Abstract
Background
Revisional bariatric surgeries are increasing for weight recurrence and return of co-morbidities. Herein, we compare weight loss and clinical outcomes following primary Roux-en-Y Gastric Bypass (P-RYGB), adjustable gastric banding to RYGB (B-RYGB), and sleeve gastrectomy to RYGB (S-RYGB) to determine if primary versus secondary RYGB offer comparable benefits.
Methods
Participating institutions’ EMRs and MBSAQIP databases were used to identify adult patients who underwent P-/B-/S-RYGB from 2013 to 2019 with a minimum one-year follow-up. Weight loss and clinical outcomes were assessed at 30 days, 1 year, and 5 years. Our multivariable model controlled for year, institution, patient and procedure characteristics, and excess body weight (EBW).
Results
768 patients underwent RYGB: P-RYGB n = 581 [75.7%]; B-RYGB n = 106 [13.7%]; S-RYGB n = 81 [10.5%]. The number of secondary RYGB procedures increased in recent years. The most common indications for B-RYGB and S-RYGB were weight recurrence/nonresponse (59.8%) and GERD (65.4%), respectively. Mean time from index operation to B-RYGB or S-RYGB was 8.9 and 3.9 years, respectively. After adjusting for EBW, 1 year %TWL (total weight loss) and %EWL (excess weight loss) were greater after P-RYGB (30.4%, 56.7%) versus B-RYGB (26.2%, 49.4%) or S-RYGB (15.6%, 37%). Overall comorbidity resolution was comparable. Secondary RYGB patients had a longer adjusted mean length of stay (OR 1.17, p = 0.071) and a higher risk of pre-discharge complications or 30-day reoperation.
Conclusion
Primary RYGB offers superior short-term weight loss outcomes compared to secondary RYGB, with decreased risk of 30-day reoperation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Bariatric surgery remains a durable treatment for obesity and its related co-morbidities. Procedural trends have varied over the past decade, with an increase in sleeve gastrectomy (SG) and decrease in adjustable gastric banding (AGB) [1]. As the landscape of bariatric surgery continues to evolve, a growing demand for revisional procedures has emerged. Revisional bariatric surgery is often performed for weight recurrence or non-response, surgical complications, or worsening or poorly controlled comorbidities [2]. Revisional surgery is classified as a conversion of the index procedure to another procedure type, a correction of the index procedure, or a reversal to normal or near-normal anatomy [3].
In 2019, revisional procedures accounted for 16.7% of all bariatric procedures in the United States, making it the third most common bariatric procedure type [4]. The majority of revisional procedures involve AGBs—specifically conversion to SG, followed by AGB removal, and conversion to Roux-en-Y Gastric Bypass (RYGB). Due to limitations of CPT coding (lack of a specific code), SG conversions to RYGB are not as readily quantified, although these procedures are becoming more prevalent. Few studies have compared weight loss outcomes of primary versus secondary RYGB. This study aims to determine whether primary (P-RYGB) and secondary RYGB—after either conversion of SG (S-RYGB) or AGB (B-RYGB)—offer comparable clinical outcomes.
Methods
This study was approved by the Institutional Review Board of the three participating institutions. Informed consent was not required due to the retrospective nature of the study. Electronic medical records and Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) Patient Use Files (PUF) were queried by each participating institution to identify all adult patients who underwent P-RYGB, B-RYGB, or S-RYGB between January 2014 and December 2019. Patient demographics, operative data, postoperative outcomes (length of stay [LOS], total weight loss [TWL], excess weight loss [EWL], BMI, comorbidity resolution), and complications (pre-discharge complication, emergency department visit, readmission, reintervention, reoperation, death) were collected and compared between cohorts.
The primary outcome was %EWL measured at 30 days, 1 year, and 5 years. Secondary outcomes were: (a) %TWL at 30 days, 1 year, and 5 years; (b) comorbidity resolution at 1 year and 5 years; (c) length of stay (LOS); (d) all predischarge complications; all postoperative (e) emergency department visits, (f) readmissions, (g) reinterventions, (h) reoperations, and (i) mortality within 30 days or 1 year.
Statistical analysis
Random effects linear regression was used to analyze %EWL and %TWL over time. This statistical methodology allowed for the analyses of all available data (as some data was unavailable for one or more timepoints) and accounted for the correlation of multiple measurements on the same patient. Logistic regression was used to analyze each clinical endpoint. Negative binomial regression was used to analyze Length of stay (LOS). The multivariable (adjusted) model for each analysis controlled for year, center, 14 patient characteristics (age, sex, hypertension, hyperlipidemia, diabetes, osteoarthritis, obstructive sleep apnea, COPD/asthma, H. pylori, GERD, gastritis, NSAID and aspirin use, ASA classification) and 6 procedure characteristics (hernia repair, surgical approach, gastrojejunostomy anastomosis technique, jejunojejunostomy anastomosis technique, Roux length, and BP length). The analysis of %EWL also controlled for baseline excess body weight, and that for %TWL also controlled for baseline weight. The primary comparison in all analyses was between primary versus revisional RYGB. A subgroup analysis of revisional RYGB broken down by revision type—conversion of B-RYGB or S-RYGB—was also performed.
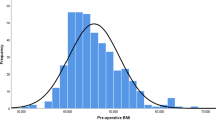
Results
A total of 768 patients were included in this study. Of these, 581 (75.7%) underwent P-RYGB, 106 (13.8%) B-RYGB, and 81 (10.5%) S-RYGB. Baseline patient demographics and procedure characteristics are reviewed in Table 1. The majority of patients were female (83.2%, n = 639). Indications for revision differed, with GERD (65%, n = 51) being the most common indication for S-RYGB and weight recurrence (60%, n = 61) being the indication for B-RYGB. There was a trending increase in the percentage of revisional gastric bypass procedures from 2016–2019. Time from index procedure to B-RYGB or S-RYGB was a mean of 8.9 years and 3.9 years, respectively. In those patients undergoing B-RYGB, 56.6% (n = 60) were done as a single-stage procedure. Concurrent hiatal hernia repair was more common in patients undergoing S-RYGB (57%, n = 46) compared to P-RYGB (21%, n = 121) or B-RYGB (26%, n = 28). Baseline EBW and BMI were substantially lower among the S-RYGB cohort (103 lb, 38.3 kg/m2) than either P-RYGB (159 lb, 47.3 kg/m2) or B-RYGB (151 lb, 46 kg/m2).
The follow up rate for our study was 95.2% (n = 731) at 30 days, 75.5% (n = 580) at 1 year, and 16.3% (n = 125) at 5 years. After controlling for baseline weight, %TWL was significantly greater after P-RYGB at 30 days and 1 year postoperatively (10.7%, 30.6%, respectively) compared to B-RYGB (7.6%, p < 0.001; 26%, p < 0.001) or S-RYGB (8%, p = 0.011; 15.4%, p < 0.001) (Fig. 1A). After controlling for baseline excess body weight, %EWL was significantly greater in the P-RYGB cohort at both 30 days and 1 year postoperatively (20.0%, 57.1%) than either revisional group (B-RYGB: 14.6% [p < 0.001], 49.1% [p = 0.002]; S-RYGB: 19.1% [p = 0.040], 36.7% [p < 0.001]) (Fig. 1B). The sample size at 5 years was underpowered for a statistically significant result for either %TWL or %TWL, as follow up data was only available for 9 patients with B-RYGB and 2 with S-RYGB (Table 2, Fig. 1A/B). Overall comorbidity resolution was comparable between P-RYGB and revisional RYGB groups at 1 year (49.7%, 40.0%, respectively [OR = 1.00 (95% CI 0.58, 1.75), p = 0.992]).
Table 3 outlines clinical outcomes following primary and secondary RYGB at 30 days and 1 year postoperatively. Patients who underwent revisional RYGB had 17% longer adjusted mean length of stay (LOS) compared to the P-RYGB group (p = 0.071). LOS did not differ significantly between the S-RYGB or B-RYGB groups (2.1 days versus 1.6 days, p = -0.179). The revisional RYGB cohort had significantly higher risk of a pre-discharge complication (OR = 2.66 [1.11, 6.34], p = 0.028) and of 30-day reoperation (OR = 3.81 [1.30, 11.1], p = 0.015) than the P-RYGB group. In contrast, at 1 year, revisional RYGB patients had significantly lower likelihood of an ED visit than P-RYGB patients (OR = 0.46 [0.24, 0.88], p = 0.018).
Discussion
This is one of few studies comparing weight loss outcomes following primary and secondary RYGB. In this multi-institutional cohort, we found that S-RYGB results in lower %TWL and %EWL than P-RYGB or B-RYGB at 30 days and 1 year postoperatively, even after adjusting for baseline weight and excess body weight, respectively. Comorbidity resolution was comparable amongst the primary and revisional groups. When counseling patients on procedural options and anticipated weight loss outcomes after revisional surgery, these differences should be taken into consideration.
These results have been replicated in smaller, pooled, cohorts. Abdulrazzaq et al. compared clinical outcomes between 120 patients who underwent P-RYGB and 34 who underwent a revisional RYGB following either AGB (n = 12) or SG (n = 22). Within this pooled revisional group, the three most common indications for revision were insufficient weight loss (32.3%), weight regain (32.3%), and GERD (32.3%). Despite no difference in preoperative BMI between groups, at 18 months, those who underwent a primary procedure had a lower mean weight, BMI, %TWL, and %EWL (p = 0.001, p < 0.001, p < 0.0001, p < 0.0001, respectively) than the revisional group. They also followed patients’ T2DM, dyslipidemia, and hypertension postoperatively and found no difference in the clinical control of comorbidities between the two groups. While many of Abdulrazzaq et al. study’s results parallel those of our own, they found no difference in the rate of early or late complication rates between the primary and revisional cohorts [5]. Our study found that reoperation was significantly more likely in the revisional RYGB group compared to P-RYGB (p = 0.015) whereas the number of emergency department visits within 1 year postoperative was significantly greater in the P-RYGB group (p = 0.018).
Other studies, such as Parmar et. al, compared the outcomes of S-RYGB based on the indication for revision—insufficient weight loss or weight regain versus GERD. Patients undergoing revision for GERD had a significantly lower BMI preoperatively than those revised for weight-related reasons. Conversion resulted in a resolution of GERD symptoms in 80% of patients; however, the cohort seeking additional weight loss only achieved a 2.5 point drop in BMI 2 years postoperatively. R-OAGB (one anastomosis gastric bypass) following primary SG has boasted a decrease of 8.3 points in BMI within this same timeframe, suggesting that revision to gastric bypass may not be the optimal procedure in this group [6, 7]. While this study did not compare outcomes of S-RYGB to P-RYGB, its findings indicate that future studies comparing P-RYGB to revisional RYGB should classify SG patients as two separate cohorts based on their indication for revision [8].
A 2017 study in Obesity Surgery both echoes and marries the two aforementioned studies [9]. The outcomes of revisional RYGB following AGB or SG were compared based on revision indication—additional weight loss versus relief of symptoms, primarily GERD—and primary procedure type. Amongst B-RYGB versus S-RYGB performed for additional weight loss, the B-RYGB cohort had a significantly higher %EWL (71.1 ± 21.6% versus 50.8 ± 23.0%, p = 0.002). These findings again suggest that revisional RYGB may not be the ideal operation following a failed primary SG when weight loss is the primary goal [10, 11]. When comparing the same two groups’ outcomes based on symptom resolution, preoperative complaints improved in 100% of the B-RYGB and 71% of the S-RYGB patients (p < 0.001). In terms of %EWL at 2 years, B-RYGB experienced less EWL compared to S-RYGB (76.9 ± 25.8% versus 80.7 ± 25.9%; p = 0.002) [9].
A 2023 study directly compared P-RYGB to S-RYGB outcomes. Importantly, the indication for revision was weight loss in all 62 S-RYGB patients, eliminating revision indication as a confounding factor. Zadeh et al. found that average %EWL was 41.5% at 1 year and 30.8% at 2 years postoperatively in the revisional group [12]. These values represent a lower %EWL when compared to that expected following P-RYGB [13]. This study also identified 2 predictors of below average weight loss at 1 year postoperative in the revisional cohort: Interval to conversion < 2 years and pre-conversion BMI > 40. When evaluating a patient for a revisional bariatric procedure, it may be prudent to consider these 2 factors when planning preoperative weight loss goals and procedure timing.
Our study’s results add support to the existing literature that suggest that, when performed for weight recurrence, S-RYGB may not necessarily maximize weight loss. This may be intrinsic to the patient and a biological or genetic predisposition to resist the effects of weight loss surgery. Alternatively, this effect may be intrinsic to the surgical technique itself. When creating the gastric pouch in a patient with previous SG, surgeons may be tempted not to change the vertical axis given concern for poor blood supply and increased risk for leak. This could theoretically result in a larger gastric pouch, decreased restriction, and lower weight loss compared to P-RYGB or B-RYGB. If the primary goal of revisional surgery is weight loss, these patients may benefit from an objective measurement of pouch size or consideration of a more malabsorptive procedure such as duodenal switch or single anastomosis duodenal-ileal bypass.
This study is limited by the small number of patients for whom 5-year follow up data was available. This was due to patients being lost to follow up or not having 5 years of postoperative data. Inclusion criteria for this study was only 1 year of follow up data. This makes it difficult to determine how long-term clinical outcomes differ amongst the P-RYGB and revisional RYGB, especially since nadir weight loss is achieved between the second and third years after surgery. Furthermore, due to its retrospective nature, the results are subject to bias, and some data were not available in the EMR. Most notably, we are unable to assess pouch size, which may have factored into weight loss outcomes. Finally, a limitation of ours and potentially other studies on this topic, is having insufficient data to allow comparisons of “total surgical therapy” (e.g. comparing outcomes after primary gastric bypass to outcomes after primary sleeve gastrectomy or band plus the subsequent revision to gastric bypass). Many of the revision patients, although suffering sub-optimal weight loss or weight recurrence, may nevertheless have a lower starting weight and BMI than they did before their primary operation. This is, in fact, the case in our S-RYGB group. Because many of these patients had their primary operations elsewhere, accurate anthropometric data (weight, BMI, etc.) before their primary operation may not be available. Such an analysis may help determine whether patients arrive at similar outcomes when accounting for their total surgical therapy.
Conclusion
This multi-institutional study suggests that patients undergoing primary RYGB have superior weight loss outcomes compared to secondary RYGB, particularly S-RYGB. Prospective studies are needed to identify contributing technical or patient specific factors.
References
Clapp B, Harper B, Dodoo C, Klingsporn W, Barrientes A, Cutshall M, Tyroch A (2020) Trends in revisional bariatric surgery using the MBSAQIP database 2015–2017. Surg Obes Relat Dis 16(7):908–915
Lim CS et al (2009) Revisional bariatric surgery. Obes Surg 19(7):827–832
Lyons W, Omar M, Tholey R, Tatarian T (2022) Revisional bariatric surgery: a review of workup and management of common complications after bariatric surgery. Mini-invasive Surg 6:11
Clapp B, Ponce J, DeMaria E, Ghanem O, Hutter M, Kothari S, LaMasters T, Kurian M, English W (2022) American Society for Metabolic and Bariatric Surgery 2020 estimate of metabolic and bariatric procedures performed in the United States. Surg Obes Relat Dis 18(9):1134–1140
Abdulrazzaq S, Elhag W, El Ansari W et al (2020) Is Revisional Gastric Bypass as Effective as Primary Gastric Bypass for Weight Loss and Improvement of Comorbidities? OBES SURG 30:1219–1229
Moszkowicz D, Rau C, Guenzi M, et al. (2013) Laparoscopic omega-loop gastric bypass for the conversion of failed sleeve gastrectomy: early experience. J Visc Surg 150(6):373–378
Homan J, Betzel B, Aarts EO, van Laarhoven KJ, Janssen IM, Berends FJ (2015) Secondary surgery after sleeve gastrectomy: Roux-en-Y gastric bypass or biliopancreatic diversion with duodenal switch. Surg Obes Relat Dis 11(4):771–777
Parmar CD, Gan J, Stier C, Dong Z, Chiappetta S, El-Kadre L, Bashah MM, Wang C, Sakran N (2020) One Anastomosis/Mini Gastric Bypass (OAGB-MGB) as revisional bariatric surgery after failed primary adjustable gastric band (LAGB) and sleeve gastrectomy (SG): a systematic review of 1075 patients. Int J Surg 81:32–38
van Wezenbeek MR, van Oudheusden TR, de Zoete JPJGM et al (2017) Conversion to gastric bypass after either failed gastric band or failed sleeve gastrectomy. Obes Surg 27:83–89
Sanchez-Pernaute A, Rubio MA, Conde M, Arrue E, Perez-Aguirre E, Torres A (2015) Single-anastomosis duodenoileal bypass as a second step after sleeve gastrectomy. Surg Obes Relat Dis 11(2):351–355
Carmeli I, Golomb I, Sadot E, Kashtan H, Keidar A (2015) Laparoscopic conversion of sleeve gastrectomy to a biliopancreatic diversion with duodenal switch or a Roux-en-Y gastric bypass due to weight loss failure: our algorithm. Surg Obes Relat Dis 11(1):79–85
Zadeh J, Alvarez R, Khaitan L, Abbas M (2023) Conversion of gastric sleeve to Roux-en-Y gastric bypass: overall outcomes and predictors of below-average weight loss. Surg Obes Relat Dis 19(2):111–117
Ignat M, Vix M, Imad I, D’Urso A, Perretta S, Marescaux J, Mutter D (2017) Randomized trial of Roux-en-Y gastric bypass versus sleeve gastrectomy in achieving excess weight loss. Br J Surg 104(3):248–256
Acknowledgements
We’d like to thank Constantine Daskalakis, ScD in the Department of Biostatistics at Thomas Jefferson University for biostatistical support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Drs. Bryan Robins, James Fraser, Luke Swaszek, Neil King, Aurora Pryor, Konstantinos Spaniolas, Renee Tholey, Sami Tannouri, Francesco Palazzo, Alec Beekley, and Talar Tatarian, Ms. Brigitte Anderson, and Ms. Caroline Sanicola have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Accepted as a Quick Shot Presentation at the SAGES 2023 Annual Meeting.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Anderson, B., Robins, B., Fraser, J.A. et al. Weight loss and clinical outcomes following primary versus secondary Roux-en-Y gastric bypass: a multi-institutional experience. Surg Endosc 37, 6445–6451 (2023). https://doi.org/10.1007/s00464-023-10133-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10133-7