Abstract
Background and aims
Endoscopic multiple plastic stents are an established first-line treatment for anastomotic biliary stricture (ABS) management after liver transplantation (LT). Fully covered self-expandable metallic stents (FCSEMSs) have recently been used with favorable outcomes, but long-term treatment outcomes remain an issue for ABS. We evaluated the long-term outcomes of FCSEMS for the management of refractory ABS after LT.
Methods
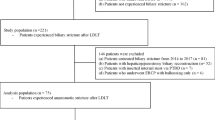
We reviewed the prospectively collected and maintained endoscopic retrograde cholangiography database at Asan Medical Center to retrieve consecutive post-LT ABS cases that underwent an endoscopic FCSEMS placement between August 2009 and August 2019 after MPS placement failure.
Results
A total of 34 patients were enrolled in this study. Technical success had been achieved in all subjects (100%). The median stent placement duration was 3.1 months (IQR 2.7–6.1). Stricture resolution was achieved in 26 patients (clinical success 76.5%, 95% confidence interval 62–91). Early adverse events developed in 3 patients (8.8%), including distal stent migration. Late adverse events occurred in 9 patients (26.5%), including cholangitis (n = 7, 20.6%) and asymptomatic distal stent migration (n = 2, 5.9%). The median follow-up period was 57.9 months (IQR 51.9–64.3). Stricture recurrence occurred in 3 of 26 patients who achieved clinical success (11.5%).
Conclusions
FCSEMS placement appears to be an effective and advisable intervention for refractory ABS as it can provide persistent stricture improvement over the long-term.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Liver transplantation (LT) is the treatment of choice for acute liver failure, cirrhosis, and hepatocellular carcinoma [1]. Despite advances in surgical techniques, graft preservation, and immunosuppressive treatment however, biliary strictures have remained the most common adverse events of an LT, occurring in up to 10% of deceased-donor liver transplantation (DDLT) and 30% of living-donor liver transplantation (LDLT) cases [2,3,4,5].
Endoscopic retrograde cholangiography (ERC) is currently the first line treatment for the management of an anastomotic biliary strictures (ABS) after LT [6]. Multiple plastic stent (MPS) placement with an increasing number of stents at each stent exchange is the preferential approach and provides a high success rate of up to 94% [4, 7,8,9]. Notably however, MPS placement usually requires 4 or 5 sessions of ERC to achieve resolution of the ABS [10, 11]. Recently, fully covered self-expandable metal stents (FCSEMSs) have been used to treat malignant biliary strictures and it have been applied also for benign biliary strictures, including post-LT ABS. An FCSEMS has a larger diameter than the plastic stent, which produces a longer patency and lower risk of stent blockage [12]. FCSEMS placement has proposed as an alternative method for MPS placement and few studies have demonstrated the efficacy of this method in patients with post-LDLT ABS [12,13,14,15,16,17]. To date however, the long-term outcomes of FCSEMS placement still remain unclear in patients with post-LDLT ABS. We therefore further evaluated the long-term outcomes of FCSEMS placement for the management of refractory post-LT ABS is in our present study.
Methods
Patients
We reviewed the prospectively collected and maintained ERC database at Asan Medical Center to retrieve information on consecutive patients with post-LDLT ABS who had undergone endoscopic FCSEMS placement between August 2009 and August 2019. Prior to the ERC in each case, an ABS had been identified on cross-sectional imaging studies, including computed tomography (CT) or magnetic resonance cholangiopancreatography (MRCP), or external biliary drainage tube cholangiogram. The inclusion criteria for this present study were: (1) an age of at least 20 years, (2) a post-LT ABS with bilobiliary anastomosis, and (3) refractory ABS. The exclusion criteria were: (1) aged below 20 years, (2) a non-anastomotic biliary stricture (NABS), (3) a biloenteric anastomosis (i.e., hepaticojeunostomy), or (4) malignant biliary strictures. Written informed consent was obtained from all patients before undergoing ERC. This study was approved by the Institutional Review Board (IRB) at Asan Medical Center (IRB number: 2020-0769).
Procedures
ERC was carried out by two experienced endoscopists (S.K.L and D.O) who each performed more than 1000 cases annually. All procedures were performed under conscious sedation with intravenous midazolam and meperidine using a therapeutic duodenoscope (TJF 260; Olympus Optical, Tokyo, Japan). Prophylactic antibiotics was administered intravenously before the procedure. After selective biliary cannulation, a cholangiogram was obtained to assess the location and configuration of the anastomotic stricture. Biliary sphincterotomy had already been performed in all patients for previous MPS to allow easier instrumentation and stent placement. Under fluoroscopic guidance, a guidewire was inserted across the anastomotic stricture. In patients with severe stricture, hydrostatic 6-mm or 8-mm balloon dilatation (Hurricane™, Boston Scientific, Natick, MA) was performed before FCSEMS placement. The FCSEMS diameter was selected according to the diameter of intrahepatic bile duct (IHD) above the stricture. The FCSEMS length was set to allow 0.5 to 1 cm of each end to extend beyond the stricture segment [18]. The center of the FCSEMS was placed at the center of the anastomotic stricture under fluoroscopic guidance. Plastic stent placement was considered if cross blockage of a branch of the IHD by the FCSEMS was suspected.Transpapillary stent placement was performed in our patient series from 2007 to 2016. From 2017 onwards, suprapapillary stent placement was conducted since a modified intraductal FCSEMS was available. The FCSEMS was placed inside the bile duct and only the long lasso was exposed to the duodenal lumen. The exchange or removal of the FCSEMS was performed 2–3 months after its placement. The FCSEMS was removed using rat-tooth forceps. A follow-up balloon-occluded cholangiogram was used after stent removal to evaluate ABS improvement. If the stricture was not resolved, a new FCSEMS was placed.
Modified FCSEMS
Conventional FCSEMS (BONASTENT; Standard Sci-Tech Inc., Seoul, South Korea) was used from 2007 to 2016 at our hospital. From 2017 onward, a newly modified FCSEMS was introduced in our institute. For stricture dilation, two types of newly designed modified intraductal FCSEMS (Kaffes, Taewoong Medical, Seoul, Korea; BONASTENT M-Intraductal, Standard Sci-Tech Inc.) were used among the current study patients, in accordance with the diameter of the IHD above the anastomotic stricture. These two stents have a common saddle-like shape in the central portion that prevents migration, and both distal ends have a large diameter. The aforementioned Kaffes stent is 6 mm in diameter at each end and gradually tapers to a central diameter of 4 mm (Fig. 1). It also has three radiopaque markers for precise positioning of the stent at the stricture site and a 10 cm length of retrievable radiopaque string at its end for endoscopic removal. The available lengths for this stent are 4, 6, and 8 cm and it is equipped with an 8.5-Fr delivery system. The M-intraductal stent is 8 and 10 mm in diameter at opposite ends and 6 mm at the central portion (Fig. 1). It also has three radiopaque markers to enable precise placement. A 7 cm length of string is attached to the distal end for endoscopic stent removal. This modified FCSEMS is available in lengths ranging from 3 to 8 cm and is equipped with an 8-Fr standard delivery device.
Follow-up
Patient follow-up was based on an outpatient examination, including clinical symptoms, abnormal laboratory findings, and signs of adverse events, including cholangitis, at least once every 4 weeks or whenever adverse events arose while the stent was in place [15]. After resolution of the ABS, a follow-up was performed every 3 months or whenever adverse events occurred. When stricture recurrence was suspected, imaging studies, such as CT or MRCP, or a diisopropyl iminodiacetic acid scan were performed [17]. After confirmation of ABS recurrence, ERC was performed for stent placement.
Definitions of outcomes
Refractory stricture was defined as an ABS relapse within 6 months after removal of a plastic stent which had been in place for at least 12 months, or persistent ABS despite MPS placement. Technical success was defined as appropriate stent placement along the stricture with free flow of contrast through the deployed FCSEMS [18]. Clinical success was defined as an ABS resolution after stent removal [13]. Stricture resolution was considered to be the disappearance of stricture on a cholangiogram at the time of stent removal and when a 12-mm extraction balloon could easily pass through the anastomosis [13]. Stent occlusion was defined as the development of obstructive jaundice, with or without cholangitis, that was confirmed clinically and via cross-sectional radiologic imaging. Stent migration was defined as any displacement of the stent into the bile duct (proximal migration) or duodenum (distal migration) [19]. Adverse events were classified in accordance with a lexicon for endoscopic adverse events proposed by consensus guideline [20]. An early adverse event was defined as any procedure-related adverse event within 14 days. A late adverse event was defined as any procedure -related adverse event occurring 14 days after the procedure [20].
Statistical analysis
All of the statistical analyses in this present study were conducted using SPSS version 22.0 (SPSS Inc., Chicago, IL). The results were expressed as a median or interquartile range (IQR) with a 95% confidence interval (CI). Categorical variables were compared using a Fisher’s exact test, and continuous variables using the Mann–Whitney U-test. The cumulative stricture recurrence free survival rate after stent removal was analyzed with the Kaplan–Meier method. A P value < 0.05 was considered statistically significant.
Results
Baseline characteristics of the study patients
The baseline characteristics of the study subjects are summarized in Table 1. A total of 34 patients with ABS were enrolled and were predominantly male (n = 29, 85.3%) with a median age of 58 years (interquartile range [IQR 52–64.3]). The most common indication of LT was liver cirrhosis (n = 18, 52.9%). The median interval from LT to stricture appearance was 7.12 months (IQR 2–91.3). ABS developed within the first year in 21 patients (61.8%). All patients had been treated endoscopically using multiple plastic stent placement prior to FCSEMS placement. The median interval from LT to metal stent placement was 41.5 months (IQR 13.1–123.5).
Clinical outcomes
The clinical outcomes of the study population are presented in Table 2. Technical success was achieved in all cases (100%). Twenty-one patients (61.8%) underwent suprapapillary stent placement and the remaining 13 patients (38.2%) underwent transpapillary stent placement. The median stent placement duration was 3.1 months (IQR 2.7–6.1). A stone was identified in 16 patients (47.1%) at the time of stent removal. All bile duct stones were removed by balloon catheter and basket. Stricture resolution was achieved in 26 patients (clinical success: 76.5%, 95% confidence interval 62–91) (Fig. 2). Stent removal was successful in all patients. In 8 patients who did not achieve clinical success, stricture resolution failed due to a refractory stricture (n = 5) or early distal stent migration (n = 3). In those five cases with a refractory stricture (14.7%), a regular stent exchange was performed (MPS, n = 3; FCSEMS, n = 2).
Placement of a modified fully covered self-expandable metal stent (FCSEMS) for treating refractory strictures. A Cholangiogram showing an anastomotic biliary stricture, B Multiple plastic stent placements were maintained at 3-month intervals for 2 years, C Cholangiogram showing a refractory stricture, D FCSEMS insertion into the stricture site, E Cholangiogram demonstrating resolution of the anastomotic stricture
Early adverse events developed in 3 patients (8.8%), including distal stent migration. These patients underwent MPS placement due to persistent ABS. After MPS placement, stricture resolution was achieved.
Late adverse events occurred in 9 patients (26.5%), including cholangitis (n = 7, 20.6%) and asymptomatic distal stent migration (n = 2, 5.9%). Among 7 patients with acute cholangitis due to stent occlusion, 6 underwent FCSEMS placement after stent removal and one did not receive any stent placement owing to improvement in the ABS. The two patients with asymptomatic distal stent migration did not undergo stent placement due to improvement of ABS.
The median follow-up period was 57.9 months (IQR 51.9–64.3). Stricture recurrence occurred in 3 of 26 patients who achieved clinical success (11.5%) at 7, 8.6, and 15.8 months after FCSEMS removal, respectively (Fig. 3). Two patients received a further FCSEMS placement and the remaining patient underwent percutaneous transhepatic biliary drainage. Stricture resolution was achieved in all of these patients with recurrent ABS.
Comparison of clinical outcomes according to stent placement type
Twenty-one patients (61.8%) underwent suprapapillary stent placement and the remaining 13 cases (38.2%) underwent transpapillary stent placement (Table 3). Subgroup analysis revealed that the clinical success rate was not statistically different between these two groups (suprapapillary stent placement: 14/21, 66.7% vs. transpapillary stent placement: 12/13, 92.3%, P = 0.218). The early adverse event rate (suprapapillary stent placement: 2/21, 9.5% vs. transpapillary stent placement: 1/13, 7.7%, P = 0.857) and late adverse event rate (suprapapillary stent placement: 7/21, 33.3% vs. transpapillary stent placement: 2/13, 15.4%, P = 0.256) also showed no statistical differences. The stricture recurrence rate was also not different between the groups (suprapapillary stent placement: 1/14, 7.1% vs. transpapillary stent placement: 2/12, 16.7%, P = 0.705).
Discussion
We here evaluated the clinical outcomes of an FCSEMS placement for the management of refractory ABS after the failure of prior MPS placement. Our results suggest that an FCSEMS placement for ABS shows an effective and reasonable safety profile in patients with refractory strictures. The stricture resolution was maintained in 67.6% of our present study patients by the end of follow-up (median 57.9 months). To best of our knowledge, our current study incorporated the longest follow-up duration to date for evaluating the efficacy and safety of FCSEMS placement in LDLT patients with refractory strictures.
In our present study, technical success was achieved in all patients and stricture resolution was achieved in 76.5% of cases. As in previous reports, FCSEMS placement in strictures after DDLT (85–90%) showed a better stricture resolution that after LDLT (58–76%) [21, 22]. Our current results revealed similar clinical outcomes to those in previous reports of patients who underwent LDLT. These lower stricture resolutions in LDLT are due to the small-caliber, multiple and complex fibrotic anastomoses, and hypertrophy of the transplanted liver [23]. In a recent study by Jang et al., stricture resolution was achieved for all post-LDLT strictures [17]. The patients in that study underwent FCSEMS placement as their initial treatment, or after receiving endoscopic or percutaneous treatment for less than 3 months. On the other hand, refractory patients without stricture resolution or recurrence after receiving MPS placement for at least 1 year were included in our current study. It seems that these cohort differences may have affected the stricture resolution outcomes. It remains unclear whether FCSEMS placement should be used as initial treatment for ABS, rather than MPS placement. FCSEMSs may be beneficial for patients refractory to MPS treatment. According to our present results and higher stricture resolution rate of previous reports, therefore, FCSEMS placement can be considered a viable initial treatment before entering the refractory phase.
Suprapapillary stent placement has recently been used to extend stent patency by preventing duodenobiliary reflux [18]. Theoretically, placing the distal end of the stent in the bile duct may reduce duodenobiliary reflux [24]. Several studies have shown that suprapapillary stent placement seems to be effective to prolong stent patency, but robust evidence is still lacking [17, 18, 24]. In addition, recent studies have reported no significant difference between suprapapillary and transpapillary stent placement in metal stents with regard to stent patency [25, 26]. In this present study, the stricture resolution rate was comparable between the suprapapillary and transpapillary placement groups. However, the number of cases in each group is too small to conclusively determine that the two methods yield comparable results. In addition, previous reports have suggested that avoiding endoscopic sphincterotomy (EST) may reduce duodenobiliary reflux [24, 27]. All of our current study subjects received EST in past MPS placement which may have affected these outcomes.
In the present patient population, the overall stent migration rate was 14.7% of patients (n = 3, early migration; n = 2, late migration), which is similar to the 10–16% range described in previous reports [13, 22, 28,29,30,31]. Stent migration is one of the major drawbacks for FCSEMS placement and an intraductal FCSEMS with a central waist has recently been developed to prevent migration. The migration rate of an intraductal FCSEMS has been reported at 0–6.4% [15,16,17,18, 32]. Compared to previous studies, stent migration was higher among the current patients. It is possible that both conventional and intraductal FCSEMS was included in our present cohort. In addition, all of our study subjects had already received endoscopic treatment, and thus already had been partially treated, which has been shown previously to increase the risk of migration [33].
One of the main concerns with FCSEMS placement is the risk of occlusion of secondary branch ducts, which induces cholangitis [32]. The margin of the FCSEMS ends may also be associated with turbulent bile flow, which will cause sludge formation [32]. In a recent study, an additional plastic stent placement was performed into the side branch duct prior to FCSEMS placement to prevent occlusion of the side branch duct [15]. In this present study, bile duct stones were identified in 47.1% of the patients at the time of stent removal. Furthermore, cholangitis without abscess formation due to stent occlusion developed in 20.6% of the present study population. In recent meta-analyses, adverse events, including cholangitis and stent migration was statistically similar between FCSEMS placement and multiple plastic stent placement [34, 35]. Stones may contribute to the development of cholestasis or cholangitis. Modifications of the stent structure are thus needed to improve bile flow within the FCSEMS and thereby reduce the risk of stone or sludge formation. In addition, placing an additional plastic stent into the side-branch duct prior to inserting the FCSEMS could help in preventing the blockage of the latter duct.
Stricture recurrence was observed in 11.5% of the present study patients during a median 57.9 months of follow-up with a median stent placement duration of 3.1 months (IQR 2.7–6.1). Previous reports have demonstrated that a short duration stent placement may increase the rate of recurrence [13, 36]. In a recent systemic review, the stricture resolution rate was reported to be higher in patients in whom the stent was maintained for more than 3 months [28]. These results emphasize the impact of the duration of FCEMS placement. Although a longer FCSEMS placement duration may improve stricture resolution and lower stricture recurrence, it could also increase the chance of stent-related adverse events, including migration or occlusion as a trade-off. These trade-offs should be factored into the decision to use FCSEMS. To date, the appropriate stent placement duration of FCSEMS in patients with ABS is still unclear and further studies are needed. Current guidelines recommend a 6-month duration of FCEMS placement for benign biliary strictures [37]. Based on our results and previous results, a 6-month duration of FCEMS placement may be helpful for management of ABS [34, 37].
This study had several limitations. First, the analyses were retrospective and involved patients from a single tertiary center. The sample size was also small, making it difficult to generalize the efficacy of the FCSEMS placement in patients with refractory ABS after LDLT. In addition, the stent placement duration for the FCSEMS was three months, which may negatively affect the recurrence rate. Further large scale prospective studies are necessary to evaluate the most effective stent placement duration of FCSEMS to resolve an ABS and reduce the recurrence rate of post-LT ABS.
In conclusion, an FCSEMS placement shows favorable long-term outcomes in patients with refractory ABS, especially those due to a failure of MPS placement. The duration of FCSEMS placement should be further investigated, however. Further large, randomized, prospective studies are required to confirm the efficacy of FCSEMS placement.
Abbreviations
- LT:
-
Liver transplantation
- ABS:
-
Anastomotic biliary stricture
- NABS:
-
Non-anastomotic biliary stricture
- ERC:
-
Endoscopic retrograde cholangiography
- FCSEMS:
-
Fully covered self-expanding metal stent
References
Halliday N, Westbrook RH (2017) Liver transplantation: need, indications, patient selection and pre-transplant care. Br J Hosp Med (Lond) 78:252–259
Akamatsu N, Sugawara Y, Hashimoto D (2011) Biliary reconstruction, its complications and management of biliary complications after adult liver transplantation: a systematic review of the incidence, risk factors and outcome. Transpl Int 24:379–392
Sharma S, Gurakar A, Jabbour N (2008) Biliary strictures following liver transplantation: past, present and preventive strategies. Liver Transpl 14:759–769
Williams ED, Draganov PV (2009) Endoscopic management of biliary strictures after liver transplantation. World J Gastroenterol 15:3725–3733
Tarantino I, Traina M, Mocciaro F, Barresi L, Curcio G, Di Pisa M, Granata A, Volpes R, Gridelli B (2012) Fully covered metallic stents in biliary stenosis after orthotopic liver transplantation. Endoscopy 44:246–250
Jimenez-Perez M, Melgar Simon JM, Duran Campos A, Gonzalez Grande R, Rodrigo Lopez JM, Manteca Gonzalez R (2016) Endoscopic management of post-liver transplantation biliary strictures with the use of fully covered metallic stents. Transplant Proc 48:2510–2514
Costamagna G, Tringali A, Mutignani M, Perri V, Spada C, Pandolfi M, Galasso D (2010) Endotherapy of postoperative biliary strictures with multiple stents: results after more than 10 years of follow-up. Gastrointest Endosc 72:551–557
Tabibian JH, Asham EH, Han S, Saab S, Tong MJ, Goldstein L, Busuttil RW, Durazo FA (2010) Endoscopic treatment of postorthotopic liver transplantation anastomotic biliary strictures with maximal stent therapy (with video). Gastrointest Endosc 71:505–512
Dumonceau JM, Tringali A, Blero D, Deviere J, Laugiers R, Heresbach D, Costamagna G (2012) Biliary stenting: indications, choice of stents and results: European society of gastrointestinal endoscopy (ESGE) clinical guideline. Endoscopy 44:277–298
Poley JW, Lekkerkerker MN, Metselaar HJ, Kuipers EJ, Bruno MJ (2013) Clinical outcome of progressive stenting in patients with anastomotic strictures after orthotopic liver transplantation. Endoscopy 45:567–570
Pasha SF, Harrison ME, Das A, Nguyen CC, Vargas HE, Balan V, Byrne TJ, Douglas DD, Mulligan DC (2007) Endoscopic treatment of anastomotic biliary strictures after deceased donor liver transplantation: outcomes after maximal stent therapy. Gastrointest Endosc 66:44–51
Bordacahar B, Perdigao F, Leblanc S, Barret M, Duchmann JC, Guillaumot MA, Chaussade S, Scatton O, Prat F (2018) Clinical efficacy of anti-migration features in fully covered metallic stents for anastomotic biliary strictures after liver transplantation: comparison of conventional and anti-migration stents. Gastrointest Endosc 88:655–664
Martins FP, De Paulo GA, Contini MLC, Ferrari AP (2018) Metal versus plastic stents for anastomotic biliary strictures after liver transplantation: a randomized controlled trial. Gastrointest Endosc 87:131–140
Tal AO, Finkelmeier F, Filmann N, Kylanpaa L, Udd M, Parzanese I, Cantu P, Dechene A, Penndorf V, Schnitzbauer A, Friedrich-Rust M, Zeuzem S, Albert JG (2017) Multiple plastic stents versus covered metal stent for treatment of anastomotic biliary strictures after liver transplantation: a prospective, randomized, multicenter trial. Gastrointest Endosc 86:1038–1045
Jang SI, Sung SY, Park H, Lee KH, Joo SM, Lee DK (2017) Salvage therapy using self-expandable metal stents for recalcitrant anastomotic strictures after living-donor liver transplantation. Therap Adv Gastroenterol 10:297–309
Sato T, Kogure H, Nakai Y, Ishigaki K, Hakuta R, Saito K, Saito T, Takahara N, Hamada T, Mizuno S, Tada M, Isayama H, Koike K (2020) A prospective study of fully covered metal stents for different types of refractory benign biliary strictures. Endoscopy 52:368–376
Jang SI, Chung TR, Cho JH, Lee KH, Joo SM, Choi JH, Kim SI, Lee DK (2021) Short fully covered self-expandable metal stent for treatment of proximal anastomotic benign biliary stricture after living-donor liver transplantation. Dig Endosc 33:840–848
Choi HJ, Moon JH, Lee YN, Kim HS, Choi MH, Lee TH, Cha SW, Cho YD, Park SH, Kim SJ (2016) Evaluation of a newly modified nonflared fully covered metal stent, 12 mm in diameter, for intraductal placement in patients with malignant biliary strictures: a feasibility study. Endoscopy 48:625–631
Lee TH, Jung MK, Kim TK, Pack CG, Park YK, Kim SO, Park DH (2019) Safety and efficacy of a metal stent covered with a silicone membrane containing integrated silver particles in preventing biofilm and sludge formation in endoscopic drainage of malignant biliary obstruction: a phase 2 pilot study. Gastrointest Endosc 90:663–672
Cotton PB, Eisen GM, Aabakken L, Baron TH, Hutter MM, Jacobson BC, Mergener K, Nemcek A Jr, Petersen BT, Petrini JL, Pike IM, Rabeneck L, Romagnuolo J, Vargo JJ (2010) A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc 71:446–454
Shah SA, Grant DR, McGilvray ID, Greig PD, Selzner M, Lilly LB, Girgrah N, Levy GA, Cattral MS (2007) Biliary strictures in 130 consecutive right lobe living donor liver transplant recipients: results of a Western center. Am J Transplant 7:161–167
Kato H, Kawamoto H, Tsutsumi K, Harada R, Fujii M, Hirao K, Kurihara N, Mizuno O, Ishida E, Ogawa T, Fukatsu H, Yamamoto K, Yagi T (2009) Long-term outcomes of endoscopic management for biliary strictures after living donor liver transplantation with duct-to-duct reconstruction. Transpl Int 22:914–921
Wang SF, Huang ZY, Chen XP (2011) Biliary complications after living donor liver transplantation. Liver Transpl 17:1127–1136
Inoue T, Suzuki Y, Okumura F, Naitoh I, Sano H, Ibusuki M, Kitano R, Kobayashi Y, Ito K, Yoneda M (2020) Intraductal placement of a fully covered metal stent with a long string for distal malignant biliary obstruction without endoscopic sphincterotomy: prospective multi-center feasibility study. Dig Endosc 32:949–956
Kovacs N, Pecsi D, Sipos Z, Farkas N, Foldi M, Hegyi P, Bajor J, Eross B, Marta K, Miko A, Rakonczay Z Jr, Sarlos P, Abraham S, Vincze A (2023) Suprapapillary biliary stents have longer patency times than transpapillary stents-a systematic review and meta-analysis. J Clin Med 12:898
Kanno Y, Ito K, Nakahara K, Kawaguchi S, Masaki Y, Okuzono T, Kato H, Kuwatani M, Ishii S, Murabayashi T, Hasegawa S, Nagahama M, Iwashita Y, Michikawa Y, Terada S, Kawakami Y, Fujii Y, Kawakubo K (2023) Suprapapillary placement of plastic versus metal stents for malignant biliary hilar obstructions: a multicenter, randomized trial. Gastrointest Endosc 98:211–221
Mangiavillano B, Montale A, Frazzoni L, Bianchetti M, Sethi A, Repici A, Fuccio L (2019) Endoscopic biliary self-expandable metallic stent in malignant biliary obstruction with or without sphincterotomy: systematic review and meta-analysis. Endosc Int Open 7:E26-35
Kao D, Zepeda-Gomez S, Tandon P, Bain VG (2013) Managing the post-liver transplantation anastomotic biliary stricture: multiple plastic versus metal stents: a systematic review. Gastrointest Endosc 77:679–691
Graziadei IW, Schwaighofer H, Koch R, Nachbaur K, Koenigsrainer A, Margreiter R, Vogel W (2006) Long-term outcome of endoscopic treatment of biliary strictures after liver transplantation. Liver Transpl 12:718–725
Gomez CM, Dumonceau JM, Marcolongo M, de Santibanes E, Ciardullo M, Pekolj J, Palavecino M, Gadano A, Davolos J (2009) Endoscopic management of biliary complications after adult living-donor versus deceased-donor liver transplantation. Transplantation 88:1280–1285
Chok KS, Chan SC, Cheung TT, Sharr WW, Chan AC, Fan ST, Lo CM (2014) A retrospective study on risk factors associated with failed endoscopic treatment of biliary anastomotic stricture after right-lobe living donor liver transplantation with duct-to-duct anastomosis. Ann Surg 259:767–772
Kaffes A, Griffin S, Vaughan R, James M, Chua T, Tee H, Dinesen L, Corte C, Gill R (2014) A randomized trial of a fully covered self-expandable metallic stent versus plastic stents in anastomotic biliary strictures after liver transplantation. Therap Adv Gastroenterol 7:64–71
Das R, Slivka A (2020) Fully covered metal stents versus plastic stents: the new kid on the block or the old standby? Gastrointest Endosc 92:1225–1227
Khan MA, Baron TH, Kamal F, Ali B, Nollan R, Ismail MK, Tombazzi C, Artifon ELA, Repici A, Khashab MA (2017) Efficacy of self-expandable metal stents in management of benign biliary strictures and comparison with multiple plastic stents: a meta-analysis. Endoscopy 49:682–694
Visconti TAC, Bernardo WM, Moura DTH, Moura ETH, Gonçalves CVT, Farias GF, Guedes HG, Ribeiro IB, Franzini TP, Luz GO, Dos Santos M, de Moura EGH (2018) Metallic vs plastic stents to treat biliary stricture after liver transplantation: a systematic review and meta-analysis based on randomized trials. Endosc Int Open 6:E914-e923
Cantu P, Tenca A, Parzanese I, Penagini R (2016) Covered metal stents in endoscopic therapy of biliary complications after liver transplantation. Dig Liver Dis 48:836–842
Dumonceau JM, Tringali A, Papanikolaou IS, Blero D, Mangiavillano B, Schmidt A, Vanbiervliet G, Costamagna G, Devière J, García-Cano J, Gyökeres T, Hassan C, Prat F, Siersema PD, van Hooft JE (2018) Endoscopic biliary stenting: indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline - Updated October 2017. Endoscopy 50:910–930
Author information
Authors and Affiliations
Contributions
Conception and design, DO; analysis and interpretation of the data: SHC, HSL, GH, DO, TJS, DWS, and SKL; drafting of the article: SHC, HSL and DO; critical revision of the manuscript for important intellectual content, DO; statistical analysis, SHC and, DO; supervision, DO; Final approval of the article, DO.
Corresponding author
Ethics declarations
Conflict of interest
Sung Hyun Cho, Ho Seung Lee, Gunn Huh, Dongwook Oh, Tae Jun Song, Dong-Wan Seo, and Sung Koo Lee have no conflicts of interest or financial ties to disclose. The authors have no conflicts of interest or financial relationships relevant to this publication to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cho, S.H., Lee, H.S., Huh, G. et al. Long-term outcomes of fully covered self-expandable metal stents for refractory biliary strictures after living donor liver transplantation: a retrospective study at a tertiary center. Surg Endosc 38, 3223–3230 (2024). https://doi.org/10.1007/s00464-024-10837-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-024-10837-4