Abstract
Background
The obesity rate is projected to reach 50% by 2030. Obesity may be modifiable prior to elective colorectal surgery, but there is no opportunity for weight loss when patients present for urgent/emergency operations. The impact of obesity focused on urgent/emergent colorectal operations has not been fully characterized. The study aim was to determine outcomes of obese patients who undergo urgent/emergency colorectal surgery and differences when compared with elective outcomes.
Methods
This is a retrospective cohort study of 30-day outcomes for normal (BMI 18.5–25), obese (BMI 30–39.9), and morbidly obese (BMI > 40) patients in the Michigan Surgical Quality Collaborative between 1/1/2009 and 12/31/2018. Propensity score weighting was used to derive adjusted rates for overall morbidity, mortality, and specific complications. Primary outcome was postoperative complications (any morbidity).
Results
The study included 5268 urgent/emergency and 10,414 elective colorectal surgery patients. Postoperative complications were significantly more common in morbidly obese and obese than the normal BMI group for both urgent/emergency (morbidly obese 42.76% vs 33.75%, p = 0.003; obese 36.46% vs 33.75%, p = 0.043) and elective (morbidly obese 18.17% vs 13.36%, p = 0.004; obese 15.45% vs 13.36%, p = 0.011) operations. Surgical site infections are were significantly more common in morbidly obese and obese BMI groups as compared to normal BMI for both urgent/emergency and elective cases. Mortality was significantly higher in the morbidly obese (14.93% vs 11.44%, p = 0.013) but not obese BMI groups as compared to the normal BMI group for urgent/emergency cases. Mortality for all groups undergoing elective operations was < 1% and with no significant differences.
Conclusions
Morbid obesity and obesity are associated with complications that are largely driven by surgical site infections after both urgent/emergency and elective colorectal surgery. Obesity is a risk factor difficult to modify prior to urgent/emergency surgery. Managing complications related to obesity after colorectal surgery will be a continued challenge with projected increasing obesity rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The rate of obesity (BMI ≥ 30) in American adults increased from 30 in 1999 to 43% in 2015, and is projected to reach 50% by 2030 [1,2,3]. For elective surgery, obesity is associated with longer operative times and higher risk of 30-day complications, especially surgical site infections, cardiac events, and thromboembolic events [4,5,6,7]. However, previous research has suggested an “obesity paradox”, described as obese patients having a lower mortality rate after nonbariatric operations and after surgery for intensive care unit patients with peritonitis and sepsis [6, 8].
Although the impact of obesity in elective colorectal procedures has been well described, patients requiring urgent/emergency colorectal resection are a particularly high-risk cohort that have not been thoroughly studied. A large, nationwide study of urgent/emergency versus elective general surgery procedures revealed that 30-day morbidity (22.8% vs 14.2%) and mortality (6.5% vs 1.4%) were significantly higher for urgent/emergency than for elective cases [9]. Others have confirmed this finding [10]. However, it is unclear if obese patients undergoing urgent/emergency colorectal resection are at higher or lower risk for morbidity and if they have the same lower mortality “obesity paradox” seen with nonbariatric and intensive care unit operations.
The goal of this study was to evaluate the association of morbid obesity and obesity compared to normal BMI on morbidity and mortality for patients who undergo urgent/emergency colorectal surgery. To provide context to the findings, we also present contemporaneous outcomes for morbidly obese, obese, and nonobese elective surgery patients. Our hypothesis was that morbidity and mortality would be even more apparent comparing morbid obesity and obesity with normal BMI patients for urgent/emergency than for elective colorectal resections.
Methods
Data source and study population
This study was approved by the Institutional Review Boards at St Joseph Mercy Hospital Ann Arbor and the University of Michigan and funded by the St Joseph Mercy Hospital Academic Research Committee. This is a retrospective study of data collected prospectively in the Michigan Surgical Quality Collaborative (MSQC), a statewide collaborative for quality improvement with a validated, prospective clinical registry. This registry is available for quality improvement and research and is financially supported by Blue Cross Blue Shield of Michigan. Funding is provided for manual data abstraction and database entry by clinical nurse reviewers. MSQC hospitals represent 90% of eligible Michigan hospitals that include small community hospitals and large academic centers in urban and rural locations [11].
Patients in this study were ≥ 18 years of age undergoing urgent, emergency, and elective colorectal surgery for colorectal neoplasia, diverticulitis, inflammatory bowel disease, and other diseases of the colon and rectum between 01–01–2009 and 12–31–2018. Cases with the Current Procedural Code (CPT) 44140, 44141, 44143, 44145, 44146, 44150, 44155, 44160 were designated open procedures while 44204, 44205, 44207, 44208, 44210, 44212 were minimally invasive. Colon cases were defined using CPT codes 44140, 44141, 44,143, 44150, 44160, 44204, 44205, 44210, and rectal cases were 44145, 44146, 44155, 44207, 44208, and 44212.
The MSQC urgent variable is defined as nonlife threatening acute medical condition for which the patient needs intervention during admission and cannot be discharged home prior to the intervention. Emergency surgery is performed within 12 h of the decision to operate and at least one of the following criteria: patient health, life, or limb in serious jeopardy, serious impairment to bodily functions, or serious dysfunction of any bodily organ or part. Elective surgery is scheduled in advance with an outpatient interval between the decision to operate and the actual operation.
Outcome and predictor variables
Patient characteristics listed in Tables 1 and 2 and included for risk adjustment were patient age, gender, race, American Society of Anesthesiologists (ASA) classification, comorbidities (hypertension, diabetes, coronary artery disease, congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD), sleep apnea, alcohol use (ETOH), smoking status, disseminated cancer, preoperative sepsis, steroid/immunosuppressive medication use), functional status (independent, partially dependent), laboratory values (white blood cell count, blood glucose, albumin, lactate), surgical priority (urgent, emergency), and surgical approach (minimally invasive, open), weight loss, operative diagnosis (colorectal cancer, diverticulitis, gastrointestinal hemorrhage, IBD, ischemia, volvulus, other), colon vs rectal resection, procedure side (left colectomy, rectal resection, right colectomy, total abdominal colectomy), and presence of ostomy.
The primary outcome was “Any Morbidity” (30-day complication rate). Secondary outcomes were death (30-day mortality), superficial, deep, and organ space surgical site infections (SSI), sepsis, anastomotic leak, ileus, myocardial infarction (MI), cardiac arrest, pneumonia, unplanned intubation, acute renal failure, deep venous thrombosis (DVT), pulmonary embolus (PE), stroke, symptomatic urinary tract infection (UTI), catheter-associated UTI, readmission, reoperation, and discharge destination not home. “Any SSI” was the sum total of superficial, deep, and organ space SSIs, and “Any VTE” was the combination of DVT and PE.
Statistical analysis
Analyses are presented comparing the outcomes of patients based on their BMI. Three treatment groups were defined as normal (BMI 18.5–25), obese (BMI 30–39.9), and morbidly obese (BMI 40+). All analyses were performed separately for urgent/emergency procedures and elective procedures. Some lab values had high rates of missingness; thus, single imputation using predictive mean matching was used.
Descriptive statistics were provided for all study variables. Presented are means and standard deviations for continuous variables, and frequencies and proportions for categorical variables.
To adjust for imbalances in the observational groups, propensity score weighting was used to make the treatment groups more comparable. All demographics and preprocedure comorbidities were included in the propensity score model. The weighted groups were then tested for balance using weighted versions of the t test and χ2 test.
Urgent and Emergency operations were combined in one group and compared with elective operations. Urgent and Emergency operations were included separately in the statistical model to control for any differences between these groups.
Outcomes were then compared between the normal, obese, and morbidly obese groups. In urgent/emergency procedures, sex, diabetes, sleep apnea, ETOH, and smoker status were still significantly different after weighting, thus p values were calculated using weighted regressions with these variables as additional controls. For elective cases, sex, age, ASA class, diabetes, sleep apnea, smoker status, disseminated cancer, and steroid/immunosuppressive medication use were included as controls. P values < 0.05 were considered statistically significant.
Results
Characteristics of the cohort
The study population included 5268 urgent/emergency colorectal surgery cases—2500 patients with normal BMI (18.5–25), 2203 obese BMI (30–40), and 565 were morbidly obese BMI (40+). There were 10,414 elective colorectal surgery cases—4073 patients with normal BMI, 5306 obese, and 1035 who were morbidly obese.
Table 1 presents patient characteristics and predictors for urgent/emergency and elective cases prior to propensity score weighting. Almost half of the urgent/emergency group cases were urgent. Almost 20% of the urgent/emergency group and 63–70% of the elective cases were done by a minimally invasive approach. There were many significant differences between BMI groups in both surgical time frames.
Table 2 reveals the balance of patient characteristics and predictors for urgent/emergency and elective cases after propensity score weighting. Obese and morbidly obese patients were more likely to be female and have diabetes and sleep apnea, and less likely to be smokers and ETOH users for both urgent/emergency and elective operations. Normal BMI patients were more likely to be older, and on steroids/immunosuppressive medications, and have weight loss for urgent/emergency and elective operations.
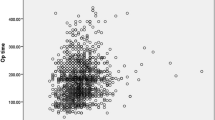
Propensity score weighted morbidity and mortality (Fig. 1)
Figure 1 shows propensity score weighted morbidity and mortality for urgent/emergency and elective cases. Postoperative complications are significantly more common in the morbidly obese than the normal BMI group for both urgent/emergency (42.76% vs 33.75%, p = 0.003) and elective (18.17% vs 13.36%, p = 0.004) operations. Postoperative complications are also significantly more common in the obese than the normal BMI group for both urgent/emergency (36.46% vs 33.75%, p = 0.043) and elective (15.45% vs 13.36%, p = 0.011) operations. Deaths are significantly more common in the morbidly obese than the normal BMI group (14.93% vs 11.44%, p = 0.013) for urgent/emergency operations. There was no significant difference between obese and normal BMI groups for urgent/emergency operations (9.5% vs 11.44%, p = 0.482). Mortality for all groups with elective operations was < 1% and there were no significant differences between groups (normal BMI 0.96% vs obese BMI 0.76%, p = 0.937; normal BMI 0.96% vs morbidly obese BMI 0.70%, p = 0.732).
Propensity score weighted individual complications (Table 3)
Any SSI was significantly higher for morbidly obese and obese compared to normal BMI groups for both urgent/emergency and elective operations. Superficial SSI was also significant higher for morbidly obese and obese compared to normal BMI groups for both urgent/emergency and elective operations. Deep SSI was significantly higher for obese groups compared to the normal BMI group for urgent/emergency operations, and for morbidly obese compared to the normal BMI group for elective operations. Anastomotic leaks were significantly higher for obese but not morbidly obese BMI groups compared to the normal BMI group for urgent/emergency operations. There were no significant differences between groups for sepsis, ileus, MI, cardiac arrest, pneumonia, unplanned intubation, and catheter-associated UTIs.
Acute renal failure was significantly more common in the morbidly obese group compared to the normal BMI group for urgent/emergency operations. Acute renal failure and DVT were significantly more common in morbidly obese and obese groups compared to the normal BMI group for elective operations. The total VTE events were significantly more common in the morbidly obese and obese BMI groups than the normal BMI group for elective, but not urgent/emergency operations. Stroke was significantly more common in the normal compared to morbidly obese groups for elective but not urgent/emergency operations. Symptomatic UTI was significantly higher for the normal group compared to the obese BMI group for urgent/emergency operations. Reoperation and readmission were significantly more common in the obese group as compared to the normal BMI group for urgent/emergency operations. Discharge destination not home was significantly more common for morbidly obese patients as compared to normal BMI patients for elective but not urgent/emergency operations.
Discussion
The results of this study show that morbid obesity (BMI > 40) and obesity (BMI 30–39.9) are associated with complications after urgent-emergency colorectal resection, with significantly higher risk-adjusted rates of SSIs. Some complications (anastomotic leak, reoperations, readmissions) are significantly higher in the obese but not the morbidly obese group compared to normal BMI after urgent/emergency operations. Overall, the significant differences in total complications (Any Morbidity) and SSIs are similar for urgent/emergency and elective operations. There are differences in individual complication patterns. For example, though venous thromboembolic events are more common after urgent/emergency than after elective operations, these complications are not significantly different between BMI groups for the urgent/emergency cases as they are for the elective cases. Reoperations and readmission are significantly more common in obese vs normal BMI for urgent/emergency operation but not for elective operations. Mortality is higher for urgent/emergency operations than for elective operations and significantly higher for morbidly obese compared to the normal BMI group for urgent/emergency operations. Mortality was low for all elective BMI groups and without significant difference between groups.
An ACS-NSQIP study of elective colorectal surgery cases showed an “obesity paradox” with significantly higher odds for mortality for the normal BMI group when compared to overweight (BMI 25.0–29.9) and mildly obese (BMI 30.0–34.9) groups [12]. In contrast to this ACS-NSQIP study, the “obesity paradox” was not apparent for urgent/emergency or for elective cases in our study. Though mortality was lower in the obese than in the normal BMI group, the difference was not significantly different (11.44% vs 9.5%, p = 0.482). Our analysis showed no difference in mortality between BMI groups for elective cases, all with strikingly low rates of mortality < 1%.
Our study showed that postoperative complications after urgent/emergency colorectal operations are twice what they are after elective operations for all BMI groups. Surgical site infections are major drivers of morbidity after colorectal surgery [7, 12]. Our study revealed significantly higher SSI rates for morbidly obese and obese patients when compared to the normal BMI group for both urgent/emergency and elective colorectal operations. Type I (superficial) SSIs were significantly higher for morbidly obese and obese BMI groups compared to the normal BMI group for both urgent/emergency and elective cases. Type II (deep) SSIs were significantly higher for obese BMI groups for urgent/emergency cases, and for the morbidly obese group for elective cases compared to the normal BMI group. There were no significant differences in type III SSIs (organ space) between BMI groups for both urgent/emergency and elective group cases.
Although high BMI has been shown to increase complications after elective colorectal surgery, our study adds to current literature as there is a paucity of studies focused on colorectal urgent/emergency operations for outcomes comparison. Other colorectal surgery studies of elective cases confirm our finding of significantly higher SSIs for higher BMIs compared to normal BMI [12]. In contrast, a systematic review showed no difference in SSIs between obese and nonobese patients undergoing elective laparoscopic colorectal resections [13]. However, BMI > 25 kg/m2 was considered obese in that study. Adherence to processes that decrease SSIs may be effectively adopted in the elective setting [11]. Mechanical bowel preparation with oral antibiotics is not practical or indicated for most urgent/emergency cases. For urgent/emergency cases, strict attention to properly administered intravenous antibiotics, normothermia, euglycemia, and MIS when possible may potentially decrease SSIs [14].
Sepsis was higher for urgent/emergency than for elective operations in our study, but there were no significant differences between BMI groups. Anastomotic leaks and reoperations were significantly higher for the obese group than the normal BMI group for urgent/emergency but not elective operations. Because the anastomotic leak rate was low for each BMI group, unmeasured differences in illness severity or other characteristics between cohorts in the urgent/emergency operations could influence these results. Obesity should likely be considered among other risk factors when deciding whether to perform an anastomosis in the urgent-emergency setting.
Other studies examining the association of obesity and postoperative complications for urgent/emergent colorectal operations are inconsistent in their conclusions and difficult to compare with our study because of differences in obesity definitions [15, 16]. A study comparing 397 morbidly obese (median BMI 39.3) and 397 nonmorbidly obese (median BMI 27.4) patients undergoing emergency Hartmann’s procedure for perforated diverticulitis showed no significant difference in postoperative complications, including SSIs [15]. This study examined only one emergency diagnosis and the definition of morbid obesity was BMI ≥ 35 kg/m2, thereby making it difficult to compare to the obese (BMI 30–39) and morbidly obese (BMI ≥ 40) groups in our study. Another study comparing outcomes for emergency surgery for obstructing colon cancer also found no difference in 30-day complications between normal (BMI < 25), overweight (BMI 25–29.9), and obese (BMI ≥ 30) groups, except for stoma-related complications in patients with left-sided obstruction. There was no morbidly obese group in this study [16]. We chose not to include the overweight BMI group because of the paucity of literature showing worse outcomes for this group. We also hypothesized and have shown that there are differences between obese and morbidly obese groups when compared to normal BMI when morbid obesity was defined as ≥ 40 kg/m2.
Other studies evaluating the impact of obesity on elective colorectal operations also show mixed results [7, 12, 17, 18]. A study that also defined morbid obesity as BMI ≥ 40, showed that an obese BMI class is an independent risk factor for adverse elective postoperative outcomes and that SSIs progressively increased with increasing BMI class [12]. In contrast to our study, sepsis also increased with increasing BMI, while our study showed no difference in sepsis between groups for elective operations. Similar to our study, patients with higher BMI had significantly more diabetes. In contrast to our study, the minimally invasive approach was used less often (48% vs 62–70%). Another large population-based study of patients undergoing elective operations for colon and rectal cancer identified obesity as a risk factor for postoperative complications for all obesity groups and an underweight group as compared to those with normal BMI [18].
There are limitations inherent to any database study that relies on accurate data reporting and submission. Although the MSQC database is comprehensive in the number of predictors and the unique nature of some predictors available for analysis, there may be other data not captured by this database that impacts outcomes. MSQC includes 90% of eligible small community hospitals and large academic centers in Michigan and the results may be generalizable to other institutions. Our study focused on the impact of obesity compared to normal BMI patients and did not include underweight (BMI < 18.5) patients that have been shown in other studies to be at high risk for complications [12]. Although many studies apply BMI to categorize obesity, others have suggested that CT-defined visceral obesity and sarcopenia may better characterize obesity risk [19, 20]. These data are not available in the MSQC registry. We chose to combine urgent and emergency groups and separated them in the statistical model. The MSQC data source does not account for selection bias with respect to which patients are chosen for minimally invasive and open options. These variables were included in the statistical model.
This study lends perspective to the impact of obesity by including both urgent/emergency and elective cohorts. Urgent/emergency cases may not allow modification of obesity as a risk factor. Because morbidity and mortality are related to the severity of the illness, acute surgical care interventions that potentially decrease perioperative risk and the use of minimally invasive surgery when possible may be the optimum strategy for urgent/emergent operations at this time. Elective cases may allow weight reduction options to improve operative outcomes related to obesity, though colorectal cancer cases are a weight loss dilemma. Global educational efforts to reduce the rising incidence of obesity may be the most effective risk-reduction strategy.
Conclusion
Morbid obesity and obesity are associated with significantly higher overall morbidity and significantly more superficial surgical site infections after urgent/emergency and elective colorectal surgery. Obesity is a risk factor difficult to modify prior to urgent/emergency surgery. Managing morbidity after urgent/emergent colorectal surgery will require further study with projected increasing obesity rates.
References
Hales CM, Carroll MD, Fryar CD, Ogden CL (2017) Prevalence of obesity among adults and youth: United States, 2015–2016. National Center for Health Statistics, Data Brief 288, 2017. https://www.cdc.gov/nchs/products/databriefs/db288.htm.
Weiss AJ, Elixhauser A. Obesity-Related Hospitalizations, 2004 versus 2009. HCUP Healthcare Cost and Utilization Project Statistical Brief #137. July 2012. Agency for Healthcare Research and Quality. Rockville, MD. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb137.pdf
Després JP, Lemieux I (2006) Abdominal obesity and metabolic syndrome. Nature 444:881–887
Bamgbade OA, Rutter TW, Nafiu OO, Dorje P (2007) Postoperative complications in obese and nonobese patients. World J Surg 31:556–560
Doyle SL, Lysaght J, Reynolds JV (2010) Obesity and post-operative complications in patients undergoing non-bariatric surgery. Obes Rev 11:875–886
Mullen JT, Moorman DW, Davenport DL (2009) The obesity paradox: body mass index and outcomes in patients undergoing nonbariatric general surgery. Ann Surg 250:166–172
Gendall KA, Raniga S, Kennedy R, Frizelle FA (2007) The impact of obesity on outcome after major colorectal surgery. Dis Colon Rectum 50:2223–2237
Utzolino S, Ditzel CM, Baier PK, Hopt UT, Kaffarnik MF (2014) The obesity paradox in surgical intensive care patients with peritonitis. J Crit Care 29:887.e1-887.e5
Becher RD, Hoth JJ, Miller PR, Mowery NT, Chang MC, Meredith JW (2011) A critical assessment of outcomes in emergency versus nonemergency general surgery using the American College of Surgeons National Surgical Quality Improvement Program database. Am Surg 77:951–959
Ingraham AM, Cohen ME, Bilimoria KY, Feinglass JM, Richards KE, Hall BL, Ko CY (2010) Comparison of hospital performance in nonemergency versus emergency colorectal operations at 142 hospitals. JACS 210:155–165
Vu JV, Collins SD, Seese E, Hendren S, Englesbe MJ, Campbell DA, Krapohl GL (2018) Evidence that a regional surgical collaborative can transform care: surgical site infection prevention practices for colectomy in Michigan. J Am Coll Surg 226:91–99
Wahl TS, Patel FC, Goss LE, Chu DI, Grams J, Morris MS (2018) The obese colorectal surgery patient: surgical site infection and outcomes. Dis Colon Rectum 61:938–945
Hotouras A, Zakeri SA, Nunes QM, Murphy J, Bhan C, Wexner SD (2016) The influence of obesity and body mass index on the outcome of laparoscopic colorectal surgery: a systematic literature review. Colorectal Dis 18:337–366
Lee YF, Brown RF, Battaglia MA, Cleary RK (2020) Laparoscopic versus open emergent sigmoid resection for perforated diverticulitis. J Gastrointest Surg 24(5):1173–1182
Weber KT, Chung PJ, La Gamma N, Procaccino JA, Alfonso AE, Coppa G, Sugiyama G (2020) Effect of body mass index on outcomes after surgery for perforated diverticulitis. J Surg Res 247:220–226
Genser L, Manceau G, Mege D, Bridoux V, Lakkis Z, Venara A, Voron T, Bege T, Sielezneff I, Karoui M, on behalf of the AFC (French Surgical Association) Working Group (2020) 30-day postoperative morbidity of emergency surgery for obstructive right- and left-sided colon cancer in obese patients: a multicenter cohort study of the French Surgical Association. Dig Surg 37:111–118
Baird DLH, Simillis C, Pellino G, Kontovounisios C, Rasheed S, Tekkis PP (2019) The obesity paradox in beyind total mesorectal excision surgery for locally advanced and recurrent rectal cancer. Updates Surg 71:313–321
Poelemeijer YQM, Lijftogt N, Detering R, Fiocco M, Tollenaar RAEM, Wouters MWJM (2018) Obesity as a determinant of perioperative and postoperative outcomes in patients following colorectal cancer surgery: a population-based study (2009–2016). Eur J Surg Oncol 44:1849–1857
Martin L, Hopkins J, Malietzis G, Jenkins JT, Sawyer MB, Brisebois R, MacLean A, Nelson G, Gramlich L, Baracos VE (2018) Assessment of computed tomography (CT)-defined muscle and adipose tissue features in relation to short-term outcomes after elective surgery for colorectal cancer: a multicenter approach. Ann Surg Oncol 25:2669–2680
Jochum SB, Kistner M, Wood EH, Hoscheit M, Nowak L, Poirier J, Eberhardt JM, Saclarides TJ, Hayden DM (2019) Is sarcopenia a better predictor of complications than body mass index? Sarcopenia and surgical outcomes in patients with rectal cancer. Colorectal Dis 21:1372–1378
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
DC MD: Substantial contributions to the design of the work and analysis and interpretation of data for the work; Drafting the work or revising it critically for important intellectual content; Final approval of the version to be published; Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. SH MD MPH: Substantial contributions to the conception and design of the work; and analysis and interpretation of data for the work; Drafting the work or revising it critically for important intellectual content; Final approval of the version to be published; Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. MIC MD: Substantial contributions to the design of the work and analysis and interpretation of data for the work; Drafting the work or revising it critically for important intellectual content; Final approval of the version to be published; Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. AA M.B.Ch.B: Substantial contributions to the acquisition, and interpretation of data for the work; Drafting the work or revising it critically for important intellectual content; Final approval of the version to be published; Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. MAB MS: Substantial contributions to the conception or design of the work and the acquisition, analysis, and interpretation of data for the work; Drafting the work or revising it critically for important intellectual content; Final approval of the version to be published; Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. RKC MD: Substantial contributions to the conception and design of the work; and analysis and interpretation of data for the work; Drafting the work or revising it critically for important intellectual content; Final approval of the version to be published; Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Disclosures
Dr Cleary has received honoraria from Intuitive Surgical, Inc. for educational speaking. Drs. Choi, Hendren, and Chang, Mr. Abunayla, and Mr. Battaglia have no conflicts of interest of financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Choi, D., Hendren, S., Chang, M.I. et al. The impact of obesity and morbid obesity on urgent/emergency colorectal resections: a regional database analysis. Surg Endosc 36, 1876–1886 (2022). https://doi.org/10.1007/s00464-021-08467-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08467-1