Abstract
Objective
To evaluate the medium- and long-term outcomes of diverticular peroral endoscopic myotomy (D-POEM) for symptomatic oesophageal diverticulum.
Methods
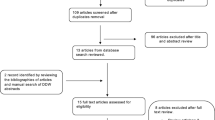
Consecutive patients with symptomatic oesophageal diverticulum who underwent D-POEM from 1st May 2016 to 1st April 2020 in 6 centres were extracted and researched. Symptoms assessed by the modified Eckardt score were registered pre- and post-D-POEM at 1, 6, 12, 24 and 36 months.
Results
A total of 34 patients with Zenker’s diverticulum (ZD, n = 12), mid-oesophageal diverticulum (MED, n = 12), and epiphrenic diverticulum (ED, n = 10) were included. Complete septotomy was achieved in a mean of 39.15 min, with 100% technical success. No severe intraoperative or postoperative complications were observed. Five patients exhibited subcutaneous emphysema, while 1 had mucosal injury. The mean Eckardt score was 8.59 preoperatively and 2.56 at 1 month, 2.09 at 6 months, 2.21 at 12 months, 2.15 at 24 months, and 2.21 at 36 months postoperatively. The total clinical success rates at 1, 6, 12, 24 and 36 months postoperatively were 97.1%, 97.1%, 94.1%, 91.2%, and 88.2%, respectively. With a median follow-up of 47.2 months, four patients suffered symptom relapse, with a total clinical success rate of 88.2%. A long disease duration, a high Eckardt score, and coexistence of achalasia were identified as risk factors for symptomatic recurrence by multivariable Cox analysis.
Conclusions
D-POEM is an effective and durable treatment for patients with symptomatic oesophageal diverticulum.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Oesophageal diverticulum is a rare outpouching of the oesophagus, with a prevalence of 3% [1, 2]. Based on the location and characteristic pathophysiology, it is divided into three types: Zenker’s diverticulum (ZD), mid-oesophageal diverticulum (MED), and epiphrenic diverticulum (ED) [3]. The generally recognized reason for oesophageal diverticulum is associated with increased intraluminal pressure secondary to dynamic abnormalities or a weakening of the oesophageal mucosal membrane [4]. Patients suffering discomfort, such as dysphagia, regurgitation, or chest pain, always need medical treatment [5].
Peroral endoscopic myotomy (POEM), a third-space endoscopy technology via submucosa creation, has been widely accepted in achalasia, gastroparesis and subepithelial tumours [6]. As submucosal tunnelling can totally expose the septum, D-POEM is deemed an innovative technique for complete diverticulum septum transection [6] and has shown satisfactory short-term outcomes [7, 8]. However, relevant data on the long-term efficacy and safety are still lacking. Herein, we summarize the technical points and lessons from the use of D-POEM for oesophageal diverticulum and evaluate its medium- to long-term outcomes.
Methods
Patients
This was multicentre and retrospective study of a prospective database performed regarding patients with symptomatic oesophageal diverticulum who underwent D-POEM between 1st May 2016 to 1st April 2020. The six centres were as follows: Zhongda Hospital, Xuyi County Peoples’s Hospital, Xuzhou Central Hospital, Xuzhou First People’s Hospital, Changshu No. 1 People’s Hospital, and Changzhou Jintan First People’s Hospital. The inclusion criteria were as follows: (1) oesophageal diverticulum diagnosed by contrast oesophagram using iodixanol, gastroscopy and clinical manifestations; (2) high-resolution manometry (HRM) performed to diagnose motility disorders, with or without achalasia but excluding other dynamic disorders (e.g., Killian-Jamieson oesophagus); and (3) no previous medical treatment (except drug therapy). The exclusion criteria were patients who had general diseases and could not tolerate anaesthesia.
Eligible patients were followed up for at least 3 years (the last follow-up date was 1st April 2023). The study complied with the ethical requirements of the Declaration of Helsinki and was approved by our institutional research ethics board (No. ZDYJLY(2016)65). All patients enrolled were confirmed to be at risk of therapy, and informed consent was obtained before the procedure.
Technical aspects of the D-POEM procedure
Procedures were performed by experienced, qualified endoscopists in our institution. All patients underwent surgery under intubation anaesthesia. Carbon dioxide insufflation and a GIF-H260 endoscope (Olympus, Tokyo, Japan) fitted with a transparent cap (Tokyo, Japan) were used during the therapy. A hybrid knife (ERBE, Tübingen, Germany) was used during the procedures. The specific cutting parameters in the operation are as follows: ERBEVIO 300hf electrotome (ERBE, Germany), effect 3, cutting width 2, time interval 4 and power 50 W, while the electrocoagulation parameters are ERBEVIO 300hf electrotome, effect 2, cutting width 2, time interval 4 and power 50/60 W.
The key notes of D-POEM were as follows (Fig. 1):
-
Step 1: Mucosal incision: a mixture of saline solution diluted with methylthionine chloride and epinephrine was used for injection submucosally. A 2-cm oblique mucosal incision was made approximately 3–5 cm above the diverticulum.
-
Step 2: Submucosal tunnelling: A longitudinal submucosal tunnel was created between the mucosal and muscular layers using the hybrid knife. Tunnelling was performed and ended 1–2 cm distal to the bottom of the diverticulum.
-
Step 3: Septum division: muscle fibres of the septum were completely dissected down to the bottom of the diverticulum and through to the normal oesophageal muscle. The key point was to dissect the septum from all around, anteriorly from the mucosa and laterally from the diverticular/oesophageal side, until the septal muscle was exposed right to its base.
-
Step 4: Mucosal closure: after careful haemostasis, the mucosal incision was closed with haemostatic clips. At the end of the procedure, widening of the mouth of the diverticulum and shallowing of the septal height were observed, with free passage of the endoscope through the oesophageal lumen.
Fig. 1 The key steps of D-POEM: A an oesophageal diverticulum was seen on the right side of the lumen, while on the left was the normal oesophageal cavity; B mucosal incision was performed at approximately 3 cm above the diverticulum; C muscle fibre exposure of intervertebral ridge within submucosal tunnel; D muscle fibres of the septum were completely dissected down to the bottom of the diverticulum and through to the normal oesophageal muscle; E mucosal closure with clips
Postprocedural management
After the procedure, all patients fasted for 24 h and were treated with acid suppression and anti-infection agents for 2–3 days. If no fever, chest pain or other discomfort was found, semifluid was taken orally on POD (postoperative day) 1.
Outcome measures and follow-up
The primary outcomes were technical success (defined as achievement of complete septotomy) and clinical success (defined as improvements in symptom scores after the procedure). The secondary endpoints included length of hospital stay (LOS), procedure time, and intraoperative and postoperative adverse events (AEs), according to the National Cancer Institute Common Terminology Criteria (NCI-CTCAE ver. 4.0).
Follow-up included the following timepoints: postoperative 1 month, 6 months, 12 months, and once a year from the second year. Upper digestive tract angiography, endoscopy and symptom scoring were performed 30 days after D-POEM. Clinical symptoms were assessed by telephone or outpatient follow-up every 6 months until 1st April 2023. If the symptom score was significantly worse than before, angiography and endoscopy were essential, and oesophageal HRM was performed when necessary.
The symptoms were scored using the modified Eckardt score: dysphagia, heartburn, vomiting/reflux, weight loss, and retrosternal pain on a scale of 0–3. The total scores range from 15 to 0, with higher scores indicating more severe symptoms. Patients scoring ≤ 3 points after D-POEM or reduced by ≥ 5 points before D-POEM were considered to have received effective treatment; otherwise, symptoms were deemed to have recurred. Those patients who refused to follow up by telephone or lost contact when their phone number changed were deemed as withdrawn.
Statistical analysis
Categorical data are expressed herein as counts and percentages. Quantitative data are expressed as the mean ± SD or median (range). Categorical data were compared between groups by Fisher’s exact test or the chi-square test; for quantitative data with a nonnormal distribution, the nonparametric Mann–Whitney U test was used. Multivariate logistic regression analysis was performed for the factors with statistical significance in univariate analysis. Analyses were performed using SPSS 26.0 statistical software (IBM, NY, United States). P < 0.05 was considered to indicate significance.
Results
Patient characteristics
A total of 34 patients with symptomatic oesophageal diverticula were enrolled (Table 1). Four patients had coexistent achalasia. There were 19 (55.9%) males and 15 (44.1%) females, with a median age of 63 years (range 39–92 years). Twelve (35.3%) patients were diagnosed with ZD, 12 (35.3%) with MED, and 10 (29.4%) with ED. There were 30 (88.2%) cases of a single diverticulum and 4 (11.8%) cases of multiple diverticula (2 diverticula, n = 3; 3 diverticula, n = 1). The median disease duration was 33 months (range 3–168 months). Nineteen (55.9%) patients had drug treatment, including PPIs and prokinetics. The median preprocedure Eckardt score was 8.59 (range 5–13).
Early outcomes
D-POEM was performed successfully in all 34 patients, with a median procedure time of 39.15 min. Four patients who had coexistent achalasia underwent myotomy extending to the lower oesophageal sphincter (LES) to treat the motility dysfunction associated with the diverticulum. Subcutaneous emphysema occurred in 5 patients (14.7%), while mucosal injury occurred in 1 patient (2.9%). No intraoperative or postoperative perforation, haemorrhage, or any other severe AEs were observed. All patients resumed a liquid diet 24 h after the operation and gradually transitioned to semiliquids. The median LOS was 6 (range 4–10) days.
Follow-up
The median length of follow-up was 47.2 months (range 36–84 months). No patients were lost to follow-up. The median Eckardt score at 1 month post-procedure was 2.56, while it was 2.09 at 6 months, 2.21 at 12 months, 2.15 at 24 months, and 2.21 at 36 months. There was a significant reduction in the mean Eckardt score at 1 and 6 months compared to baseline (Fig. 2). The clinical success rates at 1, 6, 12, 24 and 36 months were 97.1%, 97.1%, 94.1%, 91.2%, and 88.2%, respectively. Until the last follow-up, 4 patients experienced symptom relapse, with a total clinical success rate of 88.2%. D-POEM was performed twice in 2 cases. There was no impact of gender, age, BMI index, drug treatment, number or type of diverticulum on the clinical outcome according to univariate analysis (Table 2). A long disease duration, a high Eckardt score, and coexistence of achalasia were identified as risk factors for symptomatic recurrence by multivariable or univariate analysis using the Cox model (Table 3).
Discussion
The traditional therapy of oesophageal diverticulum contains open surgery, a rigid endoscope, and a flexible endoscope [9]. Since 1995, flexible endoscopic septum division (FESD) has been identified as a preferred option for treating symptomatic ZD [10, 11]. Nevertheless, subsequent trials reported that the median clinical recurrence rate of FESD reached 35% [2, 9, 12, 13]. Submucosal tunnelling endoscopic septum division (STESD), a derivative technique from POEM, first reported by Li et al. in 2016, showed favourable short-term outcomes for patients with oesophageal diverticula [7]. Afterwards, case series have shown promising results for its use in oesophageal diverticulum. However, the medium- and long-term follow-up results, especially the recurrence rate of this treatment, are still undetermined.
In the current research, 34 patients with oesophageal diverticula were followed for at least 3 years. None of them withdrew or was lost to follow-up. The mean Eckardt scores of patients after D-POEM were significantly reduced compared to baseline, and the total clinical success rate was 100%, which was consistent with previous results. Until the last follow-up, the total clinical success rate of our study was 88.2%. In terms of safety, during a median procedure time of 39.15 min, 5 patients exhibited subcutaneous emphysema, while 1 had mucosal injury. No severe AEs were observed.
In this study, four patients suffered symptom relapse at 1, 12, 22, and 40 months postoperatively. Two patients who experienced recurrence received D-POEM twice, with no complications observed. The Eckardt score was reduced and maintained at 3–4 until the latest date. Based on the multivariable analysis, a long disease duration, a high Eckardt score, and coexistence of achalasia were deemed risk factors for symptomatic recurrence.
To date, only a few studies have reported symptom recurrence. Zhang et al. followed up 21 cases of oesophageal diverticulum with D-POEM for 39 months (range 12–63) and found 1 (4.8%) symptom relapse [14]. Another study showed that 15 of 119 patients with ZD (12.6%) who received Z-POEM experienced symptom recurrence after a mean follow-up of 282 days [15]. In a multicentre international retrospective study of 75 patients with ZD, 3.2% of them relapsed 12 months after Z-POEM [13]. The inconsistent recurrence rate among reported studies may account for the diverse follow-up periods and recurrence definitions. Large sample studies and long-term follow-up are needed to summarize the recurrence rate and analyse the associated risk factors for recurrence.
Past studies have compared the size of diverticula before and after D-POEM and found a significantly reduced depth after the procedure [16,17,18]. Nevertheless, it is undetermined whether the size of the diverticulum affects the patient’s final prognosis. In our study, we did not record the size in particular. This was because we thought that the measurement of the diverticulum was more or less influenced by the individual differences among examiners. In addition, we found that the comparison of preoperative and postoperative size was not obvious. This was also verified in another study reported by Zhang et al. [14]. In the follow-up of our study, we always found an asymptomatic residual diverticulum in its original position. However, we only dealt with the residual diverticulum that had food retention.
The key point of D-POEM is to achieve complete septum division [19]. Although D-POEM has been considered superior to previous treatments, it can supply adequate septum exposure and achieve complete septotomy [6]. In clinical practice, we found that some patients suffer rumination and reflux after D-POEM. Gastroscopy revealed food retention in a residual diverticulum. We thought that simply cutting the fundus of the septum was inadequate. Therefore, in this circumstance, we modified the surgical approach, incised the upper and lower muscles of the diverticulum simultaneously, and excised the excess muscle in the centre. It has also been proven that D-POEM is feasible in patients with recurrent symptoms after prior surgical or endoscopic interventions [20]. To our knowledge, the prognosis for patients undergoing modified reoperation is satisfactory until the end of follow-up.
The other key step is to locate the septum [21], especially to ZD. Sometimes, it is not easy to perform submucosal tunnelling for diverticula located in the upper oesophagus. We believe that appropriate entry proximal to the diverticulum is important. In addition, it is vital to obtain sufficient submucosal blebs to give enough space for submucosal entry. A new technique called endoscopic transversal incision and longitudinal septostomy (TILS) was first reported by Hu et al., which does not require a submucosal tunnel and makes a transverse incision on the diverticulum septum [22]. They believed that TILS provided a large operational space and better surgical view, precisely achieving a complete and accurate septostomy. However, this was a preliminary attempt at a single centre, and further clinical studies with more patients are needed.
Oesophageal diverticula have been associated with motility disorders [23,24,25]. The mainstay of this condition is laparoscopic diverticulectomy, myotomy and anterior fundoplication [26]. However, due to the relatively high complications, this surgery has been gradually phased out. Some researchers proposed S-POEM (salvage POEM), which only performed myotomy of the LES, leaving the diverticulum intact [27, 28]. Others preferred POEM with concurrent diverticulotomy [29]. Demeter et al. performed modified S-POEM for patients with epiphrenic diverticula and achalasia [29]. Their approach to myotomy of the LES was according to the location of the diverticulum. If the diverticulum was at the 2–5 O’clock position, posterior myotomy was performed at the 6–8 O’clock position. If the diverticulum was at the 7–10 O’clock position, anterior myotomy was performed at the 1–2 O’clock position. The main concern of this approach was reflux oesophagitis, which was reported in approximately 30% of patients [29]. Here, we performed myotomy extending to the LES for patients with oesophageal diverticulum and achalasia and showed a fair prognosis. This is only our preliminary experience, and more studies are needed to explore the proper approach for particular populations.
In conclusion, our data showed that D-POEM is an effective and safe treatment modality for oesophageal diverticulum that can provide durable medium-term clinical benefits in patients with symptomatic oesophageal diverticula.
References
Chan DSY, Foliaki A, Lewis WG, Clark GWB, Blackshaw G (2017) Systematic review and meta-analysis of surgical treatment of non-Zenker’s oesophageal diverticula. J Gastrointest Surg 21:1067–1075
Aiolfi A, Scolari F, Saino G, Bonavina L (2015) Current status of minimally invasive endoscopic management for Zenker diverticulum. World J Gastrointest Endosc 7:87–93
Zeng X, Bai S, Zhang Y, Ye L, Yuan X, Hu B (2020) Peroral endoscopic myotomy for the treatment of esophageal diverticulum: an experience in China. Surg Endosc 35(5):1990–1996. https://doi.org/10.1007/s00464-020-07593-6
Aravinthan A, Nikolic M, Ouyang X, Lee YM (2012) The hidden cause of dysphagia—epiphrenic diverticulum and esophageal motility disorders. Can J Gastroenterol 26:68–69
do Nascimento FA, Lemme EM, Costa MM (2006) Esophageal diverticula: pathogenesis, clinical aspects, and natural history. Dysphagia 21:198–205
Nabi Z, Nageshwar Reddy D, Ramchandani M (2018) Recent advances in third-space endoscopy. Gastroenterol Hepatol 14:224–232
Li QL, Chen WF, Zhang XC, Cai MY, Zhang YQ, Hu JW, He MJ, Yao LQ, Zhou PH, Xu MD (2016) Submucosal tunneling endoscopic septum division: a novel technique for treating Zenker’s diverticulum. Gastroenterology 151:1071–1074
Li X, Zhang W, Yang J, Wang X, Dang Y, Hu B, Cai Q, Zhou P, Zhang G (2019) Safety and efficacy of submucosal tunneling endoscopic septum division for epiphrenic diverticula. Endoscopy 51:1141–1145
Ishaq S, Hassan C, Antonello A, Tanner K, Bellisario C, Battaglia G, Anderloni A, Correale L, Sharma P, Baron TH, Repici A (2016) Flexible endoscopic treatment for Zenker’s diverticulum: a systematic review and meta-analysis. Gastrointest Endosc 83(1076–1089):e1075
Mulder CJ, den Hartog G, Robijn RJ, Thies JE (1995) Flexible endoscopic treatment of Zenker’s diverticulum: a new approach. Endoscopy 27:438–442
Ishioka S, Sakai P, Maluf Filho F, Melo JM (1995) Endoscopic incision of Zenker’s diverticula. Endoscopy 27:433–437
Halland M, Grooteman KV, Baron TH (2016) Flexible endosopic management of Zenker’s diverticulum: characteristics and outcomes of 52 cases at a tertiary referral center. Dis Esophagus 29:273–277
Yang J, Novak S, Ujiki M, Hernandez O, Desai P, Benias P, Lee D, Chang K, Brieau B, Barret M, Kumta N, Zeng X, Hu B, Delis K, Khashab MA (2020) An international study on the use of peroral endoscopic myotomy in the management of Zenker’s diverticulum. Gastrointest Endosc 91:163–168
Zhang DF, Chen WF, Wang Y, Xu MD, Zhang XC, Cai MY, Chen SY, Zhong YS, Zhang YQ, Zhang GL, Zhou PH, Li QL (2022) Submucosal tunneling endoscopic septum division for esophageal diverticulum with a median follow-up of 39 months: a multicenter cohort study. Gastrointest Endosc 96(4):612-619.e1
Al Ghamdi SS, Farha J, Moran RA, Pioche M, Moll F, Yang DJ, Hernandez Mondragon OV, Ujiki M, Wong H, Tantau A, Sedarat A, Fejleh MP, Chang K, Lee DP, Nieto JM, Andrawes S, Ginsberg GG, Saumoy M, Bapaye A, Dashatwar P, Aghaie Meybodi M, Lopez AC, Sanaei O, Yousaf MN, Jovani M, Ichkhanian Y, Brewer Gutierrez OI, Kumbhari V, O’Rourke AK, Lentsch EJ, Elmunzer BJ, Khashab MA (2022) Zenker’s peroral endoscopic myotomy, or flexible or rigid septotomy for Zenker’s diverticulum: a multicenter retrospective comparison. Endoscopy 54:345–351
Maydeo A, Patil GK, Dalal A (2019) Operative technical tricks and 12-month outcomes of diverticular peroral endoscopic myotomy (D-POEM) in patients with symptomatic esophageal diverticula. Endoscopy 51:1136–1140
Yang J, Zeng X, Yuan X, Chang K, Sanaei O, Fayad L, Kumbhari V, Singh V, Kalloo AN, Hu B, Khashab MA (2019) An international study on the use of peroral endoscopic myotomy (POEM) in the management of esophageal diverticula: the first multicenter D-POEM experience. Endoscopy 51:346–349
Basile P, Gonzalez JM, Le Mouel JP, Irarrazaval R, Caillo L, Barthet M (2020) Per-oral endoscopic myotomy with septotomy for the treatment of distal esophageal diverticula (D-POEM). Surg Endosc 34:2321–2325
Yuan Y, Zhao YF, Hu Y, Chen LQ (2013) Surgical treatment of Zenker’s diverticulum. Dig Surg 30:207–218
Sanaei O, Ichkhanian Y, Mondragon OVH, Nieto J, Krishnan A, Tantau M, Tantau A, Desai PN, Ginsberg GG, Saumoy M, Deshmukh A, Attaar M, Farha J, Jovani M, Al-Ghamdi SS, Ujiki M, Khashab MA (2021) Impact of prior treatment on feasibility and outcomes of Zenker’s peroral endoscopic myotomy (Z-POEM). Endoscopy 53:722–726
Samanta J, Mandavdhare HS, Kumar N, Kumar MP, Jafra A, Chauhan R, Gupta P, Kumar KH, Singh H, Dutta U, Kochhar R (2022) Per oral endoscopic myotomy for the management of large esophageal diverticula (D-POEM): safe and effective modality for complete septotomy. Dysphagia 37:84–92
Hu H, Wang M, Zhu L, Zhou P (2020) Endoscopic transversal incision and longitudinal septostomy (TILS): an updated technique for treating esophageal diverticulum. Dig Dis 38:550–554
Carlson DA, Gluskin AB, Mogni B, Koo J, Sood R, Lin Z, Pandolfino JE (2016) Esophageal diverticula are associated with propagating peristalsis: a study utilizing high-resolution manometry. Neurogastroenterol Motil 28:392–398
Stefanidis D, Richardson W, Farrell TM, Kohn GP, Augenstein V, Fanelli RD, Society of American Gastrointestinal and Endoscopic Surgeons (2012) SAGES guidelines for the surgical treatment of esophageal achalasia. Surg Endosc 26:296–311
Orlandini B, Barret M, Guillaumot MA, Leandri C, Leblanc S, Prat F, Chaussade S (2020) Per-oral endoscopic myotomy for esophageal diverticula with or without esophageal motility disorders. Clin Res Hepatol Gastroenterol 44:82–89
Zaninotto G, Portale G, Costantini M, Zanatta L, Salvador R, Ruol A (2011) Therapeutic strategies for epiphrenic diverticula: systematic review. World J Surg 35:1447–1453
Sato H, Sato Y, Takeuchi M, Takahashi K, Takeda SR, Inoue H, Kobayashi M (2015) Salvage peroral endoscopic myotomy for esophageal diverticulum. Endoscopy 47(Suppl 1 UCTN):E14–E15
Demeter M, Banovcin P Jr, Duricek M, Kunda R, Hyrdel R (2018) Peroral endoscopic myotomy in achalasia and large epiphrenic diverticulum. Dig Endosc 30:260–262
Demeter M, Duricek M, Vorcak M, Hyrdel R, Kunda R, Banovcin P (2020) S-POEM in treatment of achalasia and esophageal epiphrenic diverticula—single center experience. Scand J Gastroenterol 55:509–514
Acknowledgements
We would like to thank the group hospitals for their assistance, and we thank Dr. Sachin Mulmi Shrestha for proofreading the manuscript.
Funding
This study was supported by Jiangsu Science and Technology Project, Innovative Team Project (No. 2017ZXK7QW08), National Natural Science Foundation of China (No. 81570503); and Project founded by China Postdoctoral Science Foundation (No. 347072) and Project funded by China Postdoctoral Science Foundation (No. 2023M730587).
Author information
Authors and Affiliations
Contributions
LHR contributed to data collection, data analysis and manuscript writing; HY and YZ contributed to data collection and data analysis; WHX contributed to data analysis; YL and YL contributed to technical guidance; WXC, XFC, BW, and LP contributed to data collection; RHS contributed to the conception and design of the study and performed the D-POEM procedure. All authors contributed to the revision and gave their final approval of the manuscript.
Corresponding author
Ethics declarations
Disclosures
Lihua Ren, Hui Ye, Ye Zhu, Weihua Xie, Yan Liang, Yang Liu, Jingwu Dong, Weixu Chen, Xinfu Chen, Bin Wang, Liang Pan and Ruihua Shi have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ren, L., Ye, H., Zhu, Y. et al. Diverticular peroral endoscopic myotomy (D-POEM) for symptomatic oesophageal diverticulum: a multicentre cohort study with a minimum follow-up of 3 years. Surg Endosc 38, 253–259 (2024). https://doi.org/10.1007/s00464-023-10471-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10471-6