Abstract
Background
Although upper gastrointestinal (GI) neoplasms are not rare in patients with familial adenomatous polyposis (FAP), few studies have focused on them and the long-term outcomes of their treatment by endoscopy. Therefore, we aimed to investigate the prevalence and endoscopic treatment outcomes of upper GI neoplasms in patients with FAP.
Methods
Among 215 patients diagnosed with FAP between January 1991 and December 2019, 208 who underwent esophagogastroduodenoscopy were eligible. The clinical features and endoscopic treatment outcomes of upper GI neoplasms were retrospectively investigated and analyzed.
Results
Among the enrolled patients, 113 (54.3%) had one or more upper GI neoplasms: gastric adenoma (n = 34), gastric cancer (n = 7), nonampullary duodenal adenoma (n = 86), and ampullary adenoma (n = 53). Among patients with gastric neoplasms (n = 37), 24 (64.9%) underwent treatment (endoscopic treatment: 22, surgery: 2). No tumor-related mortality occurred during median follow-up of 106 months (interquartile range [IQR] 63–174). Endoscopic treatment was performed in 47 (54.7%) of 86 patients with nonampullary duodenal adenoma and in 32 (60.4%) of 53 patients with ampullary adenoma. No patient underwent surgery for duodenal neoplasms, and no tumor-related mortality occurred during median follow-up of 88 months (IQR 42–145). The proportion of patients with increased Spigelman stage at 2 years after the initial diagnosis or treatment was significantly higher in untreated group than in the group treated for duodenal neoplasms (27.3% vs. 0.0%, p = 0.001).
Conclusion
Endoscopic surveillance in FAP patients is important for the detection and treatment of upper GI neoplasms in early stage. In particular, endoscopic therapy for duodenal neoplasms can reduce the severity of duodenal polyposis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Familial adenomatous polyposis (FAP) is a rare autosomal dominant hereditary syndrome caused by mutations in the adenomatous polyposis coli (APC) gene. Patients with FAP typically present with numerous colorectal adenomas, and their lifetime risk of colorectal cancer (CRC) can reach 100% without prophylactic total proctocolectomy [1]. In addition to colorectal adenoma and CRC, the risk of neoplasms of the upper gastrointestinal (GI) tract, including the stomach and duodenum, increases in FAP patients. The duodenum is the second most commonly involved organ in FAP [2], and duodenal cancer is the most common cause of death in FAP patients undergoing total colectomy [3]. Therefore, clinical guidelines recommend regular surveillance esophagogastroduodenoscopy (EGD), the intervals of which should be determined according to the degree of duodenal polyposis in FAP patients [4, 5]. Gastric lesions are also common in FAP patients and consist mainly of fundic gland polyps (FGPs), followed by gastric adenoma [6]. FAP-associated FGPs were generally considered as nonneoplastic lesions not requiring further treatment. However, several studies reported that gastric cancer can, although rarely, arise from FGPs in FAP patients [7, 8]. Thereby, the role of surveillance EGD should not be overlooked in FAP patients.
The prevalence of upper GI neoplasms differs between Asian and Western countries [9, 10]; however, few studies have focused on upper GI neoplasms in FAP, especially in Asian patients. Furthermore, although the endoscopic technique has evolved and endoscopy can now be performed to treat upper GI neoplasms, little evidence exists regarding endoscopic treatment for upper GI neoplasms in patients with FAP [11, 12]. Therefore, we aimed to investigate the long-term clinical outcomes of endoscopic treatment of gastric and duodenal neoplasms in these patients. Additionally, we aimed to analyze the distribution of upper GI neoplasms according to the presence of APC mutations.
Materials and methods
Patients
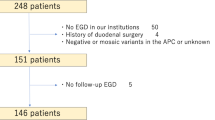
A total of 215 patients who were clinically diagnosed with FAP and visited Asan Medical Center, a tertiary university hospital in Seoul, Korea, between January 1991 and December 2019, were considered eligible. Patients with ≥ 100 colorectal adenomatous polyps or those with < 100 polyps but with APC mutations were clinically diagnosed with FAP [5]. We excluded seven patients who did not undergo EGD. Finally, 208 patients were enrolled in this study (Fig. 1). The clinical characteristics, APC mutation analysis, and endoscopic and histopathologic results were retrospectively reviewed using medical records. Informed consent was obtained from all patients before the procedure. The institutional review board of Asan Medical Center approved this study (approval no. 2020-0073).
Definitions
The histopathologic results, including information on FGPs, gastric adenoma, gastric cancer, nonampullary duodenal adenoma, and ampullary adenoma, were retrospectively reviewed. The severity of duodenal adenomatosis was classified according to the Spigelman classification [13]. At Asan Medical Center, the grade of dysplasia was described only as low or high. Therefore, we defined “low grade” as mild dysplasia (Spigelman score 1) and “high grade” as severe dysplasia (Spigelman score 3). The Spigelman classification at the EGD at the time of diagnosis or treatment of duodenal neoplasms and that at the follow-up EGD after two years were investigated to analyze the change of staging according to endoscopic treatment during the follow-up. The follow-up period was defined as the interval from the initial diagnosis of FAP to the last outpatient clinic visit.
The types of recurrence included local, synchronous, and metachronous recurrence. Local recurrence was defined as the recurrence of a neoplasm at the site of the previous endoscopic treatment. Synchronous recurrence referred to tumors being detected at a different site within 1 year of the initial endoscopic treatment, and metachronous recurrence was defined as finding a lesion more than 1 year later.
Patients who underwent a genetic test were classified into two groups according to the presence of APC mutations: group A (multiple colorectal polyps and APC mutations) and group B (≥ 100 colorectal polyps and no APC mutations). The clinical characteristics and prevalence of upper GI neoplasms in groups A and B were compared. The distribution of upper GI neoplasms according to the nucleotide change of the APC gene was also investigated.
Endoscopic treatment modalities
Patients with FGPs were usually followed up without endoscopic treatment. Forceps biopsy specimens for histology were taken from polyps > 10 mm or those showing a change in mucosal color, granularity or friability, or a microvascular pattern different from that of the surrounding polyps. If the histopathology revealed dysplasia, endoscopic treatment was performed. Patients with gastric adenoma underwent endoscopic treatment including endoscopic submucosal dissection (ESD), endoscopic mucosal resection (EMR), or argon plasma coagulation. Gastric cancer was treated with ESD or gastrectomy. In cases of nonampullary duodenal adenomas, if the lesion reached > 10 mm in size, or if the histopathology report confirmed high-grade dysplasia during the follow-up, endoscopic treatment was performed. Endoscopic papillectomy was first considered for patients with ampullary adenoma. If the lesion showed a nonlifting sign, argon plasma coagulation was considered instead of endoscopic papillectomy. After the procedure, the patients were observed in the outpatient clinic and endoscopic examination was conducted approximately every 6 months or 1 year to monitor the recurrence of upper GI neoplasm during the follow-up.
APC mutation analysis
At Asan Medical Center, mutation analysis of the APC gene on chromosome 5q21–q22 was conducted via Sanger sequencing or next-generation sequencing (NGS). Genomic DNA was extracted from EDTA-treated peripheral blood leukocytes. For Sanger sequencing, in-house primers designed to span the entire coding region and intron–exon boundaries of the APC gene (NM_000038.5) were used. Sanger sequencing was performed as previously described [14]. Sequence analysis was performed using Sequencher (Gene Codes, Ann Arbor, MI, USA) DNA analysis software, and the sequence was compared to the standard reference sequence obtained from the National Center for Biotechnology Information database [15]. For NGS, DxSeq Library Preparation Reagent and DxSeq Target Capture Reagent (Dxome, Seoul, Korea) were used for preparation, and sequencing was performed using Illumina Miseq DX (Illumina, San Diego, CA, USA). The bioinformatics software employed were Illumina VariantStudio (Illumina, San Diego, CA, USA) and DxSeq Gene Analysis System (Dxome, Seoul, Korea). When copy-number variants of APC were detected by NGS, they were confirmed using the Multiplex Ligation-dependent Probe Amplification kit (SALSA MLPA kit P043 APCl; MRC-Holland, Amsterdam, Netherlands).
Statistical analysis
Descriptive variables are summarized as median (interquartile range [IQR]). Differences in patient characteristics between two groups were appropriately compared using independent t-tests and chi-square test. The risk factors for the development of upper GI neoplasms were analyzed using logistic regression analysis. The Spigelman stage change during the follow-up was analyzed using Wilcoxon signed-rank test. A value of p < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS version 24 (IBM Corporation, Somers, NY, USA).
Results
Clinical characteristics
Among 208 patients with FAP and who underwent EGD, 113 (54.3%) had one or more upper GI neoplasms, including gastric adenoma, gastric cancer, nonampullary duodenal adenoma, and ampullary adenoma. The clinical characteristics of the study population and the comparison of patients with or without upper GI neoplasms are presented in Table 1. The median age at the initial diagnosis of FAP was 29 years (IQR 23–37 years), and 58.2% of the patients were men. The median follow-up period of these patients was 78 months (IQR 26–121 months). CLO tests were performed for 24 (11.5%) of the patients, and 10 (41.7%) of them were confirmed to be having Helicobacter pylori (H. pylori) infection. Sixty patients (28.8%) were diagnosed with CRC and 171 (82.2%) underwent total proctocolectomy with ileal–pouch anal anastomosis or colectomy with ileorectal anastomosis. During the follow-up, 10 patients died of CRC (n = 7), desmoid tumor (n = 1), brain tumor (n = 1), and septic shock (n = 1). Further, the median follow-up period was significantly longer in patients with upper GI neoplasms than in those without (89 vs. 58 months, p = 0.002).
Prevalence of gastric neoplasms and treatment outcomes
Among the enrolled patients, 37 had one or more gastric neoplasms, as follows: gastric adenoma (n = 34) and gastric cancer (n = 7) (Fig. 1). Figure 2A shows the treatment outcomes of gastric neoplasms during the median follow-up period of 106 months (IQR 61–178 months).
Treatment outcomes during the median follow-up period for A gastric neoplasms (106 months, interquartile range [IQR] 61–178 months) and B duodenal neoplasms (88 months, IQR 42–145 months). AA ampullary adenoma, ESD endoscopic submucosal dissection, GA gastric adenoma, GC gastric cancer, NonAA nonampullary adenoma, OP operation, Tx treatment
A total of 21 (61.8%) of 34 patients with gastric adenoma underwent endoscopic treatment: ESD in 11 patients, EMR in 7 patients, argon plasma coagulation in 2 patients, and band ligation in 1 patient. Of the remaining 13 patients, 10 were lost to follow-up and the other 3 patients with histopathologically confirmed low-grade dysplasia were monitored in an outpatient clinic without treatment. In 18 patients who underwent EMR or ESD for gastric adenoma, the en bloc resection rate was 100%, and the complete resection rate was 94.4% (17 of 18). Of the 21 patients who underwent endoscopic treatment, 9 (42.9%) experienced recurrence: one local, three synchronous, and five metachronous. And 7 of these cases needed further endoscopic treatment (ESD in 2, EMR in 2, and argon plasma coagulation in 3). The remaining two patients who had gastric adenoma recurrence were regularly followed up without further treatment.
Of seven patients with gastric cancer, five underwent ESD and two underwent gastrectomy. In one patient, metachronous recurrence occurred at a different site after ESD for EGC. This patient underwent repeated ESD with curative resection. No procedure-related bleeding or perforation that required surgical intervention and no procedure-related mortality occurred.
Prevalence of duodenal neoplasms and treatment outcomes
Among the enrolled patients, 100 had one or more duodenal neoplasms, as follows: nonampullary duodenal adenoma (n = 86) and ampullary adenoma (n = 53) (Fig. 1). Figure 2B shows the treatment outcome of duodenal neoplasms during the median follow-up period of 88 months (IQR 42–145 months).
Among patients with nonampullary duodenal adenoma (n = 86), 47 (54.7%) underwent endoscopic treatment: EMR in 18, argon plasma coagulation in 28, and band ligation in 1. En block resection was performed in all of the 18 patients who underwent EMR for nonampullary duodenal adenoma, and complete resection was performed in 11 (61.1%) of them. Some patients needed additional endoscopic treatments when the remnant lesion grew to > 10 mm on surveillance EGD during the follow-up: 20, 11, 5, and 1 patients underwent one, two, three, and four additional endoscopic treatments, respectively. Of 53 patients with ampullary adenoma, 31 (58.5%) were managed with endoscopic papillectomy and only 1 patient (1.9%) underwent argon plasma coagulation because a nonlifting sign was observed during submucosal saline injection. Among the 31 patients who underwent EMR for ampullary adenoma, the en bloc resection rate was 93.5% (29 of 31) and the complete resection rate was 74.2% (23 of 31). Eleven of the patients who underwent endoscopic treatment experienced local recurrence, and nine of them underwent additional endoscopic treatment: argon plasma coagulation in seven patients, EMR in one patient, and mucosectomy using forceps biopsy in one patient. No cases of procedure-related bleeding or perforation that required surgical intervention and no procedure-related mortality occurred. Further, no patient died of duodenal neoplasms during the follow-up and duodenal cancer was not observed.
Change of Spigelman stage during the follow-up
Figure 3 and Supplementary Table 1 show the change of Spigelman stage between the EGD at the time of diagnosis or treatment of duodenal neoplasms and 2 years after that. In the untreated group, the stage was significantly increased 2 years later (p = 0.0197). In the treated group, the stage after 2 years was significantly decreased (p < 0.001). The proportion of upstaging after 2 years was significantly higher in the untreated group than in the treated group (27.3% vs. 0.0%, p = 0.001).
Risk factors for upper GI neoplasms in FAP
Multivariate analysis showed that a concurrent family history of FAP (odds ratio [OR] 0.376; 95% confidence interval [CI] 0.161–0.880; p = 0.024) and duodenal neoplasms (p = 0.005) were associated with the development of gastric neoplasms. Moreover, age at diagnosis (OR 0.963; 95% CI 0.937–0.990; p = 0.007), thyroid cancer (p = 0.031), and gastric neoplasms (p = 0.005) were associated with the development of duodenal neoplasms (Table 2). In group A and B patients who underwent a genetic variant test, multivariate analysis showed that desmoid tumor (OR 5.290; 95% CI 1.196–23.403; p = 0.028) and duodenal neoplasms (p = 0.020) were associated with the development of gastric neoplasms. Moreover, gastric neoplasms (OR 6.260; 95% CI 1.504–26.056; p = 0.012) were associated with the development of duodenal neoplasms (Table 2).
Distribution of upper GI neoplasms according to APC mutations
The comparison of clinical characteristics and upper GI neoplasms between patients with and without APC mutations is summarized in Supplementary Table 2. No significant differences between the two groups were observed, including in the median age at diagnosis, underlying diseases, median follow-up period, and family history of CRC and FAP. The prevalence of gastric neoplasms was significantly higher in patients with APC mutations than in those without (18.4% vs. 0.0%, p = 0.011). The prevalence of duodenal neoplasms was not significantly different between the groups.
Figure 4 shows the distribution of gastric and duodenal neoplasms according to nucleotide number of APC mutations. Duodenal neoplasms were frequently observed in patients with changes of nucleotide number 3183_3187, followed by 532–2 and 3927_3931. The nucleotide changes and the presence of upper GI neoplasms in group A are summarized in Supplementary Table 3.
Discussion
Most patients with FAP develop > 100 colorectal adenomatous polyps at a young age. Adenomatous polyps also occur in the upper GI tract, and several studies have reported about gastric and duodenal polyps, adenoma, and cancer in patients with FAP [16,17,18]. However, few studies have focused on the outcomes of endoscopic treatment of upper GI neoplasms in these patients [11, 12]. We investigated the long-term treatment outcomes of all of the gastric and duodenal neoplasms with a larger sample size compared with the previous studies. [17, 19, 20]. In this study, upper GI neoplasms were found in 54.3% of FAP patients who underwent EGD. Among them, 6.2% had gastric cancer and 88.5% had duodenal neoplasms. Approximately half of the patients with gastric and duodenal neoplasms underwent endoscopic therapy. No procedure-related complications occurred, and no patient underwent surgery for gastric adenoma and ampullary or nonampullary duodenal adenoma during the follow-up period. Further, no patient progressed to or died of duodenal cancer.
Although the relationship between atrophic gastritis, H.pylori infection, and incidence of gastric cancer in FAP patients was not demonstrated in our study, it is well known that these factors are closely related to the incidence of gastric cancer in general population of Asia [21]. And multiple factors including high salt diet, smoking, obesity, and alcohol drinking might be played interactive roles in this regard. In FAP patients, the prevalence of gastric adenoma was reported to be up to 35% in Asia, which is higher than that in Western countries (~ 10%) [10, 22]. Gastric cancer in FAP patients was also reported to be higher in Asian than in Western countries, and this result was considered to be associated with a high prevalence of gastric cancer in the general population as previously stated. However, it has recently been reported that the incidence of gastric cancer is rapidly increasing in FAP patients in Western countries [23, 24]. Accordingly, the importance of gastric cancer as a cancer risk in FAP patients is also increasing. Previous studies have shown some cases of gastric cancer arising from FGPs [7, 8]. However, there is still no definite pathological evidence for the possibility that FGPs develop into gastric cancer. In this study, only three of seven patients presented solitary gastric cancer; the other four patients were histopathologically confirmed to have a number of adenomas around the cancer lesion. Only one patient had fundic gland polyposis on the gastric body and fundus, and we could not confirm the association between FGPs and gastric cancer in this patient. Currently, no guidelines exist for the surveillance and management of gastric lesions. It has been suggested that a classification for gastric lesions such as duodenal adenomatosis is required for the identification of early gastric cancer precursors [17]. Therefore, FAP patients with FGPs should also undergo regular surveillance EGD to monitor the change of endoscopic phenotype and detect gastric cancer early.
In FAP patients, duodenal adenoma can be found in 30–90%, and duodenal cancer is the second leading cause of death [25, 26]. The severity of duodenal adenomatosis is assessed using the Spigelman classification, and the interval of surveillance EGD is decided according to this stage [13]. The risk of duodenal cancer development also seems to be related to this stage [27]. In this study, the severity of duodenal adenomatosis, especially in the nontreated group, showed increased Spigelman stage over time. Therefore, regular follow-up for duodenal neoplasms is important for proper management in the early stage. Surgery is usually recommended for patients with stage IV disease. However, no consensus exists about the treatment of duodenal polyposis with a stage below III, and endoscopic therapy for all lesions is challenging. Because the duodenal wall is very thin, there is a risk of procedure-related complications such as perforation and bleeding. At our hospital, endoscopic therapy is mostly selectively performed for large adenomas (> 10 mm in diameter) or adenomas with high-grade dysplasia. Consequently, 58.0% of the patients with duodenal neoplasms underwent endoscopic therapy and 42.0% were carefully observed without treatment. No procedure-related mortality was observed, and no patient experienced progression to duodenal cancer during the follow-up. Considering gains and losses, treatment of all duodenal adenomatosis lesions is not necessary. However, early detection of lesions with a high risk of progressing to cancer (such as those that are larger than 10 mm, have tubulovillous or villous components on histology, and have a high grade of dysplasia) and treating them with endoscopy may be helpful in reducing invasive surgery or death from duodenal cancer. A previous study reported that endoscopic polypectomy has partly replaced open duodenotomy, as it can lower the Spigelman stage [28]. In our study, patients who underwent endoscopic therapy for duodenal adenoma showed significant downstaging according to the Spigelman classification on follow-up EGD.
In this study, the factor associated with the development of gastric neoplasms was the presence of duodenal neoplasms. Moreover, the occurrence of duodenal neoplasms was associated with the presence of gastric neoplasms. The genotype–phenotype correlation with CRC in FAP patients is well known [29]. Although it is still controversial, there have been several reports about the association between upper GI neoplasms and APC mutations at codons 564–1465 and 976–1067 [30,31,32]. In our study, duodenal neoplasms were most frequently observed in patients with changes of nucleotide number 3183_3187 (codon 1062), which is similar to the findings of a previous report. Further studies on the association between APC mutations and duodenal neoplasms are required. This association is expected to play an important role, like the Spigelman classification, in the tailored surveillance and management for each patient.
This study had several limitations. First, selection bias may be present owing to the single-center and retrospective nature of the study. In the untreated group, there were a few patients who declined treatment or were lost to follow-up. Furthermore, some of the patients who underwent endoscopic treatment were selected based on decisions made by the endoscopists. Second, more patients than anticipated (44.2%) did not undergo the APC genetic test, and it was not possible to evaluate the association between APC mutations and upper GI neoplasms in these patients. Third, some patients had a relatively short follow-up period, because patients are usually referred to a local hospital for routine evaluations after acute phase management, as Asan Medical Center is a tertiary care hospital. However, this study showed the clinical outcomes of upper GI neoplasms in a large number of FAP patients and demonstrated the different incidence of upper GI neoplasms between Asian and Western countries. Further, our study demonstrated that endoscopic treatment of selected duodenal neoplasms can decrease the severity of adenomatosis during the follow-up.
In conclusion, based on the present results, endoscopic surveillance in FAP patients is important for the detection and treatment of upper GI neoplasms in the early stage. In particular, endoscopic therapy for duodenal neoplasms can reduce the severity of duodenal polyposis and may help avoid or delay invasive surgery.
References
Brosens LA, Keller JJ, Offerhaus GJ, Goggins M, Giardiello FM (2005) Prevention and management of duodenal polyps in familial adenomatous polyposis. Gut 54:1034–1043
Järvinen H, Nyberg M, Peltokallio P (1983) Upper gastrointestinal tract polyps in familial adenomatosis coli. Gut 24:333–339
Gallagher MC, Phillips RK, Bulow S (2006) Surveillance and management of upper gastrointestinal disease in familial adenomatous polyposis. Fam Cancer 5:263–273
Syngal S, Brand RE, Church JM, Giardiello FM, Hampel HL, Burt RW (2015) ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol 110:223–262 (quiz 263)
Yang J, Gurudu SR, Koptiuch C, Agrawal D, Buxbaum JL, Abbas Fehmi SM, Fishman DS, Khashab MA, Jamil LH, Jue TL, Law JK, Lee JK, Naveed M, Qumseya BJ, Sawhney MS, Thosani N, Wani SB, Samadder NJ (2020) American Society for Gastrointestinal Endoscopy guideline on the role of endoscopy in familial adenomatous polyposis syndromes. Gastrointest Endosc 91:963–982
Aihara H, Kumar N, Thompson CC (2014) Diagnosis, surveillance, and treatment strategies for familial adenomatous polyposis: rationale and update. Eur J Gastroenterol Hepatol 26:255–262
Garrean S, Hering J, Saied A, Jani J, Espat NJ (2008) Gastric adenocarcinoma arising from fundic gland polyps in a patient with familial adenomatous polyposis syndrome. Am Surg 74:79–83
Hofgärtner WT, Thorp M, Ramus MW, Delorefice G, Chey WY, Ryan CK, Takahashi GW, Lobitz JR (1999) Gastric adenocarcinoma associated with fundic gland polyps in a patient with attenuated familial adenomatous polyposis. Am J Gastroenterol 94:2275–2281
Bianchi LK, Burke CA, Bennett AE, Lopez R, Hasson H, Church JM (2008) Fundic gland polyp dysplasia is common in familial adenomatous polyposis. Clin Gastroenterol Hepatol 6:180–185
Park SY, Ryu JK, Park JH, Yoon H, Kim JY, Yoon YB, Park JG, Lee SH, Kang SB, Park JW, Oh JH (2011) Prevalence of gastric and duodenal polyps and risk factors for duodenal neoplasm in korean patients with familial adenomatous polyposis. Gut Liver 5:46–51
Roos VH, Bastiaansen BA, Kallenberg FGJ, Aelvoet AS, Bossuyt PMM, Fockens P, Dekker E (2021) Endoscopic management of duodenal adenomas in patients with familial adenomatous polyposis. Gastrointest Endosc 93:457–466
Campos FG, Martinez CAR, Sulbaran M, Bustamante-Lopez LA, Safatle-Ribeiro AV (2019) Upper gastrointestinal neoplasia in familial adenomatous polyposis: prevalence, endoscopic features and management. J Gastrointest Oncol 10:734–744
Spigelman AD, Williams CB, Talbot IC, Domizio P, Phillips RK (1989) Upper gastrointestinal cancer in patients with familial adenomatous polyposis. Lancet 334:783–785
Jang YH, Lim SB, Kim MJ, Chung HJ, Yoo HW, Byeon JS, Myung SJ, Lee W, Chun S, Min WK (2010) Three novel mutations of the APC gene in Korean patients with familial adenomatous polyposis. Cancer Genet Cytogenet 200:34–39
O’Leary NA, Wright MW, Brister JR, Ciufo S, Haddad D, McVeigh R, Rajput B, Robbertse B, Smith-White B, Ako-Adjei D, Astashyn A, Badretdin A, Bao Y, Blinkova O, Brover V, Chetvernin V, Choi J, Cox E, Ermolaeva O, Farrell CM, Goldfarb T, Gupta T, Haft D, Hatcher E, Hlavina W, Joardar VS, Kodali VK, Li W, Maglott D, Masterson P, McGarvey KM, Murphy MR, O’Neill K, Pujar S, Rangwala SH, Rausch D, Riddick LD, Schoch C, Shkeda A, Storz SS, Sun H, Thibaud-Nissen F, Tolstoy I, Tully RE, Vatsan AR, Wallin C, Webb D, Wu W, Landrum MJ, Kimchi A, Tatusova T, DiCuccio M, Kitts P, Murphy TD, Pruitt KD (2016) Reference sequence (RefSeq) database at NCBI: current status, taxonomic expansion, and functional annotation. Nucleic Acids Res 44:D733–D745
Ngamruengphong S, Boardman LA, Heigh RI, Krishna M, Roberts ME, Riegert-Johnson DL (2014) Gastric adenomas in familial adenomatous polyposis are common, but subtle, and have a benign course. Hered Cancer Clin Pract 12:4
Leone PJ, Mankaney G, Sarvapelli S, Abushamma S, Lopez R, Cruise M, LaGuardia L, O’Malley M, Church JM, Kalady MF, Burke CA (2019) Endoscopic and histologic features associated with gastric cancer in familial adenomatous polyposis. Gastrointest Endosc 89:961–968
Wood LD, Salaria SN, Cruise MW, Giardiello FM, Montgomery EA (2014) Upper GI tract lesions in familial adenomatous polyposis (FAP): enrichment of pyloric gland adenomas and other gastric and duodenal neoplasms. Am J Surg Pathol 38:389–393
Angsuwatcharakon P, Ahmed O, Lynch PM, Lum P, Gonzalez GN, Weston B, Coronel E, Katz MHG, Folloder J, Lee JH (2020) Management of ampullary adenomas in familial adenomatous polyposis syndrome: 16 years of experience from a tertiary cancer center. Gastrointest Endosc 92:323–330
Martin I, Roos VH, Anele C, Walton SJ, Cuthill V, Suzuki N, Bastiaansen BA, Clark SK, von Roon A, Dekker E, Latchford A (2020) Gastric adenomas and their management in familial adenomatous polyposis. Endoscopy. https://doi.org/10.1055/a-1265-2716
Rahman R, Asombang AW, Ibdah JA (2014) Characteristics of gastric cancer in Asia. World J Gastroenterol 20:4483–4490
Offerhaus GJ, Giardiello FM, Krush AJ, Booker SV, Tersmette AC, Kelley NC, Hamilton SR (1992) The risk of upper gastrointestinal cancer in familial adenomatous polyposis. Gastroenterology 102:1980–1982
Mankaney G, Leone P, Cruise M, LaGuardia L, O’Malley M, Bhatt A, Church J, Burke CA (2017) Gastric cancer in FAP: a concerning rise in incidence. Fam Cancer 16:371–376
Walton SJ, Frayling IM, Clark SK, Latchford A (2017) Gastric tumours in FAP. Fam Cancer 16:363–369
Heiskanen I, Kellokumpu I, Järvinen H (1999) Management of duodenal adenomas in 98 patients with familial adenomatous polyposis. Endoscopy 31:412–416
Bülow S, Björk J, Christensen IJ, Fausa O, Järvinen H, Moesgaard F, Vasen HF, DAF Study Group (2004) Duodenal adenomatosis in familial adenomatous polyposis. Gut 53:381–386
Groves CJ, Saunders BP, Spigelman AD, Phillips RK (2002) Duodenal cancer in patients with familial adenomatous polyposis (FAP): results of a 10 year prospective study. Gut 50:636–641
Lepistö A, Kiviluoto T, Halttunen J, Järvinen HJ (2009) Surveillance and treatment of duodenal adenomatosis in familial adenomatous polyposis. Endoscopy 41:504–509
Zhang L, Shay JW (2017) Multiple roles of APC and its therapeutic implications in colorectal cancer. J Natl Cancer Inst 109:djw332
Enomoto M, Konishi M, Iwama T, Utsunomiya J, Sugihara KI, Miyaki M (2000) The relationship between frequencies of extracolonic manifestations and the position of APC germline mutation in patients with familial adenomatous polyposis. Jpn J Clin Oncol 30:82–88
Bertario L, Russo A, Sala P, Varesco L, Giarola M, Mondini P, Pierotti M, Spinelli P, Radice P (2003) Multiple approach to the exploration of genotype-phenotype correlations in familial adenomatous polyposis. J Clin Oncol 21:1698–1707
Disciglio V, Fasano C, Cariola F, Forte G, Grossi V, Sanese P, Lepore Signorile M, Resta N, Lotesoriere C, Stella A, Lolli I, Simone C (2020) Gastric polyposis and desmoid tumours as a new familial adenomatous polyposis clinical variant associated with APC mutation at the extreme 3’-end. J Med Genet 57:356–360
Funding
This study did not receive a specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
Jin Hee Noh, Eun Mi Song, Ji Yong Ahn, Dong-Hoon Yang, Woochang Lee, Jinyoung Hong, Aram Kim, Hee Kyong Na, Jeong Hoon Lee, Kee Wook Jung, Do Hoon Kim, Kee Don Choi, Ho June Song, Gin Hyug Lee, and Hwoon-Yong Jung have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Noh, J.H., Song, E.M., Ahn, J.Y. et al. Prevalence and endoscopic treatment outcomes of upper gastrointestinal neoplasms in familial adenomatous polyposis. Surg Endosc 36, 1310–1319 (2022). https://doi.org/10.1007/s00464-021-08406-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08406-0