Abstract
Background
Laparoscopic gastrectomy is a common procedure for early gastric cancer treatment. Improving postoperative pain control enhances patient recovery after surgery. The use of multimodal analgesia can potentially enhance the analgesic effect, minimize side effects, and change the postoperative management. The purpose of this study was to evaluate and compare the efficacies of the use of patient-controlled intravenous analgesia with regular acetaminophen (PCIA + Ace) and patient-controlled thoracic epidural analgesia (PCEA) for postoperative pain control.
Methods
We retrospectively collected the data of 226 patients who underwent laparoscopic distal gastrectomy (LDG) with delta-shaped anastomosis between 2016 and 2019. After 1:1 propensity-score matching, we compared 83 patients who used PCEA alone (PCEA group) with 83 patients who used PCIA + Ace (PCIA + Ace group). Postoperative pain was assessed using a numeric rating scale (NRS) with scores ranging from 0 to 10. An NRS score ≥ 4 was considered the threshold for additional intravenous rescue medication administration.
Results
Although NRS scores at rest were comparable between the PCEA and PCIA + Ace groups, NRS scores of patients in the PCIA + Ace group during coughing or movement were significantly better than those of patients in the PCEA group on postoperative days 2 and 3. The frequency of additional rescue analgesic use was significantly lower in the PCIA + Ace group than in the PCEA group (1.1 vs. 2.7, respectively, p < 0.001). The rate of reduction or interruption of the patient-controlled analgesic dose was higher in the PCEA group than in the PCIA + Ace group (74.6% vs. 95.1%, respectively, p = 0.0002), mainly due to hypotension occurrence in the PCEA group. Physical recovery time, postoperative complication occurrence, and liver enzyme elevation incidence were not significantly different between groups.
Conclusions
PCIA + Ace can be safely applied without an increase in complications or deterioration in gastrointestinal function; moreover, PCIA + Ace use may provide better pain control than PCEA use in patients following LDG.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Globally, gastric cancer has the sixth highest incidence and is the second leading cause of death among all cancers [1]. Gastrectomy is a commonly performed procedure for the treatment of gastric cancer. The use of improved surgical and minimally invasive techniques can reduce the occurrence of postoperative complications, thereby contributing to survival prognosis [2]. In addition, the enhanced recovery after surgery (ERAS) protocol highlights that perioperative management also leads to a better survival prognosis [3, 4]. Furthermore, pain reduction can enhance early ambulation and gastrointestinal function recovery, which leads to complication improvement, patient satisfaction, shorter hospital stays, and reduced healthcare costs [5,6,7,8].
The American Society of Anesthesiologists (ASA) Task Force on Acute Pain and the ERAS protocol recommend the use of thoracic epidural analgesia for perioperative pain management in patients undergoing open abdominal surgery [7, 9]. The use of patient-controlled thoracic epidural analgesia (PCEA) has been shown to improve postoperative pain scores and physical findings more effectively and quickly than the use of patient-controlled intravenous analgesia (PCIA) alone in patients undergoing open surgery for gastric cancer [7, 10,11,12]. Presently, the use of PCEA is generally considered to be superior to that of PCIA alone in terms of postoperative pain control and gastrointestinal function recovery [13,14,15]. However, several studies have reported that the use of PCIA alone for laparoscopic colon surgery is promising, as it induces fewer complications and enhances pain control; these findings are different from those obtained when using PCEA for open surgery [16]. Furthermore, a recent study reported that the use of PCIA alone in combination with regular acetaminophen (PCIA + Ace) was superior to PCEA use in terms of pain control after laparoscopic colon surgery [17]. Laparoscopic surgery is advantageous in that it induces less pain, faster gastrointestinal function recovery, and fewer postoperative complications [5, 18, 19], and thus, PCIA + Ace use is proposed as a promising and novel emerging tool for pain control after laparoscopic surgery. The use of PCIA alone is effective in pain control and gastrointestinal function recovery after laparoscopic gastrectomy; these effects are similar when PCIA alone is used for laparoscopic colon surgery, although the advantages of using PCIA alone or PCIA + Ace compared to that of using PCEA have remained elusive.
The application of recently developed multimodal analgesic methods has changed the course of postoperative pain management. That is, a combination of various analgesic methods is expected to enhance the analgesic effect, minimize side effects, and reduce the pain score and opioid dose [20,21,22]. Acetaminophen has been commonly used for postoperative analgesia, and its safety is guaranteed [23]. In addition, the combined use of acetaminophen with PCIA has advantages such as postoperative pain score improvement, rescue frequency reduction, gastrointestinal function recovery, and reduced postoperative nausea and vomiting (PONV) [24,25,26,27]. In this study, we performed propensity-score matching to evaluate and compare the efficacies of PCIA + Ace and PCEA on postoperative pain score reduction, gastrointestinal function recovery, and postoperative complications in patients who underwent radical laparoscopic distal gastrectomy (LDG) with delta-shaped anastomosis.
Materials and methods
Patient selection and study setting
In this retrospective study conducted in our institution between April 2016 and December 2019, we included consecutive patients who underwent radical LDG with delta-shaped anastomosis for gastric cancer [28]. We switched trainee surgeons in April 2018 for annual staff reassignment. Thus, postoperative analgesic methods were changed from epidural to intravenous anesthesia depending on the preference of each surgical team. PCEA was preferred between April 2016 and April 2018, whereas PCIA + Ace was preferred between May 2018 and December 2019. We evaluated and compared the efficacy of the use of PCIA + Ace versus that of PCEA for postoperative pain control. To harmonize the baseline data related to anesthesia use, we excluded patients who used both PCEA and PCIA alone, PCEA with regular intravenous acetaminophen, and PCIA alone, as well as those with missing data. Clinical data such as physical and laboratory findings were obtained retrospectively from medical records. We regularly scheduled blood tests on postoperative days (PODs) 1, 3, 5, and 7. Postoperative pain scores were measured using a numeric rating scale (NRS) with scores ranging from 0 to 10. Wound pain was assessed at rest or at the time of maximum pain during the day. The moments of maximum wound pain were claimed during body movement and/or coughing. An NRS score ≥ 4 was considered the threshold for additional intravenous rescue medication administration. All patients were provided informed consent for surgery and anesthesia, and the study was approved by our institutional ethics committee (approval number 19-226).
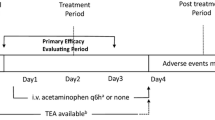
Anesthesia/multimodal analgesia protocol
Based on the baseline common analgesic protocol, patients were divided into PCEA and PCIA + Ace groups. In PCEA patients, the epidural catheter was inserted into the T7-8 or T8-9 spinal level for anesthesia induction, after which general anesthesia was administered. Fentanyl (1.0 mg, 20 mL), levobupivacaine (200 mg, 200 mL), and normal saline (80 mL) were mixed and continuously infused through the epidural catheter at a starting rate of 4 mL/h until POD3. In PCIA + Ace patients, 1.0 mg fentanyl (20 mL) and normal saline (80 mL) were mixed and continuously infused intravenously at a starting rate of 2 mL/h with 15–20 mg/kg regular intravenous acetaminophen (Acelio bag for intravenous injection 1000 mg; TERUMO, Tokyo, Japan) every 6 h until POD2. In the postoperative period, patients were allowed to administer patient-controlled analgesia (PCA). PCA was reduced or discontinued whenever hypotension or PONV occurred. Additionally, for patients with NRS scores ≥ 4 or requiring rescue analgesia, intravenous acetaminophen (15–20 mg/kg) or intravenous flurbiprofen (50 mg/time) was used as a rescue analgesic; the choice between the two analgesics was made based on the presence of contraindications such as allergy or renal dysfunction. Moreover, regular oral non-steroidal anti-inflammatory drugs (NSAIDs) such as celecoxib (400 mg/day), a selective COX-2 inhibitor, or oral acetaminophen (1200 mg/day) was added for patients with persistent pain.
Operative procedure
According to the 4th and 5th editions of the Japanese Gastric Cancer Treatment guidelines, we performed LDG with extended systemic lymphadenectomy (D2) or less extensive lymphadenectomy (< D2) based on the gastric cancer clinical stage. Surgical quality was guaranteed by a board-certified chief trainer who was accredited by the Japan Society for Surgical Endoscopy. To standardize the surgical technique and wound incision, all patients underwent delta-shaped reconstruction. We inserted a 12 mm trocar through the umbilical pathway, and then arranged two pieces of 5 mm trocars and two pieces of 12 mm trocars in the form of an inverted trapezoid. After gastrectomy, we extended the umbilical incision to approximately 40 mm and to exteriorize the gastric specimens. Delta-shaped reconstruction using double stapling was performed completely in the peritoneal cavity. The abdominal wall fascia at the 12 mm port site and the umbilical wound were closed with absorbable sutures.
Statistical analysis
Categorical variables were compared using the chi-squared tests. Continuous variables were expressed as mean and standard deviation and compared using the Mann–Whitney U test. A p value < 0.05 was considered statistically significant. To reduce bias related to the non-randomized and observational study design, we applied propensity-score-matching analyses to the PCEA and PCIA + Ace groups. Propensity scores were estimated using a logistic regression model based on the following preoperative characteristics: age, sex, body mass index (kg/m2), ASA stage, clinical stage, and lymphadenectomy. Moreover, 1:1 matching was performed between the two groups using a 0.1 caliper width, and 83 matched patient pairs were analyzed. Correlation between the matched pairs was analyzed using JMP software (version 14; SAS Institute, Cary, NC).
Results
Patient characteristics and LDG outcomes between groups
This study included 238 patients with clinical stage IA/IB/IIA gastric cancer who underwent LDG. Figure 1 shows the participant flow in this study. There were no significant between-group differences in age, sex, ASA physical status, clinical tumor stage, or lymphadenectomy. However, the anesthesia induction time was significantly shorter in the PCIA + Ace group than in the PCEA group (39.4 ± 5.5 vs. 52.3 ± 7.3, respectively; p < 0.001). The operative time was higher in the PCIA + Ace group (234.3 ± 47.6 vs. 261.2 ± 51.9, respectively; p = 0.0002). There were no significant between-group differences in intraoperative findings (fluid infusion volume and urinary output) or surgical outcomes (blood loss and the number of perioperative blood transfusions) (Table 1).
Differences in pain-related factors between groups
Patients in both the PCEA and PCIA + Ace groups underwent a common method of analgesia at baseline and an additional unique method of analgesia whenever the NRS pain score was high (≥ 4) (Table 2). Table 3 shows a comparison of pain-related factors between groups after LDG. Resting NRS scores from POD1 to POD3 were not significantly different between the two groups; however, the NRS scores during coughing or movement on POD2 and POD3 were significantly better in the PCIA + Ace group than in the PCEA group (3.7 ± 1.3 vs. 4.6 ± 1.8 and 3.2 ± 1.3 vs. 4.0 ± 1.8, p = 0.0006 and p = 0.004, respectively). Moreover, the number of additional oral medications used at POD2 was significantly smaller in the PCIA + Ace group than in the PCEA group (23 vs. 38, respectively, p = 0.0157); further, additional intravenous rescue medication use was significantly less frequent in the PCIA + Ace group than in the PCEA group (mean numbers: 1.2 vs. 2.7, respectively, p < 0.0001). Nevertheless, patients in both groups needed oral medication rescue until POD3.
Difference in PCA-related complications between groups
PONV was observed in both groups, with no significant between-group difference in frequency. In the PCEA group, 20 patients (24.9%) had their PCA dose reduced or interrupted, mainly due to hypotension; however, four patients (4.8%) who received PCIA + Ace interrupted PCA due to PONV (2.4% vs 4.8%, p = 0.405). The final rates of initial PCA dose continuation were 74.6% and 95.1% in the PCEA and PCIA + Ace groups, respectively (p = 0.0002).
Physical and laboratory findings between groups
There was no significant between-group difference in postoperative recovery in terms of the time to first ambulation and gastrointestinal movement recuperation (flatus and defecation) (Table 4). However, body temperatures on POD1 and POD2 were significantly lower in the PCIA + Ace group than in the PCEA group (37.1 ± 0.4 vs. 37.5 ± 0.5 and 37.0 ± 0.4 vs. 37.2 ± 0.4, p < 0.0001 and p = 0.002, respectively), although there was no significant between-group difference in body temperature on POD3. Urethral catheter removal was performed significantly earlier in the PCIA + Ace group than in the PCEA group (p < 0.0001). Furthermore, the white blood cell (WBC) count and C-reactive protein (CRP) levels were significantly higher in the PCIA + Ace group than in the PCEA group on POD1 (Table 4; p = 0.002 and p < 0.001, respectively). However, the abovementioned parameters became comparable in both groups on POD3 and POD5. Alanine aminotransferase (ALT) levels were almost equal in both groups, except on POD5 (p = 0.048).
Postoperative complications between groups
Table 5 shows a comparison of postoperative complications between the PCEA and PCIA + Ace groups. There were no between-group differences in the incidences of early (POD1 to POD3) and late (POD5 to POD7) abnormal liver enzyme (ALT and aspartate aminotransferase) elevations, based on the Common Terminology Criteria for Adverse Events (CTCAE). Both groups had almost equal incidences of infection-related postoperative complications such as abdominal abscess, anastomotic leakage, and pulmonary infection.
Discussion
In this study, we used propensity-score matching to evaluate and compare the efficacies of PCIA + Ace and PCEA application after LDG on postoperative pain control. Compared with PCEA use, PCIA + Ace use was found to reduce the NRS score during movement or coughing and decrease the number of rescue analgesia medications used without an increase in postoperative complications or deterioration in gastrointestinal function.
The ASA Task Force on Acute Pain guidelines state that it is crucial to control postoperative pain until POD3 [9]. PCEA assures better pain control, and thus is the most common anesthetic method for patients undergoing open gastrectomy [10]. However PCEA has disadvantages including longer anesthesia induction time and a predisposition to complications such as hypotension, urinary retraction, hematoma formation, and neuropathy [11, 12]. The smaller skin incision performed during laparoscopic gastrectomy results in less pain than in open gastrectomy [5]. However, few studies have reported better pain control with quick and simple administration of fentanyl as PCIA alone than PCEA [13, 14]. Our study demonstrated that NRS scores during coughing or movement on POD2 and POD3 were significantly better in the PCIA + Ace group than in the PCEA group (p = 0.0006 and p = 0.004, respectively), although the NRS scores at rest from POD1 to POD3 were comparable between the two groups.
The mechanisms of action of acetaminophen in fever alleviation and analgesia have not been fully elucidated; nevertheless, our clinical data demonstrate that acetaminophen use alleviated fever. Acetaminophen exerts its antipyretic effect by acting on the hypothalamus temperature control center, which triggers pain threshold elevation in the thalamus and cerebral cortex [29]. In contrast, fentanyl is a μ-opioid receptor agonist which acts on the brainstem, medial thalamus, and spinal cord [30]. The trigger points of fentanyl and acetaminophen do not overlap. Therefore, multimodal analgesia, which combines intravenous acetaminophen and fentanyl, is beneficial in terms of its synergistic effects and induces better patient pain control [20, 21]. Enhanced pain control is also associated with a decrease in the number of rescues, especially using NSAIDs. This reduces labor and treatment costs associated with rescue medication use. In addition, the frequent use of non-selective NSAIDs for rescue has been suggested to increase the incidence of anastomotic leakage and surgical-site bleeding [31, 32]. This may be related not only to pain control but also to a reduction in postoperative complications.
Minimizing perioperative opioid use through multimodal analgesia is one of the goals of ERAS. In this study, although the total opioid dose remained same in both groups, pain control was better with the less invasive PCIA + Ace. Particularly in laparoscopic surgery, combining regular acetaminophen administration with transverse abdominis plane (TAP) block by non-opioid analgesics, such as gabapentinoids, ketamine and lidocaine, also has the potential to achieve effective pain control, and such new approach is expected to further reduce opioid use and opioid associated side effects [33,34,35].
In terms of PCA-related adverse events, hypotension was more common in the PCEA group. In the PCEA group, 20 patients (24.9%) experienced a dose reduction or analgesic discontinuation due to hypotension. Although epidural anesthesia directly affects the spinal cord to produce an analgesic effect, it also triggers peripheral vasodilation, which reduces blood pressure. Thus, it may be necessary to change the flow rate of the anesthetic or discontinue its use. PCA dose reduction or discontinuation may cause insufficient pain control, and thus may need more frequent rescue attempts. Postoperative hypotension may also increase the risk of falls, thereby interfering with early postoperative ambulation, which is inconvenient for postoperative management.
Nevertheless, four patients (4.8%) discontinued PCA in the PCIA + Ace group due to PONV. Intravenous fentanyl extensively affects the brainstem and spinal cord, and hence may accidently induce PONV and paralytic ileus [36]. Although it has been reported that acetaminophen reduces PONV [24, 25], no clear inhibitory effect of acetaminophen on PONV could be confirmed in this study. However, there were no obvious differences in the incidence of PONV or gastrointestinal function recovery between the groups. Decreased NRS scores during movement and early urinary catheter removal promote ambulation; hence, these factors may be attributed to gastrointestinal function recovery [8].
Postoperative complications, including liver enzyme level abnormalities, were comparable in both groups. Thus, especially for LDG, liver enzyme level elevation until POD3 is more likely caused by liver retraction than medication use [37]. Moreover, drug-induced liver enzyme level elevation is apparent on POD5 to POD7 due to drug dose accumulation [38]. In this study, ALT was temporarily slightly elevated in the PCIA + Ace group mainly due to regular acetaminophen use on POD5 but did not differ significantly from the PCEA group, based on CTCAE grade. Acetaminophen can be safely used if an adequate dose is prescribed and administered for a short period of time (until POD2) [27, 38, 39].
Furthermore, on POD1, inflammation markers such as WBC count and CRP levels were significantly lower in the PCEA group than in the PCIA + Ace group. Intraoperative PCEA administration triggers cortisol level reduction and inflammatory marker level suppression, thereby decreasing the intraoperative and immediate postoperative stress response [40, 41]. Thus, the PCEA-induced suppression of inflammation may have an advantage on the body’s response against surgical stress. However, there was no increase in the occurrence of systemic complications such as anastomotic leakage, intraabdominal abscess, and deep vein thrombosis, and therefore there was no increase in hospitalization in our clinical setting.
In recent years, the number of patients with vascular comorbidities or obesity has increased. It is necessary for these patients to pause antiplatelet or anticoagulant oral medications and to resume them after surgery. In addition, perioperative deep venous thrombosis can be prevented using anticoagulant medications. Under the abovementioned circumstances, the risk of epidural approach complications associated with epidural catheter insertion and removal (such as hematoma formation) is expected to increase in patients using PCEA [42,43,44]. PCIA + Ace is simple and easy to administer with fewer complications, and it can replace PCEA based on efficacy and safety.
Our study has several limitations. First, we used propensity-score matching to balance patient background characteristics; however, the two groups were divided in a metachronous fashion in a single center. In effect, the two groups underwent a switch in trainee surgeons, which resulted in a significant increase in operative time, although intraoperative parameters such as blood loss were comparable between the two groups. Second, we focused on the delta reconstruction for LDG to achieve uniformity in the small umbilical incision, surgical technique, and operative time. However, under Roux-en-Y reconstruction or laparoscopic total gastrectomy, the umbilical incision may be slightly widened due to the nature of these techniques. Additional validation should be performed in multicenter studies to enhance the generalizability of our findings. Finally, we did not examine the incidence of PCA rescue use. There was a discrepancy between the actual and self-reported numbers of PCA rescues, although the total PCA dose was determined for all patients, and no patient received additional PCA doses.
In conclusion, we confirmed that PCIA + Ace use may provide better pain control compared to PCEA use in patients after LDG; moreover, PCIA + Ace can be safely administered without increasing the risk of complications or gastrointestinal function deterioration.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424
Hwang SI, Kim HO, Yoo CH, Shin JH, Son BH (2009) Laparoscopic-assisted distal gastrectomy versus open distal gastrectomy for advanced gastric cancer. Surg Endosc 23:1252–1258
Aoyama T, Yoshikawa T, Sato T, Hayashi T, Yamada T, Ogata T, Cho H (2019) Equivalent feasibility and safety of perioperative care by ERAS in open and laparoscopy-assisted distal gastrectomy for gastric cancer: a single-institution ancillary study using the patient cohort enrolled in the JCOG0912 phase III trial. Gastric Cancer 22:617–623
Beverly A, Kaye AD, Ljungqvist O, Urman RD (2017) Essential elements of multimodal analgesia in enhanced recovery after surgery (ERAS) guidelines. Anesthesiol Clin 35:e115–e143
Takiguchi S, Fujiwara Y, Yamasaki M, Miyata H, Nakajima K, Sekimoto M, Mori M, Doki Y (2013) Laparoscopy-assisted distal gastrectomy versus open distal gastrectomy. A prospective randomized single-blind study. World J Surg 37:2379–2386
Sakuramoto S, Yamashita K, Kikuchi S, Futawatari N, Katada N, Watanabe M, Okutomi T, Wang G, Bax L (2013) Laparoscopy versus open distal gastrectomy by expert surgeons for early gastric cancer in Japanese patients: short-term clinical outcomes of a randomized clinical trial. Surg Endosc 27:1695–1705
Hughes MJ, Ventham NT, McNally S, Harrison E, Wigmore S (2014) Analgesia after open abdominal surgery in the setting of enhanced recovery surgery: a systematic review and meta-analysis. JAMA Surg 149:1224–1230
Ohkura Y, Shindoh J, Ueno M, Iizuka T, Haruta S, Udagawa H (2018) A new postoperative pain management (intravenous acetaminophen: Acelio(R)) leads to enhanced recovery after esophagectomy: a propensity score-matched analysis. Surg Today 48:502–509
American Society of Anesthesiologists Task Force on Acute Pain Management (2012) Practice guidelines for acute pain management in the perioperative setting: an updated report by the American society of anesthesiologists task force on acute pain management. Anesthesiology 116:248–273
Wang L, Li X, Chen H, Liang J, Wang Y (2018) Effect of patient-controlled epidural analgesia versus patient-controlled intravenous analgesia on postoperative pain management and short-term outcomes after gastric cancer resection: a retrospective analysis of 3,042 consecutive patients between 2010 and 2015. J Pain Res 11:1743–1749
Zhu Z, Wang C, Xu C, Cai Q (2013) Influence of patient-controlled epidural analgesia versus patient-controlled intravenous analgesia on postoperative pain control and recovery after gastrectomy for gastric cancer: a prospective randomized trial. Gastric Cancer 16:193–200
Shi WZ, Miao YL, Yakoob MY, Cao JB, Zhang H, Jiang YG, Xu LH, Mi WD (2014) Recovery of gastrointestinal function with thoracic epidural vs. systemic analgesia following gastrointestinal surgery. Acta Anaesthesiol Scand 58:923–932
Cho JS, Kim HI, Lee KY, Son T, Bai SJ, Choi H, Yoo YC (2017) Comparison of the effects of patient-controlled epidural and intravenous analgesia on postoperative bowel function after laparoscopic gastrectomy: a prospective randomized study. Surg Endosc 31:4688–4696
Yanagimoto Y, Takiguchi S, Miyazaki Y, Mikami J, Makino T, Takahashi T, Kurokawa Y, Yamasaki M, Miyata H, Nakajima K, Mori M, Doki Y (2016) Comparison of pain management after laparoscopic distal gastrectomy with and without epidural analgesia. Surg Today 46:229–234
Kikuchi S, Kuroda S, Nishizaki M, Matsusaki T, Kuwada K, Kimura Y, Kagawa S, Morimatsu H, Fujiwara T (2019) Comparison of the effects of epidural analgesia and patient-controlled intravenous analgesia on postoperative pain relief and recovery after laparoscopic gastrectomy for gastric cancer. Surg Laparosc Endosc Percutan Tech 29:405–408
Levy BF, Scott MJ, Fawcett W, Fry C, Rockall TA (2011) Randomized clinical trial of epidural, spinal or patient-controlled analgesia for patients undergoing laparoscopic colorectal surgery. Br J Surg 98:1068–1078
Naito M, Sato T, Nakamura T, Yamanashi T, Miura H, Tsutsui A, Watanabe M (2017) Pain management using acetaminophen throughout postoperative course of laparoscopic colorectal surgery: a case-matched control study. Ann Med Surg (Lond) 17:38–42
Mochiki E, Nakabayashi T, Kamimura H, Haga N, Asao T, Kuwano H (2002) Gastrointestinal recovery and outcome after laparoscopy-assisted versus conventional open distal gastrectomy for early gastric cancer. World J Surg 26:1145–1149
Lee SJ, Hyung WJ, Koo BN, Lee JY, Jun NH, Kim SC, Kim JW, Liu J, Kim KJ (2008) Laparoscopy-assisted subtotal gastrectomy under thoracic epidural-general anesthesia leading to the effects on postoperative micturition. Surg Endosc 22:724–730
Brown EN, Pavone KJ, Naranjo M (2018) Multimodal general anesthesia: theory and practice. Anesth Analg 127:1246–1258
Kehlet H, Dahl JB (1993) The value of “multimodal” or “balanced analgesia” in postoperative pain treatment. Anesth Analg 77:1048–1056
Hausken J, Fretland AA, Edwin B, Andersen MH, Dagenborg VJ, Bjornelv GMW, Kristiansen R, Roysland K, Kvarstein G, Tonnessen TI (2019) Intravenous patient-controlled analgesia versus thoracic epidural analgesia after open liver surgery: a prospective, randomized, controlled, noninferiority trial. Ann Surg 270(2):193–199
Sinatra RS, Jahr JS, Reynolds LW, Viscusi ER, Groudine SB, Payen-Champenois C (2005) Efficacy and safety of single and repeated administration of 1 gram intravenous acetaminophen injection (paracetamol) for pain management after major orthopedic surgery. Anesthesiology 102:822–831
Apfel CC, Turan A, Souza K, Pergolizzi J, Hornuss C (2013) Intravenous acetaminophen reduces postoperative nausea and vomiting: a systematic review and meta-analysis. Pain 154:677–689
Ohkura Y, Haruta S, Shindoh J, Tanaka T, Ueno M, Udagawa H (2016) Effectiveness of postoperative intravenous acetaminophen (Acelio) after gastrectomy: a propensity score-matched analysis. Medicine (Baltimore) 95:e5352
Lee Y, Yu J, Doumouras AG, Ashoorion V, Gmora S, Anvari M, Hong D (2019) Intravenous acetaminophen versus placebo in post-bariatric surgery multimodal pain management: a meta-analysis of randomized controlled trials. Obes Surg 29:1420–1428
Kinoshita J, Fushida S, Kaji M, Oyama K, Fujimoto D, Hirono Y, Tsukada T, Fujimura T, Ohyama S, Yabushita K, Kadoya N, Nishijima K, Ohta T (2019) A randomized controlled trial of postoperative intravenous acetaminophen plus thoracic epidural analgesia vs. thoracic epidural analgesia alone after gastrectomy for gastric cancer. Gastric Cancer 22:392–402
Kanaya S, Gomi T, Momoi H, Tamaki N, Isobe H, Katayama T, Wada Y, Ohtoshi M (2002) Delta-shaped anastomosis in totally laparoscopic Billroth I gastrectomy: new technique of intraabdominal gastroduodenostomy. J Am Coll Surg 195:284–287
Smith HS (2009) Potential analgesic mechanisms of acetaminophen. Pain Phys 12:269–280
Trescot AM, Datta S, Lee M, Hansen H (2008) Opioid pharmacology. Pain Phys 11:S133-153
Hakkarainen TW, Steele SR, Bastaworous A, Dellinger EP, Farrokhi E, Farjah F, Florence M, Helton S, Horton M, Pietro M, Varghese TK, Flum DR (2015) Nonsteroidal anti-inflammatory drugs and the risk for anastomotic failure: a report from Washington state’s surgical care and outcomes assessment program (SCOAP). JAMA Surg 150:223–228
Mathiesen O, Wetterslev J, Kontinen VK, Pommergaard HC, Nikolajsen L, Rosenberg J, Hansen MS, Hamunen K, Kjer JJ, Dahl JB, Scandinavian Postoperative Pain Alliance (ScaPAlli) (2014) Adverse effects of perioperative paracetamol, NSAIDs, glucocorticoids, gabapentinoids and their combinations: a topical review. Acta Anaesthesiol Scand 58:1182–1198
Wick EC, Grant MC, Wu CL (2017) Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg 152:691–697
Li Z, Wang Q, Li B, Bai B, Zhao Q (2017) Influence of enhanced recovery after surgery programs on laparoscopy-assisted gastrectomy for gastric cancer: a systematic review and meta-analysis of randomized control trials. World J Surg Oncol 15:207
Robertson TC, Hall K, Bear S, Thompson KJ, Kuwada T, Gersin KS (2019) Transversus abdominis block utilizing liposomal bupivacaine as a non-opioid analgesic for postoperative pain management. Surg Endosc 33(8):2657–2662
de Boer HD, Detriche O, Forget P (2017) Opioid-related side effects: Postoperative ileus, urinary retention, nausea and vomiting, and shivering. A review of the literature. Best Pract Res Clin Anaesthesiol 31:499–504
Kinjo Y, Okabe H, Obama K, Tsunoda S, Tanaka E, Sakai Y (2011) Elevation of liver function tests after laparoscopic gastrectomy using a Nathanson liver retractor. World J Surg 35:2730–2738
Dart RC, Bailey E (2007) Does therapeutic use of acetaminophen cause acute liver failure? Pharmacotherapy 27:1219–1230
Watkins PB, Kaplowitz N, Slattery JT, Colonese CR, Colucci SV, Stewart PW, Harris SC (2006) Aminotransferase elevations in healthy adults receiving 4 grams of acetaminophen daily: a randomized controlled trial. JAMA 296:87–93
Moselli NM, Baricocchi E, Ribero D, Sottile A, Suita L, Debernardi F (2011) Intraoperative epidural analgesia prevents the early proinflammatory response to surgical trauma. Results from a prospective randomized clinical trial of intraoperative epidural versus general analgesia. Ann Surg Oncol 18:2722–2731
Day AR, Smith RV, Scott MJ, Fawcett WJ, Rockall TA (2015) Randomized clinical trial investigating the stress response from two different methods of analgesia after laparoscopic colorectal surgery. Br J Surg 102:1473–1479
Litz RJ, Hubler M, Koch T, Albrecht DM (2001) Spinal-epidural hematoma following epidural anesthesia in the presence of antiplatelet and heparin therapy. Anesthesiology 95:1031–1033
Litz RJ, Gottschlich B, Stehr SN (2004) Spinal epidural hematoma after spinal anesthesia in a patient treated with clopidogrel and enoxaparin. Anesthesiology 101:1467–1470
Schott M, Gehrke A, Gaab M, Jantzen JP (2013) Subdural hematoma after dural puncture: fateful complication of epidural anesthesia. Anaesthesist 62:392–395
Funding
This work was not financially supported.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Gen Ebara, Shinichi Sakuramoto, Kazuaki Matsui, Keiji Nishibeppu, Shouhei Fujita, Shiro Fujihata, Shuichiro Oya, Seigi Lee, Yutaka Miyawaki, Hirofumi Sugita, Hiroshi Sato, Keishi Yamashita declare that they have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ebara, G., Sakuramoto, S., Matsui, K. et al. Efficacy and safety of patient-controlled thoracic epidural analgesia alone versus patient-controlled intravenous analgesia with acetaminophen after laparoscopic distal gastrectomy for gastric cancer: a propensity score-matched analysis. Surg Endosc 37, 8245–8253 (2023). https://doi.org/10.1007/s00464-023-10370-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10370-w