Abstract
Background
Several strategies have been implemented to better identify the course of the ureters intra-operatively due of the morbidity associated with ureteric injuries especially during gynaecological surgery. We described our experience with pre-operative ureteric catherisation in women who underwent major endoscopic gynaecological surgery.
Methods
A case-controlled study of 862 women who underwent major endoscopic gynaecological surgery sourced from two health institutions were conducted. Two groups were compared: those who had pre-operative prophylactic ureteric catherisation (study group) and those who had routine cystoscopy performed immediately post surgery (control group).
Results
There were no intra-operative ureteric injuries or associated complications noted in the study group. When compared to the control group, length of hospital stay (2 days vs 5 days; p < 0.05) and overall mean time for cystoscopy (11 min vs 35 min; p < 0.05) was significantly shorter in the study group. There was no long-term morbidity recorded in the study group.
Conclusion
Our experiences with prophylactic pre-operative bilateral ureteric catheterisation for major endoscopic gynaecological surgeries were favourable and are associated with low complication rates. Routine or adjunct use before major gynaecological and pelvic surgery combined with meticulous surgical technique can help reduce iatrogenic and unintentional ureteric injuries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
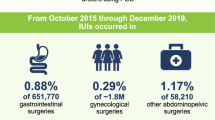
Injuries to the urinary tract system, especially the ureters, are uncommon complications of gynaecological surgery, but are nonetheless associated with significant morbidity. With the rising trend of minimally invasive endoscopic techniques, the reported incidence of ureteric injuries varies from 0.1 up to 2% [1]. The risk is especially increased in patients with previous pelvic inflammatory disease, obesity, uterine fibroids, pelvic organ prolapse, and endometriosis [1, 2]. The normal anatomical course of the ureters may be distorted or dilated in these instances, making them prone to injuries if not exposed or identified adequately.
Several strategies have been implemented to better identify the course of the ureters intra-operatively due of the morbidity associated with ureteric injuries. One strategy includes the prophylactic placement of ureteric catheters prior to commencement of gynaecological surgery [3]—a common practice in our institutions overseeing complex endoscopic cases. Previous studies including randomised controlled studies have shown no difference in rates of ureteric injuries with such a procedure [1, 4, 5], however recent reviews have suggested there are advantages to this method in selected patients undergoing high-risk pelvic surgeries [6, 7]. We described our experience with pre-operative ureteric catherisation in women who underwent major complex endoscopic gynaecological surgery.
Methods
A retrospective case-controlled study of 862 women who underwent major complex endoscopic gynaecological surgery sourced from two health institutions was undertaken. This was conducted according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline (see Appendix 1). Surgeries include laparoscopic hysterectomy (with complexity such as multi-fibroid uterus, presence of adhesions/endometriosis obscuring pelvic sidewalls, and obesity), excision of American Society for Reproductive Medicine (ASRM) grade 3–4 endometriosis, pelvic reconstruction for Pelvic Organ Prolapse Quantification (POP–Q) system grade 3–4 prolapse and post-hysterectomy adnexal surgery. All surgeries were attended by 3 consultant gynaecologists. Two groups were compared: those who had pre-operative prophylactic ureteric catherisation (study group) and those who had routine cystoscopy performed immediately post surgery (control group). This procedure in this latter group was to ensure ureteric patency through ureteric jet visualisation. Women who underwent laparotomy or surgery for gynaecological malignancies were excluded.
The demographics and clinical data extracted for all patients identified included age, ethnicity, body mass index (BMI), previous abdomino-pelvic surgery, indications for surgery, surgery performed as well as complications. Complications were defined as injuries to urinary tract, postoperative bleeding, urinary tract infection (UTI), need for blood transfusions, unplanned return to theatre (defined as defined as a return to the theatre due to complications or untoward outcomes related to the initial surgery), readmission to hospital, and length of hospital stay. All patients were followed-up at 6 weeks and 12 weeks post surgery.
Surgical technique
Study group
A rigid 30-degree cystoscopy with a double channel bridge was performed in lithotomy position after general anaesthesia administration. Bilateral open-end ureteral catheters (Cook Medical 5.0 and 6.0 French) were inserted after identification of ureteral orifices through a 0.035 guide wire. The ureteral catheters were secured to a Foley indwelling urinary catheter with steri-strips. Both ureteral catheters were removed after immediate completion of gynaecological surgery. Intravenous fluids therapy (IVT) was administered post-operatively to encourage “flushing” of blood clots and debris, both of which may arise from mechanical manipulation of ureters. All cystoscopy and ureteric catherisations were performed by 3 gynaecological surgeons.
Control group
A rigid 30-degree cystoscopy was performed upon immediate completion of gynaecological surgery to ensure ureteric patency. This involved direct visualisation of bilateral ureteric jets vermiculation.
Statistical analysis
Statistical analysis was conducted using InStat version 3.1 (GraphPad Software, Inc). Descriptive statistics were reported using mean with interquartile range for continuous data and frequencies with percentages for categorical data. Data was compared using Fisher’s and chi-square tests. Medians with interquartile ranges were compared using Mann–Whitney U test. Results are expressed as odds ratios (OR) with 95% confidence intervals (CI). All reported P values are two-sided, and p < 0.05 was considered significant. Ethics approval was obtained from both health institutions Human Research Ethics Committee.
Results
The mean age was 41.4 (range 17–89) and over 70% of women had a BMI of 25–30 kg/m2. The characteristics and complications of 862 women who underwent major endoscopic gynaecological surgery are presented in Table 1.
A total of 276/862 women (32%) were identified as smokers, with 142/862 women (16.4%) being on anticoagulant therapy and 570/862 women (66.1%) with previous abdomino-pelvic surgery. Main surgical procedures performed included total laparoscopic hysterectomy 564/862 (65.4%), excision of ASRM stage 3–4 endometriosis 186/862 (21.5%), and adnexal surgery (ovarian cystectomy and/or oophorectomy) in the post-hysterectomy state 89/862 (10.3%). There were 148/862 (17.1%) cases of POP-Q stage 3–4 pelvic organ prolapse, where pelvic reconstruction surgery was performed in conjunction with hysterectomy. Indications for hysterectomies were heavy menstrual bleeding 206/564 (36.5%), uterine fibroids 183/564 (32.4%), uterine prolapse 148/564 (26.2%) and complex endometrial hyperplasia 50/564 (8.8%).
A total of 489 women were identified in the study group. Seven women were excluded due to ureteric anomaly and technical difficulty. These include ureteric orifice strictures, the inability to pass guide wires, and obstruction of ureteric orifice due to bladder mass. Cystoscopy and bilateral ureteric catheterisation took an average mean time of 11.7 min (range: 8–15 min, median: 10 min) to perform. There were no intra-operative ureteric injuries or associated complications noted. Post-operative complications included hematuria 205/489 (43.2%), urinary tract infection 2/489 (0.4%) and post-operative bleeding 1/489 (0.2%). A total of 440/489 women (90%) had follow-up ranging from 4 to 12 weeks post-surgery. Twenty-four women relocated overseas and 14 had changed contact details; there was no attempt at follow-up. There was no long-term morbidity recorded in the study group.
When compared to the control group, overall mean time for cystoscopy was significantly shorter in the study group (11 min vs 35 min; p < 0.05). Rates of hematuria were higher for women in the intervention group (43.2% vs 10.1%; p < 0.05) and total operative times were shorter although this was not statistically significant (120 min vs 150 min; p < 0.1). Rates of ureteric and bladder injuries were higher in the control group (40.8% vs 16.2%; p < 0.05) as well as length of hospital stay (2 days vs 5 days; p < 0.05). There were no differences in prevalence of acute renal injury, or post-operative bleeding between both groups.
Discussion
Our experiences with prophylactic pre-operative bilateral ureteric catheterisation for major complex endoscopic gynaecological surgeries were favourable and are associated with low complication rates. This procedure facilitates real-time intra-operative identification of the ureters during surgical dissection, and took significantly shorter time to perform when compared to cystoscopy with at the end of surgery. It is important to note that the long operative time for cystoscopy in the control group relates to the waiting time for ureteric jets to vermiculate and expel urine, rather than the act of performing the cystoscopy itself. In some instances, administration of frusemide and/or use of 50% dextrose as a distending medium were used to facilitate visualisation.
The high rates of asymptomatic hematuria in the study group were due to mechanical manipulation of the ureters during catherization. We observed this to be a transient phenomenon that resolved in the first 24 h post-operation with IVT, with no short or long-term morbidity. There was one case of reflex oligo-anuria reported, which is recognised as a complication of ureteral catheterization [8]. The etiology is not well understood, and is thought to be caused by transient ureteric obstruction after removal of catheters. It is hypothesised that manipulation and irritation of the ureters causes local edema and spasm, leading to symptoms of suprapubic and flank pain, as well as low urine output. We believe that our routine practice of post-operative IVT provided a continuous diuresis, which prevented this uncommon complication.
The 3 cases of ureteric injuries occurred in the control group—the first occurred during excision of endometriosis was diagnosed during cystoscopy. The remaining two occurred on transection of the uterine arteries during hysterectomy where excessive haemorrhage transpired; both were diagnosed 24–48 h post-operatively. The delay in diagnosis, compounded by further recovery from subsequent return to theatre contributed to the longer median length of hospital stay. There were also two cases of complicated UTI in the control group which required prolonged intravenous administration of antibiotics.
It is important to highlight that ureteric catherisation is different to ureteric stenting, as the latter involves a plastic device (e.g. double-J stents) that may be left in situ to alleviate obstructive symptoms. Stenting can be associated with pain and infection, and requires removal a few weeks, or months, after initial placement. Apart from ureteric catherisation, other techniques described to better identify ureters intra-operatively include the use of methylene blue injection and intraureteral indocyanine green [9]. Nevertheless, it is important to emphasise that ureteral catheters should not be employed at the expense of a clear appreciation of retroperitoneal pelvic anatomy, safe electro-surgery procedural knowledge as well as meticulous surgical dissection techniques during endoscopic surgery. Surgeons with high surgical volume load as well as training in fellowship program of minimally invasive gynaecologic surgery (MIGS) have shown lower than average rate of ureteric injuries as well as other complications in surgeries performed [10].
The limitations of our study include the potential for recall bias given the retrospective nature of analysis. Grading of hematuria was not performed though majority were mild. We did not divide cases based on each surgeon’s operative experience and skill, although all 3 surgeons are trained or have been practicing MIGS inside their scope of specialisation. Other aspects to consider include the cost saving and effectiveness of routine ureteric catherisation in high-risk surgeries. Nevertheless, our routine use of ureteric catherisation has shown to be efficacious in complex surgeries in identifying and preventing ureteric injuries. Such practice may be beneficial during peripartum hysterectomy [11] and other surgical specialities [12]. It may also play a role in resource-limited healthcare settings where prevalence of urinary tract injuries are much higher, given the risk of delayed diagnosis and access to treatment [13].
Conclusion
Our study shows that prophylactic pre-operative ureteric catheterisations facilitates real-time intra-operative identification of the ureters during complex surgeries, and are associated with low morbidity rates. Routine or adjunct use before major complex gynaecological surgery combined with meticulous surgical technique can help reduce iatrogenic and unintentional ureteric injuries.
References
Chou MT, Wang CJ, Lien RC (2009) Prophylactic ureteral catheterization in gynecologic surgery: a 12-year randomized trial in a community hospital. Int Urogynecol J Pelvic Floor Dysfunct 20(6):689–693
Chan JK, Morrow J, Manetta A (2003) Prevention of ureteral injuries in gynecologic surgery. Am J Obstet Gynecol 188(5):1273–1277
Merritt AJ, Crosbie EJ, Charova J et al (2013) Prophylactic pre-operative bilateral ureteric catheters for major gynaecological surgery. Arch Gynecol Obstet 288(5):1061–1066
Tanaka Y, Asada H, Kuji N et al (2008) Ureteral catheter placement for prevention of ureteral injury during laparoscopic hysterectomy. J Obstet Gynaecol Res 34(1):67–72
Kuno K, Menzin A, Kauder HH et al (1998) Prophylactic ureteral catheterization in gynecologic surgery. Urology 52(6):1004–1008
Minas V, Gul N, Aust T et al (2014) Urinary tract injuries in laparoscopic gynaecological surgery; prevention, recognition and management. Obstet Gynaecol 16(1):19–28
Feng D, Tang Y, Yang Y et al (2020) Does prophylactic ureteral catheter placement offer any advantage for laparoscopic gynecological surgery? a urologist’ perspective from a systematic review and meta-analysis. Transl Androl Urol 9(5):2262–2269
Merritt AJ, Zommere I, Slade RJ et al (2014) Oliguria after prophylactic ureteric stenting in gynaecological surgery—a report of three cases and review of the literature. Gynecol Surg 11:23–26
Cabanes M, Boria F, Hernández Gutiérrez A et al (2020) Intra-operative identification of ureters using indocyanine green for gynecological oncology procedures. Int J Gynecol Cancer 30(2):278
Gupta S, Maghsoudlou P, Ajao M et al (2022) Very low rates of ureteral injury in laparoscopic hysterectomy performed by fellowship-trained minimally invasive gynecologic surgeons. J Minim Invasive Gynecol 29(9):1099–1103
Lim WH, Pavlov T, Dennis AE (2014) Analysis of emergency peripartum hysterectomy in Northern Tasmania. Aust J Rural Health 22(5):235–240
Chong JT, Kan KM, Phillips CK et al (2018) Ureteral catheters for colorectal surgery: influence on operative times and complication outcomes: an observational study. Investig Clin Urol 59(2):119–125
Raassen TJIP, Ngongo CJ, Mahendeka MM (2018) Diagnosis and management of 365 ureteric injuries following obstetric and gynecologic surgery in resource-limited settings. Int Urogynecol J 29(9):1303–1309
Acknowledgements
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Wei How Lim, Dr. Vincent P Lamaro, Dr. Sarah Livingstone has no funding or conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lim, W.H., Lamaro, V.P. & Livingstone, S. Pre-operative ureteric catherisation for major endoscopic gynaecological surgery. Surg Endosc 37, 8335–8339 (2023). https://doi.org/10.1007/s00464-023-10359-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10359-5