Abstract
Background
Previous studies analyzing short-term outcomes for per-oral endoscopic myotomy (POEM) have shown excellent clinical response rates and shorter operative times compared to laparoscopic Heller myotomy (LHM). Despite this, many payors have been slow to recognize POEM as a valid treatment option. Furthermore, comparative studies analyzing long-term outcomes are limited. This study compares perioperative and long-term outcomes, cost-effectiveness, and reimbursement for POEM and LHM at a single institution.
Methods
Adult patients who underwent POEM or LHM between 2014 and 2021 and had complete preoperative data with at least one complete follow up, were retrospectively analyzed. Demographic data, success rate, operative time, myotomy length, length of stay, pre- and postoperative symptom scores, anti-reflux medication use, cost and reimbursement were compared.
Results
58 patients met inclusion with 25 undergoing LHM and 33 undergoing POEM. There were no significant differences in preoperative characteristics. Treatment success (Eckardt ≤ 3) for POEM and LHM was achieved by 88% and 76% of patients, respectively (p = 0.302). POEM patients had a shorter median operative time (106 min. vs. 145 min., p = 0.003) and longer median myotomy length (11 cm vs. 8 cm, p < 0.001). All LHM patients had a length of stay (LOS) ≥ 1 day vs. 51.5% for POEM patients (p < 0.001). Both groups showed improvements in dysphagia, heartburn, regurgitation, Eckardt score, GERD HRQL, RSI, and anti-reflux medication use. The improvement in dysphagia score was greater in patients undergoing POEM (2.30 vs 1.12, p = 0.003). Median hospital reimbursement was dramatically less for POEM ($3,658 vs. $14,152, p = 0.002), despite median hospital costs being significantly lower compared to LHM ($2,420 vs. $3,132, p = 0.029).
Results
POEM is associated with a shorter operative time and LOS, longer myotomy length, and greater resolution of dysphagia compared to LHM. POEM costs are significantly less than LHM but is poorly reimbursed.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
In the years since it was first described, per-oral endoscopic myotomy (POEM) has been established in the literature as a first line therapy for achalasia [1] and selected motility disorders of the esophagus [2, 3], with symptomatic treatment outcomes equal to those seen with laparoscopic Heller myotomy (LHM) [4, 5]. For decades, the mainstays of long-term treatment for achalasia were pneumatic dilation [6] and Heller myotomy [7, 8]. LHM has been considered the gold-standard of achalasia therapy in the surgical world, resulting in durable and effective treatment of the symptoms of achalasia [7]. However, over the last few years, the utilization of POEM as a primary therapeutic modality in the treatment of achalasia has been rapidly increasing [9, 10], and more than 6000 POEM procedures have been performed around the world [11].
Several studies have compared the outcomes of POEM and LHM, with most demonstrating similar rates of success despite shorter operative times and length of stay (LOS) with POEM [12, 13]. Other studies have compared the cost-effectiveness of the two procedures, with hospital charges for POEM less than for LHM [14, 15]. However, no study has combined procedure outcomes and cost-effectiveness with hospital reimbursement data. Our study aims to compare perioperative and long-term outcomes, cost-effectiveness, and hospital reimbursement of POEM and LHM at a single institution. We hypothesize, due to the minimally invasive nature of POEM that it will be more cost-effective compared to LHM without compromising on efficacy or safety. Furthermore, we hypothesize that hospital reimbursement data will demonstrate a lack of recognition by payers for the clear benefit to patients and institutions in choosing POEM over LHM.
Methods
Patients
Prior to its initiation, the study methods were reviewed and approved by the Institutional Review Board at the Geisinger Health System. Data were collected retrospectively from a single healthcare system data repository. All patients seen in a surgical clinic and advanced gastroenterology clinic with a diagnosis of achalasia, esophagogastric junction outflow obstruction (EGJOO), Jackhammer variant with EGJOO, or ineffective esophageal motility, undergoing primary laparoscopic Heller myotomy (LHM) or per-oral endoscopic myotomy (POEM) between 2014 and 2021, were included in the study. Patients were excluded if less than 18 years of age, underwent surgery at an outside facility, or if they did not have complete preoperative data and at least one complete follow-up for all variables. The most recent follow-up time point was utilized for each patient.
Surgical techniques
Heller myotomy
Heller myotomy was performed laparoscopically with the patient positioned supine with the arms out. The primary surgeon was positioned to the patient’s right side with the assistant to the patient’s left side. Endoscopy was routinely performed at the beginning of the procedure to assess the gastroesophageal junction. Laparoscopic access was obtained via a 5 mm Optiview port placed under direct visualization in the left epigastrium. Additional 5 mm right and left subcostal ports were placed. An 8 mm port was placed in the right epigastrium. A Nathanson liver retractor was used for liver retraction. Dissection was primarily carried out with a Harmonic scalpel. The pars flaccida was dissected. The esophagus was then mobilized at the right crus and the junction of the right and left crus were identified posterior to the esophagus. The phrenoesophageal membrane was divided followed by division of the short gastric vessels along the greater curvature up to the left crus. The esophagus was circumferentially mobilized. The gastroesophageal fat pad was mobilized off the gastroesophageal junction. The anterior and posterior vagus nerves were identified and preserved. 20 mL of 1:20,000 units of epinephrine were injected submucosally. The longitudinal and circular muscle fibers were divided 5 cm onto the esophagus and 3 cm onto the stomach (8 cm total myotomy length). Endoscopy was again performed at this point to assess for mucosal defects. Partial fundoplication was performed if there were no contraindications.
Peroral endoscopic myotomy
POEM was performed in the endoscopy suite. Patients were positioned supine with the primary surgeon positioned to the patient’s left side. The gastroesophageal junction (GEJ) was assessed endoscopically to identify a hypertonic lower esophageal sphincter indicated by resistance to endoscope advancement into the stomach. Retroflexion of the scope was performed to assure a normal GEJ and cardia. A transparent distal cap was fitted to the endoscope and a T-type Hybrid Knife (ERBE, Marietta, GA) was used for the submucosal tunnel dissection. Using an epinephrine solution, an anterior submucosal bleb was raised approximately 18 cm proximal to the Z-line and a vertical mucosal mucosotomy was performed. At the entry site, the endoscope was advanced within the submucosa creating a submucosal tunnel, while preserving the integrity of the mucosa. The submucosal tunnel was extended to the GEJ and then the tunnel was extended 2 to 3 cm beyond the GEJ onto the stomach. A myotomy of the circular muscle layer was then performed starting 10 cm above the GEJ and extending 2–3 cm below the GEJ. For some esophageal dysmotility cases, a 15 cm myotomy was performed. Upon completing the myotomy, adequate hemostasis and integrity of the mucosa was ensured. Closure of the initial mucosal incision was then performed with endoscopic clips. Final endoscopic assessment assured a widely patent lower esophageal sphincter.
Evaluation
Evaluation of response to treatment was done through subjective scores. Symptom scores were acquired through routine patient assessments during preoperative clinic visits, 3 months postoperatively and subsequent 1 year postoperative intervals via in-person clinic visits, telephone calls, and tele video visits. Preoperative and postoperative symptoms related to achalasia were assessed using the Eckardt score [16]], reflux symptom index (RSI) evaluation [17], and gastroesophageal reflux disease health-related quality of life (GERD HRQL) questionnaire [18].
Patients were also asked about the severity of specific symptoms including heartburn (0 = none, 1 = minimal/episodic without ongoing treatment, 2 = moderate/reasonably well controlled with ongoing treatment, 3 = severe/interferes with daily activity or not well controlled with ongoing treatment), dysphagia (0 = none, 1 = less than or equal to once per week, 2 = greater than once per week or requiring dietary modification, 3 = severe/preventing ingestion of solid food), and regurgitation (0 = none, 1 = mild/after straining or large meal, 2 = moderate/positional, 3 = severe/constant regurgitation with or without aspiration). Use of anti-reflux medications such as proton pump inhibitors (PPI) or H2 receptor blockers was also noted and scored (0 = none, 1 = occasional use/as needed, 2 = daily or 20 mg dose, 3 = twice daily or 40 mg dose).
Perioperative data included operative time in minutes, myotomy location (anterior versus posterior), myotomy length in centimeters, length of stay (LOS), and 30 day readmission rates. Cost data were reported as variable cost, defined as costs directly related to the services provided, including ancillary services, room and board, anesthesia, recovery, laboratory costs, radiology cost, and pharmacy cost. Reimbursement data (actual payment) was obtained from the hospital billing department.
Cost analysis
All variable costs were calculated within the decision support system (DSS) cost accounting software and are based on a hospital relative value unit (RVU) allocation factor and applicable volumes. Total variable costs included OR/anesthesia, pharmacy, endoscopy, laboratory, radiology, recovery, room and board, and ancillary (all additional services not already listed, including but not limited to, respiratory therapy, clinical nutrition, echo, etc.). Professional costs such as physician and/or advanced practitioner salary costs were not included in the analysis.
Statistical analysis
Categorical variables were summarized using frequencies and percentages. Continuous variables with an underlying normal distribution were reported as mean and standard deviation (SD), whereas those with a non-normal distribution were reported as median and interquartile range (IQR). For comparing patient characteristics among the treatment groups, the Mann–Whitney U test was employed for continuous variables; for categorical variables, Chi-squared tests or Fisher’s exact tests were employed. An analysis of permutation t-tests (two-sample equal variances) was conducted to determine if there was a statistically significant difference between the average change in symptoms scores pre- and post-surgery for the two procedure groups. Welch’s t-test was used to compare the difference in average itemized variable costs between Heller and POEM. Analyses were performed using R Version 4.0.5 (R Core Team, 2021) [19]. All statistical tests were two-sided, and a p-value < 0.05 was considered statistically significant.
Results
Demographics
A total of 58 patients who had a diagnosis of achalasia or another primary esophageal motility disorder who met the inclusion and exclusion criteria were identified from 2014 to 2021. Among those, 25 (43.1%) underwent LHM while 33 (56.9%) underwent POEM (Fig. 1). Our institution began performing POEM procedures starting in 2015 and POEM has comprised the majority of cases since 2019 (Figs. 2 and 3). Median age, BMI and co-morbidity burden as measured by Charlson Comorbidity Index were comparable between LHM and POEM cohorts as shown in Table 1. The majority of patients in our cohort had Type 2 achalasia as shown in Fig. 4. The POEM patient classified as “achalasia unspecified” is a young patient who did not tolerate manometry but underwent a contrast esophagography consistent with achalasia, and thus was analyzed along with the type I, II and III achalasia patients in Table 4.
14 (24.1%) patients had received previous treatment for achalasia overall, and this was comparable between LHM and POEM groups (28% vs 21.2%, p > 0.05). Previous treatments included Botox injection, pneumatic balloon dilation or previous POEM or LHM.
Perioperative outcomes
The median operative time for LHM was greater compared to POEM (145 min vs 106 min, p = 0.003). The length of myotomy was significantly longer in POEM than in LHM (11 cm vs 8 cm, p < 0.001). The location of myotomy was anterior in both groups. Length of stay (LOS) was significantly longer for LHM than for POEM (median LOS LHM vs POEM was 1.2 vs 0.76 days, p < 0.001). All patients in the LHM cohort stayed for ≥ 1 day, compared to 17 (51.5%) of patients in the POEM group. 30 day ED visit and readmission rates were low in both groups and comparable, as shown in Table 2. Early post-op complications were too rare to compare between two groups.
Long term outcomes
Average symptoms scores pre- and post-procedure for Heller and POEM are shown in Table 3. Length of follow up for each variable assessed is listed in Fig. 5. Average follow up in months was longer for LHM patients compared to POEM patients. The mean Eckardt score pre and post-procedure were 6.80 and 2.44 for LHM and 6.91 and 1.30 for POEM. The average changes in Eckardt score for LHM and POEM were comparable (−4.36 and −5.61, p = 0.173).
We also calculated changes in regurgitation and dysphagia scores pre and post-procedure individually. Dysphagia score decreased from 2.20 to 1.08 after LHM and 2.88 to 0.58 after POEM. The average decrease in dysphagia score was significantly more in POEM than LHM (−2.30 vs −1.12, p = 0.003). Average changes in regurgitation score were −1.32 after LHM and −1.45 after POEM and were comparable (p = 0.650).
There was a major decrease in GERD HRQL score and RSI score after both LHM and POEM. GERD HRQL decreased from 24.5 to 8.88 after LHM with average change of −15.63 and after POEM it decreased from 24.4 to 9.4 with an average change of −15.73. Similarly, prior to LHM, RSI score was 23 and after LHM it decreased to 8.48 with an average change of −14.48. The RSI score after POEM decreased from 22.9 to 9.48 with an average change of −13.42. Average change in GERD HRQL score and RSI score after LHM and POEM were comparable (p > 0.05).
We also analyzed heartburn score and anti-acid medication use score between two groups. Mean heartburn score decreased from 1.52 to 0.88 in LHM and remained the same, 1.39, pre- and post-surgery in the POEM Group. The average change in heartburn score for LHM was −0.64. The mean anti-acid medication use decreased from 1.72 to 1 after LHM and 1.82 to 1.58 after POEM and the average change was comparable between 2 groups. (−0.72 vs −0.24, p > 0.05).
Symptom scores were compared between the achalasia and non-achalasia patients in our cohort, as shown in Table 4. Except for heartburn score, there were no significant differences in symptomatic outcomes between achalasia and non-achalasia patients. Achalasia patients had an average decrease of 0.42 in heartburn score post-procedure, compared to an average increase of 0.60 in the non-achalasia patients (p = 0.03).
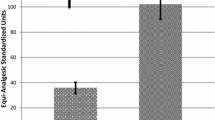
Cost analysis
Cost data were available for 57 of the 58 patients in our study cohort (the patient with missing data underwent POEM). Our cost analysis showed that POEM costs significantly less than LHM. The total median procedure costs for POEM and LHM were $2,420 and $3,132, respectively (p = 0.029), as shown in Fig. 6. The median hospital reimbursement for POEM was $3,658, which was significantly less than LHM at $14,152 (p = 0.002), as shown in Table 5. Itemized variable costs (Table 6) demonstrates OR/anesthesiology and room and board (R&B) as major drivers in cost difference between the two procedures.
Discussion
Though the treatment of achalasia by endoscopic myotomy was first reported by Ortega et al. in 1980 [20], it was adopted as an alternative to LHM only after Inoue et al. [17] described this approach in 2010 with favorable outcomes and named it POEM. With continued refinement of the POEM technique and increasing amounts of data supporting its effectiveness [21], adoption of this procedure in recent years has become widespread, and in many centers POEM has replaced LHM as a primary procedure for achalasia [22, 23].
In our own center, POEM has become the most common treatment modality utilized for achalasia due to the favorable outcomes demonstrated in the literature. Our current provider preference is for POEM, however both POEM and LHM are offered to the patient as therapeutic options. As part of our standard informed consent process, patients are notified of the benefits and risks of any given procedure along with alternatives to the procedure.
Over the last few years many studies have compared LHM and POEM and have reported comparable early outcomes [21], but very few studies have compared the long-term outcomes observed 1 year or more after surgery. Furthermore, only a handful of studies have compared the costs of these procedures, and none have evaluated reimbursement. Our study is unique in that, in addition to the long-term outcomes, we have analyzed the cost-effectiveness and reimbursement of POEM compared to LHM.
The increasing popularity of POEM lies in the benefits it provides across all spectrums of achalasia treatment, with similar or even better outcomes compared to LHM. Our study has reaffirmed what existing literature has shown, with POEM’s shorter operative time, decreased length of stay [24] and ability for a lengthier myotomy [25]. At our institution, almost half of patients that underwent POEM were able to go home the same day. POEM patients that stayed ≥ 1 day were mostly during the early years of our institution’s adoption of the POEM technique, and currently, all POEM procedures are done on an outpatient basis, with rare exceptions. The surgeons at our institution have been performing LHM for a longer period of time than POEM. Despite this, our results show a shorter operative time for POEM. Learning curves certainly play a role in operative time and the difference in operative time between LHM and POEM may increase as we gain more experience with POEM. Operative time trend since POEM was first performed in 2015 is represented in Supplemental Fig. 1. Our median myotomy length for POEM was 11 cm, as the majority of patients have Type 1 or Type 2 achalasia and did not need a lengthier myotomy. However, the myotomy length could easily be extended beyond 11 cm if warranted, as reported by several different studies [26, 27].
Improvement of dysphagia is comparable between LHM and POEM in the short-term as reported by several studies [4], but it appears that in the long-term, POEM has better dysphagia scores, as seen in our study. This may be attributed to the fact that POEM induces less scarring at EGJ than in LHM, leading to better EGJ distensibility [28, 29].
An interesting finding in our study is the decrease in heartburn score after LHM and decrease in anti-acid medication use after both POEM and LHM. Myotomy at the GE junction across the lower esophageal sphincter increases the chances of pathologic acid reflux [30] and many studies have reported increased incidence of esophagitis and positive BRAVO PH studies after LHM and POEM. In fact, some studies have reported an incidence of post-POEM abnormal GERD as high as 40% to 60% on 24-h-pH studies and 18–40% erosive esophagitis on endoscopy [31, 32, 33]. We believe the reported increased heartburn score pre-procedure in our study has to do more with the symptoms complex[34] present in achalasia rather than true acid reflux from stomach. Chest pain is an early complaint in achalasia and can be reported as heartburn as there is constant regurgitation of food that can irritate the lining of the esophagus. Additionally, the continued presence of food in lower esophagus leads to fermentation of food decreasing the pH of the lower esophagus. Constant regurgitation, chest pain and increased acid milieu of lower esophagus can masquerade as heartburn and lead to an increase in heartburn score [35].
We did not perform routine endoscopy or pH studies after POEM or LHM to evaluate for GERD and the lack of this physiologic testing limits the ability to comment on objective GERD outcomes in this patient cohort. However, all patients who present to our foregut clinic complete questionnaires for GERD and RSI as a part of the standard preoperative evaluation process. Although pre-operative GERD HRQL and RSI may not reflect true acid reflux, it provides an additional tool that can be useful in assessing response to surgery.
Median costs were lower in the POEM patients ($2,420 vs $3,132). Our stated costs are significantly lower than those reported previously [14], in part, because other cost-effectiveness comparison studies reported hospital charges, which are often dramatically higher than actual hospital costs [36, 37]. Wirsching et al. did report on actual costs and reported total costs of $13,328 for LHM and $14,201 for POEM; but this analysis also included indirect costs, which our analysis excluded [38]. Future cost analyses could investigate the difference in long-term healthcare associated costs for POEM and LHM patients, rather than procedure-related costs alone, such as the health-related expenditures reported by Lois et al. [39].
New treatment alternatives to LHM need to be not only comparable to LHM in terms of outcomes but must also be cost-effective. The lower costs this study found with POEM can be attributed to substantially lower OR cost due to the ability to perform POEM in the endoscopy suite, its shorter operative time, and high percentage of same day discharges. Despite POEM’s cost-effectiveness, payors often fail to adequately reimburse for POEM despite its favorable clinical outcomes compared to LHM, lower costs, shorter length of stay and thus decreased use of hospital resources, and the benefits to patients in terms of recovery time. Reimbursement for LHM was nearly fourfold the reimbursement for POEM in our study ($14,152 vs. $3,658). The POEM procedures included in our study were performed prior to a CPT code for POEM being implemented. Without a CPT code for POEM, hospitals and endoscopists often only hope to obtain reimbursement for a simple endoscopy, if anything. The tide appears to be turning, however, as more and more societies are embracing POEM as a first line therapy for achalasia [40, 41]. Undoubtedly, support from organizations like SAGES and ASGE has played a significant role in the addition of a new POEM CPT code (43,497) effective January 1, 2022. The goal of the cost analysis was to show that POEM has been disproportionately reimbursed by insurance companies compared to LHM despite similar outcomes and lower costs. We hope that the results of this study encourage increased reimbursement for POEM.
Conclusion
At our institution, POEM as a treatment modality for achalasia results in symptomatic outcomes that are at least as good as LHM, shorter operative times, shorter hospital stays, and lower variable costs; but thus far POEM has been reimbursed very poorly. Given these results, insurance companies should be encouraged to recognize POEM as a highly efficacious and cost-effective treatment modality for achalasia and selected motility disorders of the esophagus. The designation of a CPT code for POEM as of January 1, 2022, should be a big step in the direction of improved reimbursements for the procedure and may increase patient access to it.
References
Guidelines for the Use of Peroral Endoscopic Myotomy (POEM) for the Treatment of Achalasia [Internet]. SAGES. 2020 [cited 2022 Mar 6]. Available from: https://www.sages.org/publications/guidelines/guidelines-for-the-use-of-peroral-endoscopic-myotomy-poem-for-the-treatment-of-achalasia/
Wong I, Law S (2017) Peroral endoscopic myotomy (POEM) for treating esophageal motility disorders. Ann Transl Med 5(8):192. https://doi.org/10.21037/atm.2017.04.36
Filicori F, Dunst CM, Sharata A, Abdelmoaty WF, Zihni AM, Reavis KM et al (2019) Long-term outcomes following POEM for non-achalasia motility disorders of the esophagus. Surg Endosc 33(5):1632–1639. https://doi.org/10.1007/s00464-018-6438-z
Shea GE, Johnson MK, Venkatesh M, Jolles SA, Prout TM, Shada AL et al (2020) Long-term dysphagia resolution following POEM versus Heller myotomy for achalasia patients. Surg Endosc 34(4):1704–1711. https://doi.org/10.1007/s00464-019-06948-y
Werner YB, Hakanson B, Martinek J, Repici A, von Rahden BHA, Bredenoord AJ et al (2019) Endoscopic or surgical myotomy in patients with idiopathic achalasia. N Engl J Med 381(23):2219–2229. https://doi.org/10.1056/NEJMoa1905380
Chuah SK, Wu KL, Hu TH, Tai WC, Changchien CS (2010) Endoscope-guided pneumatic dilation for treatment of esophageal achalasia. World J Gastroenterol 16(4):411–417. https://doi.org/10.3748/wjg.v16.i4.411
Nau P, Rattner D (2014) Laparoscopic Heller myotomy as the gold standard for treatment of achalasia. J Gastrointest Surg 18(12):2201–2207. https://doi.org/10.1007/s11605-014-2655-5
Boeckxstaens GE, Annese V, des Varannes SB, Chaussade S, Costantini M, Cuttitta A, et al (2011) Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med 364(19):1807–1816. https://doi.org/10.1056/NEJMoa1010502
Is Per-oral Endoscopic Myotomy (POEM) More Effective than Pneumatic Dilation and Heller myotomy? A Systematic Review and Meta-Analysis . SAGES. 2020 [cited 2022 Mar 6]. https://www.sages.org/publications/guidelines/is-per-oral-endoscopic-myotomy-poem-more-effective-than-pneumatic-dilation-and-heller-myotomy-a-systematic-review-and-meta-analysis/
Runge TM, Ichkhanian Y, Khashab MA (2020) POEM for achalasia: endoscopic myotomy enters its golden age, and we are taking NOTES. Gastrointest Endosc 91(5):1045–9.e1. https://doi.org/10.1016/j.gie.2020.01.008
Costantini M, Salvador R, Costantini A (2021) Spastic motility disorders: diagnosis and management in the era of the chicago classification. Foregut 1(3):254–262. https://doi.org/10.1177/26345161211044971
Kumagai K, Tsai JA, Thorell A, Lundell L, Håkanson B (2015) Per-oral endoscopic myotomy for achalasia are results comparable to laparoscopic Heller myotomy. Scand J Gastroenterol 50(5):505–512. https://doi.org/10.3109/00365521.2014.934915
Cappell MS, Stavropoulos SN, Friedel D (2020) Updated systematic review of achalasia, with a focus on poem therapy. Dig Dis Sci 65(1):38–65. https://doi.org/10.1007/s10620-019-05784-3
Greenleaf EK, Winder JS, Hollenbeak CS, Haluck RS, Mathew A, Pauli EM (2018) Cost-effectiveness of per oral endoscopic myotomy relative to laparoscopic Heller myotomy for the treatment of achalasia. Surg Endosc 32(1):39–45. https://doi.org/10.1007/s00464-017-5629-3
Conte TM, de Haddad LB, P, Ribeiro IB, de Moura ETH, DʼAlbuquerque LAC, de Moura EGH. (2020) Peroral endoscopic myotomy (POEM) is more cost-effective than laparoscopic Heller myotomy in the short term for achalasia economic evaluation from a randomized controlled trial. Endosc Int Open 8(11):E1673–E1680. https://doi.org/10.1055/a-1261-3417
Pasricha PJ, Hawari R, Ahmed I, Chen J, Cotton PB, Hawes RH et al (2007) Submucosal endoscopic esophageal myotomy a novel experimental approach for the treatment of achalasia. Endoscopy 39(9):761–764. https://doi.org/10.1055/s-2007-966764
Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M et al (2010) Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 42(4):265–271. https://doi.org/10.1055/s-0029-1244080
Rieder E, Swanström LL, Perretta S, Lenglinger J, Riegler M, Dunst CM (2013) Intraoperative assessment of esophagogastric junction distensibility during per oral endoscopic myotomy (POEM) for esophageal motility disorders. Surg Endosc 27(2):400–405. https://doi.org/10.1007/s00464-012-2484-0
R Core Team (2021) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/
Ortega JA, Madureri V, Perez L (1980) Endoscopic myotomy in the treatment of achalasia. Gastrointest Endosc 26(1):8–10. https://doi.org/10.1016/s0016-5107(80)73249-2
Crosthwaite GL, Sejka M (2020) Per-oral endoscopic myotomy (POEM) overview and experience of 100 cases by a single surgeon in Australia. Ann Esophagus 3:12–12. https://doi.org/10.21037/aoe.2020.03.01
Kohn GP (2018) Is peroral endoscopic myotomy (POEM) ready to replace laparoscopic Heller’s myotomy for achalasia comments on a recent systematic review. Ann Laparosc Endosc Surg 3:8–8. https://doi.org/10.21037/ales.2018.01.03
Kim JY, Min YW (2020) Peroral Endoscopic Myotomy for Esophageal Motility Disorders. Clin Endosc 53(6):638–645. https://doi.org/10.5946/ce.2020.223
Cloutier Z, Mann A, Doumouras AG, Hong D (2021) Same-day discharge is safe and feasible following POEM surgery for esophageal motility disorders. Surg Endosc 35(7):3398–3404. https://doi.org/10.1007/s00464-020-07781-4
Ramirez M, Zubieta C, Ciotola F, Amenabar A, Badaloni A, Nachman F et al (2018) Per oral endoscopic myotomy vs. laparoscopic Heller myotomy, does gastric extension length matter. Surg Endosc 32(1):282–288. https://doi.org/10.1007/s00464-017-5675-x
Kane ED, Budhraja V, Desilets DJ, Romanelli JR (2019) Myotomy length informed by high-resolution esophageal manometry (HREM) results in improved per-oral endoscopic myotomy (POEM) outcomes for type III achalasia. Surg Endosc 33(3):886–894. https://doi.org/10.1007/s00464-018-6356-0
Nabi Z, Ramchandani M, Sayyed M, Chavan R, Darisetty S, Goud R et al (2021) Comparison of short versus long esophageal myotomy in cases with idiopathic achalasia: a randomized controlled trial. J Neurogastroenterol Motil 27(1):63–70. https://doi.org/10.5056/jnm20022
Vackova Z, Mares J, Krajciova J, Rabekova Z, Zdrhova L, Loudova P et al (2021) Esophageal motility patterns after peroral endoscopic myotomy in patients with achalasia. J Neurogastroenterol Motil 27(2):205–214. https://doi.org/10.5056/jnm20126
Verlaan T, Rohof WO, Bredenoord AJ, Eberl S, Rösch T, Fockens P (2013) Effect of peroral endoscopic myotomy on esophagogastric junction physiology in patients with achalasia. Gastrointest Endosc 78(1):39–44. https://doi.org/10.1016/j.gie.2013.01.006
Wang XH, Tan YY, Zhu HY, Li CJ, Liu DL (2016) Full-thickness myotomy is associated with higher rate of postoperative gastroesophageal reflux disease. World J Gastroenterol 22(42):9419–9426. https://doi.org/10.3748/wjg.v22.i42.9419
Kumbhari V, Familiari P, Bjerregaard NC, Pioche M, Jones E, Ko WJ et al (2017) Gastroesophageal reflux after peroral endoscopic myotomy: a multicenter case-control study. Endoscopy 49(7):634–642. https://doi.org/10.1055/s-0043-105485
Lu B, Li M, Hu Y, Xu Y, Zhang S, Cai LJ (2015) Effect of peroral esophageal myotomy for achalasia treatment: a Chinese study. World J Gastroenterol 21(18):5622–5629. https://doi.org/10.3748/wjg.v21.i18.5622
Jones EL, Meara MP, Schwartz JS, Hazey JW, Perry KA (2016) Gastroesophageal reflux symptoms do not correlate with objective pH testing after peroral endoscopic myotomy. Surg Endosc 30(3):947–952. https://doi.org/10.1007/s00464-015-4321-8
Laurino-Neto RM, Herbella F, Schlottmann F, Patti M (2018) Evaluationofesophageal Achalasia: from symptoms to the chicago classification. Arq Bras Cir Dig. https://doi.org/10.1590/0102-672020180001e1376
Jung DH, Is PH (2017) Gastroesophageal reflux disease and achalasia coincident or not? J Neurogastroenterol Motil 23(1):5–8. https://doi.org/10.5056/jnm16121
Attaar M, Su B, Wong HJ, Kuchta K, Denham W, Linn JG et al (2021) Comparing cost and outcomes between peroral endoscopic myotomy and laparoscopic Heller myotomy. Am J Surg 222(1):208–213. https://doi.org/10.1016/j.amjsurg.2020.10.037
Khashab MA, Kumbhari V, Tieu AH, El Zein MH, Ismail A, Ngamruengphong S et al (2017) Peroral endoscopic myotomy achieves similar clinical response but incurs lesser charges compared to robotic heller myotomy. Saudi J Gastroenterol 23(2):91–96. https://doi.org/10.4103/1319-3767.203360
Wirsching A, Boshier PR, Klevebro F, Kaplan SJ, Seesing MF, El-Moslimany R et al (2019) Comparison of costs and short-term clinical outcomes of per-oral endoscopic myotomy and laparoscopic Heller myotomy. Am J Surg 218(4):706–711. https://doi.org/10.1016/j.amjsurg.2019.07.026
Lois AW, Oelschlager BK, Wright AS, Templeton AW, Flum DR, Farjah F (2022) Use and safety of per-oral endoscopic myotomy for achalasia in the US. JAMA Surg 157(6):490–497. https://doi.org/10.1001/jamasurg.2022.0807
Kohn GP, Dirks RC, Ansari MT, Clay J, Dunst CM, Lundell L et al (2021) SAGES guidelines for the use of peroral endoscopic myotomy (POEM) for the treatment of achalasia. Surg Endosc 35(5):1931–1948. https://doi.org/10.1007/s00464-020-08282-0
Khashab MA, Vela MF, Thosani N, Agrawal D, Buxbaum JL, Abbas Fehmi SM et al (2020) ASGE guideline on the management of achalasia. Gastrointest Endosc 91(2):213–27.e6. https://doi.org/10.1016/j.gie.2019.04.231
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Lena Shally, Katie Frank, and Drs. Kashif Saeed, Derek Berglund, Mark Dudash, Vladan N Obradovic, David M Parker, Anthony T Petrick, David L Diehl and Jon D Gabrielsen have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplemental Figure 1. POEM operative times since the procedure was first performed in June 2015 (n = 72). Pearson’s correlation coefficient r and associated p-value given in top right corner. Observed values (black points) are overlaid on top of the line of best fit (blue) and its estimated 95% confidence interval (shaded gray band).

Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shally, L., Saeed, K., Berglund, D. et al. Clinical and financial outcomes of per-oral endoscopic myotomy compared to laparoscopic heller myotomy for treatment of achalasia. Surg Endosc 37, 5526–5537 (2023). https://doi.org/10.1007/s00464-022-09652-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09652-6