Abstract
Aim
Laparoscopic and endoscopic cooperative surgery for early non-ampullary duodenum tumors (D-LECS) is now noted because of its safety and lower invasiveness. Here, we introduce two distinct approaches (antecolic and retrocolic) according to the tumor location during D-LECS.
Methods
From October 2018 to March 2022, 24 patients (25 lesions) underwent D-LECS. Two (8%), two (8%), 16 (64%), and five (20%) lesions were located in the first portion, in the second portion to Vater’s papilla, around the inferior duodenum flexure, and in the third portion of the duodenum, respectively. The median preoperative tumor diameter was 22.5 mm.
Results
Antecolic and retrocolic approaches were employed in 16 (67%) and 8 (33%) cases, respectively. LECS procedures, such as two-layer suturing after full-thickness dissection and laparoscopic reinforcement by seromuscular suturing after endoscopic submucosal dissection (ESD), were performed in five and 19 cases, respectively. Median operative time and blood loss were 303 min and 5 g, respectively. Intraoperative duodenal perforations occurred in three of 19 cases during ESD; however, they were successfully laparoscopically repaired. Median times until start diet and postoperative hospital stay were 4.5 and 8 days, respectively. Histological examination of the tumors revealed nine adenomas, 12 adenocarcinomas, and four GISTs. Curative resection (R0) was achieved in 21 cases (87.5%). In a comparison of the surgical short outcomes between antecolic and retrocolic approaches, there was no significant difference.
Conclusion
D-LECS can be a safe and minimally invasive treatment option for non-ampullary early duodenal tumors, and two distinct approaches according to the tumor location are feasible.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Duodenal tumors are rare; the incidence of primary duodenum neoplasia based on autopsy studies is approximately 0.5% [1, 2]. Therefore, there are no treatment guidelines for non-ampullary duodenal tumors due to the low number of cases and insufficient evidence. Early non-ampullary duodenal tumors including adenoma, adenocarcinoma, gastrointestinal stromal tumor (GIST), and neuroendocrine tumor are increasingly detected as a result of recent advances in endoscopic screening and radiological examination. Pancreatoduodenectomy is considered the standard approach for non-ampullary duodenal tumors but is undeniably very invasive for early non-ampullary duodenal tumors, which are associated with a lower risk of lymph node metastasis [3, 4]. Partial duodenal resection has also been attempted as an alternative treatment option for early non-ampullary duodenal tumors that do not require lymph node dissection. It is difficult to identify the location of the tumor from the serosal surface. Therefore, an incision in the duodenal wall might be excessive, possibly leading to duodenal leakage and stenosis after surgery [5,6,7,8]. There are a few reports of endoscopic submucosal dissection (ESD) and endoscopic mucosal resection (EMR) for early non-ampullary duodenal tumors [9, 10]. However, they are not used as standard treatment because the anatomical features of the duodenum, such as its narrow lumen and thin walls, make endoscopic resection of tumors very difficult. Indeed, several recent reports have demonstrated that severe complications such as perforation and bleeding frequently occur during and after endoscopic treatment [10,11,12,13].
Hiki et al. described laparoscopic and endoscopic cooperative surgery (LECS) for gastric GIST [14, 15]. This procedure enables precise assessment of tumor boundaries under endoscopic observation, thus facilitating adequate tumor resection. Laparoscopic suturing can minimize distortion of the shape of the gastrointestinal tract, which contributes to procedure safety and preservation of gastrointestinal function [14, 15]. Several studies have validated this technique for early non-ampullary duodenal tumors [16, 17]. However, the feasibility and safety of D-LECS for early non-ampullary duodenal tumors are not fully discussed. We evaluate the feasibility and safety of D-LECS for early non-ampullary duodenal tumors and introduce two distinct approaches during D-LECS according to the tumor location with key technical points.
Methods
Patients
From March 2018 to January 2022, 26 patients with a non-ampullary duodenal tumor (27 lesions) planned D-LECS at Kumamoto University Hospital. One patient had two mucosal lesions in the duodenum. Of 26 cases who planned D-LECS, two cases were treated with only ESD. In the remaining 24 cases with D-LECS, clinicopathological data were prospectively collected and retrospectively analyzed. This retrospective cohort study was approved by the Kumamoto University Hospital Ethics Committee (approval number #1789). The LECS procedures, namely two-layer suturing after full-thickness dissection and laparoscopic reinforcement by seromuscular suturing after ESD, were performed in four and 21 cases, respectively. Here we evaluate the safety and feasibility of two distinct and novel approaches (antecolic and retrocolic approaches) during this new technique, and present the short-term outcomes. Table 1 presents the baseline patient and clinical characteristics of the 24 patients. All patients underwent diagnostic endoscopy with biopsy. All subjects gave written informed consent prior to undergoing treatment by LECS. The clinicopathological features of these patients were retrospectively reviewed from their hospital records.
Indications for D-LECS
The indications for D-LECS to treat early non-ampullary duodenal tumors included tumors with a low risk of lymph node metastasis, expectation of cure with local resection, and approachable with endoscopic and laparoscopic techniques. The eligibility criteria were as follows: (1) early non-ampullary duodenum tumors including adenoma, adenocarcinoma, and GIST; (2) tumor depth confined to the mucosa for adenoma and adenocarcinoma, with no exclusion criteria based on tumor size; (3) tumor located more than 5 mm distal to the ampulla of Vater; and (4) tumor comprising less than half of the duodenum lumen.
Operative method during ESD
For epithelial tumors such as early duodenal cancers and large adenomas, a patient is placed in the left lateral position and a common ESD procedure is performed by a gastroenterologist prior to the laparoscopic procedure. Endoscopic approaches were done by gastroenterologist in all cases. Marking dots are made around the lesion with a Dual knife (KD-650Q; Olympus, Tokyo, Japan). Sodium hyaluronic acid (MucoUp®; Boston Scientific, Marlborough, MA, USA) with a small amount of indigo carmine is injected into the submucosa. A Dual knife and/or a Clutch Cutter (DP2618DT, Fujifilm Medical, Tokyo, Japan) are used for incision and dissection. The electrosurgical unit VIO300D (Erbe, Tübingen, Germany) was used for these procedures. After the ESD procedure, the patient is changed into the supine position to perform laparoscopic procedures. In full-thickness circumferential dissection (exposure procedure) for submucosal tumor, the patient is placed in the supine position to perform endoscopy and laparoscopy procedures simultaneously. The tumor location is confirmed using both endoscopy and laparoscopy. The periphery of the tumor is carefully marked using the endoscope, and a circumferential mucosal incision around the tumor is made by the ESD technique. A laparoscopic full-thickness dissection using laparoscopic coagulating shears (Harmonic Scalpel, Ethicon Endo-Surgery, Cincinnati, OH, USA) is then performed with endoscopic assist by a gastroenterologist.
Surgical procedure in antecolic approach
Under general anesthesia, a 12-mm laparoscopy port was inserted through the umbilicus using the open technique. After pneumoperitoneum with carbon dioxide, four additional trocars were inserted as shown in Fig. 1a. The trocars, except the trocar for the laparoscope, were symmetrically located along the line connecting the location of the target tumor and the umbilicus. From the left side of the patient, the greater omentum was divided at 3 cm from the right gastroepiploic vessels, using laparoscopic coagulating shears (Harmonic Scalpel, Ethicon Endo-Surgery).
The attachment of the transverse mesocolon was freed from the pancreatic head and retroperitoneal tissues. During exfoliation, the accessory right colic vein was clipped and divided to avoid unnecessary bleeding due to intraoperative tensions during laparoscopic procedures (Fig. 2a). Next, the second part of the duodenum and the head of the pancreas were exposed (Fig. 2b). For tumors located in the third part of the duodenum, the hepatocolic ligament was also dissected, and the right colic flexure was mobilized from the retroperitoneum to achieve a good visual field for the horizontal part of the duodenum (Fig. 2c). The duodenum was then mobilized along with the pancreatic head from the retroperitoneum. The attachment of the transverse mesocolon was freed from the head of the pancreas and retroperitoneal tissues. The duodenum and the head of the pancreas were mobilized from the retroperitoneum using the Kocher maneuver until the dorsal pancreas head and inferior vena cava were confirmed (Fig. 2d). For the duodenal tumor in the horizontal part, the Treitz ligament was dissected to achieve a good visual field (Fig. 2e). The tumor location was confirmed using both endoscopy and laparoscopy according to serosal color variations and thinning (Fig. 2f).
Antecolic approach. a The accessory right colic vein was clipped and divided to avoid unnecessary bleeding due to intraoperative tensions during laparoscopic procedures. b The second part of the duodenum and the head of the pancreas were exposed. c The duodenum was mobilized along with the pancreatic head from the retroperitoneum. d The duodenum and the head of the pancreas were mobilized from the retroperitoneum using the Kocher maneuver until the dorsal pancreas head and inferior vena cava were confirmed (optional). e Full mobilization of the horizontal part of the duodenum by dissecting the Treitz ligament (optional). f The tumor location was confirmed using both endoscopy and laparoscopy, and the periphery of the tumor was carefully marked using the endoscope. The bracket indicates the mucosal defect area after ESD
Surgical procedure in retrocolic approach
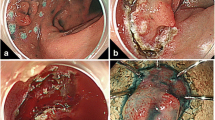
After the ESD procedure, a 12-mm laparoscopy port was inserted through the umbilicus using the open technique under general anesthesia. After pneumoperitoneum with carbon dioxide, four additional trocars were inserted as shown in Fig. 1b. From the left side of the patient, the mesentery was divided at the right side of the middle colic vessels through the transverse mesocolon, using laparoscopic coagulating shears (Harmonic Scalpel, Ethicon Endo-Surgery) (Fig. 3a). Careful attention was paid not to injure the right branch of the middle colic artery (Fig. 3b). The duodenum was then mobilized along with the pancreatic head from the retroperitoneum with a minimum mobilization (Fig. 3c). The tumor location was confirmed using both endoscopy and laparoscopy (Fig. 3d, e). As an optional procedure, the transverse colon was pulled up to the cranial side using a retractor (Fig. 3f).
Retrocolic approach. a Confirmation of the horizontal part of the duodenum. The mesentery was divided at the right side of the middle colic vessels through the transverse mesocolon. b The right branch of the middle colic artery (arrow) is carefully preserved so as not to injure it. c The duodenum and the head of the pancreas are mobilized from the retroperitoneum with a minimum mobilization. d and e Confirmation of the tumor location using both endoscopy (d) and laparoscopy (e). The mucosal defect area (bracket in (e)) after ESD is visualized with serosal color variations and thinning. f The transverse colon is pulled up to the cranial side using a retractor to obtain a good visual field for the horizontal part of the duodenum as an optional procedure
Suturing procedure in D-LECS
For submucosal tumor, full-thickness circumferential dissection (exposure procedure) was applied endoscopically and laparoscopically. In full-thickness dissection, the duodenal wall defect is closed using a laparoscopic hand-sewn suturing technique with two-layer suturing (full-thickness and seromuscular continuous sutures) (Fig. 4a) with care taken to avoid any stenosis or deformity. On the other hand, for epithelial tumors such as early duodenal cancers and large adenomas, the common ESD procedure was usually employed. The tumor location was confirmed using both endoscopy and laparoscopy according to serosal color variations and thinning. After ESD (non-exposure procedure), we reinforced the ESD ulcer bed of the duodenum using the laparoscopic hand-sewn suturing technique with seromuscular continuous suturing (Fig. 4b). In both suturing procedures, Stratafix® spiral knotless barbed suture (size 4–0, length 15 cm) (Ethicon Endo-Surgery) was used. After completing the procedure, the endoscope was inserted and passed over the resected location to confirm that there was neither stenosis nor leakage.
Two-layer continuous suturing after full-thickness dissection and seromuscular continuous suturing during D-LECS. a Two-layer suturing after full-thickness dissection. The duodenal wall defect is closed using a laparoscopic hand-sewn suturing technique with two-layer suturing (full-thickness and seromuscular continuous sutures). b Seromuscular continuous suturing to reinforce the ESD ulcer bed of the duodenum using the laparoscopic hand-sewn suturing technique. In both suturing procedures, Stratafix® spiral knotless barbed suture (size 4–0, length 15 cm) (Ethicon Endo-Surgery, Cincinnati, OH, USA) is used
Statistical analysis
Statistical analysis was performed using SPSS Version 25.0 (SPSS, Chicago, IL, USA). Continuous variables were expressed as the median (range) and compared using the Mann–Whitney U-test. Categorical variables were analyzed using the chi-squared or Fisher's exact test as indicated. A P-value of < 0.05 was considered to indicate statistical significance.
Results
Patient characteristics
Table 1 shows patients’ demographic and clinicopathological features. Twenty-four patients with a non-ampullary duodenal tumor (25 lesions) underwent D-LECS. One patient had two mucosal lesions in the duodenum. Two (8%), two (8%), 16 (64%) and five (20%) lesions were located in the first portion, in the second portion to Vater’s papilla, around the inferior duodenum flexure, and in the third portion of the duodenum, respectively. The median preoperative tumor diameter was 22.5 mm (5–35). LECS procedures, namely two-layer suturing after full-thickness dissection and laparoscopic reinforcement by seromuscular suturing after ESD, were performed in four and 21 cases, respectively.
Surgical outcome
Figure 1 shows representative intraoperative views of the D-LECS procedure with antecolic approach. Figure 2 shows representative intraoperative views of the D-LECS procedure with retrocolic approach. Surgical outcomes are summarized in Table 1. Median operative time and blood loss were 311 min (124–595) and 8 g (0–310), respectively. Antecolic and retrocolic approaches were employed in 16 (67%) and 8 (33%) cases of 24 cases with D-LECS, respectively. There were no conversions to open surgery in this series. Intraoperative duodenal perforation occurred in three cases of 19 epithelial tumor-like lesions during ESD; however, they were successfully laparoscopically repaired and there was no case with postoperative perforation. Morbidity and mortality were not found in any cases. Median time until start diet and postoperative hospital stay were 4.5 and 8 days, respectively. Histological examination of the tumors revealed nine adenomas with moderate atypia, 11 adenocarcinomas, and four GISTs. The en bloc resection rate was 100% in this series, and curative resection (R0) was achieved in 21 cases (87.5%). A positive or inconclusive horizontal margin (HM1 or HMX) on histological evaluation was found in one (adenoma) and two cases, respectively. Finally, the surgical short outcomes were compared between antecolic and retrocolic approaches (Table 1). There was no significant difference in the background and surgical short outcomes between antecolic and retrocolic approaches except for gender. All cases received endoscopic examination in one year after D-LCES, and there was no case with duodenal stenosis required for surgical intervention. With a median follow up of 24.5 months (range, 12.5–52.4 months), there is no case with tumor recurrence including benign and malignant diseases.
Discussion
In this study, we confirmed that D-LECS is feasible and safe for early non-ampullary duodenal tumors. Furthermore, we introduced two distinct and novel approaches (antecolic and retrocolic approaches), and presented their feasibility according to tumor location. The retrocolic approach is available and effective for a duodenal tumor located at the anal side of the papilla of Vater in the descending portion and horizontal portion (Fig. 5). The merit of the retrocolic approach is that it requires minimal mobilization of the duodenum from the retroperitoneum. On the other hand, the conventional antecolic approach consists of division of the accessory right colic vein, mobilization of the right colic flexure, and mobilization of the duodenum and the head of the pancreas from the retroperitoneum using the Kocher maneuver. The conventional antecolic approach is available for a wide range of duodenal tumors, but requires several complicated procedures and entails a risk of duodenal wall injury. Furthermore, the two distinct approaches can be available with similar safety and curability for non-ampullary duodenal tumors according to tumor location.
The least invasive procedures for non-ampullary duodenal tumors are EMR and ESD. However, EMR has a low en bloc resection rate of 62–82%, a low curative resection rate of 30–59%, and a high local recurrence rate of 5.8–8.3% [18,19,20]. These results suggest that EMR leads to oncologically unacceptable outcomes. ESD has more favorable outcomes for non-ampullary duodenal tumors: the en bloc resection rate is 86–100%, the curative resection rate is 78–90%, and the local recurrence rate is 0% [18,19,20,21]. However, ESD has a higher complication rate than EMR. For example, the intraoperative perforation rate is 6.6–35.7%, the delayed perforation rate is 0–35.7%, the bleeding rate is 0–18.4%, and the emergency surgery rate is 3.3–14.3% [18,19,20,21,22]. ESD for duodenal tumors is also considered to be more difficult than for tumors in other parts of the gastrointestinal tract, such as the esophagus, stomach, and colon [9,10,11,12, 21]. Maneuvering a flexible endoscope in the narrow duodenal lumen is technically difficult, and the thin wall increases the perforation risk of ESD for superficial duodenal tumors. In the present series, the en bloc resection rate was 100%, and curative resection was achieved in 87.5%. There were no complications such as intraoperative bleeding and postoperative leakage, bleeding, or stenosis. These favorable results were considered to reflect the advantages of both laparoscopic surgery and ESD. ESD can access tumor boundaries precisely, thus allowing for resection with minimal tumor boundaries. Laparoscopic suturing can minimize distortion of the duodenum, which decreases the risk of perforation. Perforation during ESD was observed in three patients. Almost all of our cases consisted of pinhole perforations that could be repaired under laparoscopic surgery. Leakage after D-LECS was not observed after closing the perforations and reinforcing the serosa. These results showed that ESD alone for a non-ampullary duodenal tumor is associated with a non-negligible risk of perforation; it should be supported by laparoscopy surgery. Otowa and Ichikawa reported a D-LECS procedure using the antecolic approach. Their procedure was associated with a few postoperative complications such as leakage and pancreatic fistula [17, 23]. In addition, regarding the purpose of suturing the duodenum, only the duodenum was mobilized from the retroperitoneum using the Kocher maneuver in their procedure. However, in our novel retrocolic approach, the duodenum had to be minimally mobilized from the retroperitoneum. Our procedure using the retrocolic approach may also be beneficial for tumors that are small or located in the third portion of the duodenum. Duodenum dysfunction, such as stasis, is associated with destruction of the surrounding duodenum tissue, which was not observed in this series. Moreover, there have been brief case reports where the indications for treatment included tumor size less than 10 mm; such tumors can be safely resected using EMR [24, 25]. In the present series, the median tumor size was 20 mm. Therefore, D-LECS may be suitable for relatively large tumors that commonly require ESD. Endoscopy-assisted laparoscopic full-thickness resection is another technique for non-ampullary duodenal tumors that has been reported to have favorable short-term outcomes [16, 17]. However, this technique is associated with a risk of spreading tumor cells and digestive juices into the abdominal cavity. In this study, full-thickness resection was performed in five cases (three GISTs and two adenocarcinomas in pathological diagnosis). Previous studies have reported that no recurrence was recorded in 90 cases with perforation during ESD treatment [26]. Although the two cases with adenocarcinoma treated by full-thickness resection do not show any sign of recurrence, careful follow-up may be required.
From our experience, preoperative diagnostic endoscopic ultrasonography is advocated for the circumferential localization of tumors. If the tumor is found to extend to the pancreatic side of the duodenum, endoscopic closure using clips should be considered.
This study has several limitations. First, it comprised a small number of cases analyzed retrospectively at a single institution. Therefore, the sample size may not be sufficient to accurately evaluate short-term outcomes. The ideal study design would consist of multiple surgical teams and prospective analysis. Second, oncological safety has not yet been determined. In particular, perforation during ESD and full-thickness resection may involve the risk of intra-abdominal dissemination of tumor cells. There were no recurrences during the follow-up period; however, that is just a medium-term outcome, and long-term outcomes should be evaluated in future. Although future large trials are needed for confirmation, the LECS procedure appears to be safe, minimally invasive, and to represent an adequate treatment option for non-ampullary early duodenal tumors with a negligible risk of lymph node metastasis.
Conclusion
D-LECS is feasible and safe for non-ampullary duodenal tumors. Furthermore, two distinct approaches (antecolic and retrocolic approaches) are available according to tumor location with similar safety and curability.
Abbreviations
- EMR:
-
Endoscopic mucosal resection
- LECS:
-
Laparoscopic and endoscopic co-operative surgery
- ESD:
-
Endoscopic submucosal dissection
- GIST:
-
Gastrointestinal stromal tumor
References
Darling RC, Welch CE (1959) Tumors of the small intestine. N Engl J Med 260:397–408
Hoffman BP, Grayzel DM (1945) Benign tumors of the duodenum. Am J Surg 70:394–400
Chok AY, Koh YX, Ow MY, Allen JC Jr, Goh BK (2014) A systematic review and meta-analysis comparing pancreaticoduodenectomy versus limited resection for duodenal gastrointestinal stromal tumors. Ann Surg Oncol 21:3429–3438
Cloyd JM, George E, Visser BC (2016) Duodenal adenocarcinoma: advances in diagnosis and surgical management. World J Gastrointest Surg 8:212–221
Chung JC, Kim HC, Hur SM (2016) Limited resections for duodenal gastrointestinal stromal tumors and their oncologic outcomes. Surg Today 46:110–116
Tanaka E, Kim M, Lim JS, Choi YY, Saklani A, Noh SH, Hyung WJ (2015) Usefulness of laparoscopic side-to-side duodenojejunostomy for gastrointestinal stromal tumors located at the duodenojejunal junction. J Gastrointest Surg 19:313–318
Kanaji S, Nakamura T, Nishi M, Yamamoto M, Kanemitu K, Yamashiita K, Imanishi T, Sumi Y, Suzuki S, Tanaka K, Kakeji Y (2014) Laparoscopic partial resection for hemangioma in the third portion of the duodenum. World J Gastroenterol 20:12341–12345
Stauffer JA, Raimondo M, Woodward TA, Goldberg RF, Bowers SP, Asbun HJ (2013) Laparoscopic partial sleeve duodenectomy (PSD) for nonampullary duodenal neoplasms: avoiding a whipple by separating the duodenum from the pancreatic head. Pancreas 42:461–466
Marques J, Baldaque-Silva F, Pereira P, Arnelo U, Yahagi N, Macedo G (2015) Endoscopic mucosal resection and endoscopic submucosal dissection in the treatment of sporadic nonampullary duodenal adenomatous polyps. World J Gastrointest Endosc 7:720–727
Kakushima N, Kanemoto H, Tanaka M, Takizawa K, Ono H (2014) Treatment for superficial non-ampullary duodenal epithelial tumors. World J Gastroenterol 20:12501–12508
Takimoto K, Imai Y, Matsuyama K (2014) Endoscopic tissue shielding method with polyglycolic acid sheets and fibrin glue to prevent delayed perforation after duodenal endoscopic submucosal dissection. Dig Endosc 26(Suppl 2):46–49
Inoue T, Uedo N, Yamashina T, Yamamoto S, Hanaoka N, Takeuchi Y, Higashino K, Ishihara R, Iishi H, Tatsuta M, Takahashi H, Eguchi H, Ohigashi H (2014) Delayed perforation: a hazardous complication of endoscopic resection for non-ampullary duodenal neoplasm. Dig Endosc 26:220–227
Matsumoto S, Yoshida Y (2014) Selection of appropriate endoscopic therapies for duodenal tumors: an open-label study, single-center experience. World J Gastroenterol 20:8624–8630
Hiki N, Yamamoto Y, Fukunaga T, Yamaguchi T, Nunobe S, Tokunaga M, Miki A, Ohyama S, Seto Y (2008) Laparoscopic and endoscopic cooperative surgery for gastrointestinal stromal tumor dissection. Surg Endosc 22:1729–1735
Hiki N, Nunobe S, Matsuda T, Hirasawa T, Yamamoto Y, Yamaguchi T (2015) Laparoscopic endoscopic cooperative surgery. Dig Endosc 27:197–204
Ohata K, Murakami M, Yamazaki K, Nonaka K, Misumi N, Tashima T, Minato Y, Shozushima M, Mitsui T, Matsuhashi N, Fu K (2014) Feasibility of endoscopy-assisted laparoscopic full-thickness resection for superficial duodenal neoplasms. ScientificWorldJournal 2014:239627
Ichikawa D, Komatsu S, Dohi O, Naito Y, Kosuga T, Kamada K, Okamoto K, Itoh Y, Otsuji E (2016) Laparoscopic and endoscopic co-operative surgery for non-ampullary duodenal tumors. World J Gastroenterol 22:10424–10431
Hoteya S, Yahagi N, Iizuka T, Kikuchi D, Mitani T, Matsui A, Ogawa O, Yamashita S, Furuhata T, Yamada A, Kimura R, Nomura K, Kuribayashi Y, Kaise M (2013) Endoscopic submucosal dissection for nonampullary large superficial adenocarcinoma/adenoma of the duodenum: feasibility and long-term outcomes. Endosc Int Open 1:2–7
Yamamoto Y, Yoshizawa N, Tomida H, Fujisaki J, Igarashi M (2014) Therapeutic outcomes of endoscopic resection for superficial non-ampullary duodenal tumor. Dig Endosc 26(Suppl 2):50–56
Maruoka D, Arai M, Kishimoto T, Matsumura T, Inoue M, Nakagawa T, Watanabe Y, Katsuno T, Tsuyuguchi T, Imazeki F, Yokosuka O (2013) Clinical outcomes of endoscopic resection for nonampullary duodenal high-grade dysplasia and intramucosal carcinoma. Endoscopy 45:138–141
Matsumoto S, Miyatani H, Yoshida Y (2013) Endoscopic submucosal dissection for duodenal tumors: a single-center experience. Endoscopy 45:136–137
Irino T, Nunobe S, Hiki N, Yamamoto Y, Hirasawa T, Ohashi M, Fujisaki J, Sano T, Yamaguchi T (2015) Laparoscopic-endoscopic cooperative surgery for duodenal tumors: a unique procedure that helps ensure the safety of endoscopic submucosal dissection. Endoscopy 47:349–351
Otowa Y, Kanaji S, Morita Y, Suzuki S, Yamamoto M, Matsuda Y, Matsuda T, Oshikiri T, Nakamura T, Kawara F, Tanaka S, Ishida T, Toyonaga T, Azuma T, Kakeji Y (2017) Safe management of laparoscopic endoscopic cooperative surgery for superficial non-ampullary duodenal epithelial tumors. Endosc Int Open 5:E1153–E1158
Tsushimi T, Mori H, Harada T, Nagase T, Iked Y, Ohnishi H (2014) Laparoscopic and endoscopic cooperative surgery for duodenal neuroendocrine tumor (NET) G1: report of a case. Int J Surg Case Rep 5:1021–1024
Kyuno D, Ohno K, Katsuki S, Fujita T, Konno A, Murakami T, Waga E, Takanashi K, Kitaoka K, Komatsu Y, Sasaki K, Hirata K (2015) Laparoscopic-endoscopic cooperative surgery is a safe and effective treatment for superficial nonampullary duodenal tumors. Asian J Endosc Surg 8:461–464
Ikehara H, Gotoda T, Ono H, Oda I, Saito D (2007) Gastric perforation during endoscopic resection for gastric carcinoma and the risk of peritoneal dissemination. Br J Surg 94:992–995
Funding
This work was supported by the Japanese Foundation for Research and Promotion of Endoscopy (to H.H.).
Author information
Authors and Affiliations
Contributions
Conceived and designed the study: HH and HM. Performed the procedures: HH, HM, SN, and KM. Analyzed the data: HH and HM. Wrote the manuscript: HH and HM. Collected clinical data: MT, MT, KM, and HN. Provided critical revisions for scientific findings: YH and HB. Organized the paper and approved the final version to be published: HH, HM, YH, and HB.
Corresponding author
Ethics declarations
Disclosures
Drs. Hiromitsu Hayashi, Hideaki Miyamoto, Shigeki Nakagawa, Kenshi Matsuno, Tatsunori Miyata, Masayo Tsukamoto, Kosuke Mima, Hidetoshi Nitta, Yasuhito Tanaka, and Hideo Baba have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hayashi, H., Miyamoto, H., Nakagawa, S. et al. Distinct approaches (antecolic and retrocolic) according to tumor location in laparoscopic and endoscopic cooperative surgery for non-ampullary duodenum tumors. Surg Endosc 37, 6718–6726 (2023). https://doi.org/10.1007/s00464-023-10114-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10114-w