Abstract
Background
Informed consent is of paramount importance in surgery. Digital media can be used to enhance patient’s comprehension of the proposed operation. The objective of this study was to examine the effects of adding a digital educational platform (DEP) to a standard verbal consent (SVC) for a laparoscopic Roux-en-Y gastric bypass (LRYGB) on patient’s knowledge of the procedure, satisfaction with the clinical encounter and duration of the consent appointment.
Methods
This prospective non-blinded randomized controlled trial allocated 51 patients, who were candidates for a LRYGB, into DEP+SVC (intervention, n = 26) or SVC (control, n = 25) groups. Data were collected at one Bariatric Centre of Excellence (Ontario, Canada) between December 2018 and December 2019. DEP consisted of a 29-slide video-supplemented module detailing the risks, benefits, expectations and outcomes for the LRYGB. Primary outcome was knowledge about the LRYGB operation following the consent discussion. Secondary outcomes were knowledge retention, patient satisfaction, and duration of time required to obtain an informed consent.
Results
Baseline demographic data were equivalent between groups except for a greater proportion of male patients in the DEP+SVC group (7/19 vs 0/25; p < 0.01). Baseline procedure-specific knowledge was equivalent between the groups (72.3 ± 11.3% vs 74.7 ± 9.6%; p = 0.41). Post-consent knowledge was significantly higher in the DEP + SVC vs SVC group (85.0 ± 8.8% vs 78.7 ± 8.7%; p = 0.01; ES = 0.72). The duration of time to obtain informed consent was significantly shorter for the DEP + SVC vs SVC group (358 ± 198 sec vs 751 ± 212 sec; p < 0.01; ES = 1.92). There was no difference in knowledge retention at 4–6 weeks (84.4 ± 10.2% vs 82.9 ± 6.8%; p = 0.55) and in patient satisfaction (31.5 ± 1.1 vs 31 ± 2.7; p = 0.10).
Conclusion
The addition of a DEP online module to a standard verbal consent for LRYGB resulted in improved patient’s understanding of the procedure-specific risks and benefits, high patient satisfaction, and over 50% time savings for the bariatric surgeon conducting the consent discussion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The modern physician–patient relationship, based on shared decision making, differs vastly from the traditional paternalistic models of care. In surgery, true informed consent illustrates a practical application of this shared decision making platform [1]. Although informed consent has become a legal statute in many countries, it is often poorly executed in practical application [2]. In fact, the Canadian Medical Protective Association reported that 65% of medicolegal cases from 2008 to 2013 involved informed consent for surgery [3].
To ensure true informed consent, patients must comprehend the information presented to them [4]. Consent without understanding undermines the shared decision making necessary in the modern surgeon–patient relationship [4]. Yet, a variety of factors inherent to current surgical practice often lead to suboptimal consent processes [5]. Demonstrating this, a 2015 quality assurance review of informed surgical consent documented a recorded consent discussion in only 26% in surgical dictations [6].
Technology has the ability to not only enhance a patient’s understanding of the risks, benefits and alternatives to a proposed operative procedure, but also to standardize and ensure the comprehensiveness of the consent discussion [6]. Current literature examining the use of technology for informed consent discussions is sparse. Use of a 7-min video resulted in an 18% increase in knowledge of a urological procedure as compared to standard verbal communication during consent in one randomized controlled trial [7]. The addition of an iPad application to the standard verbal consent for pelvic reconstructive surgery did not improve patient comprehension immediately post-counselling and resulted in poorer retention of the information 6 weeks after surgery [8]. These conflicting results represent the current state of the literature examining the role of technology in informed consent discussions.
The objective of this study was to add a 29-slide interactive, video-supplemented module (DEP) for the laparoscopic Roux-en-Y gastric bypass (LRYGB) to a standard verbal consent (SVC), and to explore the effects of completing the DEP module on patient’s immediate and delayed knowledge of risks, benefits, alternatives and expected outcomes of the LRYGB, satisfaction with the consent appointment, and duration of time required for a face-to-face interaction between a bariatric surgeon and a patient to obtain an informed consent.
Hypothesis
-
1.
Patients who complete the DEP module in addition to the SVC will have greater knowledge about the risks, benefits, alternatives and expected outcomes of the LRYGB operation, as compared to patients that complete the SVC alone.
-
2.
Patients who complete the DEP module in addition to the SVC will have greater retention of knowledge about the risks, benefits, alternatives and expected outcomes of the LRYGB operation in 4–6 weeks after the consent appointment, as compared to patients that complete the SVC alone.
-
3.
Patients who complete the DEP module in addition to the SVC will report equivalent satisfaction with the clinical encounter as compared to patients that complete the SVC alone.
-
4.
Patients who complete the DEP module in addition to the SVC will require less face-to-face time with the bariatric surgeon to obtain an informed consent for the LRYGB operation as compared to patients that complete the SVC alone.
Methods
Study design
This prospective non-blinded randomized controlled trial was conducted at a Bariatric Centre of Excellence of a tertiary-care academic hospital in Ontario, Canada between December 2018 and December 2019. CONSORT study flow diagram is shown in Fig. 1. The University Research Ethics Board approved this study (6024294).
Participants, inclusion and exclusion criteria
Adult patients (age > 18 years) who underwent a multidisciplinary assessment at the Bariatric Centre of Excellence and were deemed eligible to proceed with a primary LRYGB for management of severe obesity and obesity-related comorbidities were included in this study. Patients who were proceeding with a conversion bariatric procedure to a LRYGB; who were not able to speak, read, and write English; who were not able to access and view the interactive DEP module; and who were not able to give informed consent were excluded from the study.
Randomization
Patients were randomly allocated in a 1:1 ratio to the intervention group (interactive digital education module in addition to the standard verbal consent, DEP+SVC) or the control group (standard verbal consent, SVC). The participant allocation sequence was generated using unrestricted randomization with a closed envelope technique. All participants were allocated to study groups prior to the start of the intervention and data collection.
Baseline demographic data
Participant’s demographic data including age, sex, level of education (“did not complete high school”, “high school”, “college”, “university”), background in medical field (yes/no), and English literacy score were collected. Participants were also asked whether they had previous consultations with a bariatric surgeon (yes/no).
Baseline assessment of procedure-specific knowledge
Participants were asked to complete a multiple choice test (MCQ, 19 questions, with a maximum score of 19, Online Appendix 1) to assess their knowledge of the risks, benefits, alternatives and expected outcomes of the LRYGB operation. Results of the baseline knowledge test were not discussed with the participants. Study participants were also asked to rate their level of understanding of the LRYGB operation on a scale from 0 to 10 (0—no prior knowledge/10—I know everything).
Intervention Group (DEP+SVC)
Participants randomized to the DEP+SVC group began their visit with the bariatric surgeon with a standardized history, physical examination and a review of pertinent investigations. Participants were then given access to a computer with a link to an online interactive, video-supplemented DEP module that consisted of 29 slides discussing risks, benefits, alternatives and expected outcomes for a LRYGB operation. The surgeon left the room while the participant was completing the DEP module (Online Appendix 2). There was no time limit to complete the module and participants progressed through the module at their own pace. Participants were allowed to scroll back and forth within the module to review topics that they may not have completely understood. Once the participant completed the module, the surgeon returned to review and clarify the consent issues and answer additional questions. Upon the completion of this process, informed consent was assumed and documented with a signed consent form.
Control group (SVC)
Participants randomized to the SVC group began their visit with the bariatric surgeon with a standardized history, physical examination and a review of pertinent investigations. The surgeon then discussed the LRYGB operation, indications for surgery, alternatives, risks, complications, weight loss expectations and anticipated recovery. The participant was given the opportunity to ask questions during the consent process. Upon the completion of this process, informed consent was assumed and documented with a signed consent form.
Bariatric surgeons
There were three bariatric surgeons at our institution at the time of this study. The operative technique was standardized between all three surgeons. The history and physical examination was performed using a standard template to ensure all relevant information was collected. The information regarding indications for surgery, alternatives, risks, complications, weight loss expectations and anticipated recovery that surgeons delivered as part of the standard verbal consent (SVC) was standardized to limit variability between surgeons.
Post-intervention procedure-specific knowledge
Once the clinical encounter with the surgeon was completed and consent form for LRYGB operation was signed, participants were asked to complete the 19-question MCQ test to assess their knowledge of the risks, benefits, alternatives and expected outcomes of the LRYGB operation. The MCQ test was identical to the one used for baseline assessment (Online Appendix 1). Participants also rated their level of understanding of the LRYGB operation after the consent appointment on a scale from 0 to 10 (0—no prior knowledge/10—I know everything). Retention of procedure-specific knowledge was assessed again in 4–6 weeks using the same 19-question MCQ test.
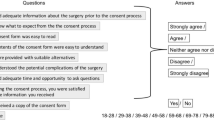
Participant satisfaction
Participants in both groups completed a modified Client Satisfaction Questionnaire (CSQ-8, maximum score 32) [9] after signing a consent form to assess their level of satisfaction with the clinical encounter.
Time to obtain an informed consent
The duration of time for the face-to-face encounter between the bariatric surgeon and the participant was measured in seconds. This time excludes the time required to obtain the history, perform the physical examination and review relevant investigations. For participants in the DEP+SVC group, the timer was started when the surgeon returned to review and clarify the consent issues and answer additional questions following completion of the DEP module. The timer was stopped once the consent form was signed. For participants in the SVC group, the timer was started when the surgeon started the discussion of the risks, benefits, alternatives and expected outcomes of the LRYGB operation and was stopped once the consent form was signed.
Sample size
Assuming a standard deviation of 3.5 for the MCQ scores and a large Cohen’s d effect size of 1.1, we recruited 51 patients to detect a 4 point difference in MCQ score (20%) between the two groups, with 80% power for the two-sample t test (∝ = 0.05). We chose to power our study to detect a 20% difference in MCQ scores as we deemed this to be a clinically significant difference in knowledge of the LRYGB operation.
Statistical analyses
Descriptive statistics were calculated. A two-sample t test was used for between-group comparisons and a paired t test was used for within-group comparisons of continuos variables. A Pearson Chi 2 test was used for between-group comparisons of categorical variables. Effect sizes were calculated using Cohen’s d. Pearson correlation coefficients (2-tailed) were calculated for level of education, immediate and delayed post-intervention knowledge assessment scores stratified by group allocation. Statistical significance was set to α = 0.05. Data are reported as mean (standard deviation) unless otherwise stated. All statistical analysis was performed using STATA version 16.0.
Results
A total of 51 patients were recruited and randomly allocated to the DEP+SVC group (intervention, n = 26) and the SVC group (control, n = 25). Baseline demographic data for participants in each group are presented in Table 1. Participant characteristics were similar between groups with the exception of sex (7 M:19F vs 0 M:25F, p < 0.01).
Procedure-specific knowledge
Baseline procedure-specific knowledge was similar between the groups (Table 2). Participants in both groups had good knowledge of the LRYGB operation prior to the consent appointment with a mean score of over 70%. Immediate post-intervention knowledge was significantly higher in the DEP+SVC group as compared to the SVC group with a Cohen’s d effect size of 0.72 (Table 2). Participants in the DEP+SVC group also demonstrated a significantly greater increase in knowledge from baseline to post-intervention as compared to participants in the SVC group (12.7(9.4)% vs 4.0(7.6)%; p < 0.01). There was a significant within-group knowledge increase from baseline to post-intervention for participants in the DEP+SVC group (72.3(11.3)% vs 85.0(8.8)%; p < 0.01; Effect size (d) = 1.23) and for participants in the SVC group (74.7(9.6)% vs 78.7(8.7); p = 0.02; Effect size (d) = 0.45).
Delayed post-intervention procedure-specific knowledge was similar between DEP+SVC and SVC group (Table 2). There was a significant increase in the procedure-specific knowledge between immediate and delayed post-intervention assessment within the SVC group (78.7(8.7)% vs 82.9(6.8)%; p = 0.03; Effect size (d) = 0.53); however, no significant increase within the DEP + SVC group (85.0(8.8)% vs 84.4(10.2)%; p = 0.54). There was a significant increase in the procedure-specific knowledge between baseline and delayed post-intervention assessment within the DEP+SVC group (72.3(11.3)% vs 84.4(10.2)%; p < 0.01; Effect size(d) = 1.12) and the SVC group (74.7(9.6)% vs 82.9(6.8)%; p < 0.01; Effect size (d) = 0.96).
Examining the correlation between level of education and immediate post-intervention knowledge assessment scores demonstrated a significant moderate positive correlation for participants in the DEP+SVC group (rho = 0.58; p < 0.01; Table 3). Similarly, a significant weak positive correlation was demonstrated for level of education and delayed post-intervention knowledge assessment scores for participants in the DEP+SVC group (rho = 0.49; p = 0.02; Table 3).
Self-reported level of understanding of the LRYGB operation
Self-reported level of understanding of the LRYGB operation at baseline and post-intervention was similar between the groups (Table 2). There was a significant increase in self-reported level of understanding of the LRYGB operation from baseline to post-intervention in the DEP+SVC group (70(17)% vs 90.0(0.6)%; p < 0.01; Effect size (d) = 1.20) and the SVC group (68(18)% vs 85.8(1.4)%; p < 0.01; Effect size (d) = 1.03).
Time to obtain informed consent
The time required for the face-to-face encounter between the bariatric surgeon and the participant was significantly shorter in the DEP+SVC group as compared to the SVC group with a Cohen’s d effect size of 1.92 (Table 2).
Satisfaction with the clinical encounter
The self-reported post-intervention satisfaction with the clinical encounter was very high and similar between the groups (Table 2).
Satisfaction with the DEP online module
Ninety-seven percent of participants in the intervention group were satisfied with the online DEP module.
Discussion
We conducted a prospective single-centre non-blinded randomized controlled trial to compare the effects of adding a 29-slide interactive, video-supplemented online digital education platform (DEP) module to a standard verbal consent (SVC) versus SVC alone. Completion of the online DEP module in addition to the SVC resulted in greater procedure-specific knowledge immediately after the consent appointment with a moderate to large effect size (Cohen’s d = 0.72), and significantly shorter face-to-face time between the bariatric surgeon and the participant (Cohen’s d = 1.92), with equivalent and very high patient satisfaction. The DEP online module was seamlessly integrated into the flow of a busy bariatric surgery clinic, and resulted in a significant increase in knowledge from baseline to post-intervention with a large effect size (Cohen’s d = 1.23). Completion of the DEP module along with the SVC resulted in a significant increase in the self-reported level of understanding of the LRYGB operation (Cohen’s d = 1.20).
Completion of DEP module in addition to the SVC resulted in greater knowledge of risks, benefits, alternatives and expected outcomes of the LRYGB operation immediately post-consent discussion when compared to the SVC alone. Similar results for a digital education platform were reported in an Australian study using portable video media for the procedure of ureteric stent insertion and cystoscopy [7]. The DEP module in our study had a unique combination of text, images and video, delivered in a visually appealing and concise package. We believe that presenting the information in this way supported a more engaged and dynamic learning process. This was demonstrated by a 97% mean satisfaction score for the module reported in our study. Furthermore, our DEP module had several checkpoints, where the study participant had to click a tickbox confirming they have understood the information that was presented to them. These checkpoints were placed at each critical part of the informed consent module (e.g. creation of gastrojejunostomy anastomosis and the potential risk of an anastomotic leak).
The result of the higher score on the post-intervention procedure-specific knowledge assessment with a smaller standard deviation, and a moderate to large effect size for the DEP intervention highlights the benefits of learning by means of an interactive digital media, as compared to the traditional didactic verbal consent process. Our result is likely a reflection of the passive role that patients often play in the traditional verbal consent, whereby they passively listen to the surgeon describing a procedure and its risks, often riddled with medical jargon. It is important to emphasize that bariatric surgeons in our study did their best and spent an average of 12.5 min explaining the risks, benefits, alternatives and expected outcomes of the LRYGB operation to participants randomized to the SVC group. They used a standardized consent template to ensure all relevant information was discussed and to decrease possible surgeon-related confounding. Indeed, within-group significant increase in procedure-specific knowledge for participants in the SVC group confirms appropriate delivery of information to the study participants; however, participants who completed the DEP module still had significantly higher post-intervention procedure-specific knowledge. This highlights an important strength of the DEP module—patients can progress through relevant information at their own pace, with pictures and videos emphasizing the most salient teaching points. Because participants were allowed to progress at their own pace, the face-to-face time spent between the surgeon and the study participant to obtain informed consent was significantly shorter in the DEP+SVC group compared to the SVC group. Nearly 7 min of face-to-face time were saved per clinical encounter in the DEP+SVC group, which can translate into a substantial increase in the overall efficiency of a busy bariatric surgery clinic, potentially allowing the surgeon to see a greater number of patients per day. This, in turn, can reduce wait times between referral and consultation, and improve access to care. Importantly, patients’ satisfaction with the clinical encounter in the DEP+SVC group remained very high despite spending less face-to-face time with the surgeon.
Delayed post-intervention assessment of procedure-specific knowledge at 4–6 weeks did not show a significant decrease in knowledge within the DEP+SVC group, suggesting retention of acquired knowledge over time. Interestingly, there was a significant increase in procedure-specific knowledge between immediate and delayed assessment for participants in the SVC group. This could have been because participants in the SVC group decided to engage in additional independent research following their immediate post-intervention assessment; however, we were not able to capture this information in our study. This is an area that warrants further research as it could suggest a barrier to knowledge acquisition at the time of consent discussion for participants in the SVC group as perhaps they did not want to ask additional questions or admit that they did not fully understand. The DEP module can address some of these barriers.
In future studies we plan to develop additional DEP modules for other bariatric and general surgery operations, including operations performed in an emergency setting when there may be limited time for a comprehensive discussion of risks and benefits. The effectiveness of these modules should be established using a similar methodology to the current study. As our results demonstrate, the use of the digital education platform has clear benefits for the patients, who are more likely to be adequately informed about their procedure and be very satisfied with the consent process. We are also hopeful that our results will be replicated across different patient populations and other surgical specialties.
Our study has several limitations. First, we were not able to blind the bariatric surgeon or the patient to the group randomization given the requirement for the surgeon to know when to ask the patient to view the DEP module and when to proceed with a standard verbal consent. Our finding of significant within-group increase in knowledge from baseline to post-intervention assessment for participants in the SVC group, and an average of 12.5 min spent on a comprehensive discussion of the LRYGB operation in that group minimizes the likelihood of biased delivery of information between the surgeon and the patient. Second, our results should not be generalized to other procedures or to other settings, such as emergency surgery. The relatively high baseline procedure-specific knowledge for participants in our study could be attributed to most of our patients having at least a high school level of education, most completing a mandatory “pre-surgical” class prior to their consent appointment, and most doing some research on the risk and benefits of the LRYGB operation prior to coming to see the bariatric surgeon for the consent appointment. We would not expect to see such a high baseline level of procedure-specific knowledge for operations that are performed without a multidisciplinary assessment or in an emergency setting. Third, we excluded participants who could not read English. Future studies can consider narrated online module for patients who cannot read and translated modules for patients who do not speak or understand English. In fact, translating these modules to other languages would allow us to better serve a diverse and multicultural patient population. There remains significant untapped potential in harnessing digital education modules to address the wide breadth of surgical procedures as well as the diverse patient population that comprise the modern surgical practice.
Conclusions
Addition of an interactive, video-supplemented online digital education module to standard verbal consent for a laparoscopic Roux-en-Y gastric bypass operation resulted in greater comprehension of the procedure-specific information and substantial time savings for the bariatric surgeon without compromise to patient satisfaction or surgeon–patient relationship. Implementation of this module in bariatric surgery clinics is expected to result in higher efficiency, improved patient flow and reduced wait times to see a bariatric surgeon for consultation.
References
(1980) Reibl v. Hughes. Dominion law reports, Supreme Court of Canada, pp 1–35
Murphy G (2004) Law Reform Agencies, Department of Justice Canada.
Evans KG (2006) Consent: A guide for Canadian physicians.
Murphy WJ (1976) Canterbury v. Spence–the case and a few comments. Forum 11:716–726
Armstrong AW, Alikhan A, Cheng LS, Schupp C, Kurlinkus C, Eisen DB (2010) Portable video media for presenting informed consent and wound care instructions for skin biopsies: a randomized controlled trial. Br J Dermatol 163:1014–1019
Hanson M, Pitt D (2017) Informed consent for surgery: risk discussion and documentation. Can J Surg 60:69–70
Winter M, Kam J, Nalavenkata S, Hardy E, Handmer M, Ainsworth H, Lee WG, Louie-Johnsun M (2016) The use of portable video media vs standard verbal communication in the urological consent process: a multicentre, randomised controlled, crossover trial. BJU Int 118:823–828
Kinman CL, Meriwether KV, Powell CM, Hobson DTG, Gaskins JT, Francis SL (2018) Use of an iPad application in preoperative counseling for pelvic reconstructive surgery: a randomized trial. Int Urogynecol J 29:1289–1295
Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD (1979) Assessment of client/patient satisfaction: development of a general scale. Eval Program Plann 2:197–207
Acknowledgements
The authors would like to thank patients from Kingston Bariatric Centre of Excellence for participating in this study. They would also like to thank Jennifer Bunn for help in data collection and patients recruitment.
Funding
Department of Surgery Research Fund, Queen’s University.
Author information
Authors and Affiliations
Contributions
MA, UM, BZ: Study conception and design. BZ: Acquisition of data. MA, UM, DIR, BZ: Analysis and interpretation of data. MA, UM, BZ: Drafting of manuscript. MA, UM, DIR, BZ: Critical revision.
Corresponding author
Ethics declarations
Disclosures
Boris Zevin received an educational grant from Ethicon and research funding from Medtronic. Mancini, Almakky and Robertson do not have conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zevin, B., Almakky, M., Mancini, U. et al. Digital approach to informed consent in bariatric surgery: a randomized controlled trial. Surg Endosc 36, 809–816 (2022). https://doi.org/10.1007/s00464-020-08277-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08277-x