Abstract
Background and objective
Benign retroperitoneal tumors (BRTs) are clinically rare solid tumors. This study aimed to compare the safety and efficacy of laparoscopic transperitoneal versus retroperitoneal resection for BRTs.
Methods
The clinical data of 43 patients who had pathologically confirmed BRTs and underwent laparoscopic resection in a single center from January 2019 to May 2022 were retrospectively analyzed. Patients were divided into two groups according to the surgical methods: the Transperitoneal approach group (n = 24) and the Retroperitoneal approach group (n = 19). The clinical characteristics and perioperative data between the two groups were compared. The baseline data and surgical variables were analyzed to determine the impact of different surgical approaches on the treatment outcomes of BRTs.
Results
No significant difference was observed between the two groups in gender, age, body mass index, the American Society of Anesthesiologists score, presence of underlying diseases, tumor size, tumor position, operation duration, intraoperative hemorrhage, postoperative hospital stay, intestinal function recovery time, and postoperative complication rate. The conversion rate from laparoscopic to open surgery was significantly lower in the Transperitoneal approach group than in the Retroperitoneal approach group (1/24 vs. 5/19, χ2 = 4.333, P = 0.037). Tumor size was an independent influencing factor for the effect of surgery (odds ratio = 1.869, 95% confidence interval = 1.135–3.078, P = 0.014) and had a larger efficacy on the retroperitoneal group (odds ratio = 3.740, 95% confidence interval = 1.044–13.394, P = 0.043).
Conclusion
The laparoscopic transperitoneal approach has the inherent advantages of anatomical hierarchies and surgical space, providing a better optical perspective of the targeted mass and improved bleeding control. This approach may have better efficacy than the retroperitoneal approach, especially in cases of a large tumor or when the tumor is located near important blood vessels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Retroperitoneal tumors (RTs) are clinically rare solid tumors originating from the retroperitoneal mesenchymal or neural tissues with the properties of expansive growth [1]. They possess either benign or malignant histological features, with the occurrence rate of benign retroperitoneal tumors (BRTs) four times lower than that of malignant RTs [2, 3]. The most common pathological types of BRTs, in descending order of incidence, are neurofibromas, schwannomas, paraganglioma, and lipomas, with a higher morbidity rate in females than in males [4]. The gold standard of treatment for BRTs is laparoscopic R0 or R1 resection, with a success rate of over 90% [5]. However, there is ongoing debate regarding the optimal approach to laparoscopic resection. While urologists prefer the retroperitoneal approach, general surgeons typically tend to favor the transperitoneal approach [6, 7]. Previous evidence suggests that laparoscopic retroperitoneal resection is a safe and feasible approach for retroperitoneal paraganglioma as it provides direct exposure to the retroperitoneal space with less interference to adjacent tissues in the peritoneal cavity [8]. However, whether laparoscopic retroperitoneal resection is superior to the transperitoneal approach remains unclear. In this study, we aimed to compare the safety and efficacy of laparoscopic transperitoneal versus retroperitoneal resection for different types of BRTs.
Patients and methods
Patients and data
In this retrospective cohort study, patients who were diagnosed with pathological BRTs and underwent laparoscopic resection between January 2019 and May 2022 in our hospital were eligible for screening. The inclusion criteria were as follows: (1) aged between 18 and 80 years; (2) postoperatively diagnosed with BRTs and confirmed by pathological examination; (3) the maximum diameter of the tumor was less than 10 cm; (4) the tumor was in the middle and upper abdomen; (5) with no history of abdominal surgeries; (6) with complete demographic and clinical data, including perioperative examination results, surgical records, and pathological reports. Patients were excluded if they: (1) had an American Society of Anesthesiologists (ASA) score of > 3; (2) were diagnosed with coagulation disorders; (3) underwent exploratory surgery or were combined with other organ resections; or (4) had incomplete clinical data. The surgical approach was selected depending on the tumor size, type, and anatomical location. For tumors situated near the posterior area, transperitoneal resection was employed. However, when tumors are positioned away from the posterior region, the retroperitoneal approach was used. A total of 43 patients were finally enrolled in the study. Among them, 24 were treated using the transperitoneal approach (Transperitoneal approach group) by the surgical team in the Department of Hepatobiliary and Pancreatic Surgery, while 19 were treated using the retroperitoneal approach (Retroperitoneal approach group) by the surgical team in the Department of Urology. This study was approved by the local ethics committee (approval number: 20211682) and performed in accordance with the Declaration of Helsinki. As all clinical data were collected anonymously, informed consent was waived.
Surgical procedures
All surgical procedures were performed by surgeons who that had performed more than 50 laparoscopic surgeries. All patients underwent combined intravenous-inhalation anesthesia and endotracheal intubation. According to the resection approaches, the patient was placed in the split-leg supine position or the lateral decubitus position. The pneumoperitoneum was established at 10–12 mmHg. The 4 K laparoscope (2100 Series, OptoMedic Technologies, China), ultrasonic scalpel (Harmonic scalpel, Ethicon, Johnson Medical, USA), bipolar coagulation forceps (Aierbo, Germany), and Hem-O-Lok clamp (Wick Polymer Plastic Ligation Clip, Teleflex Medical, USA) were used for surgery.
The retroperitoneal approach
The patient was placed in a lying position on the unaffected side, with the ipsilateral side facing up and the lumbar region elevated. A 10-mm trocar was placed 2 cm above the iliac crest in the midaxillary line, and the scope was inserted. A 5- and 10-mm trocar were placed in the anterior and posterior axillary lines under the 12th rib, respectively. Manipulation and assistant devices were inserted. In some cases, such as those involving large tumors, the number of trocars could be increased. Blunt dissection and water balloon injection were used to create an operating space. Subsequently, an ultrasonic scalpel and bipolar coagulation forceps were used to dissect the perirenal fat sac to expose the tumor. Resection along the tumor capsule was performed, with the Hem-O-Lok clamping of the inflow and outflow of the tumor. Then, the incision was sutured. The important vessels and organs were protected during the operation.
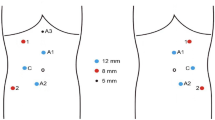
The transperitoneal approach
The patient was placed in a supine position with split legs, and if necessary, in a side decubitus position. Four or five trocars were placed in a fan shape surrounding the targeted area, with 4 or 5 trocars used. For tumors on the right or posterior side, the right-sided approach was used. The head of the pancreas and duodenum were dissected following the Kocher’s manual. Subsequently, the plane of the right renal vein, the inferior vena cava, and the abdominal aorta could be directly visualized. If necessary, the hepatic flexure and the ascending colon could be separated. Before exposing the target mass, the Toldt’s fascia could be dissected and extended to the left and caudal sides to facilitate the resection. The procedure of laparoscopic transperitoneal resection for a patient with BRTs in the left upper area is shown in Fig. 1. The procedure for direct exposure and resection of BRTs using intraoperative ultrasound is shown in Fig. 2.
Laparoscopic transperitoneal resection for BRT in the left upper area. A, B Patient No. 20 in the Transperitoneal approach group had lipoma (5.0 * 4.5 cm) located between the right side of the left kidney and the lower level of the spleen, and the tail of the pancreas. C, D After removing the gastrocolic ligament and suspending the gastric body, the omental sac was then entered, and the dorsal peritoneum from the tail of the pancreas to the spleen was dissected along the inferior margin of the pancreas from the right side in a horizontal direction. E, F After tumor exposure, the borders between the target and the tail of the pancreas, spleen, and left kidney were completely dissociated along the target. G–I Complete resection of BRT after ligation and dissection of the tumor blood supply vessels. G The white line indicates the medial border of the tumor, and the white arrow indicates the tumor blood supply vessels. H The yellow arrow indicates the tail of the pancreas; the black arrow indicates the splenic hilum; the white arrow indicates the left kidney. I The complete resected tumor specimen
Laparoscopic transperitoneal resection procedure for BRT using intraoperative ultrasound. A, B Patient No. 21 in the Transperitoneal approach group had a paraganglioma (4.6 * 3.5 cm) located in the ventral side of the left renal vein, close to the hilum. C, D Intraoperative ultrasound was used to confirm the position of the target without dissecting the lateral peritoneum and entering the prerenal space by opening the mesentery of the left colon. During the procedure, Gerota’s fascia was carefully transected while taking care of the inferior mesenteric vein (IMV) and genital vein. E, F The ultrasonic scalpel was used to dissect any adhesions and disconnect any inflow vessels that were blocked. The tumor was then completely stripped and removed
Data collection
The demographic and clinical data, including age, sex, body mass index (BMI), presence of underlying disease, the ASA score, tumor size, and tumor position, were collected. The following surgical data were also obtained and analyzed: operation duration, conversion rate from laparoscopic to open surgery, number of cases with hemorrhage, rate of intraoperative blood transfusion, length of postoperative hospital stay, time to recovery of intestinal function, and postoperative complications, which were determined by the Clavien-Dindo Classification [9].
Efficacy assessment
Since there is no established agreement on the criteria for assessing the efficacy of laparoscopic resection for BRTs, this study defined “good curative effect” as meeting the following criteria: no conversion to open surgery, no postoperative complications, hospitalization for no more than 4 days, and bowl recovery within 2 days. Other conditions were defined as having a “general curative effect.” “No conversion to open surgery” and “no postoperative complications” are common indicators of successful postoperative recovery in laparoscopic surgery [10]. The duration of postoperative hospitalization varies based on the discharge criteria of different medical facilities in China. At our hospital, postoperative hospitalization for laparoscopic procedures without gastrointestinal or vascular reconstruction typically lasts less than 4 days, making this timeframe a reference criterion for favorable postoperative recovery. The bowel function recovery time was determined following the criterion proposed by Zhao et al. [11].
Statistical analysis
Statistical analysis was performed using the SPSS Statistics 26.0 software (SPSS Inc., USA), with P < 0.05 indicating statistical significance. Normally distributed measurement data were represented as mean ± standard deviation and compared by independent samples t-test. Non-normally distributed measurement data were expressed as median (Q1, Q3) and compared by Wilcoxon rank-sum test. Categorical data were shown as numbers of cases and percentages, and Pearson’s χ2 test or Fisher’s exact test was used for comparison.
Multiple linear regression analysis was performed with BMI, tumor size, and tumor position as independent variables, and operation time and intraoperative bleeding as dependent variables. The dummy variables setting was as follows: post area = 0, right upper area = 010000, right lower area = 001000, left upper area = 000100, left lower area = 000010, between left upper and lower = 000001. The influencing factors were first screened by univariate linear regression analysis. Then, factors that showed statistical significance were included in the binary logistic regression analysis to identify the influencing factors for efficacy.
Results
Demographic and clinical characteristics at baseline
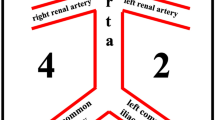
The general characteristics of each patient are shown in Table 1. The position of the tumor, in terms of its spatial relationship with the inferior vena cava and the renal, includes the posterior area (n = 6), right upper area (n = 7), right lower area (n = 3), upper left area (n = 16), lower left area (n = 7), and junction of the upper and lower left area (n = 4) (Fig. 3). The baseline data of the Transperitoneal (n = 24) and Retroperitoneal (n = 19) approach groups are summarized in Table 2. There was no significant difference between the two groups in age, sex, BMI, ASA score, presence of underlying disease, tumor size, or tumor position (all P > 0.05).
Surgical outcomes
Although the Transperitoneal approach group was parallel with the Retroperitoneal approach group in the number of cases with hemorrhage, rate of intraoperative blood transfusion, length of postoperative hospital stay, time to recovery of intestinal function, and rates of postoperative complications, the rate of conversion to open surgery in patients treated with transperitoneal resection was significantly lower than that of those who underwent retroperitoneal laparoscopy (1/24 vs. 5/19, χ2 = 4.333, P = 0.037, Table 3).
In the Transperitoneal approach group, one patient (No. 22) underwent conversion to open surgery. She was diagnosed with paraganglioma in the left lower area with a tumor size of 7.0 * 6.0 cm. The conversion was necessary due to the large size and hazardous location of the tumor, which was close to the left dorsal side of the abdominal aorta. In the Retroperitoneal approach group, five patients (No. 2, 7, 14, 18, and 19) underwent conversion. Patient No. 2 had an injury to the right common iliac artery during the surgery, resulting in almost 1000 mL of bleeding, which required transfusion with 4.5 units of erythrocyte suspension and 400 mL of plasma. Patient No. 7 experienced a left renal vein injury during the surgery, resulting in 800 mL of bleeding. Intraoperatively transfusion with 2 units of erythrocyte suspension was administered. Patients No. 14, 18, and 19 had tumors located at a deep position and were of a large size (6.5 * 4.5, 7.0 * 6.0, and 9.0 * 5.5 cm, respectively), leading to conversion to open surgery.
There were two patients with Clavien-Dindo Grade II complications in the Transperitoneal approach group. Patient No. 11 experienced pancreatic leakage, which was managed with adequate drainage and inhibition of the secretion. Patient No. 13 was discharged from the hospital with a wound infection and severe hypoalbuminemia and received symptomatic treatment. In the Retroperitoneal approach group, two patients with a wound infection had Grade I complications. Two patients (No. 2 and 7) with Grade II complications had an abdominal cavity infection and underwent intraoperative conversion.
Multiple linear regression analysis of surgical outcomes
Multiple linear regression analysis was then performed with intraoperative hemorrhage and operation duration as dependent variables, respectively, and tumor diameter, position, and BMI index as independent variables. The results showed that no variables were significantly correlated with intraoperative hemorrhage (Table 4) or operation duration (Table 5).
Identification of influencing factors for the efficacy of laparoscopic resection
According to the criteria proposed in this study for the assessment of efficacy, there were 27 patients with a good curative effect and 16 with a general curative effect. There was no significant difference in the type of laparoscopic resection approach, sex, age, BMI, ASA score, or tumor position between the two groups. Notably, the average tumor size was smaller in patients with a curative effect than those with a general curative effect (4.2 ± 1.1 vs. 5.6 ± 2.0 cm, t = 2.971, P = 0.005) (Table 6).
Binary logistic regression analysis
The factor “tumor size” was then subjected to binary logistic regression analysis. The results showed that tumor size was an independent influencing factor for surgical outcomes (odds ratio = 1.869, 95% confidence interval = 1.135–3.078, P = 0.014). Sub-analysis revealed that tumor size had a more significant effect on the Retroperitoneal approach group (odds ratio = 3.740, 95% confidence interval = 1.044–13.394, P = 0.043) (Fig. 4).
Discussion
In the present study, we compared the safety and efficacy of laparoscopic transperitoneal versus retroperitoneal resection for BRTs and found that the conversion rate from laparoscopic to open surgery was lower in the Transperitoneal approach group than in the Retroperitoneal approach group, suggesting that transperitoneal resection may have better efficacy than retroperitoneal resection, especially in cases of large tumors or when the tumor is located near important blood vessels.
Most patients with BRTs experience chronic abdominal pain and distension prior to receiving therapy, largely due to the asymptomatic nature of these tumors. As a result, the benign tumor expands to surround giant, vital vessels, which increases the surgical risk [12]. It is recommended to undergo intervention when the tumor is causing pain, compressive symptoms, or endocrine disorders, is rapidly growing, or has ambiguous malignant features [5]. There have been significant advancements in laparoscopic resection over time, with numerous studies demonstrating its safety and feasibility [13,14,15]. For instance, the study by Ahn et al. has shown that laparoscopic resection is a safe and effective treatment option for patients with nonadrenal retroperitoneal tumors that are less than 10 cm, even in cases with large tumors and when adjacent vascular structures are involved [16]. Laparoscopy also possesses advantages in visual magnification, postoperative recovery, and minimally invasive incision [17]. Ji et al. reported that laparoscopic resection is comparable to open surgery in the treatment of BRTs due to parallel efficacy in surgical outcomes, such as operation time, bleeding, and complications [18]. Our study confirmed the safety and feasibility of laparoscopic resection, as none of the 43 patients experienced serious postoperative complications despite the various distribution of the tumors.
The retroperitoneal approach was first considered the standard treatment for retroperitoneal adrenal tumors less than 6 cm [19], and then has become a treatment option for neurogenic tumors and paraganglioma. However, it has also been claimed that the retroperitoneal approach is limited by the narrow space available for surgery [1]. The study by Xu et al., in which 49 patients diagnosed with paraganglioma and treated either with retroperitoneal or transperitoneal resection were recruited, showed that the operation time of the former approach was shorter than that of the latter one [20]. In this study, however, we found that the retroperitoneal approach is non-superior to the transperitoneal one in terms of short-term surgical outcomes. Moreover, the rate of conversion to open surgery in patients treated with retroperitoneal resection was significantly higher than that of those who underwent transperitoneal laparoscopy, especially in cases with large tumors. These findings indicate that, in cases where the tumor is large and close to vessels, the transperitoneal approach may provide a better anatomical hierarchy and a more spacious surgical environment, while the retroperitoneal approach may offer a shorter operation time, albeit in a more limited surgical space.
The postoperative prognosis of patients with retroperitoneal tumors is associated with various factors, such as tumor size, tumor grade, and surgical method of tumor resection [21, 22]. R2 resection of primary tumors was found to be associated with poor prognosis in malignant retroperitoneal tumors, while complete surgical resection of recurrent tumors was associated with a better oncological outcome [23]. In the present study, we found that tumor size was an independent influencing factor for the efficacy of laparoscopic resection in patients with BRTs. Further analysis revealed that tumor size had a more significant effect on the Retroperitoneal approach group than on patients treated with transperitoneal resection.
Conclusions
Our study demonstrated that tumor size is an independent factor that affects the efficacy of laparoscopic resection for the treatment of BRTs, especially in patients undergoing retroperitoneal resection. The lower conversion in the Transperitoneal approach group could be due to the superiority in surgical space and anatomical hierarchy. The transperitoneal approach provides better tumor exposure and bleeding control. Thus, it confers advantages such as higher efficiency, minimal invasiveness, and rapid recovery compared to the retroperitoneal approach. These findings could provide valuable references for the clinical application of these two approaches.
Data availability
The raw data supporting the conclusions of this manuscript will be made available by the corresponding author, without undue reservation, to any qualified researcher.
References
Gemici K, Buldu İ, Acar T, Alptekin H, Kaynar M, Tekinarslan E et al (2015) Management of patients with retroperitoneal tumors and a review of the literature. World J Surg Oncol 13:143
Tambo M, Fujimoto K, Miyake M, Hoshiyama F, Matsushita C, Hirao Y (2007) Clinicopathological review of 46 primary retroperitoneal tumors. Int J Urol 14(9):785–788
Gamboa AC, Gronchi A, Cardona K (2020) Soft-tissue sarcoma in adults: an update on the current state of histiotype-specific management in an era of personalized medicine. CA Cancer J Clin 70(3):200–229
Gulati V, Swarup MS, Kumar J (2022) Solid primary retroperitoneal masses in adults: an imaging approach. Indian J Radiol Imaging 32(2):235–252
(2020) Intercontinental collaborative experience with abdominal retroperitoneal and pelvic schwannomas. Br J Surg 107(4):452–463
Shi C, Li F, Wang Y, Pei L, Wang T (2018) Retroperitoneoscopic resection of retroperitoneal nonadrenal ganglioneuromas: our technique and clinical outcomes. Int Braz J Urol 44(6):1166–1173
Kang CM, Kim DH, Seok JY, Lee WJ (2008) Laparoscopic resection of retroperitoneal benign schwannoma. J Laparoendosc Adv Surg Tech A 18(3):411–416
Xu W, Li H, Ji Z, Yan W, Zhang Y, Xiao H et al (2015) Comparison of retroperitoneoscopic versus transperitoneoscopic resection of retroperitoneal paraganglioma: a control study of 74 cases at a single institution. Medicine (Baltimore) 94(7):e538
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD et al (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196
Romeo L, Bagolini F, Ferro S, Chiozza M, Marino S, Resta G et al (2021) Laparoscopic surgery for splenic injuries in the era of non-operative management: current status and future perspectives. Surg Today 51(7):1075–1084
Zhao G, Cao S, Cui J (2014) Fast-track surgery improves postoperative clinical recovery and reduces postoperative insulin resistance after esophagectomy for esophageal cancer. Support Care Cancer 22(2):351–358
Sassa N (2020) Retroperitoneal tumors: review of diagnosis and management. Int J Urol 27(12):1058–1070
Buia A, Stockhausen F, Hanisch E (2015) Laparoscopic surgery: a qualified systematic review. World J Methodol 5(4):238–254
Ribeiro MA Jr, Elias YG, Augusto SS, Néder PR, Costa CT, Maurício AD et al (2020) Laparoscopic resection of primary retroperitoneal schwannoma: a case report. World J Clin Cases 8(18):4114–4121
Abe T, Sazawa A, Harabayashi T, Oishi Y, Miyajima N, Tsuchiya K et al (2016) Laparoscopic resection of paraaortic/paracaval neurogenic tumors: surgical outcomes and technical tips. Surg Endosc 30(10):4640–4645
Ahn KS, Han HS, Yoon YS, Kim HH, Lee TS, Kang SB et al (2011) Laparoscopic resection of nonadrenal retroperitoneal tumors. Arch Surg 146(2):162–167
Petrucciani N, Sirimarco D, Magistri P, Antolino L, Gasparrini M, Ramacciato G. (2015) Retroperitoneal schwannomas: advantages of laparoscopic resection: review of the literature and case presentation of a large paracaval benign schwannoma (with video). Asian J Endosc Surg 8(1):78–82.
Ji JH, Park JS, Kang CM, Yoon DS, Lee WJ (2017) Laparoscopic resection of retroperitoneal benign neurilemmoma. Ann Surg Treat Res 92(3):149–155
Simutis G, Lengvenis G, Beiša V, Strupas K (2014) Endoscopic retroperitoneal adrenalectomy for adrenal metastases. Int J Endocrinol 2014:806194
Xu W, Li H, Ji Z, Yan W, Zhang Y, Zhang X et al (2016) Retroperitoneal laparoscopic management of paraganglioma: a single institute experience. PLoS ONE 11(2):e0149433
Nathan H, Raut CP, Thornton K, Herman JM, Ahuja N, Schulick RD et al (2009) Predictors of survival after resection of retroperitoneal sarcoma: a population-based analysis and critical appraisal of the AJCC staging system. Ann Surg 250(6):970–976
Chen J, Hang Y, Gao Q, Huang X (2021) Surgical diagnosis and treatment of primary retroperitoneal liposarcoma. Front Surg 8:672669
Fujimoto N, Kubo T, Hisaoka M, Udo K, Yokomizo A, Shibuya T et al (2018) Demographics, management and treatment outcomes of benign and malignant retroperitoneal tumors in Japan. Int J Urol 25(1):61–67
Acknowledgements
We thank everyone, who supports us to finish this study.
Funding
This work was supported by grants from the National multidisciplinary collaborative diagnosis and treatment capacity building project for major diseases (Grant No. TJZ202104), the Natural Science Foundation of China (Grant Nos. 82270643, 82070644 and 82170621), the Science and Technology Major Program of Sichuan Province (Grant No. 2022ZDZX0019), 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (Grant Nos. ZYJC18008, ZYGD22006).
Author information
Authors and Affiliations
Contributions
QX, ZH, CL, JH: Guarantor of integrity of the entire study, Study concepts, Study design, Manuscript preparation—editing—review, and Definition of intellectual content. QX, ZH, GQ, ZJ, SM: Literature research, Clinical studies, Experimental studies, and Data acquisition. QX, ZH: Data analysis and Statistical analysis.
Corresponding authors
Ethics declarations
Disclosures
Ziqi Hou, Qingyun Xie, Guoteng Qiu, Zhaoxing Jin, Shizheng Mi, Chang Liu and Jiwei Huang have no conflicts of interest or financial ties to disclose.
Ethical approval
This study was approved by the Ethics Review Committee of the West China Hospital.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hou, Z., Xie, Q., Qiu, G. et al. Safety and efficacy of laparoscopic transperitoneal versus retroperitoneal resection for benign retroperitoneal tumors: a retrospective cohort study. Surg Endosc 37, 9299–9309 (2023). https://doi.org/10.1007/s00464-023-10504-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10504-0