Abstract
Background
Evidence regarding the outcomes benefits of robotic approach, when compared to a laparoscopic approach, in colectomy remain limited.
Objective
This study aimed to analyze the value of robotic approach compared to laparoscopic approach in minimally invasive colectomy.
Design
Cohort study of the National Surgical Quality Improvement Program (NSQIP).
Setting
This study included data from the NSQIP from 1/2016 to 12/2021.
Patient
Adult patients undergoing minimally invasive (laparoscopic or robotic) colorectal surgery.
Intervention
Robotic versus laparoscopic colectomy.
Outcome measures
Risk ratios for the incidence of medical and surgical morbidity and overall mortality.
Results
Compared to laparoscopic, robotic colectomy was associated with a significant decrease in postoperative morbidity [RR 0.84 (95%CI 0.72–0.96), P < 0.001], a significant reduction in postoperative mortality [RR 0.83 (95%CI 0.79–0.90), P 0.010)], and in post operative ileus [RR: 0.80 (95%CI 0.75–0.84), P < 0.001]. Yet, robotic approach was associated with a significant increase in total operative time despite a significant decrease in total length of stay. No benefit was observed regarding anastomotic leak.
Limitations
Observational nature of the study cannot exclude residual bias.
Conclusions
In this prospective cohort from the NSQIP, robotic colectomy was associated with a significant reduction in postoperative ileus, unplanned conversion to open surgery, morbidity, and overall mortality when compared to laparoscopic colectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Robotic surgery has been rapidly incorporated into surgical practice over the last 30 years. [1, 2] in many surgical fields, including colorectal procedures. While initial reports have suggested potential benefits, such as reduced incidence of postoperative ileus [3] and shorter hospital stays, the evidence supporting these claims remains inconclusive when adjusting for confounding factors [4, 5]. Moreover, relevant outcomes of surgical success, including anastomotic leak rates and overall mortality, have shown comparable results between robotic and laparoscopic approaches (3.4) The benefits of robotic approach over laparoscopic approach in colectomy has presented equivocal surgical and medical outcomes in previous studies. A recent analysis of a large national database [6] has shown similar surgical outcomes for robotic colectomy in colon cancer, though the findings were partially influenced by inclusion of early years of robotic adoption in medical practice. To address this relevant question, we abstracted a prospective collected cohort using the American Colleges of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) across multiple indications for colectomy. We hypothesized that robotic colectomy could present improved morbidity and mortality when compared to laparoscopic approaches.
Methods
Study oversight—IRB exemption
The data in these studies were de-identified and thus were exempt from formal review by our Institutional Review Board.
Cohort abstraction
We abstracted data from the ACS-NSQIP participant user files from 1/2016 through 12/2021. First, we identified all patients who underwent surgery at participating NSQIP hospitals and collected the data for the procedure targeted colectomy files. We included only patients treated with minimally invasive (laparoscopic or robotic) colectomy. We included all cases in which robotic and laparoscopic surgery was included for the overall analysis. We also included cases with unplanned conversion to open surgery as an “intention to treat”population, as well as cases with planned open assist.
Left versus right colectomy
Patients who underwent a right-sided colectomy were defined as those patients who had a partial colectomy with ileocolic anastomosis (CPT code 44160 or 44205). Patients who underwent left-sided colectomy were defined as those who had a partial colectomy with anastomosis (CPT codes 44140, 44204, 44145 or 44207). Due to misclassification regarding segmental colectomies, we also included a segmental colectomy subgroup (CPT codes 44140 and 44204) for the purpose of multivariate analysis.
Interventions
The intervention for this study was surgical approach to colectomy (either robotic or laparoscopic). The NSQIP codes cases as purely robotic as well as robotic with open assist and robotic with unplanned conversion. We included all approaches as an overall “intention to treat” robotic colectomy approach cohort. Similarly, the laparoscopic group included case codes as purely laparoscopic as well as laparoscopic with open assist or unplanned conversion. To improve the homogeneity of our cohort, we excluded natural orifice transluminal endoscopic surgery (NOTES), single incision laparoscopy surgery (SILS) and hybrid procedures.
Covariates
Trained clinical research abstractors collected the covariates of age, gender, body mass index (BMI), presence of diabetes mellitus with and without insulin use, hypertension, smoking history, use of steroids, and history of heart failure. American Society of Anesthesiologists (ASA) scores were also abstracted.
Primary outcomes
Our primary outcomes were all-cause morbidity, as well as overall 30 days mortality. All-cause morbidity included all patients who experienced any episode of return to the operating room, myocardial infarction, deep vein thrombosis, pneumonia, acute renal failure, cardiac arrest, urinary tract infection, wound disruption, pulmonary embolism, progression of renal failure, superficial and deep surgical site infection and postoperative sepsis. This all-cause morbidity outcome has been validated in previous studies using the NSQIP [7], and was included in our pre-specified statistical analysis plan [8].
Secondary outcomes
Our secondary outcomes included the incidence of postoperative ileus, total operative time, total length of in -hospital stay, rate of unplanned conversion to open surgery.
Statistical analysis
We aggregated the data to compare robotic versus laparoscopic colectomy. We performed univariate analysis incorporating χ2 tests, Fisher exact tests, and independent-sample t tests to compare patient baseline characteristics by time to intervention. Chi-squared risk ratios were used for categorical data. Next, our multivariable analyses used Poisson regression models to estimate relative risks adjusted for potential confounders, including demographic (age, gender, weight), patient risk factors (diabetes mellitus, hypertension, smoking status, heart failure) ASA scores, indication for surgery (Inflammatory Bowel Disease, Colon Cancer and Diverticular Disease) and surgical intervention (right, left colectomy and segmental colectomy), emergency vs elective and specialty of surgical provider. We also conducted propensity-score match analysis for our primary outcomes with treatment effect logistic models to obtain coefficients paired by the same demographics and risk factors as our Poisson Regression, using Probit Regression Module. All the analysis were conducted on STATA 18 Standard Edition.
The reporting of this study conforms to the strengthening the reporting of observational studies in epidemiology (STROBE) reporting guidelines. Our statistical analysis plan was published as a pre-specified statistical analysis plan (SAP) [8].
Results
Cohort
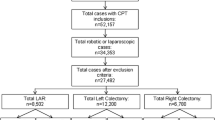
The NSQIP registered 219,981 patients with colectomy procedures from 1/1/2016 to 12/31/2021. After excluding open surgery cases our “intention to treat minimally invasive” cohort—including cases of unplanned conversion to open surgery comprised 132,071 patients.
Robotic and laparoscopic colectomy cohorts
Of the 132,071 patients in the minimally invasive cohort 25,175 cases were robotic, and 106,896 cases were laparoscopic. As compared to laparoscopic colectomy, robotic patients were significantly older, male and presented a higher proportion of cases with smoking, hypertension, diabetes and ASA 2 or higher scores. Demographic results are summarized in Table 1. The most frequent indication for surgery was colon cancer in both cohorts, although we noted proportionately more cancer cases in the robotic patients.
Overall mortality
Any cause 30 days mortality was significantly reduced with robotic approach, both in crude analysis and after adjusting for multiple confounders. The absolute incidence of mortality was around 2% in the laparoscopic group and 1.8% in the robotic group (RR 0.83 (95%CI 0.79–0.90), P 0.010). Absolute incidences are presented on Table 2.
Morbidity
We also analyzed the outcome of any-cause 30 day morbidity. Robotic approach was associated with a significant reduction in all-cause morbidity, after adjusting for multiple confounders {adjusted RR: 0.84 (95%CI 0.72–0.96), P < 0.001}. Absolute incidences are presented in Table 2.
Ileus
A total of 14,001 patients experienced postoperative ileus, 10.97% in the laparoscopic colectomy group and 9.03% in the robotic group. The incidence of ileus was significantly reduced with a robotic approach, even after adjusting for multiple confounders {adjusted RR: 0.83 (95%CI 0.79–0.87), P < 0.001}.
Anastomotic leak
A total of 3403 patients experienced an anastomotic leak, 2.5% in the laparoscopic cohort and 2.7% in the robotic cohort. There was no statistically significant difference in the incidence of anastomotic leak in the crude analysis {RR:1.10 (95%CI 0.96–1.15), P = 0.2}, and after adjusting for multiple confounders {RR:1.05 (95%CI 0.95–1.17), P = 0.309}. We also stratified leak incidence by BMI status—as previous studies have noticed significant advantages for robotic colectomy in the obese population [9]. We did not find evidence for effect modification by BMI in the anastomotic leak subgroup. The primary outcomes are presented in Table 2.
Operative time and length of stay
Robotic approach was associated with a significant increase in total operative time (P < 0.001), with a mean increase of 12 min. On the contrary, a robotic approach was associated with a significant reduction in total length of stay, of approximately 1 day (P < 0.001). We analyzed the trend over time for operative duration in robotic colectomy using the Jonckheere–Terpstra test for trends and linear regression models, with no evidence of decrease in additional operative time over the years of analysis.
Unplanned conversion rate
Unplanned conversion to open surgery was significantly reduced in robotic approach when compared to laparoscopic approach (12.6% vs. 6.1%, P < 0.001).
Propensity-score match analysis
Due to the observational nature of our study, we decided to run Propensity-score match analysis—analysis for our primary outcomes. Robotic Approach was still associated with a significant reduction in mortality (Coef—0.99, 95%CI {− 0.17 to − 0.21}. P 0.013) and medical-related morbidity (Coef—0.16, 95%CI {− 0.19 to − 0.13}, P < 0.001).
Discussion
In this global prospective cohort study of 219,981 patients treated from 1/2016 through 12/2021 using the American college of surgeons national surgical quality improvement program, robotic colectomy was associated with a significant reduction in overall mortality, a significant reduction in all-cause morbidity, a significant reduction in length of stay, and significant reduction in postoperative ileus and ostomy creation when compared to a laparoscopic approach. These results were statistically significant in the crude and adjusted analysis and indicate signficant immediate advantages to robotic procedures.
Previous studies have shown improved surgical and medical outcomes with robotic approaches (3–5). However, these results lost significance after adjusting for standard covariates, and limiting analysis to particular populations. The most consistent findings across prior observational trials was the reduction in total length of stay, at the expense of an increase in total operative time. Our present cohort includes a much larger sample size, including the last 6 available years in the ACS—NSQIP database. In addition, other studies utilized administrative data, whereas NSQIP is clinical in nature, with validated outcomes.
As previously described, we noted an increase in total operative time with robotic colectomy. We conducted analysis of temporal trends within the NSQIP database, hypothesizing that additional operative time could be reduced as surgeons became more efficient with a robotic approach. On the contrary, we found evidence of the opposite effect: a trend towards increased operative time with a robotic approach.Although operative time may be prolonged, it should not be necessarily considered as an adverse outcome. Interestingly, there is evidence from one cohort study [10] indicating that a longer operative time was not associated with poorer outcomes in the setting of minimally invasive surgery. Also, the definition of operative time in NSQIP database includes set up time for the robot, and does not reflect only procedural time per se. Hence, it is essential to consider the context and individual patient characteristics when evaluating the significance of a prolonged operative time. Further research is needed to address this important topic to help explain the additional time for robotic procedures and the lack of improved efficiency with time.
We did not identify a difference in anastomotic leak between laparoscopic and robotic colectomy. A lack of difference was noted regardless of BMI categories. We conducted further analyses to assess whether indication for colectomy may be influential in the anastomotic leak rates by diagnostic category. Results were similar between laparoscopic and robotic approach colectomy in colon cancer, inflammatory bowel disease, and diverticular disease. These results may be explained by similar anastomotic methods or stapling technologies regardless of indication. Also, we could not adjust for the use of indocyanine green in anatomic perfusion tests due to lack of this report in our database.
We found a significant reduction in overall mortality with robotic approaches to colectomy when compared to laparoscopic colectomy. This result must be considered with the understanding that the robotic colectomy population was significantly older and more morbid than the laparoscopic group, with a significantly higher cancer prevalence. Even after adjusting for multiple confounders, the mortality results were highly significant indicating a superiority of robotic surgery over laparoscopic surgery. Previous studies have failed to demonstrate a mortality benefit with robotic approaches in colectomy [11, 12]. The likely improvement in mortality is likely related to overall similar reduction in morbidity.
Our study has several limitations. We can not adjust for possible confounders as surgical expertise and hospital volume or teaching facility. Also, although we adjudged for multiple different indications (IBD, cancer, diverticular disease) the influence of surgical complexity in the presented outcomes is also a possible bias. Also, the literature shows that NSQIP may misidentify ostomy creation [13], specially diverting loop ileostomy. Thus, we could not accurately report on ostomy creation differences across groups.
Additionally, our analysis was also limited by the lack of financial data in the NSQIP database, which could bring about relevant analysis. Institutional protocols differences and discharge criteria could not be adjusted for. Finally, due to the observational nature of the study, the risk of residual bias cannot be excluded. However, compared to previous publications, our work has several strengths. First, our data from the ACS-NSQIP has a prospective design and is in clinical in nature, lowering limitations of observational design. Also, we are presenting a very large sample, comprising the last five available years of the NSQIP cohort. Because adverse outcomes in contemporary minimal invasive colectomy are rare, previous studies may have been underpowered to detect significant differences in robotic colectomy.
Conclusions
In summary, in this global prospective cohort using ACS- NSQIP data, robotic colectomy was associated with a reduced incidence of ileus, morbidity and overall short-term (30 days) mortality when compared to laparoscopic colectomy. It was also associated with a reduced total length of stay, ostomy creation, at the expense of longer operative times.
References
Lane T (2018) A short history of robotic surgery. Ann R Coll Surg Engl 100(6):5–7. https://doi.org/10.1308/rcsann.supp1.5
Leal Ghezzi T, Campos Corleta O (2016) 30 years of robotic surgery. World J Surg 40(10):2550–2557. https://doi.org/10.1007/s00268-016-3543-9
Benlice C, Aytac E, Costedio M, Kessler H, Abbas MA, Remzi FH, Gorgun E (2017) Robotic, laparoscopic, and open colectomy: a case-matched comparison from the ACS-NSQIP. Int J Med Robot Comput Assist Surg. https://doi.org/10.1002/rcs.1783.10.1002/rcs.1783
Miller PE, Dao H, Paluvoi N, Bailey M, Margolin D, Shah N, Vargas HD (2016) Comparison of 30-day postoperative outcomes after laparoscopic vs robotic colectomy. J Am Coll Surg 223(2):369–373. https://doi.org/10.1016/j.jamcollsurg.2016.03.041
Al-Mazrou AM, Chiuzan C, Kiran RP (2017) The robotic approach significantly reduces length of stay after colectomy: a propensity score-matched analysis. Int J Colorectal Dis 32(10):1415–1421. https://doi.org/10.1007/s00384-017-2845-1
Ahuja V, Paredes LG, Leeds IL, Perkal MF, King JT Jr (2023) Clinical outcomes of elective robotic vs laparoscopic surgery for colon cancer utilizing a large national database. Surg Endosc 37(9):7199–7205. https://doi.org/10.1007/s00464-023-10215-6
de Almeida Leite RM, de Souza AV, Bay CP, Cauley C, Bordeianou L, Goldstone R, Francone T, Kunitake H, Ricciardi R (2022) Delayed operative management in complicated acute appendicitis-is avoiding extended resection worth the wait ? Results from a global cohort study. J Gastrointest Surg. https://doi.org/10.1007/s11605-022-05311-2
de Almeida Leite RM (2022) Outcomes for robotic colectomy. https://doi.org/10.17605/OSF.IO/B4JUC
Harr JN, Haskins IN, Amdur RL, Agarwal S, Obias V (2018) The effect of obesity on laparoscopic and robotic-assisted colorectal surgery outcomes: an ACS-NSQIP database analysis. J Robot Surg 12(2):317–323. https://doi.org/10.1007/s11701-017-0736-7
Jochum SB, Becerra AZ, Zhang Y, Hayden DM, Saclarides TJ, Bhama AR (2022) Keep them on the table: outcomes are improved after minimally invasive colectomy despite longer operative times in patients with high-risk colon cancer. Dis Colon Rectum 65(9):1143–1152. https://doi.org/10.1097/DCR.000000000000211910
Spinoglio G, Marano A, Bianchi PP, Priora F, Lenti LM, Ravazzoni F, Formisano G (2016) Robotic right colectomy with modified complete mesocolic excision: long-term oncologic outcomes. Ann Surg Oncol 23(5):684–691. https://doi.org/10.1245/s10434-016-5580-x
Anderson M, Lynn P, Aydinli HH, Schwartzberg D, Bernstein M, Grucela A (2020) Early experience with urgent robotic subtotal colectomy for severe acute ulcerative colitis has comparable perioperative outcomes to laparoscopic surgery. J Robot Surg 14(2):249–253. https://doi.org/10.1007/s11701-019-00968-5
Luo WY, Holubar SD, Bordeianou L, Cosman BC, Hyke R, Lee EC, Messaris E, Saraidaridis J, Scow JS, Shaffer VO, Smith R, Steinhagen RM, Vaida F, Eisenstein S, National Surgical Quality Improvement Program-Inflammatory Bowel Disease (NSQIP-IBD) Collaborative: Collaborating Institutions and Investigators (2021) Better characterization of operation for ulcerative colitis through the National surgical quality improvement program: a 2-year audit of NSQIP-IBD. Am J Surg 221(1):174–182. https://doi.org/10.1016/j.amjsurg.2020.05.035
Funding
This work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Ms. Hannah Bossie works for Intuitive inc as a Medical Science Liaison and is a stockholder of the company. Ms Bossie did not participate in the statistical analysis or in the results/ conclusions sections of the manuscript. Dr Rodrigo Leite, Dr. Rocco Ricciardi, Dr. Sergio Eduardo Alonso Araujo, Mr. Gustavo Yano Callado, Dr. Alexandre Venancio de Souza, Dr. Robert Neil Goldstone, Dr. Todd Francone, Dr Leandro Barchi, Dr. Larissa Fagundes, Dr. Ulysses Ribeiro jr does not have any conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
de Almeida Leite, R.M., Araujo, S.E.A., de Souza, A.V. et al. Surgical and medical outcomes in robotic compared to laparoscopic colectomy global prospective cohort from the American college of surgeons national surgical quality improvement program. Surg Endosc 38, 2571–2576 (2024). https://doi.org/10.1007/s00464-024-10717-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-024-10717-x