Abstract
Introduction
It is still unclear whether enhanced recovery programs (ERPs) reduce postoperative morbidity after liver surgery. This study investigated the effect on liver surgery outcomes of labeling as a reference center for ERP.
Materials and methods
Perioperative data from 75 consecutive patients who underwent hepatectomy in our institution after implementation and labeling of our ERP were retrospectively compared to 75 patients managed before ERP. Length of hospital stay, postoperative complications, and adherence to protocol were examined.
Results
Patient demographics, comorbidities, and intraoperative data were similar in the two groups. Our ERP resulted in shorter length of stay (3 days [1–6] vs. 4 days [2–7.5], p = 0.03) and fewer postoperative complications (24% vs. 45.3%, p = 0.0067). This reduction in postoperative morbidity can be attributed exclusively to a lower rate of minor complications (Clavien-dindo grade < IIIa), and in particular to a lower rate of postoperative ileus, after labeling. (5.3% vs. 25.3%, p = 0.0019). Other medical and surgical complications were not significantly reduced. Adherence to protocol improved after labeling (17 [16–18] vs. 14 [13–16] items, p < 0.001).
Conclusions
The application of a labeled enhanced recovery program for liver surgery was associated with a significant shortening of hospital stay and a halving of postoperative morbidity, mainly ileus.
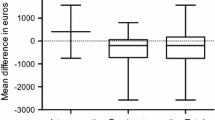
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Enhanced recovery after surgery programs (ERPs) form a multidisciplinary, multimodal approach designed to control the surgical stress response and hasten postoperative recovery [1]. ERPs reduce the incidence of postoperative morbidity and length of hospital stay (LOS) in colorectal surgery [2]. First developed for this type of surgery, ERPs have been applied to several other surgical specialties and procedures with similar benefits [3]. Drawing on the guidelines for ERPs in colorectal surgery, specific recommendations for perioperative care in liver surgery have been developed considering the differences between liver and colorectal surgeries [4]. Recent meta-analyses demonstrate that ERPs for liver surgery are associated with shorter LOS [5,6,7]. However, the existing literature on the impact of ERPs on postoperative morbidity in liver surgery is inconclusive [8]. Meta-analyses suggest that ERPs may be specifically associated with lower complication rates in laparoscopic liver resection [9], but less clearly when liver surgery is performed through laparotomy [10, 11]. Furthermore, in the existing literature, ERP protocols also vary widely among studies, patients are often selected to be eligible for ERPs, and actual adherence to each ERP items is seldom documented [4,5,6,7,8,9,10,11].
An ERP for colorectal surgery was progressively introduced in the early 2000s in the Department of Abdominal Surgery at the Liege University Hospital in Belgium [12] and has been formally applied as a standard labeled program for all colorectal surgery patients since 2015, regardless of comorbidities, surgical approach, indication, or site [13]. Although no specific protocol had been developed for liver surgery at that time, since then, the perioperative management of patients scheduled for liver surgery was indirectly influenced by colorectal patient care.
In a preliminary unpublished study, the authors compared the data of 49 consecutive patients who underwent elective liver surgery in 2015 (when our formal ERP for colorectal surgery began) with the data of 50 consecutive patients scheduled for elective liver surgery in 2020, just prior to the implementation of a formal ERP in hepatic surgery. There were more laparoscopic hepatectomies in 2020 than in 2015 (69.1% vs. 44.9%, respectively, p = 0.018). The median length of stay (LOS) was significantly shorter in 2020 (4 [2–8] days) than in 2015 (9 [3–12] days) (p = 0.004). There were no significant differences in overall postoperative complications (43.6% vs. 53.1% in 2020 and 2015 respectively, p = 0.50), medical complications (25.5% vs. 30.6%, respectively, p = 0.56), surgical complications (40% vs. 42.9%, respectively, p = 0.77), or ileus (21.8% vs. 28.6%, respectively, p = 0.43).
Formal specific pathways and the complete enhanced recovery protocol designed for liver surgery were finally implemented in December 2020, and the Liege University Hospital was labeled as a reference medical center for ERP in liver surgery by the “Groupe Francophone pour la Réhabilitation Améliorée après Chirurgie” (GRACE, Beaumont, France; www.grace-asso.fr) in 2021. Here we assessed to what degree an institutionalized ERP for liver surgery and of the labeling of our center shortened length of hospital stay and reduced postoperative morbidity.
Material and methods
Patients
After approval by the Institutional Ethics Committee of the Liege University Hospital (Comité d’Ethique Hospitalo-Facultaire Universitaire de Liège, Belgium; President: Prof. V. Seutin; IRB number: 707; internal reference: 2022/121), the authors retrospectively analyzed and compared the data of the first 75 consecutive patients scheduled for liver surgery after implementing ERP for liver surgery (ERP group) at the Liege University Hospital and of the last 75 consecutive patients who underwent elective liver surgery before ERP for liver surgery was implemented (no enhanced recovery program group; NERP group). All 75 patients from the ERP group were managed with the same ERP protocol, regardless of their age, comorbidities, surgical approach, and type and indication of liver surgery. Data were prospectively uploaded in the GRACE audit database. Data and database entries were monitored by G.T. and J.J. This study was conducted and reported in accordance with the STROBE Checklist.
Perioperative management
The formalized, consensual protocol was edited for anesthesia management, surgical procedures, and perioperative care. This protocol drew on our colorectal surgery protocol [13] and was adapted for liver surgery. The ERP comprised 21 items consisting of pre-, intra-, and post-operative measures. Information and training sessions for paramedical staff were organized. An anesthesiologist gave the patients oral information at the time of the preoperative visit. An information brochure was provided to the patients, explaining perioperative optimization and management, enhanced recovery pathways, and the importance of patient involvement. The ERP protocol included the following items:
-
Fasting was as short as possible, aiming for 6 h for food and 2 h for clear fluids.
-
A preoperative carbohydrate load was given 2 h before induction of anesthesia (except in case of insulin-requiring diabetes mellitus or known gastroparesis).
-
Preoperative oral immunonutrition or nutrition therapy was prescribed to patients with preoperative malnutrition.
-
No sedative premedication was administered.
-
Antibioprophylaxis was started before surgery and followed guidelines.
-
Active prevention of perioperative hypothermia was applied.
-
A laparoscopic approach was always preferred, when possible.
-
Multimodal analgesia was performed intra-and post-operatively, combining the use of locoregional techniques with systemic analgesia. Epidural analgesia was not used even in laparotomy cases. Patients sometimes received intrathecal morphine (0.3 mg) in cases of laparotomy and absence of coagulation disorders.
-
A bilateral subcostal transversus abdominis plane (TAP) block (40 ml of 0.375% levobupivacaine, containing epinephrine at a 1:200,000 ratio) was used in all patients.
-
A continuous intravenous infusion of lidocaine and ketamine was administered intraoperatively (2 mg kg h−1 of lidocaine and 0.1 mg kg h−1 of ketamine, 45 min after the TAP block) and prolonged postoperatively (1 mg kg h−1 of lidocaine and 0.05 mg kg h−1 of ketamine) unless contra-indicated (renal failure, epilepsy, second- and third-degree atrio-ventricular blocks, major liver resection potentially resulting in reduced clearance of lidocaine).
-
Use of dexamethasone was systematic in the absence of uncontrolled insulino-requiring diabetes.
-
Use of non-steroidal anti-inflammatory drugs (NSAIDs) was systematic in the absence of contraindications (renal failure, ischemic cardiopathy, peptic ulcer).
-
Intravenous fluids and norepinephrine were titrated using a goal-directed therapy (Variations of systolic and pulsatile pressure estimated using Carescape Monitor™ B850 2013, GE HealthCare or Clearsight® 2021 Edwards Lifesciences Corporation).
-
Prevention of postoperative nausea and vomiting combined the effect of dexamethasone and 4 mg of ondansetron or 0.625 mg of dehydrobenzperidol if necessary.
-
No prophylactic abdominal drains were placed.
-
Systematically, a nasogastric tubes and urinary catheters were either not used or withdrawn at the end of surgery.
-
Thromboprophylaxis was performed using intra-operative pneumatic compression stockings and low-molecular-weight heparin was prescribed as soon as possible after surgery.
-
Early mobilization with the help of a physiotherapist and early feeding were started within the first 24 h postoperative.
Besides ERP items, glycemia was monitored and maintained below 200 mg dl−1 using intravenous insulin, if necessary, from the intraoperative period particularly in case of repeated vascular clamping [14]. Finally, an intraoperative protective ventilation strategy (tidal volume = 6–7 ml kg−1 of ideal body weight) was used with no or minimal end-expiratory pressure during the dissection phase to reduce bleeding. The respiratory rate was adjusted to maintain an arterial CO2 partial pressure < 45 mmHg.
Endpoints
The primary endpoints were the overall postoperative complication rate 30 days after surgery. Postoperative complications were described according to the European Perioperative Clinical Outcome Definitions [15]. Complications were also rated following Clavien-Dindo classification.
Secondary endpoints were LOS and adherence to ERP (number of protocol items that were adhered to), adherence to postoperative items of ERP (number of postoperative items from the ERP that were adhered to, since a major effect of these items on optimal recovery is attested [16]), and postoperative medical and surgical complications (parietal complications, intra-abdominal complications, redo surgery) including ileus (defined as the absence of flatus or feces during the first 72 h postoperatively). Time of readiness for discharge (TRD) was also recorded. The criteria for discharge were tolerance of feeding, flatus, pain amenable to oral analgesics, mobilization, and ambulation without assistance. Incidence of postoperative nausea and vomiting, unplanned hospital readmission, and 30-day and 90-day mortality were also recorded.
The variables retrospectively retrieved from the prospective database (ERP group) and the medical records of all patients were age, weight, height, preoperative comorbidities, surgical approach (laparotomy vs. laparoscopy), type of surgery (minor or major hepatectomy), and indication for surgery (primary cancer, metastasis, cyst, or echinococcus).
Statistical analysis
Descriptive analyses were performed by group for all the variables collected. The normality of distribution for quantitative variables was numerically assessed by comparing the value of the mean and the value of the median, and graphically using the histogram and quantile–quantile plot as well as using the Shapiro–Wilk normality test. Data are presented as mean (SD) or median [interquartile range] and were analyzed using Student’s t test or the Mann–Whitney U test for parametric and non-parametric variables, respectively. Proportions were analyzed using Chi-squared tests or Fisher’s exact tests and are presented as percentages (%). Sequential univariate and multivariate binary logistic regression modeling of the risk of developing an ileus as a function of each item of the improved recovery protocol was performed. The items that showed a statistically significant relationship in the univariate analyses were included in the final model.
As the complication rate before ERP labeling was approximately 45%, we ran a sample size calculation (using G*Power, version 3.1.9.2, Franz Faul, Universität Kiel, Germany) and estimated that 75 patients per group would allow the detection of a 50% reduction in postoperative complications after ERP implementation at an alpha level of 0.05, with 80% power. This 50% reduction in postoperative morbidity was expected from a meta-analysis published in Journal of Visceral Surgery in 2019 [7]. All statistical analyses were performed on all available data, and missing data were not replaced (between-subject design). All analyses were performed using SAS version 9.4 for Windows (SAS Institute Inc., Cary, USA).
Results
Patients and surgery characteristics
There were no differences in demographic characteristics, indications for liver surgery (Table 1), or preoperative risk factors (Table 2) between groups. Table 3 shows the operative data. More tranexamic acid was administered in the ERP group (p = 0.0019). However, large (> 500 ml) intraoperative blood loss or the need for transfusion during hospitalization were similar in the two groups (p > 0.05). Fewer patients in the ERP group had to stay overnight in the post-anesthesia care unit (p = 0.0002).
Primary outcome
The implementation of a labeled ERP resulted in a 53% reduction in postoperative morbidity (24% vs. 45.3%, respectively after and before labeling (p = 0.0067) (Table 4).
There were significantly fewer minor complications, i.e. Clavien-Dindo grade < IIIa (9.3% in the ERP group vs. 29.3% in the NERP group, p = 0.002) in the ERP group. More particularly, the Clavien-Dindo grade II complications were less in the ERP group (6.7% in the ERP group vs. 13.3% in the NERP group, p = 0.001). On the other hand, there were no significant differences between the two groups for major complications, i.e. Clavien-Dindo grade ≥ IIIa.
Secondary outcomes
ERP labeling significantly shortened LOS (ERP: 3 days [1–6] vs. NERP: 4 days [2–7.5], p = 0.03) and TRD (ERP: 2 days [1–4] vs. NERP: 3 days [1–7], p < 0.001).
Overall adherence to ERP items, meaning adherence to the 21 ERP items from our institutional protocol, and adherence to the 7 postoperative items, assessed as medians, were better in the ERP group than in the NERP group (p < 0.001, Table 5). More patients in the ERP group received preoperative information on ERP (p < 0.0001) and nutritional support (p = 0.014) and were given a preoperative carbohydrate load (p = 0.0037). Intravenous crystalloid infusions were stopped earlier in the ERP group (2 days [1, 2]) than in the NERP group (2 days [2–5]) (p < 0.0001). More patients in the ERP group had early mobilization within the first 24 postoperative hours (p < 0.0001) as well as early feeding (p < 0.0001). Intraoperative NSAIDs were given to more patients in the ERP group (p = 0.0001). Postoperative surgical drains were avoided significantly more often in the ERP group (p = 0.024). Similarly, more patients in the ERP group had their bladder catheter removed at the end of the procedure (p < 0.0001).
Details on the incidence of each possible complication are given in the Supplementary materials (Supplementary Material 1). Rate of ileus was significantly lower after labeling (5.3 and 25.3% in the ERP and NERP group, respectively; p = 0.0019). The rates of other medical and surgical complications were not significantly different between the groups, although atelectasis was less frequent in the ERP group (p = 0.05).
The risks of readmission to the hospital on the 30 or 90 postoperative day, unscheduled consultation within 3 months postoperatively or redo surgery were not significantly affected by ERP (Supplementary Material 1). Death rates within 30 and 90 days after surgery were comparable in the two groups (Supplementary Material 1).
Discussion
This study found that labeling as a reference center by GRACE, which involves meeting a set of requirements for ERP assessment, improved the implementation of the ERP protocol for liver surgery and halved overall postoperative complications. The incidence of postoperative ileus was most markedly decreased. It also hastened TRD and shortened LOS. These benefits were observed despite the absence of patient selection.
To the best of our knowledge, this is the first study demonstrating the impact of labeling as a reference center for ERP after liver surgery since the publication of the ERAS® Society (Enhanced Recovery After Surgery Society; erassociety.org) guidelines in 2016 [4].
We report a halving of postoperative complications associated with implementing our enhanced recovery program, although the rate of complications in the NERP group was in the range reported in studies using ERP [17]. The benefit of ERP for liver surgery on postoperative outcomes remains controversial [18]. A recent meta-analysis described positive effects of ERP on postoperative outcomes in liver surgery [19]. Conflicting findings may result from patient selection, surgical approach (laparoscopy vs. laparotomy), ERP protocol and adherence to protocol.
In this study, all patients scheduled for elective liver surgery were managed with the same ERP regardless of age, comorbidities, surgical approach (laparoscopic or open surgery), surgical indication (cancer or not), and size of hepatic resection (major or minor hepatectomy).
Recently, the EuroPOWER international observational study reported that treating complications in a self-declared ERAS center did not improve outcome after colorectal surgery [20]. However, increased adherence to the ERAS® pathway is associated with a significant reduction in overall postoperative complications. Interestingly, management of our liver surgery patients in the spirit of ERP but without an actual institutional protocol shortened LOS, but with no impact on the rate of postoperative complications. The implementation of our ERP and our labeling resulted in improved adherence to the items of the protocol. Adherence to the postoperative items of the protocol, considered critically important for optimal recovery [16], was also better. Moreover, adherence of our patients to ERP was greater than in other reports from large series of patients [5, 19]. Our findings suggest that the reduction in postoperative complications observed in our study was due to the high adherence rates in our ERP patients. We should not rely on key factors such as the use of laparoscopy, but rather on the whole protocol, as described in previous ERP studies [20, 21]. Between 2015 and 2020, we increased the use of laparoscopy from 50 to 70%, but with no benefit on postoperative outcomes. Taken overall, our data confirm that the protocol alone is not enough to ensure efficient patient management [22].
The beneficial impact of ERP on postoperative complication after colorectal surgery mainly concerns medical rather than surgical complications [2]. We observed a near-significant (p = 0.055) reduction in postoperative pulmonary complications and a significant reduction in postoperative atelectasis (p = 0.05) in the ERP group. Our study was probably not powerful enough to specifically detect a significant reduction in medical complications. Among postoperative complications, we observed a marked reduction in the incidence of postoperative ileus. The beneficial impact on postoperative ileus is probably multifactorial: greater use of laparoscopy [23], early mobilization and feeding [24], opioid-sparing multimodal analgesia [25], and the use of NSAIDs [26]. We compared patients who experienced postoperative ileus with those who did not, with the aim of identifying ERP items that may have influenced the risk of postoperative ileus. Statistical results are consistent with the literature and are available in the Supplementary materials (Supplementary Material 2), but the infrequent occurrence of ileus and our sample size prevented us from trying to determine factors responsible for its reduced incidence.
This study also confirms that an ERP for hepatic surgery can produce a significant reduction in LOS [27]. The duration of hospitalization after liver surgery had already been reduced by 4 days to 5 days in our institution between 2015 and 2020, despite the lack of any formal institutional ERP for liver surgery. The perioperative management of patients scheduled for liver resection had been indirectly influenced by colorectal patient care managed with an ERP since 2016 [12, 13]. The proportion of laparoscopic liver surgeries significantly increased between 2015 and 2020, with a significant effect on LOS, as described in the literature [28]. However, there was no decrease in postoperative morbidity. Nevertheless, formal implementation of our ERP for liver surgery associated with our labeling as reference center, which implies internal and external audits, optimized the adherence of our patients to the ERP, thereby accelerating patient TRD and further shortening LOS.
Our study has some limitations. First, although the analyzed data of the ERP group were prospectively collected and entered in our GRACE database, the study remains a retrospective one. No selection was carried out and all the patients undergoing elective liver surgery were included. Second, the data from the control group (before labeling) were retrospectively retrieved from the medical records fully digitized since the end of the 2010s. Although length of hospital stay is systematically recorded, some complications may be missing. Third, there were more cases of liver fibrosis in the ERP post-labeling group, known to increase the risk of postoperative complications. Differences in postoperative complications might be even greater without these limitations.
For conclusion, this study shows that implementation of an institutional ERP in liver surgery associated with the requirements imposed for labeling as a reference center shortened LOS and decreased postoperative morbidity, mainly postoperative ileus. Our observations point to a marked impact of adherence to the protocol on improving postoperative outcomes.
Data availability
Research data supporting this publication are available on demand to the authors.
Abbreviations
- ASA:
-
American Society of Anesthesiologists.
- BMI:
-
Body mass index
- COPD:
-
Chronic obstructive pulmonary disease
- CRC:
-
Colorectal cancer
- DVT:
-
Deep vein thrombosis
- ERP:
-
Enhanced recovery programs
- GRACE:
-
Groupe francophone de Réhabilitation Améliorée après Chirurgie (French Group for Enhanced Recovery after Surgery)
- ICU:
-
Intensive care unit
- LOS:
-
Length of hospital stay
- MELD:
-
Model for end-stage liver disease
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- PACU:
-
Postoperative anesthetic care unit
- PONV:
-
Postoperative nausea and vomiting
- TAP:
-
Transversus abdominis plane
- TRD:
-
Time of readiness for discharge
References
Scott MJ, Baldini G, Fearon KCH et al (2015) Enhanced recovery after surgery (ERAS) for gastrointestinal surgery, part 1: pathophysiological considerations. Acta Anaesthesiol Scand 59:1212–1231
Greco M, Capretti G, Beretta L, Gemma M, Pecorelli N, Braga M (2014) Enhanced recovery program in colorectal surgery: a meta-analysis of randomized controlled trials. World J Surg 38:1531–1541
Visioni A, Shah R, Gabriel E, Attwood K, Kukar M, Nurkin S (2018) Enhanced recovery after surgery for noncolorectal surgery? Ann Surg 267:57–65
Melloul E, Hübner M, Scott M et al (2016) Guidelines for perioperative care for liver surgery: enhanced recovery after surgery (ERAS) society recommendations. World J Surg 40:2425–2440
Hughes MJ, McNally S, Wigmore SJ (2014) Enhanced recovery following liver surgery: a systematic review and meta-analysis. HPB 16:699–706
Page AJ, Ejaz A, Spolverato G et al (2015) Enhanced recovery after surgery protocols for open hepatectomy—physiology, immunomodulation, and implementation. J Gastrointest Surg 19:387–399
Brustia R, Slim K, Scatton O (2019) Enhanced recovery after liver surgery. J Visc Surg 156:127–137
Damania R, Cocieru A (2017) Impact of enhanced recovery after surgery protocols on postoperative morbidity and mortality in patients undergoing routine hepatectomy: review of the current evidence. Ann Transl Med. https://doi.org/10.21037/atm.2017.07.04
Yang R, Tao W, Chen YY, Zhang BH, Tang JM, Zhong S, Chen XX (2016) Enhanced recovery after surgery programs versus traditional perioperative care in laparoscopic hepatectomy: a meta-analysis. Int J Surg 36:274–282
Li M, Zhang W, Jiang L, Yang J, Yan L (2016) Fast track for open hepatectomy: a systemic review and meta-analysis. Int J Surg 36:81–89
Jones C, Kelliher L, Dickinson M, Riga A, Worthington T, Scott MJ, Vandrevala T, Fry CH, Karanjia N, Quiney N (2013) Randomized clinical trial on enhanced recovery versus standard care following open liver resection. Br J Surg 100:1015–1024
Kaba A, Laurent SR, Detroz BJ, Sessler DI, Durieux ME, Lamy ML, Joris JL (2007) Intravenous lidocaine infusion facilitates acute rehabilitation after laparoscopic colectomy. J Am Soc Anesthesiol 106(1):11–18
Daenen C, Coimbra C, Hans G, Joris J (2018) Labelling as reference Centre of GRACE (Groupe francophone de Réhabilitation Améliorée après ChirurgiE) for colorectal surgery: its impact on the implementation of enhanced recovery programme at the University Hospital of Liège. Acta Chir Belg 118:294–298
Maeda H, Okabayashi T, Nishimori I, Yamashita K, Sugimoto T, Hanazaki K (2010) Hyperglycemia during hepatic resection: continuous monitoring of blood glucose concentration. Am J Surg 199:8–13
Jammer I, Wickboldt N, Sander M et al (2015) Standards for definitions and use of outcome measures for clinical effectiveness research in perioperative medicine: European Perioperative Clinical Outcome (EPCO) definitions: a statement from the ESA-ESICM joint taskforce on perioperative outcome measures. Eur J Anaesthesiol 32:88–105
Aarts MA, Rotstein OD, Pearsall EA, Victor JC, Okrainec A, McKenzie M, McCluskey SA, Conn LG, McLeod RS (2018) Postoperative ERAS interventions have the greatest impact on optimal recovery. Ann Surg 267:992–997
Chua DW, Sim D, Syn N, Abdul Latiff JB, Lim KI, Sim YE, Abdullah HR, Lee SY, Chan CY, Goh BKP (2022) Impact of introduction of an enhanced recovery protocol on the outcomes of laparoscopic liver resections: a propensity-score matched study. Surgery 171:413–418
Ovaere S, Boscart I, Parmentier I, Steelant PJ, Gabriel T, Allewaert J, Pottel H, Vansteenkiste F, D’Hondt M (2018) The effectiveness of a clinical pathway in liver surgery: a case-control study. J Gastrointest Surg 22:684–694
Brustia R, Mariani P, Sommacale D et al (2021) The impact of enhanced recovery program compliance after elective liver surgery: results from a multicenter prospective national registry. Surgery 170:1457–1466
Ripollés-Melchor J, Abad-Motos A, Cecconi M et al (2022) Association between use of enhanced recovery after surgery protocols and postoperative complications in colorectal surgery in Europe: the EuroPOWER international observational study. J Clin Anesth. https://doi.org/10.1016/j.jclinane.2022.110752
Jurt J, Slieker J, Frauche P, Addor V, Solà J, Demartines N, Hübner M (2017) Enhanced recovery after surgery: can we rely on the key factors or do we need the bel ensemble? World J Surg 41:2464–2470
Byrne BE, Faiz OD, Bottle A, Aylin P, Vincent CA (2021) A protocol is not enough: enhanced recovery program-based care and clinician adherence associated with shorter stay after colorectal surgery. World J Surg 45:347–355
Magne Augestad K, AugestadDelaney DKMCP (2010) Postoperative ileus: impact of pharmacological treatment, laparoscopic surgery and enhanced recovery pathways. World J Gastroenterol 16:2067–2074
Kehlet H, Holte K (2001) Review of postoperative ileus. Am J Surg 182(5):S3–S10
Wick EC, Grant MC, Wu CL (2017) Postoperativemultimodal analgesia pain management with nonopioid analgesics and techniques a review. JAMA Surg 152:691–697
Brolet EA, Joris JL, Monseur JJ, Donneau AFH, Slim K (2021) Impact of non-steroidal anti-inflammatory drugs on the efficiency of enhanced recovery programmes after colorectal surgery: a retrospective study of the GRACE database. Anaesth Crit Care Pain Med. https://doi.org/10.1016/j.accpm.2021.100880
Zhao Y, Qin H, Wu Y, Xiang B (2017) Enhanced recovery after surgery program reduces length of hospital stay and complications in liver resection. Medicine. https://doi.org/10.1097/MD.0000000000007628
Wong-Lun-Hing EM, van Dam RM, van Breukelen GJP et al (2017) Randomized clinical trial of open versus laparoscopic left lateral hepatic sectionectomy within an enhanced recovery after surgery programme (ORANGE II study). Br J Surg 104:525–535
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Gabriel THIERRY and Jean JORIS received financial support from GRACE (Francophone Group for Enhanced Recovery after Surgery, Beaumont, France, www.grace-asso.fr) for correction and translation of this manuscript. The funding source was not involved in study design, in collection, analysis, or interpretation of data, in the writing of the report, or in the decision to submit this article for publication. Jean JORIS is an honor member of GRACE. However, Gabriel THIERRY (first author) and Jean JORIS have no conflicts of interest relative to this study. Vincent BONHOMME has no conflicts of interest relative to this study but has received an unrestricted grant from Orion Pharma for research support, support for a specific training from Medtronic, support for attending meetings from Edwards Medical, support for publication of a book chapter from Elsevier and reports speaker’s consultancy fees on behalf of Grünenthal. Florian BECK has no conflicts of interest relative to this study but has received honoraria from Fresenius-Kabi and Viatris for logistic implementations at Liege University Hospital in Belgium. Morgan VANDERMEULEN has no conflicts of interest relative to this study but has received a research grant from the Belgian national scientific research foundation (FNRS). Olivier DETRY has no conflicts of interest relative to this study but has received contracts from Medtronic, Corza, Applied, Boston medical, a research grant from the Belgian national scientific research foundation (FNRS) and received equipment and materials from Medtronic and Johnson & Johnson. Abdourahmane KABA, Arielle BLANJEAN, Pierre-Yves HARDY and Pierre HONORE declare they have no conflicts of interest.
Ethical approval
All procedures were performed in accordance with the ethical standards of the institutional research committee and the 1964 Helsinki Declaration and its subsequent amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Thierry, G., Beck, F., Hardy, PY. et al. Impact of enhanced recovery program implementation on postoperative outcomes after liver surgery: a monocentric retrospective study. Surg Endosc 38, 3253–3262 (2024). https://doi.org/10.1007/s00464-024-10796-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-024-10796-w