Abstract
Background
The aim of this study was to evaluate the use of laparoscopic surgery for common emergency general surgery (EGS) procedures within an integrated Acute Care Surgery (ACS) network. We hypothesized that laparoscopy would be associated with improved outcomes.
Methods
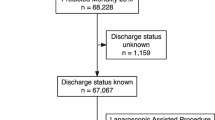
Our integrated health care system’s EGS registry created from AAST EGS ICD-9 codes was queried from January 2013 to October 2015. Procedures were grouped as laparoscopic or open. Standard descriptive and univariate tests were performed, and a multivariable logistic regression controlling for open status, age, BMI, Charlson Comorbidity Index (CCI), trauma tier, and resuscitation diagnosis was performed. Laparoscopic procedures converted to open were identified and analyzed using concurrent procedure billing codes across episodes of care.
Results
Of 60,604 EGS patients identified over the 33-month period, 7280 (12.0%) had an operation and 6914 (11.4%) included AAST-defined EGS procedures. There were 4813 (69.6%) surgeries performed laparoscopically. Patients undergoing a laparoscopic procedure tended to be younger (45.7 ± 18.0 years vs. 57.2 ± 17.6, p < 0.001) with similar BMI (29.7 ± 9.0 kg/m2 vs. 28.8 ± 8.3, p < 0.001). Patients in the laparoscopic group had lower mean CCI score (1.6 ± 2.3 vs. 3.4 ± 3.2, p ≤ 0.0001). On multivariable analysis, open surgery had the highest association with inpatient mortality (OR 8.67, 4.23–17.75, p < 0.0001) and at all time points (30-, 90-day, 1-, 3-year). At all time points, conversion to open was found to be a statistically significant protective factor.
Conclusion
Use of laparoscopy in EGS is common and associated with a decreased risk of all-cause mortality at all time points compared to open procedures. Conversion to open was protective at all time points compared to open procedures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Acute Care Surgery (ACS) is composed of the three pillars of Trauma, Surgical Critical Care (SCC), and Emergency General Surgery (EGS) [1, 2]. Unlike the first two disciplines listed above, the evaluation of EGS outcomes is relatively new. In 2012 the American Association for the Surgery of Trauma (AAST) proclaimed the need for more research and quality improvement in EGS [3, 4] and consequently a defined set of EGS ICD-9 codes were endorsed by the AAST [5]. This code-set elucidated that EGS has one of the highest burdens of disease in the USA with over 4 million admissions per year [5] and higher incidence rates than diabetes, cardiovascular disease, and cancer [6]. Readmissions within this group of conditions range from approximately 6% to 15.5% [7]. EGS procedures are estimated to account for over 50% of all complications [6, 8], 50% of all surgical mortality [4, 9,10,11], and cost over $28 billion USD in 2010 [12].
In contrast to trauma, no structured system exists to evaluate and coordinate the care of the EGS patient. Further, national data suggest that the majority of EGS is performed outside of large academic tertiary medical centers [8, 13]. Because the majority of EGS cases exist outside academic centers, a lack of in-depth analysis of the regional differences in EGS outcomes results in a significant challenge to improving quality of care and reducing mortality.
Surgeons have a broad set of technical skills but may have varying levels of laparoscopic expertise. Graduating general surgeons are increasingly being exposed to a broader set of minimally invasive techniques for a wider set of indications [14, 15]. Currently, a lack of data exists regarding the use of laparoscopy across the scope of EGS conditions and practice environments, from community-based practice to tertiary centers.
The principal aim of this study was to define how EGS procedures within our integrated regional healthcare system are approached and to evaluate all-cause mortality across EGS procedures by laparoscopic vs open procedure type. We hypothesized that patients would be more likely to undergo laparoscopic surgeries at tertiary care centers and would have reduced mortality compared to those undergoing open procedures.
Methods
Patient population and data source
Atrium Health is an integrated health care system composed of over 40 hospital and acute care facilities in the Southeast. It includes 13 hospitals in the Charlotte metropolitan area, including a pediatric hospital, two ACS-Verified Level III, and the region’s only Level I Trauma Center, totaling over 2600 hospital beds. These facilities share a common EMR, billing software, physician transfer line, helicopter EMS service, and similar oversight of county-based EMS medical directorship. Surgeons operating at these facilities are composed of both fellowship-trained physicians in Acute Care Surgery, as well as General Surgeons operating in the community. Given these commonalities, shared experience and data, variable practice patterns, and majority of the market share in the region, this system was chosen to examine the practice patterns of EGS procedures within a regional system.
The AAST-defined EGS ICD-9 diagnosis codes identified by Shafi et al. were used to query our electronic data warehouse (EDW) from the beginning of reliable system billing data, January 1, 2013 to October 1, 2015, when ICD-10 codes were introduced in the USA [5]. Inpatient and observation admissions, classified as emergent encounters within our administrative dataset, with an AAST EGS diagnosis code in any code position were included. Eight of the facilities had complete billing data for the entire time period and were included in the analysis. All facilities are located in the Charlotte, North Carolina metropolitan area. No AAST-defined codes were excluded. Patients less than age 18 and outpatient encounters were excluded.
Variables, diagnosis, and procedure code grouping
Patient encounters identified by ICD-9 billing codes were aligned with demographic and administrative data from the EDW and post-discharge survival was elicited from the Social Security Death Index (SSDI). Variables included were age, sex, body mass index (BMI), hospital trauma tier level, comorbidities, Charlson Comorbidity Index [16, 17], length of stay, and discharge disposition.
Patients were then classified according to their diagnosis categories as defined per the original AAST code-set into the following 10 diagnosis groups: resuscitation, general abdominal, intestinal obstruction, upper gastrointestinal (UGI), hepatopancreatobiliary (HPB), colorectal, hernia, soft tissue, vascular, and cardiothoracic. Patients were identified by ICD-9 procedure codes who underwent a procedure that contributed to the most common EGS procedures as established by Scott et al. that account for 80% of all procedures, 80.3% of all deaths, 78.9% of all complications, and 80.2% of all costs in EGS patients [9]. These were partial colectomy, small bowel resection, cholecystectomy, peptic ulcer operations, lysis of adhesions (LOA), appendectomy, and laparotomy.
Study design
After examination of the entire patient population to evaluate the regional burden of EGS, an analysis of mortality outcomes by procedure type (open vs laparoscopic) was performed. The diagnosis codes for common laparoscopic and open EGS cases and their grouping are displayed in Table 1. Patient demographics, diagnoses, operations, and outcomes were compared between these two groups. The primary endpoint was inpatient mortality and secondary endpoints were 30- and 60-day and 1- and 3-year mortality rates. For diagnosis codes where an open procedure code was listed, the procedure was categorized as “open.” Procedures with only laparoscopic codes listed were deemed “laparoscopic.” If a procedure listed both open and laparoscopic codes, it was coded as “conversion” to open. Conversion was coded as a separate variable in the multivariate regression analysis.
Statistical analysis
All data were analyzed using Statistical Analysis Software, version 9.3 (SAS Institute, Inc., Cary, NC), after the study was approved by the Carolinas Medical Center Institutional Review Board. Descriptive statistics were reported as means with corresponding standard deviations for continuous variables and percentages for categorical variables. Global univariate analyses were between patients by open vs lap status. Categorical variables were evaluated using Pearson’s chi-squared and Fisher’s exact test where appropriate. Continuous and ordinal variables were evaluated using Wilcoxon–Mann–Whitney and the Kruskal–Wallis tests. Multivariable reverse stepwise logistic regression was performed to evaluate the open versus laparoscopic procedure type and inpatient mortality, controlling for key confounding variables which were established a priori. These included standard demographics (age, sex, BMI group, CCI), conversion to open, and diagnoses and procedures shown to have high rates of mortality on prior national EGS studies (obstruction, resuscitation and soft tissue diagnoses, laparotomy, and number of procedures performed). Odds ratios with corresponding 95% confidence intervals were used to report the results of the multivariate regression models. Statistical significance was set at p < 0.05, and all reported p values are two-tailed.
Results
Of 60,604 EGS patients identified over the 33-month period, 7280 (12.0%) had an operation and 6914 (11.4%) included the above surgery types. There were 4813 (69.6%) surgeries performed laparoscopically. Table 2 demonstrates an overview of patient characteristics included in this study by laparoscopic vs open status. Patients undergoing a laparoscopic procedure tended to be younger (45.7 ± 18.0 years vs 57.2 ± 17.6, p < 0.001). Roughly half of patients in both groups were female and BMI was roughly similar (29.7 ± 9.0 kg/m2 vs 28.8 ± 8.3, p < 0.001). Patients in the laparoscopic group had on average a lower Charlson Comorbidity Index (1.6 ± 2.3 vs 3.4 ± 3.2, p < 0.0001).
Procedure type by diagnosis, location, and operation
Patient procedures are displayed by location, diagnosis type, and AAST-defined diagnosis groups in Table 3. Of note, disease and operative categories are not mutually exclusive and therefore percentages are not cumulative to 100%. The highest magnitude of procedures were performed at non-trauma centers within the integrated health care system, making up 55.0% of laparoscopic procedures and 40.9% of open procedures. As shown in Fig. 1, the diagnosis of cholecystitis and appendicitis were most prevalent in patients receiving a laparoscopic procedure, and hepatopancreatobiliary (HPB) diagnosis groups made up 53.8% of laparoscopic procedures. Patients with ventral hernia diagnosis codes were most commonly treated using an open procedure. When patients did undergo a laparoscopic procedure for ventral hernia, it was almost always for a non-incarcerated ventral hernia repair. Incarcerated ventral hernias were most often corrected using an open approach (42 vs 311 cases) and all strangulated ventral hernias were performed open. A similar trend was found among inguinal hernia repair, with the majority of cases using an open approach. Across AAST-defined diagnosis groups, intestinal obstruction and upper GI tract conditions were listed most commonly for open procedures (38.4% and 54.9%, respectively).
The percentage of operations by type are found in Table 4. Appendectomy and cholecystectomy were the most common laparoscopic procedures performed, whereas colorectal procedures codes were involved in 83% of all open EGS procedures. Ventral and inguinal hernias were more likely to be performed in an open fashion, whereas umbilical hernia repairs were split. All umbilical hernia repairs with mesh were done laparoscopically (8 total) versus 177 cases without mesh performed in an open fashion. The majority of appendectomies and cholecystectomies were performed laparoscopically (1949 vs 253 and 2580 vs 312, respectively). Peptic ulcer disease repair, small bowel resection, and intestinal anastomoses were all primarily approached with open procedures. Lysis of adhesions had a mixed procedure type, with approximately one-third performed laparoscopically (209 vs 631).
Patient mortality by operation type
Mortality over time by open surgery status is displayed in Fig. 2 and was statistically higher at all time points in the open group (p < 0.001 for all). On multivariable analysis (Table 5), open surgery had the highest association with inpatient mortality with an OR 8.67 (4.23–17.75), which was followed by resuscitation diagnosis, OR 7.68 (5.05–11.7), and age 65 + OR 3.27 (1.4–7.62). A similar trend was seen for 30- and 90-day and 1- and 3-year mortality as shown in Table 6. Odds of mortality for open procedures decreased at each time point, with the lowest being at year 3 (OR 2.13, 95% CI 1.7–2.7). At all time points, operations at non-trauma centers had an OR less than or equal to 1.00.
In this dataset, 181 procedures were characterized by diagnosis codes that included both laparoscopic and open procedure codes indicating a conversion to open during the case. At all time points, conversion to open was found to be a statistically significant protective factor. For inpatient mortality, patients with conversion to open had an OR 0.18 (0.04–0.82; p = 0.03). OR for conversion to open continued to protective (OR < 1) across 30- and 90-day and 1- and 3-year mortality, with a trend toward decreased odds of mortality in early recovery when compared to open cases (Lowest OR 0.18 for inpatient stay versus OR 0.43 for 3-year mortality).
Discussion
The evidence provided in this study illustrates that EGS procedures at hospitals in a large integrated health care system are most often approached via minimally invasive techniques and, when done in this matter, are associated with a decreased risk of mortality at all time points. We found that patients undergoing laparoscopic procedures tended to be younger with similar BMIs and on average had a lower CCI compared to those undergoing open procedures. Having an open procedure with an emergency general surgery diagnosis code was an independent risk factor for inpatient mortality. However, patients undergoing laparoscopy that converted to open had decreased mortality at all time points compared to those undergoing open procedures. A key to understanding this result, and other similar studies, is that patient physiology, hemodynamics, and level of contamination and/or obstruction often dictate the ability to pursue a laparoscopic approach. Furthermore, if laparoscopy is feasible to attempt, the known benefits of laparoscopic surgery do translate to EGS patients.
The findings from this study are similar to what has been found internationally regarding the use of minimally invasive techniques. Overall, the use of laparoscopy has been increasing in abdominal emergency operations [18]; and a laparoscopic approach has shown to provide benefit in multiple EGS disease processes [19,20,21]. Laparoscopic procedures in emergency surgery in the past have not always been recommended due to concerns regarding patient physiology, lack of overall laparoscopic training, and/or experience with laparoscopic emergencies [22]. However, uptake of laparoscopic skills has increased with newly trained general and acute care surgeons [23, 24], and it is clear from our data that this trend is continuing in the USA both in Level I trauma centers and non-trauma centers. In fact, our data show that non-trauma centers perform the majority of these minimally invasive procedures. Since 2008, the ACGME further increased case requirements for minimally invasive surgeries in general surgery residency training programs [25], further signaling the importance of minimally invasive surgical techniques.
It has been shown that laparoscopic procedures can be safe and associated with reduced length of stay, early resumption of daily activities, and earlier return to work [26,27,28,29]. Our data further these findings in regard to all-cause mortality demonstrating that open procedures have an increased risk of death at all time points compared to laparoscopic procedures. The majority of procedures done laparoscopically were for biliary disease and appendicitis. This has been shown to be standard of care across Europe and is an expected result for a large integrated health care system in the USA [30]. In contrast, the majority of open procedures involved colorectal and small bowel obstruction diagnosis codes. It has been shown that laparoscopy can be a safe first approach in these diagnosis groups as well. A systematic review of laparoscopy for small bowel obstruction and lysis of adhesions showed a success rate of 64% and when completed, patients undergoing minimally invasive techniques had reduced morbidity and length of stay [31].
The magnitude of open procedures on mortality outcomes found in our study therefore may be less due to the safety of the surgical approach or the laparoscopic expertise and experience of the surgeon, but more likely due to the presenting physiology. Without significant clinical data (vitals, labs, imaging) for these cases, multivariate analysis is unable to fully explain surgical decision-making, particularly at higher-level trauma centers where patients may be referred for their complexity or worsening clinical status. These data also highlight the importance of laparoscopic training in general surgery residents, so that graduating general surgeons have the operative skills to perform these common procedures in a minimally invasive manner. Currently, ACGME requires a minimum of 150 laparoscopic cases and completion of the Fundamentals of Laparoscopic Surgery (FLS) training in order to graduate [32]; however, the average number of laparoscopic cases has increased substantially in the last 20 years. A recent study by Bingmer et al. demonstrated that in 5 key procedures, number of laparoscopic cases have increased from 23 to 136 a year (462% increase) from 2000 to 2018 [33]. At the same time there was an overall increase in cases but decreased percentage of open cases, signifying that graduates of general surgery residency are getting more exposure and experience with laparoscopic surgery.
After controlling for age, BMI, resuscitation diagnosis, trauma tier, emergency exploratory laparotomy (known higher risk), and comorbidities, conversion from laparoscopic to open procedure was found to be protective in this cohort undergoing common EGS procedures. It has been shown in prior studies that patients undergoing appendectomy who converted to open had a higher likelihood of complications [34]. Similarly, patients undergoing cholecystectomy who converted to open were shown to have higher 30-day morbidity and longer postoperative length of stay [35]. However, all-cause mortality findings in prior work have not demonstrated a similar trend. In patients undergoing cholecystectomy, it has been shown that 30-day mortality rates were similar among those undergoing laparoscopic versus cases converted to open [35]. This trend has been demonstrated among other common EGS procedures, such as colorectal resections, where multivariate regression analysis has shown in-hospital mortality rates for converted procedures that are similar to laparoscopic cases (0.5% vs 0.6%, respectively) [36]. This finding indicates that patients undergoing EGS procedures may benefit from attempted laparoscopic intervention, even if later converted to open.
Unfortunately, our dataset does not currently incorporate physiologic data such as vitals, laboratory values, and subsequent risk scores such as Shock Index, SOFA score, and APACHE. Therefore, the multivariate model was not able to control for the significant confounding factors that represent the physiologic derangement that is present in the high acuity and emergent conditions that constitute EGS. While these factors are not likely to affect a significant portion of less complex and comorbid disease processes such as cholecystitis and appendicitis, presentations for perforation, obstruction, and intra-abdominal sepsis are likely to present with severely compromised hemodynamics and organ dysfunction. In these scenarios, laparoscopy may not be appropriate given decreased preload and possible bradycardia associated with pneumoperitoneum [37]. In addition, the principles of damage control and early source control in sepsis may not be feasible with laparoscopy in complex and unstable patients. These factors may be the largest influencers of choosing to perform a laparoscopic surgery at the onset of surgery; however, other factors can also lead to an open first approach or lead to conversion. Specifically, higher rates of obstructive and infectious processes can lead to decreased abdominal domain and working room during laparoscopy. However, this multivariate analysis does show that of patients that could be started laparoscopic (likely in the setting of stable hemodynamics) and had to subsequently be converted, mortality risk was similar to laparoscopic surgery.
Multiple studies have contributed to the understanding of disease severity and the optimal management for the most common EGS procedures [38,39,40]. The continued push toward standardization in the management of common EGS procedures improves outcomes and limits variance. The development of guidelines based on severity can help achieve improved outcomes for all patients [41]. Multiple risk-based scoring systems have been developed to aid in decision-making regarding laparoscopic versus open approaches across various procedures, including for cholecystectomy and appendectomy [42, 43]. These initiatives have demonstrated perioperative and intraoperative findings that may help predict safest clinical practice in regard to surgical approach. However, practice decisions at academic versus community hospitals vary significantly [44]. The results found in this study indicate that utilizing a laparoscopic first approach may improve immediate and long-term mortality in patients undergoing common EGS procedures.
The limitations of this study include the use of ICD-9 billing code data, which serves only as a proxy for the diagnosis and final surgery. Because of the non-specificity of the data, some procedures may be coded for multiple types of operations (for example, right hemicolectomy and small bowel resection). Additionally, this analysis relied on AAST-defined diagnosis groupings, which group appendicitis diagnosis codes under upper GI diagnosis groups and cholecystitis diagnosis codes under HPB diagnosis groupings, which may impact data reporting. This data therefore provides a snapshot of the procedures but lacks more specific details about the operation or why it was performed. Additionally, results may vary depending on the resources of the varying facilities, causing one institution to opt to send more complicated pathologies to larger centers and for open procedures to be more common at tertiary centers. This in turn may be why we saw a lower CCI index in patients undergoing laparoscopic surgeries, as well as why most minimally invasive cases are done at non-trauma centers. Regarding generalizability, this dataset demonstrates referral and treatment patterns for a single large integrated health care system in the Southeastern United States. Given procedure guideline variation across various institutions and US regions, these results may vary geographically. Lastly, this study is limited in understanding the training across surgeons operating at various facilities (fellowship-trained Acute Care Surgeons versus general surgery and minimally invasive surgery training). In the future, we hope to utilize patient-specific clinical data (such as vitals, lab values, and clinical imaging) to better characterize the treatment patterns and outcomes for emergency general surgery cases in an integrated health system.
Conclusion
Use of laparoscopic techniques in emergency general surgery cases is common within a large integrated health care system. When adjusted for preoperative risk factors, use of laparoscopic techniques were associated with a decreased risk of all-cause mortality at all time points compared to open procedures. When controlling for age, BMI, and CCI, patients undergoing EGS procedures laparoscopically who convert to open had decreased odds of mortality compared to open procedures at all time points, providing some evidence to pursue a laparoscopic first approach in EGS cases.
References
Britt LD (2012) Acute care surgery: what’s in a name? J Trauma Acute Care Surg 72:319–320. https://doi.org/10.1097/TA.0b013e31824b15c1
Britt LD (2012) American association for the surgery of trauma and the clinical congress of acute care surgery 2011 presidential address. J Trauma Acute Care Surg 72:4–10. https://doi.org/10.1097/TA.0b013e31823fbda3
Morris JA, Fildes J, May AK, Diaz J, Britt LD, Meredith JW (2013) A research agenda for emergency general surgery: health policy and basic science. J Trauma Acute Care Surg 74:322–328. https://doi.org/10.1097/TA.0b013e31827d0fe3
Morris JA, Diaz J, Fildes J, May AK, Britt LD, Meredith JW (2013) A research agenda for emergency general surgery: clinical trials. J Trauma Acute Care Surg 74:329–333. https://doi.org/10.1097/TA.0b013e31827542cd
Shafi S, Aboutanos MB, Agarwal S, Brown CVR, Crandall M, Feliciano DV, Guillamondegui O, Haider A, Inaba K, Osler TM, Ross S, Rozycki GS, Tominaga GT (2013) Emergency general surgery: definition and estimated burden of disease. J Trauma Acute Care Surg 74:1092–1097. https://doi.org/10.1097/TA.0b013e31827e1bc7
Gale SC, Shafi S, Dombrovskiy VY, Arumugam D, Crystal JS (2014) The public health burden of emergency general surgery in the United States: a 10-year analysis of the Nationwide Inpatient Sample—2001 to 2010. J Trauma Acute Care Surg 77:202–208. https://doi.org/10.1097/TA.0000000000000362
Havens JM, Olufajo OA, Cooper ZR, Haider AH, Shah AA, Salim A (2016) Defining rates and risk factors for readmissions following emergency general surgery. JAMA Surg 151:330–336. https://doi.org/10.1001/jamasurg.2015.4056
Shah AA, Haider AH, Zogg CK, Schwartz DA, Haut ER, Zafar SN, Schneider EB, Velopulos CG, Shafi S, Zafar H, Efron DT (2015) National estimates of predictors of outcomes for emergency general surgery. J Trauma Acute Care Surg 78:482–491. https://doi.org/10.1097/TA.0000000000000555
Scott JW, Olufajo OA, Brat GA, Rose JA, Zogg CK, Haider AH, Salim A, Havens JM (2016) Use of national burden to define operative emergency general surgery. JAMA Surg 151:1–7. https://doi.org/10.1001/jamasurg.2016.0480
Ingraham AM, Cohen ME, Raval MV, Ko CY, Nathens AB (2011) Comparison of hospital performance in emergency versus elective general surgery operations at 198 hospitals. J Am Coll Surg 212:20-28.e1. https://doi.org/10.1016/j.jamcollsurg.2010.09.026
McCoy CC, Englum BR, Keenan JE, Vaslef SN, Shapiro ML, Scarborough JE (2015) Impact of specific postoperative complications on the outcomes of emergency general surgery patients. J Trauma Acute Care Surg 78:912–919. https://doi.org/10.1097/TA.0000000000000611
Ogola GO, Gale SC, Haider A, Shafi S (2015) The financial burden of emergency general surgery: national estimates 2010 to 2060. J Trauma Acute Care Surg 79:444–448. https://doi.org/10.1097/TA.0000000000000787
Hall EC, Hashmi ZG, Zafar SN, Zogg CK, Cornwell EE, Haider AH (2015) Racial/ethnic disparities in emergency general surgery: explained by hospital-level characteristics? Am J Surg 209:604–609. https://doi.org/10.1016/j.amjsurg.2014.11.005
Eckert M, Cuadrado D, Steele S, Brown T, Beekley A, Martin M (2010) The changing face of the general surgeon: national and local trends in resident operative experience. Am J Surg 199:652–656. https://doi.org/10.1016/j.amjsurg.2010.01.012
Malangoni MA, Biester TW, Jones AT, Klingensmith ME, Lewis FR (2013) Operative experience of surgery residents: trends and challenges. J Surg Educ 70:783–788. https://doi.org/10.1016/j.jsurg.2013.09.015
Charlson M, Szatrowski TP, Peterson J, Gold J (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47:1245–1251. https://doi.org/10.1016/0895-4356(94)90129-5
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 40:373–383. https://doi.org/10.1016/0021-9681(87)90171-8
Agresta F, Campanile FC, Podda M, Cillara N, Pernazza G, Giaccaglia V, Ciccoritti L, Ioia G, Mandalà S, La Barbera C, Birindelli A, Sartelli M, Di Saverio S, Anania G, Vettoretto N, Arezzo A, Campli M, Bergamini C, Carlucci M, Zago M, Mirabella A, Lupo M, Piccoli M, Ansaloni L, Cocorullo G, Baiocchi L, Allaix M, Saia M, Luridiana G (2017) Current status of laparoscopy for acute abdomen in Italy: a critical appraisal of 2012 clinical guidelines from two consecutive nationwide surveys with analysis of 271,323 cases over 5 years. Surg Endosc 31:1785–1795. https://doi.org/10.1007/s00464-016-5175-4
Johnson B, Bogert J, Dennis B, Fox N, Gunter O, Sawhney J, Schroeder L, Yeh DD, Young J (2020) Role of laparoscopy in small bowel obstruction 2018. In: East. Assoc. Surg. Trauma. https://www.east.org/education/practice-management-guidelines/details/64/role-of-laparoscopy-in-small-bowel-obstruction. Accessed 1 Oct 2020
Pansa A, Kurihara H, Memon MA (2020) Updates in laparoscopic surgery for perforated peptic ulcer disease: state of the art and future perspectives. Ann Laparosc Endosc Surg 5:5. https://doi.org/10.21037/ales.2019.11.03
Rodriguez RMJ, Segura-Sampedro JJ, Flores-Cortés M, López-Bernal F, Martín C, Diaz VP, Ciuro FP, Ruiz JP (2016) Laparoscopic approach in gastrointestinal emergencies. World J Gastroenterol 22:2701–2710. https://doi.org/10.3748/wjg.v22.i9.2701
Mandrioli M, Inaba K, Piccinini A, Biscardi A, Sartelli M, Agresta F, Catena F, Cirocchi R, Jovine E, Tugnoli G, Di Saverio S (2016) Advances in laparoscopy for acute care surgery and trauma. World J Gastroenterol 22:668–680. https://doi.org/10.3748/wjg.v22.i2.668
Richards MK, McAteer JP, Drake FT, Goldin AB, Khandelwal S, Gow KW (2015) A national review of the frequency of minimally invasive surgery among general surgery residents. JAMA Surg 150:169. https://doi.org/10.1001/jamasurg.2014.1791
McCoy AC, Gasevic E, Szlabick RE, Sahmoun AE, Sticca RP (2013) Are open abdominal procedures a thing of the past? An analysis of graduating general surgery residents’ case logs from 2000 to 2011. J Surg Educ 70:683–689. https://doi.org/10.1016/j.jsurg.2013.09.002
Brown NM, Helmer SD, Yates CL, Osland JS (2012) The revised ACGME laparoscopic operative requirements: How have they impacted resident education? Surg Endosc 26:1737–1743. https://doi.org/10.1007/s00464-011-2103-5
Zerey M, Heniford BT (2006) Laparoscopic versus open surgery for ventral hernia repair: Which is best? Commentary. Nat Clin Pract Gastroenterol Hepatol 3:372–373. https://doi.org/10.1038/ncpgasthep0548
Rosen MJ, Cobb WS, Kercher KW, Heniford BT (2006) Laparoscopic versus open colostomy reversal: A comparative analysis. J Gastrointest Surg 10:895–900. https://doi.org/10.1016/j.gassur.2005.11.008
Giordano S, Victorzon M (2014) Laparoscopic Roux-En-Y gastric bypass is effective and safe in over 55-year-old patients: a comparative analysis. World J Surg 38:1121–1126. https://doi.org/10.1007/s00268-013-2399-5
Tyson AF, Sola R, Arnold MR, Cosper GH, Schulman AM (2017) Thoracoscopic versus open congenital diaphragmatic hernia repair: single tertiary center review. J Laparoendosc Adv Surg Tech 27:1209–1216. https://doi.org/10.1089/lap.2017.0298
Sauerland S, Agresta F, Bergamaschi R, Borzellino G, Budzynski A, Champault G, Fingerhut A, Isla A, Johansson M, Lundorff P, Navez B, Saad S, Neugebauer EAM (2006) Laparoscopy for abdominal emergencies. Surg Endosc 20:14–29. https://doi.org/10.1007/s00464-005-0564-0
O’Connor DB, Winter DC (2012) The role of laparoscopy in the management of acute small-bowel obstruction: a review of over 2000 cases. Surg Endosc 26:12–17. https://doi.org/10.1007/s00464-011-1885-9
Training Requirements for General Surgery Certification. In: Am. Board Surg. https://www.absurgery.org/default.jsp?certgsqe_training
Bingmer K, Ofshteyn A, Stein SL, Marks JM, Steinhagen E (2020) Decline of open surgical experience for general surgery residents. Surg Endosc 34:967–972. https://doi.org/10.1007/s00464-019-06881-0
Finnerty BM, Wu X, Giambrone GP, Gaber-Baylis LK, Zabih R, Bhat A, Zarnegar R, Pomp A, Fleischut P, Afaneh C (2017) Conversion-to-open in laparoscopic appendectomy: A cohort analysis of risk factors and outcomes. Int J Surg 40:169–175. https://doi.org/10.1016/j.ijsu.2017.03.016
Kaafarani HMA, Smith TS, Neumayer L, Berger DH, DePalma RG, Itani KMF (2010) Trends, outcomes, and predictors of open and conversion to open cholecystectomy in Veterans Health Administration hospitals. Am J Surg 200:32–40. https://doi.org/10.1016/j.amjsurg.2009.08.020
Masoomi H, Moghadamyeghaneh Z, Mills S, Carmichael JC, Pigazzi A, Stamos MJ (2015) Risk factors for conversion of laparoscopic colorectal surgery to open surgery: does conversion worsen outcome? World J Surg 39:1240–1247. https://doi.org/10.1007/s00268-015-2958-z
Yong J, Hibbert P, Runciman WB, Coventry BJ (2015) Bradycardia as an early warning sign for cardiac arrest during routine laparoscopic surgery. Int J Qual Health Care 27:473–478. https://doi.org/10.1093/intqhc/mzv077
Hernandez M, Murphy B, Aho JM, Haddad NN, Saleem H, Zeb M, Morris DS, Jenkins DH, Zielinski M (2018) Validation of the AAST EGS acute cholecystitis grade and comparison with the Tokyo guidelines. Surgery 163:739–746. https://doi.org/10.1016/j.surg.2017.10.041
Sekimoto M, Takada T, Kawarada Y, Nimura Y, Yoshida M, Mayumi T, Miura F, Wada K, Hirota M, Yamashita Y, Strasberg S, Pitt HA, Belghiti J, de Santibanes E, Gadacz TR, Hilvano SC, Kim S-W, Liau K-H, Fan S-T, Belli G, Sachakul V (2007) Need for criteria for the diagnosis and severity assessment of acute cholangitis and cholecystitis: Tokyo guidelines. J Hepatobiliary Pancreat Surg 14:11–14. https://doi.org/10.1007/s00534-006-1151-z
Takada T, Strasberg SM, Solomkin JS, Pitt HA, Gomi H, Yoshida M, Mayumi T, Miura F, Gouma DJ, Garden OJ, Büchler MW, Kiriyama S, Yokoe M, Kimura Y, Tsuyuguchi T, Itoi T, Gabata T, Higuchi R, Okamoto K, Hata J, Murata A, Kusachi S, Windsor JA, Supe AN, Lee SG, Chen X-P, Yamashita Y, Hirata K, Inui K, Sumiyama Y (2013) TG13: Updated Tokyo guidelines for the management of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci 20:1–7. https://doi.org/10.1007/s00534-012-0566-y
Hussain A (2011) Difficult laparoscopic cholecystectomy: current evidence and strategies of management. Surg Laparosc Endosc Percutaneous Tech 21:211–217. https://doi.org/10.1097/SLE.0b013e318220f1b1
Sugrue M, Coccolini F, Bucholc M, Johnston A, Manatakis D, Ioannidis O, Bonilauri S, Gachabayov M, Isik A, Ghnnam W, Shelat V, Aremu M, Mohan R, Montori G, Walȩdziak M, Pisarska M, Kong V, Strzałka M, Fugazzola P, Nita GE, Nardi M, Major P, Negoi I, Allegri A, Konstantoudakis G, Di Carlo I, Massalou D, D’Amico G, Solaini L, Ceresoli M, Bini R, Zielinski M, Tomasoni M, Litvin A, De Simone B, Lostoridis E, Hernandez F, Panyor G, Machain GMV, Pentara I, Baiocchi L, Ng KC, Ansaloni L, Sartelli M, Arellano ML, Savala N, Couse N, McBride S (2019) Intra-operative gallbladder scoring predicts conversion of laparoscopic to open cholecystectomy: a WSES prospective collaborative study. World J Emerg Surg 14:10–17. https://doi.org/10.1186/s13017-019-0230-9
Di Saverio S, Birindelli A, Kelly MD, Catena F, Weber DG, Sartelli M, Sugrue M, De Moya M, Gomes CA, Bhangu A, Agresta F, Moore EE, Soreide K, Griffiths E, De Castro S, Kashuk J, Kluger Y, Leppaniemi A, Ansaloni L, Andersson M, Coccolini F, Coimbra R, Gurusamy KS, Campanile FC, Biffl W, Chiara O, Moore F, Peitzman AB, Fraga GP, Costa D, Maier RV, Rizoli S, Balogh ZJ, Bendinelli C, Cirocchi R, Tonini V, Piccinini A, Tugnoli G, Jovine E, Persiani R, Biondi A, Scalea T, Stahel P, Ivatury R, Velmahos G, Andersson R (2016) WSES Jerusalem guidelines for diagnosis and treatment of acute appendicitis. World J Emerg Surg 11:1–25. https://doi.org/10.1186/s13017-016-0090-5
Birkmeyer JD, Reames BN, McCulloch P, Carr AJ, Campbell WB, Wennberg JE (2013) Understanding of regional variation in the use of surgery. Lancet 382:1121–1129. https://doi.org/10.1016/S0140-6736(13)61215-5
Acknowledgements
Jill Jurgensen for medical editing and proofing.
Funding
This research received no specific grant from a funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Sean J. Donohue, Caroline E. Reinke, Susan L. Evans, Mary M. Jordan, Yancey E. Warren, Timothy Hetherington, Marc Kowalkowski, Addison K. May, Brent D. Matthews, and Samuel W. Ross have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Donohue, S.J., Reinke, C.E., Evans, S.L. et al. Laparoscopy is associated with decreased all-cause mortality in patients undergoing emergency general surgery procedures in a regional health system. Surg Endosc 36, 3822–3832 (2022). https://doi.org/10.1007/s00464-021-08699-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08699-1