Abstract
Background
Subepithelial tumors (SETs) in the upper gastrointestinal (GI) tract are frequently discovered during upper endoscopy, and their management is determined based on size and histopathological diagnosis. We aimed to evaluate the diagnostic performance of endoscopic ultrasonography-guided fine-needle biopsy (EUS-FNB) in upper GI SETs of 2–5 cm in size.
Methods
We included 63 patients who underwent EUS-FNB for upper GI SETs of 2–5 cm in size between January 2013 and February 2020. The diagnostic yield of EUS-FNB, ability of EUS-FNB in discriminating malignant from non-malignant lesions, and histopathological concordance between EUS-FNB specimens and resected specimens were evaluated.
Results
Successful acquisition of macroscopic tissue cores was possible in all 63 cases, and the diagnostic yield of EUS-FNB was 92.1% (58/63). The sensitivity, specificity, and accuracy of EUS-FNB in discriminating malignant from non-malignant lesions were 100% (95% confidence interval [CI] 85.3–100%), 87.8% (95% CI 79.9–87.8%), and 92.1% (95% CI 81.8–92.1%), respectively. Of the 26 SETs that were endoscopically or surgically resected after EUS-FNB, the histopathological concordance rate between the EUS-FNB specimens and resected specimens was 100% (24/24), except in two cases of inadequate results with EUS-FNB specimens.
Conclusion
EUS-FNB provides high diagnostic yield and high capability in discriminating malignant from non-malignant lesions in upper GI SETs of 2–5 cm in size.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Subepithelial tumors (SETs) in the upper gastrointestinal (GI) tract are incidentally discovered during upper endoscopy for an unrelated condition, especially during national gastric cancer screening programs in Korea, and the incidence of SETs has gradually increased. The accurate incidence of upper GI SETs is unknown, but the prevalence of SETs detected during routine esophagogastroduodenoscopy is 0.8–2% [1, 2]. GI SETs include various types of tumors from benign lesions, such as leiomyoma, schwannoma, lipoma, and ectopic pancreas, to malignant lesions, such as neuroendocrine tumor or gastrointestinal stromal tumor (GIST).
Since it is difficult to differentiate malignant from benign lesions exclusively by white-light endoscopy, several techniques have been introduced for the accurate diagnosis of SETs (such as endoscopic ultrasonography [EUS] and computed tomography [CT]). Although EUS is known as the most useful diagnostic modality for SETs, its diagnostic accuracy is limited because of its inability to provide histopathological diagnosis. Pre-treatment histopathological diagnosis of SETs can help establish a treatment plan in patients with SETs. Therefore, techniques for tissue acquisition, such as bite-on-bite forceps biopsy and EUS-guided fine-needle aspiration (EUS-FNA), have been introduced. However, bite-on-bite forceps biopsy sampling cannot yield adequate amounts of subepithelial tissue for definitive diagnosis, which results in an unsatisfactory diagnostic accuracy of 17–42% [3, 4]. Although EUS-FNA is a good modality for procuring tissue from GI SETs, it has a limited sample adequacy (80.6%) and a low diagnostic accuracy (64%) according to a recent meta-analysis [5]. This limitation is probably caused because the acquisition of cells via EUS-FNA does not always include the stroma or related tissue structures, which are necessary for definitive histopathological diagnosis [5]. Since GI mesenchymal tumors, such as GIST, schwannoma, and leiomyoma, have similar morphologic appearances, diagnosis based on a small amount of specimen obtained by EUS-FNA is not reliable; therefore, immunohistochemical analysis is highly advisable in these SETs [6]. To overcome the limitations of previous methods, EUS-guided fine-needle biopsy (EUS-FNB) was recently introduced. Sampling via EUS-FNB facilitates the procurement of macroscopic tissue cores and preservation of the cellular structure, which enables to perform immunohistopathological analysis [7]. A recent meta-analysis showed that the sample adequacy and diagnostic accuracy of EUS-FNB are acceptable (94.9% and 87.9%, respectively) [5].
Recent guidelines for SETs suggest that when SETs < 2 cm in size are detected, they can usually be followed up by periodic endoscopy or EUS once or twice a year until the SETs increase in size or become symptomatic, even if they are diagnosed as GISTs subsequently [1, 8,9,10]. When SETs are 2–5 cm in size, the decision-making policy can be discussed with patients regarding whether to make a histopathological diagnosis (for example, by EUS-FNB) or whether to use modalities such as EUS or CT [10]. In case of GISTs or other malignant lesions, the patient should undergo further endoscopic or surgical treatment, and in case of benign lesions, such as leiomyoma or schwannoma, serial follow-up is usually performed [8, 10, 11]. SETs ≥ 5 cm in size are recommended for surgical resection and subjected to histopathological examination [8, 9]. Herein, we aimed to evaluate the diagnostic performance of EUS-FNB, such as the diagnostic yield and capability of EUS-FNB in discriminating malignant from non-malignant lesions, in upper GI SETs of 2–5 cm in size.
Patients and methods
Study population
Between January 2013 and February 2020, 78 patients who underwent EUS-FNB for GI SETs at Pusan National University Hospital (Busan, Korea) were retrospectively enrolled in this study. Of these patients, seven patients with tumor in the rectum and eight patients with tumor size < 2 cm or ≥ 5 cm were excluded. Finally, a total of 63 patients with upper GI SETs of 2–5 cm in size were included in the analysis. This study was reviewed and approved by the Pusan National University Hospital Institutional Review Board (IRB number, 2110-002-107).
EUS-FNB procedure
All procedures were performed using a linear array echoendoscope (GF-C2000 or UCT 260; Olympus, Tokyo, Japan) by a single experienced endoscopist (Kim GH) with the patients placed in the left lateral decubitus position under intravenous conscious sedation (midazolam with or without propofol). After the target lesion was endosonographically visualized, a 20- or 22-gauge ProCore needle (EchoTip ProCore; Wilson-Cook Medical, USA) was advanced into the target lesion under endosonographic guidance. After penetrating the lesion, the endoscopist moved the needle to-and-fro for more than 10 to 15 times within the lesion, while an assistant simultaneously pulled out the stylet slowly and continuously over 20 s to achieve minimal negative pressure within the needle (slow-pull technique) [6]. After sufficient sampling, the needle was withdrawn from the lesion.
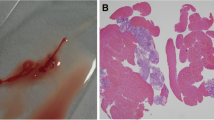
Histopathological analysis
EUS-FNB samples were harvested and stored for subsequent processing by the endoscopist. The specimens were expelled onto slides by re-insertion of a stylet or by flushing air into the needle assembly to harvest the tissue core. Subsequently, the endoscopist inspected the materials on the slides and determined whether the tissue cores were optimal—defined as whitish pieces of tissue with apparent bulk. If the core tissues were visible macroscopically, they were lifted off with a filter paper strip and fixed in formalin. The histopathological diagnosis was based on hematoxylin and eosin staining with or without immunohistochemical staining for CD34, CD117, DOG1, S-100, and smooth muscle actin. When the morphological characteristics of tumors were nonspecifically mesenchymal, a diagnosis by EUS-FNB was only considered true positive when immunohistochemical analysis was conclusive. For patients who underwent endoscopic or surgical resection for SETs, the final diagnosis was made based on histopathological assessment of the resected specimen. Otherwise, histopathological assessment of the EUS-FNB specimens was regarded as the gold standard for diagnosis.
Outcome parameters
The primary outcome was the diagnostic performance of EUS-FNB in upper GI SETs of 2–5 cm in size; diagnostic yield of EUS-FNB, and capability of EUS-FNB in discriminating malignant from non-malignant lesions. The diagnostic yield of EUS-FNB was defined as the rate of cases in which acquisition of adequate tissue specimen for histopathological interpretation was achieved. The capability of EUS-FNB in discriminating malignant from non-malignant lesions was evaluated based on the assumption that EUS-FNB could definitely diagnose malignant lesions based on the histopathological results of EUS-FNB specimens alone. Because inadequate results on EUS-FNB specimens could not definitely rule out a possibility of malignant lesion, such cases were included in the category of the malignant lesions for analysis. Additionally, the factors of SETs and EUS-FNB influencing the diagnostic yield of EUS-FNB were analyzed. The secondary outcome was the histopathological concordance between EUS-FNB specimens and resected specimens for cases that were endoscopically or surgically resected after EUS-FNB.
Statistical analysis
Descriptive statistics were used to document the characteristics of SETs and procedure-related outcomes. Continuous variables are presented as median values with range, and categorical variables are presented as numbers with percentage. Sensitivity, specificity, and accuracy were calculated for the capability of EUS-FNB in discriminating malignant from non-malignant lesions. To evaluate the factors that were associated with diagnostic yield of EUS-FNB, χ2 or Fisher’s exact test was used. A p value < 0.05 was considered statistically significant. The statistical analyses were performed using the SPSS version 25.0 for Windows software (SPSS Inc., Chicago, IL, USA).
Results
Baseline characteristics of patients with SETs and EUS-FNB
The baseline clinical and endosonographic characteristics of 63 patients (63 SETs) are summarized in Table 1. Of the 63 patients, 32 were men and 31 were women (median age 56.0 years; range 17–81 years). Most tumors (50/63, 79.4%) were located in the stomach, and the median tumor size was 2.5 cm (range 2.0–4.9 cm). EUS-FNB was performed until adequate macroscopically visible tissue cores were obtained. According to the location of SETs and availability of needles, 20-gauge needles were used in 33 patients and 22-gauge needles in 30 patients. In six cases (9.5%), adequate macroscopic tissue cores were not obtained. Therefore, the needle size of EUS-FNB was changed from 22 to 20 gauge in five cases (three cases located in the mid-esophagus and two cases in the upper third of the stomach), and from 20 to 22 gauge in one case (located in the middle third of the stomach); subsequently, adequate macroscopic tissue cores were procured in all six cases. The median value of needle passes performed was 4 (range 2–8).
After EUS-FNB, bleeding and abscess formation occurred in 3 (4.8%) patients and 1 (1.6%) patient, respectively. All bleeding was mild intra-procedural bleeding, which was managed successfully with endoscopic hemostasis using hemoclips. Abscess was encountered 2 days after EUS-FNB in one patient with the SET located in the lower esophagus. The patient was treated successfully with EUS-guided abscess drainage and intravenous antibiotics.
Diagnostic performance of EUS-FNB for SETs
Successful acquisition of macroscopic tissue cores was possible in all 63 cases, but the sampling specimens were insufficient to make a definitive histopathological diagnosis in five cases. Therefore, the diagnostic yield of EUS-FNB was 92.1% (58/63). Based on the histopathological results of EUS-FNB, 26 were diagnosed with leiomyoma, 21 with GIST, six with schwannoma, two with ectopic pancreas, one with squamous cell carcinoma (SCC), one with ectopic splenosis, and one with abscess (Table 2). There were no significant differences in the diagnostic yield in relation to tumor location, tumor size, and number of needle passes (Table 3). The diagnostic yield with a 20-gauge EUS-FNB needle was higher than that with a 22-gauge EUS-FNB needle, but this did not reach statistical significance (97.0% vs. 86.7%, p = 0.183).
Based on the results of EUS-FNB, 27 cases (including five non-diagnostic cases) were classified as malignant lesions and 36 cases as non-malignant lesions. Accordingly, the sensitivity, specificity, and accuracy of EUS-FNB in discriminating malignant from non-malignant lesions were 100% (95% confidence interval [CI] 85.3–100%), 87.8% (95% CI 79.9–87.8%), and 92.1% (95% CI 81.8–92.1%), respectively (Table 4).
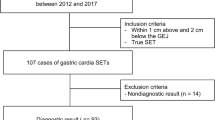
Management of patients with SETs
Figure 1 shows the flowchart depicting the management of patients included in this study. Of the 21 patients with GIST, 15 patients underwent surgical resection and one underwent endoscopic resection; two GISTs were diagnosed as very low risk, 10 as low risk, and four as intermediate risk, based on National Institute of Health classification. The remaining five patients with GIST did not undergo surgical resection; four patients refused surgical resection due to old age or concurrent diseases, and one patient underwent imatinib treatment for recurrent GIST. One patient with esophageal SCC was treated with chemotherapy due to poor general condition. Of the 36 patients diagnosed with non-malignant lesions based on EUS-FNB, three patients with leiomyoma and three with schwannoma underwent surgical resection, and one patient with leiomyoma underwent endoscopic resection due to the increase in size during follow-up and presence of symptoms or bleeding risk (presence of ulceration on the surface of SETs). An additional one patient with schwannoma underwent surgical resection due to the patient’s request. Of the five patients with non-diagnostic results, two patients underwent surgical resection and the final histopathology was schwannoma in both patients. The remaining three patients were followed up without increase in size for 24 months or longer.
Histopathological concordance between EUS-FNB specimens and resected specimens
Histopathological concordance between EUS-FNB specimens and resected specimens is described in Table 5. After EUS-FNB, 24 patients (15 with GIST, three with leiomyoma, four with schwannoma, and two with non-diagnostic results) underwent surgical resection and two patients (one with GIST and one with leiomyoma) underwent endoscopic resection. Finally, 16 cases were diagnosed with GIST, four with leiomyoma, and six with schwannoma in the resected specimens. The histopathological concordance rate was 100% (24/24), excluding the two cases with inadequate results on EUS-FNB specimens.
Discussion
Recently, GI SETs have become one of the most commonly encountered lesions during endoscopy. When managing patients with a GI SET, the important point to consider is whether the SET has malignant potential. However, since conventional endoscopic forceps biopsy cannot reveal accurate information on the malignant potential in most cases of SETs, especially those located in the proper muscle layer, their clinical management is mainly determined by their size. SETs < 2 cm in size are usually followed up, and SETs ≥ 5 cm in size should be surgically resected. The management of SETs of 2–5 cm in size differs according to the histopathological diagnosis. Therefore, we focused the diagnostic yield of EUS-FNB for SETs of 2–5 cm in size. Macroscopically optimal tissue cores were obtained for all 63 SETs, and the diagnostic yield of EUS-FNB was 92.1%. Furthermore, the sensitivity and specificity of EUS-FNB in discriminating malignant from non-malignant lesions were 100% and 87.8%, respectively.
Although EUS-FNA has been used for tissue acquisition of SETs in the past, its diagnostic yield was not satisfactory. To overcome the limitations of EUS-FNA, newly designed special needles, such as a reverse-bevel needle (EchoTip ProCore; Wilson-Cook Medical), a needle with fork-tip design (SharkCore; Medtronic, USA), or a needle with symmetric cutting edges (Acquire; Boston Scientific, USA), were developed for use in EUS-FNB. These needles can improve tissue capture and enable macroscopic on-site evaluation for optimal tissue cores by an endoscopist without a cytopathologist [12]. In the present study, EUS-FNB was performed using ProCore needles, and the endoscopist himself evaluated the macroscopic tissue cores immediately after every needle pass. As a result, the macroscopically optimal tissue acquisition and diagnostic rates of EUS-FNB for upper GI SETs were 100% and 92.1%, respectively. These results are consistent with those of other recent studies in which the diagnostic yields of EUS-FNB were 64.3–86.9% [13,14,15]. According to a recent meta-analysis, the sample adequacy and diagnostic yield of EUS-FNB for GI SETs were 94.9% and 89.7%, respectively, and EUS-FNB outperformed EUS-FNA in all diagnostic outcomes [5].
We tried to identify the factors that influence the diagnostic yield of EUS-FNB. The diagnostic yield was higher with 20-gauge EUS-FNB needles than with 22-gauge EUS-FNB needles, but without any statistical significance. Tumor location, tumor size, and the number of needle passes were not associated with the diagnostic yield. These results are consistent with those of previous studies, which state that the diagnostic yield of EUS-FNB is not associated with tumor size and location, needle size, and number of needle passes [16, 17]. Several studies have reported that a large tumor size (≥ 2 cm) was related to a higher diagnostic yield of EUS-FNB compared with a small tumor size (< 2 cm) [13, 18, 19]. In the present study, only SETs of 2–5 cm in size were included.
We also evaluated the capability of EUS-FNB in discriminating malignant from non-malignant lesions, which is important when managing SETs of 2–5 cm in size. In a previous study that included 70 SETs ≥ 2 cm in size, the sensitivity and accuracy of EUS-FNB for diagnosing malignant lesions were 90% and 83%, respectively [16]. Similarly, in the present study, the sensitivity, specificity, and accuracy of EUS-FNB in discriminating malignant from non-malignant lesions were 100%, 87.8%, and 92.1%, respectively. Our results confirmed that EUS-FNB is an effective diagnostic modality in decision-making during the management of upper GI SETs of 2–5 cm in size.
In terms of safety of EUS-FNB, many studies have reported adverse event rates as 1.2–5.7% and the most common adverse event being minor bleeding [7, 13, 15, 16, 18,19,20]. Similarly, in the present study, adverse events occurred in four (6.4%) patients—minor intra-procedural bleeding in three patients and abscess formation in one patient. All these adverse events occurred with the 20-gauge needle, and the patient with abscess formation was treated successfully with EUS-guided abscess drainage and intravenous antibiotics. Although the incidence of abscess formation occurring after EUS-FNB is very low, it could lead to severe sepsis [21]. Therefore, when a patient complains of infection signs, such as fever, chilling, or persistent pain after EUS-FNB, the possibility of abscess formation should be considered and cases should be treated with intravenous antibiotics and endoscopic drainage [22].
Because EUS-FNB provides only small amounts of tissues for histopathological analysis, the histopathological concordance between EUS-FNB and resected specimens is important and should be validated. In previous studies, the histopathological concordance rate between EUS-FNB and surgical specimens were 100% in cases diagnosed as GIST in EUS-FNB [15, 17]. Similarly, in the present study, the histopathological concordant rate was 100% in 16 GISTs, four leiomyomas, and four schwannomas, excluding two cases with inadequate results on EUS-FNB specimens. Although we did not evaluate the difference in mitotic index between EUS-FNB and resected specimens, a recent study showed that the concordance rate of the mitotic index between EUS-FNB and surgical specimens in GIST was 89.7% [20].
This study has several limitations. First, this was a single-center retrospective study that evaluated the diagnostic yield of EUS-FNB for SETs. Therefore, the patients were selected to undergo EUS-FNB based on the endoscopists’ clinical opinions and the patients’ needs. Second, all EUS-FNB procedures were performed by a single experienced endoscopist. Because tissue acquisition through EUS-FNB requires a high level of technical skill and expertise, the diagnostic performance of EUS-FNB might vary depending on the endoscopists. Third, the immediate cytologic assessment after EUS-FNB by a cytopathologist is not available in our hospital. Therefore, the endoscopist performed the macroscopic assessment of sample adequacy after every needle pass, which could decrease the adequacy of tissue acquisition and increase the number of needle passes. However, recent studies have demonstrated the diagnostic feasibility of macroscopic on-site evaluation of the EUS-FNB specimen by an endoscopist [12, 23, 24]. Further, there was only one case of duodenal SET. Considering the low incidence and high malignant potential of duodenal mesenchymal tumors, the low number of duodenal SETs included in the present study seems unavoidable.
In conclusion, EUS-FNB provided high diagnostic yield and high capability in discriminating malignant from non-malignant lesions in upper GI SETs of 2–5 cm in size. Therefore, EUS-FNB is an effective diagnostic modality that aids clinical decision-making for the management of upper GI SETs of 2–5 cm in size. Further prospective, multicenter studies are needed to validate our results in a large number of cases of upper GI SETs.
References
Hwang JH, Rulyak SD, Kimmey MB (2006) American gastroenterological association institute technical review on the management of gastric subepithelial masses. Gastroenterology 130:2217–2228
Choe Y, Cho YK, Kim GH, Kim JH, Kim TH, Kim ES, Choi EK, Choi JH, Kim SH, Kim DH (2020) The prevalence, natural course, and clinical practice of upper gastrointestinal subepithelial tumors in Korea. Gastrointest Endosc 91:AB321
Cantor MJ, Davila RE, Faigel DO (2006) Yield of tissue sampling for subepithelial lesions evaluated by EUS: a comparison between forceps biopsies and endoscopic submucosal resection. Gastrointest Endosc 64:29–34
Kim GH (2021) Systematic endoscopic approach for diagnosing gastric subepithelial tumors. Gut Liver 16:19–27
Facciorusso A, Sunny SP, Del Prete V, Antonino M, Muscatiello N (2020) Comparison between fine-needle biopsy and fine-needle aspiration for EUS-guided sampling of subepithelial lesions: a meta-analysis. Gastrointest Endosc 91:14-22.e12
Kim GH, Cho YK, Kim EY, Kim HK, Cho JW, Lee TH, Moon JS (2014) Comparison of 22-gauge aspiration needle with 22-gauge biopsy needle in endoscopic ultrasonography-guided subepithelial tumor sampling. Scand J Gastroenterol 49:347–354
Lee JH, Cho CJ, Park YS, Ahn JY, Kim DH, Na HK, Choi KD, Song HJ, Lee GH, Jung HY (2016) EUS-guided 22-gauge fine needle biopsy for the diagnosis of gastric subepithelial tumors larger than 2 cm. Scand J Gastroenterol 51:486–493
Nishida T, Blay J-Y, Hirota S, Kitagawa Y, Kang Y-K (2016) The standard diagnosis, treatment, and follow-up of gastrointestinal stromal tumors based on guidelines. Gastric Cancer 19:3–14
Nishida T, Kawai N, Yamaguchi S, Nishida Y (2013) Submucosal tumors: comprehensive guide for the diagnosis and therapy of gastrointestinal submucosal tumors. Dig Endosc 25:479–489
Nishida T, Hirota S, Yanagisawa A, Sugino Y, Minami M, Yamamura Y, Otani Y, Shimada Y, Takahashi F, Kubota T (2008) Clinical practice guidelines for gastrointestinal stromal tumor (GIST) in Japan: English version. Int J Clin Oncol 13:416–430
Demetri GD, von Mehren M, Antonescu CR, DeMatteo RP, Ganjoo KN, Maki RG, Pisters PW, Raut CP, Riedel RF, Schuetze S, Sundar HM, Trent JC, Wayne JD (2010) NCCN Task Force report: update on the management of patients with gastrointestinal stromal tumors. J Natl Compr Cancer Netw 8(Suppl 2):S1–S41 (quiz S42–44)
So H, Seo DW, Hwang JS, Ko SW, Oh D, Song TJ, Park DH, Lee SK, Kim MH (2021) Macroscopic on-site evaluation after EUS-guided fine needle biopsy may replace rapid on-site evaluation. Endosc Ultrasound 10:111–115
Park J, Park JC, Jo JH, Kim EH, Shin SK, Lee SK, Lee YC (2019) Prospective comparative study of endoscopic ultrasonography-guided fine-needle biopsy and unroofing biopsy. Dig Liver Dis 51:831–836
Iglesias-Garcia J, Poley JW, Larghi A, Giovannini M, Petrone MC, Abdulkader I, Monges G, Costamagna G, Arcidiacono P, Biermann K, Rindi G, Bories E, Dogloni C, Bruno M, Dominguez-Muñoz JE (2011) Feasibility and yield of a new EUS histology needle: results from a multicenter, pooled, cohort study. Gastrointest Endosc 73:1189–1196
Kim GH, Ahn JY, Gong CS, Kim M, Na HK, Lee JH, Jung KW, Kim DH, Choi KD, Song HJ, Lee GH, Jung H-Y (2020) Efficacy of endoscopic ultrasound-guided fine-needle biopsy in gastric subepithelial tumors located in the cardia. Dig Dis Sci 65:583–590
Hedenström P, Marschall HU, Nilsson B, Demir A, Lindkvist B, Nilsson O, Sadik R (2018) High clinical impact and diagnostic accuracy of EUS-guided biopsy sampling of subepithelial lesions: a prospective, comparative study. Surg Endosc 32:1304–1313
Lee M, Min BH, Lee H, Ahn S, Lee JH, Rhee PL, Kim JJ, Sohn TS, Kim S, Kim KM (2015) Feasibility and diagnostic yield of endoscopic ultrasonography-guided fine needle biopsy with a new core biopsy needle device in patients with gastric subepithelial tumors. Medicine (Baltimore) 94:e1622
Inoue T, Okumura F, Sano H, Mizushima T, Tsukamoto H, Fujita Y, Ibusuki M, Kitano R, Kobayashi Y, Ishii N, Ito K, Yoneda M (2019) Impact of endoscopic ultrasound-guided fine-needle biopsy on the diagnosis of subepithelial tumors: a propensity score-matching analysis. Dig Endosc 31:156–163
Sekine M, Miura T, Fujiwara J, Uehara T, Asano T, Matsumoto S, Miyatani H, Mashima H (2021) Utility of endoscopic ultrasonography-guided fine-needle biopsy (EUS-FNB) for diagnosing small subepithelial lesions (< 20 mm). J Ultrasound 25:35–40
Kamata K, Kurita A, Yasukawa S, Chiba Y, Nebiki H, Asada M, Yasuda H, Shiomi H, Ogura T, Takaoka M, Hoki N, Ashida R, Shigekawa M, Yanagisawa A, Kudo M, Kitano M (2021) Utility of a 20G needle with a core trap in EUS-guided fine-needle biopsy for gastric submucosal tumors: a multicentric prospective trial. Endosc Ultrasound 10:134–140
Polkowski M, Gerke W, Jarosz D, Nasierowska-Guttmejer A, Rutkowski P, Nowecki ZI, Ruka W, Regula J, Butruk E (2009) Diagnostic yield and safety of endoscopic ultrasound-guided trucut [corrected] biopsy in patients with gastric submucosal tumors: a prospective study. Endoscopy 41:329–334
DeWitt J, Al-Haddad M, Fogel E, Sherman S, LeBlanc JK, McHenry L, Schmidt CM (2009) Endoscopic transduodenal drainage of an abscess arising after EUS-FNA of a duodenal GI stromal tumor. Gastrointest Endosc 70:185–188
Chong CCN, Lakhtakia S, Nguyen N, Hara K, Chan WK, Puri R, Almadi MA, Ang TL, Kwek A, Yasuda I, Doi S, Kida M, Wang HP, Cheng TY, Jiang Q, Yang A, Chan AWH, Chan S, Tang R, Iwashita T, Teoh AYB (2020) Endoscopic ultrasound-guided tissue acquisition with or without macroscopic on-site evaluation: randomized controlled trial. Endoscopy 52:856–863
Iwashita T, Yasuda I, Mukai T, Doi S, Nakashima M, Uemura S, Mabuchi M, Shimizu M, Hatano Y, Hara A, Moriwaki H (2015) Macroscopic on-site quality evaluation of biopsy specimens to improve the diagnostic accuracy during EUS-guided FNA using a 19-gauge needle for solid lesions: a single-center prospective pilot study (MOSE study). Gastrointest Endosc 81:177–185
Author information
Authors and Affiliations
Contributions
GHK: conception and design of this work; DCJ and GHK: acquisition and interpretation of data, drafting this work; MWL, BEL, DHB, and GAS revising it critically for important intellectual content. All authors approve the manuscript in its current form for publication and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Disclosures
Dong Chan Joo, Gwang Ha Kim, Moon Won Lee, Bong Eun Lee, Dong Hoon Baek, Geun Am Song have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Joo, D.C., Kim, G.H., Lee, M.W. et al. Diagnostic performance of endoscopic ultrasonography-guided fine-needle biopsy in upper gastrointestinal subepithelial tumors measuring 2–5 cm in size. Surg Endosc 36, 8060–8066 (2022). https://doi.org/10.1007/s00464-022-09243-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09243-5