q-LSCI, using LSPU and RPU, to Q-ICG and were found to have poor correlation, although they were both found to correlate well to tissue lactate levels [26]. Importantly, this study used two different imaging systems, a commercially available, minimally invasive ICG-FI system, and a non-minimally invasive laser speckle imaging system. Because of the difference in form factors, distance and angle to the tissue could not be controlled. In contrast, our study captured both near-infrared imaging modalities in a single unified, minimally invasive imaging platform. This single imaging platform is not only more clinically relevant as it is a minimally invasive system that offers both ICG-FI and LSCI, but it also allows for capturing the ICG-FI and LSCI video at the exact same distance and angle in this study compared to previous study.
Q-LSCI vs Q-ICG
Q-ICG is a promising technology that may improve more objective interpretation of the ICG-FI video, bypassing error-prone subjective interpretation. However, Q-ICG does not allow for on-demand real-time quantification and clinical utility at this time has major limitations; the camera and tissue must remain fixed for a long period of time during the injection of contrast dye and collection of ICG-FI video, any movement of the camera or tissue degrades the spatial resolution as more and more pixels are averaged together [19], and repeat dosing is difficult, with the minimal time between injections described as 15–20 min. [20] In contrast, Q-LSCI is real-time, dye-free, on-demand with minimal latency, and repeatable which may make it a more satisfactory option for use in minimally invasive surgeries.
Study limitations and conclusion
This study is limited by the fact we could not compare Q-ICG parameter of normalized slope between different ICG-FI systems and quantification platforms and that quantification using the given platform was done with non-commercially available custom software.
In conclusion, this study showed that quantified laser speckle contrast imaging offers on-demand, real-time, dye-free, and repeatable perfusion quantification comparable to validated quantified indocyanine green fluorescence imaging in a porcine model and thus shows great potential for clinical utility as an objective measure of tissue perfusion.
References
Ikeda Y, Niimi M, Kan S, Shatari T, Takami H, Kodaira S (2001) Clinical significance of tissue blood flow during esophagectomy by laser Doppler flowmetry. J Thorac Cardiovasc Surg 122:1101–1106. https://doi.org/10.1067/mtc.2001.117835
Vignali A, Gianotti L, Braga M, Radaelli G, Malvezzi L, Carlo VD (2000) Altered microperfusion at the rectal stump is predictive for rectal anastomotic leak. Dis Colon Rectum 43:76–82. https://doi.org/10.1007/BF02237248
Karliczek A, Harlaar NJ, Zeebregts CJ, Wiggers T, Baas PC, van Dam GM (2009) Surgeons lack predictive accuracy for anastomotic leakage in gastrointestinal surgery. Int J Colorectal Dis 24:569–576. https://doi.org/10.1007/s00384-009-0658-6
Jafari MD, Wexner SD, Martz JE, McLemore EC, Margolin DA, Sherwinter DA, Lee SW, Senagore AJ, Phelan MJ, Stamos MJ (2015) Perfusion assessment in laparoscopic left-sided/anterior resection (PILLAR II): a multi-institutional study. J Am Coll Surg 220:82-92.e1. https://doi.org/10.1016/j.jamcollsurg.2014.09.015
Nachiappan S, Askari A, Currie A, Kennedy RH, Faiz O (2014) Intraoperative assessment of colorectal anastomotic integrity: a systematic review. Surg Endosc 28:2513–2530. https://doi.org/10.1007/s00464-014-3520-z
Galema HA, Faber RA, Tange FP, Hilling DE, van der Vorst JR, Upper-GI ICG Quantification Study Group (2023) A quantitative assessment of perfusion of the gastric conduit after oesophagectomy using near-infrared fluorescence with indocyanine green. Eur J Surg Oncol 49(5):990–995. https://doi.org/10.1016/j.ejso.2023.02.017
Larsen PO, Nerup N, Andersen J, Dohrn N, Klein MF, Brisling S, Salomon S, Andersen PV, Möller S, Svendsen MBS, Rahr HB, Iversen LH, Gögenur I, Qvist N, Ellebaek MB (2023) Anastomotic perfusion assessment with indocyanine green in robot-assisted low-anterior resection, a multicenter study of interobserver variation. Surg Endosc 37:3602–3609. https://doi.org/10.1007/s00464-022-09819-1
Dalli J, Joosten JJ, Jindal A, Hardy NP, Camilleri-Brennan J, Andrejevic P, Hompes R, Cahill RA (2024) Impact of standardising indocyanine green fluorescence angiography technique for visual and quantitative interpretation on interuser variability in colorectal surgery. Surg Endosc 38:1306–1315. https://doi.org/10.1007/s00464-023-10564-2
Hardy NP, Dalli J, Khan MF, Andrejevic P, Neary PM, Cahill RA (2021) Inter-user variation in the interpretation of near infrared perfusion imaging using indocyanine green in colorectal surgery. Surg Endosc 35:7074–7081. https://doi.org/10.1007/s00464-020-08223-x
Hardy NP, Joosten JJ, Dalli J, Hompes R, Cahill RA, Van Berge Henegouwen MI (2022) Evaluation of inter-user variability in indocyanine green fluorescence angiography to assess gastric conduit perfusion in esophageal cancer surgery. Dis Esophagus 35:doac016. https://doi.org/10.1093/dote/doac016
Jafari MD, Pigazzi A, McLemore EC, Mutch MG, Haas E, Rasheid SH, Wait AD, Paquette IM, Bardakcioglu O, Safar B, Landmann RG, Varma MG, Maron DJ, Martz J, Bauer JJ, George VV, Fleshman JW, Steele SR, Stamos MJ (2021) Perfusion assessment in left-sided/low anterior resection (PILLAR III): a randomized, controlled, parallel, multicenter study assessing perfusion outcomes with PINPOINT near-infrared fluorescence imaging in low anterior resection. Dis Colon Rectum 64:995–1002. https://doi.org/10.1097/DCR.0000000000002007
Watanabe J, Takemasa I, Kotake M, Noura S, Kimura K, Suwa H, Tei M, Takano Y, Munakata K, Matoba S, Yamagishi S, Yasui M, Kato T, Ishibe A, Shiozawa M, Ishii Y, Yabuno T, Nitta T, Saito S, Saigusa Y, Watanabe M, EssentiAL Trial Group (2023) Blood perfusion assessment by indocyanine green fluorescence imaging for minimally invasive rectal cancer surgery (EssentiAL trial): a randomized clinical trial. Ann Surg 278(4):e688–e694. https://doi.org/10.1097/SLA.0000000000005907
Alekseev M, Rybakov E, Shelygin Y, Chernyshov S, Zarodnyuk I (2020) A study investigating the perfusion of colorectal anastomoses using fluorescence angiography: results of the FLAG randomized trial. Colorectal Dis 22:1147–1153. https://doi.org/10.1111/codi.15037
Nerup N, Andersen HS, Ambrus R, Strandby RB, Svendsen MBS, Madsen MH, Svendsen LB, Achiam MP (2017) Quantification of fluorescence angiography in a porcine model. Langenbecks Arch Surg 402:655–662. https://doi.org/10.1007/s00423-016-1531-z
Goncalves LN, van den Hoven P, van Schaik J, Leeuwenburgh L, Hendricks CHF, Verduijn PS, van der Bogt KEA, van Rijswijk CSP, Schepers A, Vahrmeijer AL, Hamming JF, van der Vorst JR (2021) Perfusion parameters in near-infrared fluorescence imaging with indocyanine green: a systematic review of the literature. Life 11:433. https://doi.org/10.3390/life11050433
Van Den Hoven P, Osterkamp J, Nerup N, Svendsen MBS, Vahrmeijer A, Van Der Vorst JR, Achiam MP (2023) Quantitative perfusion assessment using indocyanine green during surgery — current applications and recommendations for future use. Langenbecks Arch Surg 408:67. https://doi.org/10.1007/s00423-023-02780-0
Nerup N, Svendsen MBS, Svendsen LB, Achiam MP (2020) Feasibility and usability of real-time intraoperative quantitative fluorescent-guided perfusion assessment during resection of gastroesophageal junction cancer. Langenbecks Arch Surg 405:215–222. https://doi.org/10.1007/s00423-020-01876-1
Nerup N, Svendsen MBS, Rønn JH, Konge L, Svendsen LB, Achiam MP (2022) Quantitative fluorescence angiography aids novice and experienced surgeons in performing intestinal resection in well-perfused tissue. Surg Endosc 36:2373–2381. https://doi.org/10.1007/s00464-021-08518-7
Park S-H, Park H-M, Baek K-R, Ahn H-M, Lee IY, Son GM (2020) Artificial intelligence based real-time microcirculation analysis system for laparoscopic colorectal surgery. World J Gastroenterol 26:6945–6962. https://doi.org/10.3748/wjg.v26.i44.6945
Lütken CD, Achiam MP, Svendsen MB, Boni L, Nerup N (2020) Optimizing quantitative fluorescence angiography for visceral perfusion assessment. Surg Endosc 34:5223–5233. https://doi.org/10.1007/s00464-020-07821-z
Heeman W, Dijkstra K, Hoff C, Koopal S, Pierie J-P, Bouma H, Boerma EC (2019) Application of laser speckle contrast imaging in laparoscopic surgery. Biomed Opt Express 10:2010. https://doi.org/10.1364/BOE.10.002010
Nwaiwu CA, McCulloh CJ, Skinner G, Shah SK, Kim PCW, Schwaitzberg SD, Wilson EB (2023) Real-time first-in-human comparison of laser speckle contrast imaging and ICG in minimally invasive colorectal & bariatric surgery. J Gastrointest Surg. https://doi.org/10.1007/s11605-023-05855-x
Heeman W, Wildeboer ACL, Al-Taher M, Calon JEM, Stassen LPS, Diana M, Derikx JPM, Van Dam GM, Boerma EC, Bouvy ND (2023) Experimental evaluation of laparoscopic laser speckle contrast imaging to visualize perfusion deficits during intestinal surgery. Surg Endosc 37:950–957. https://doi.org/10.1007/s00464-022-09536-9
Skinner G, Liu Y, Harzman A, Husain S, Gasior A, Cunningham L, Traugott A, McCulloh C, Kalady M, Kim P, Huang E (2024) Clinical utility of laser speckle contrast imaging (LSCI) compared to indocyanine green (ICG) and quantification of bowel perfusion in minimally invasive, left-sided colorectal resections. Dis Colon Rectum 67:850–859. https://doi.org/10.1097/DCR.0000000000003098
Mehrotra S, Liu YZ, Nwaiwu CA, Buharin VE, Stolyarov R, Schwaitzberg SD, Kalady MF, Kim PCW (2023) Real-time quantification of bowel perfusion using laparoscopic laser speckle contrast imaging (LSCI) in a porcine model. BMC Surg 23:261. https://doi.org/10.1186/s12893-023-02161-w
Rønn JH, Nerup N, Strandby RB, Svendsen MBS, Ambrus R, Svendsen LB, Achiam MP (2019) Laser speckle contrast imaging and quantitative fluorescence angiography for perfusion assessment. Langenbecks Arch Surg 404:505–515. https://doi.org/10.1007/s00423-019-01789-8
Percie Du Sert N, Hurst V, Ahluwalia A, Alam S, Avey MT, Baker M, Browne WJ, Clark A, Cuthill IC, Dirnagl U, Emerson M, Garner P, Holgate ST, Howells DW, Karp NA, Lazic SE, Lidster K, MacCallum CJ, Macleod M, Pearl EJ, Petersen OH, Rawle F, Reynolds P, Rooney K, Sena ES, Silberberg SD, Steckler T, Würbel H (2020) The ARRIVE guidelines 2.0: updated guidelines for reporting animal research. PLoS Biol 18:e3000410. https://doi.org/10.1371/journal.pbio.3000410
Briers D, Duncan DD, Hirst E, Kirkpatrick SJ, Larsson M, Steenbergen W, Stromberg T, Thompson OB (2013) Laser speckle contrast imaging: theoretical and practical limitations. J Biomed Opt 18:066018. https://doi.org/10.1117/1.JBO.18.6.066018
Liu YZ, Mehrotra S, Buharin VE, Marois M, Nwaiwu CA, Wilson EB, Kim PCW (2023) Dye-less perfusion quantification of porcine gastric conduit with laser speckle contrast imaging and laser Doppler imaging. J Gastrointest Surg. https://doi.org/10.1007/s11605-023-05708-7
Liu YZ, Mehrotra S, Nwaiwu CA, Buharin VE, Oberlin J, Stolyarov R, Schwaitzberg SD, Kim PCW (2023) Real-time quantification of intestinal perfusion and arterial versus venous occlusion using laser speckle contrast imaging in porcine model. Langenbecks Arch Surg 408:114. https://doi.org/10.1007/s00423-023-02845-0
D’Urso A, Agnus V, Barberio M, Seeliger B, Marchegiani F, Charles A-L, Geny B, Marescaux J, Mutter D, Diana M (2021) Computer-assisted quantification and visualization of bowel perfusion using fluorescence-based enhanced reality in left-sided colonic resections. Surg Endosc 35:4321–4331. https://doi.org/10.1007/s00464-020-07922-9
Son GM, Kwon MS, Kim Y, Kim J, Kim SH, Lee JW (2019) Quantitative analysis of colon perfusion pattern using indocyanine green (ICG) angiography in laparoscopic colorectal surgery. Surg Endosc 33:1640–1649. https://doi.org/10.1007/s00464-018-6439-y
Pruimboom T, Van Kuijk SMJ, Qiu SS, Van Den Bos J, Wieringa FP, Van Der Hulst RRWJ, Schols RM (2020) Optimizing indocyanine green fluorescence angiography in reconstructive flap surgery: a systematic review and ex vivo experiments. Surg Innov 27:103–119. https://doi.org/10.1177/1553350619862097
Zakharov P, Scheffold F, Weber B (2015) Laser speckle analysis synchronised with cardiac cycle. Novel Biophotonics Techniques and Applications III. Optica Publishing Group, Washington, p 954008
Acknowledgements
We would like to thank our hardworking team members at Tufts University Comparative Medicine Services for providing exceptional care to the animal subjects in this study.
Funding
This study was funded by Activ Surgical Inc., Boston, MA, USA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Steven Schwaitzberg and Garrett Skinner are consultants for Activ Surgical. Drs. Mikael Marois and John Oberlin are former employees of Activ Surgical. Dr. Christopher McCulloh is a current employee of Activ Surgical. Dr. Peter Kim is founder of Activ Surgical.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Skinner, G.C., Marois, M., Oberlin, J. et al. Dye-less quantification of tissue perfusion by laser speckle contrast imaging is equivalent to quantified indocyanine green in a porcine model. Surg Endosc (2024). https://doi.org/10.1007/s00464-024-11061-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00464-024-11061-w